Dairy free foods for baby
Meal Plans & Recipe Ideas for Your Dairy-Free Baby or Tot
Some babies and toddlers are not able to tolerate dairy, whether from a lactose intolerance or a cow’s milk protein allergy.1 Knowing what foods and beverages to feed your little one while avoiding dairy can help make sure they are getting the nutrients needed for growth and development.
When do babies need to avoid dairy?Breastfed Baby
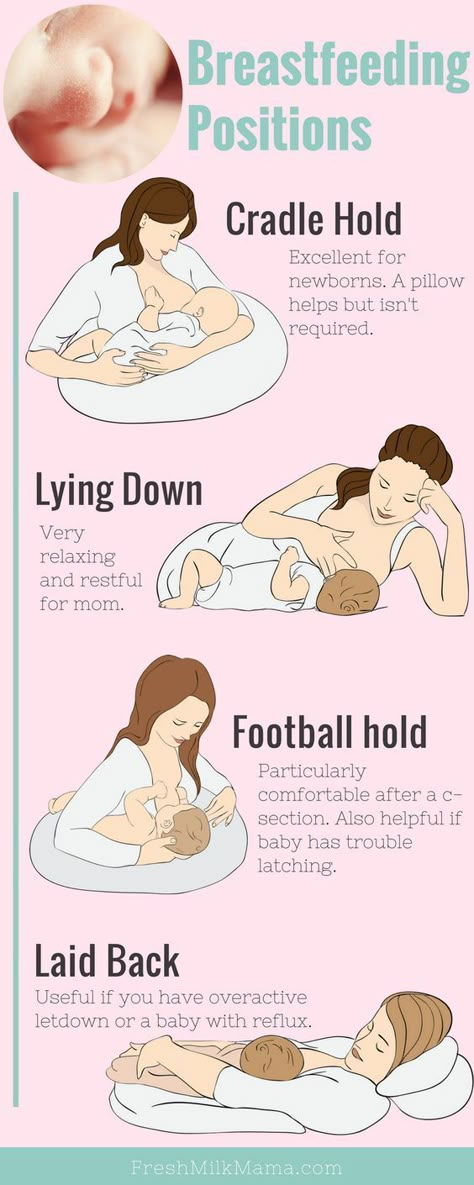
If your breastfed baby has been diagnosed with a cow’s milk protein allergy or lactose intolerance, you can likely continue to breastfeed as long as you eliminate sources of dairy from your own diet.2,3 Continue to work with your or your child’s health care provider as you eliminate sources of dairy.
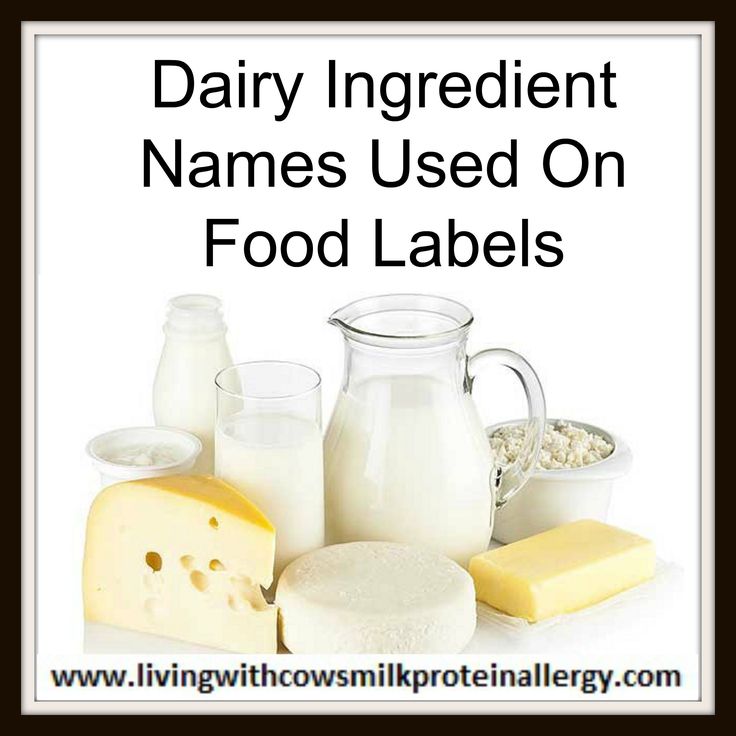
Be sure to always read all foods labels to see if there are any dairy ingredients in the product you purchase.
Read more:
Meal Plan & Tips to Eat Dairy Free while Breastfeeding
Is Your Baby Reacting to Something in your Milk?
Formula Fed Baby
If your formula fed baby has been diagnosed with a cow’s milk protein allergy or sensitivity to lactose, you will likely need to choose either a low lactose or lactose-free formula, or a formula that does not contain intact cow’s milk protein.4
Always speak with your child’s health care provider before switching formulas.
Read more:
Does Your Baby Need a Sensitive Formula?
Does my Baby Need a Hypoallergenic Formula?
Once your baby begins to eat solids, look at labels carefully to avoid dairy ingredients. Read on for information, tips, and meal ideas.
For more information on lactose intolerance versus a cow’s milk protein allergy, check out this article:
Does my Baby or Toddler have a Milk Allergy or a Lactose Intolerance?
Making sure your child gets the right nutrition while eliminating dairyDairy foods provide several important nutrients, including protein, calcium, and vitamin D (which is often fortified, or added to, dairy products). 5 When eliminating dairy, it is necessary to incorporate other food sources (in the texture your baby is ready for) that are rich in these particular nutrients.6
5 When eliminating dairy, it is necessary to incorporate other food sources (in the texture your baby is ready for) that are rich in these particular nutrients.6
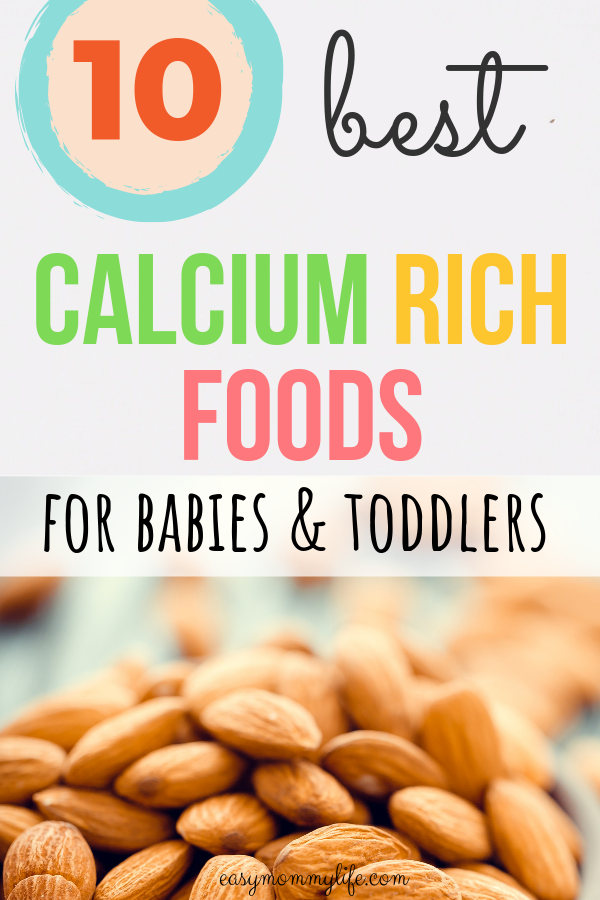
Food sources of calcium: Fortified plant-based milk alternatives, fortified orange juice, canned sardines and salmon with bones, fortified dairy alternatives such as a non-dairy yogurt, tofu, soybeans, spinach, kale.8
Read more: Why Does Calcium Matter for Babies, Tots, and Mama
Food sources of vitamin D: Salmon, fortified plant-based milk alternatives, fortified cereals, eggs, canned light tuna, portabella mushrooms, and sunlight.9
Read more: Why Does Vitamin D Matter for Babies, Tots, and Mama
Food sources of protein: Fish, poultry, meat, beans, legumes, peas, nuts, seeds, tofu, eggs, whole grains.
Read more: Protein: Getting Enough and the Best Sources
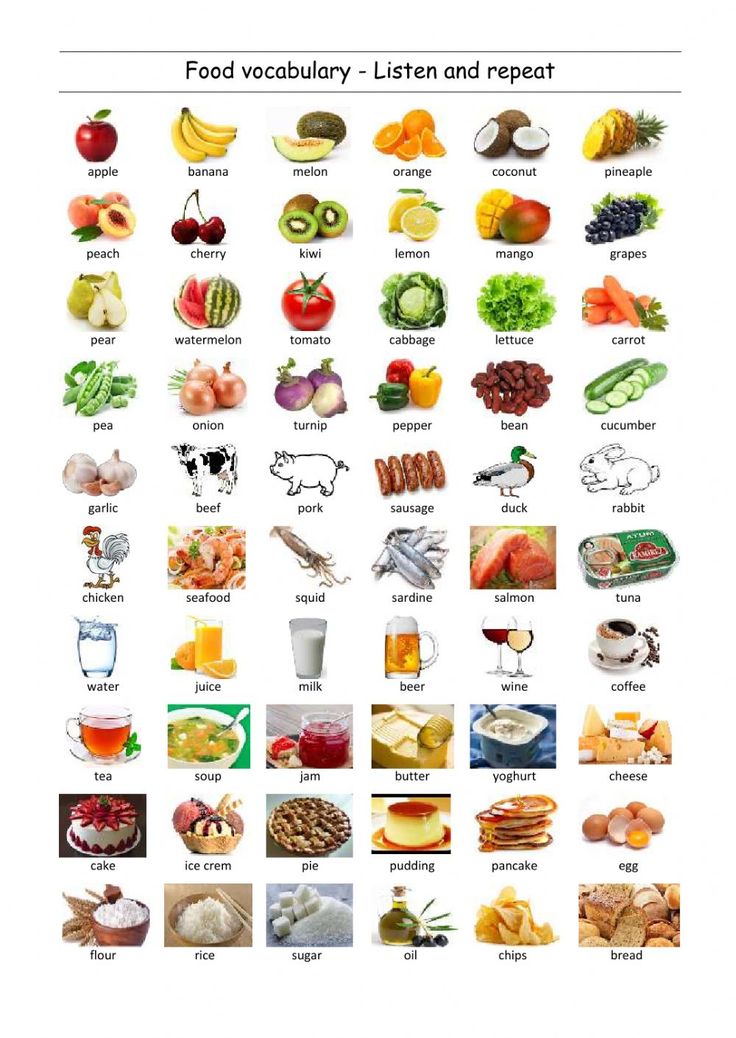
Offer a wide variety of dairy-free foods to your childIt’s important to know that there are plenty of other foods that do not contain dairy. Offer these foods often as long as your child is not allergic to them. All whole fruits, vegetables, whole grains, legumes, beans, nuts, seeds, poultry, fish, and eggs are dairy free. Be sure to feed your child a wide variety of these foods to help meet their nutrient needs.
Offer these foods often as long as your child is not allergic to them. All whole fruits, vegetables, whole grains, legumes, beans, nuts, seeds, poultry, fish, and eggs are dairy free. Be sure to feed your child a wide variety of these foods to help meet their nutrient needs.
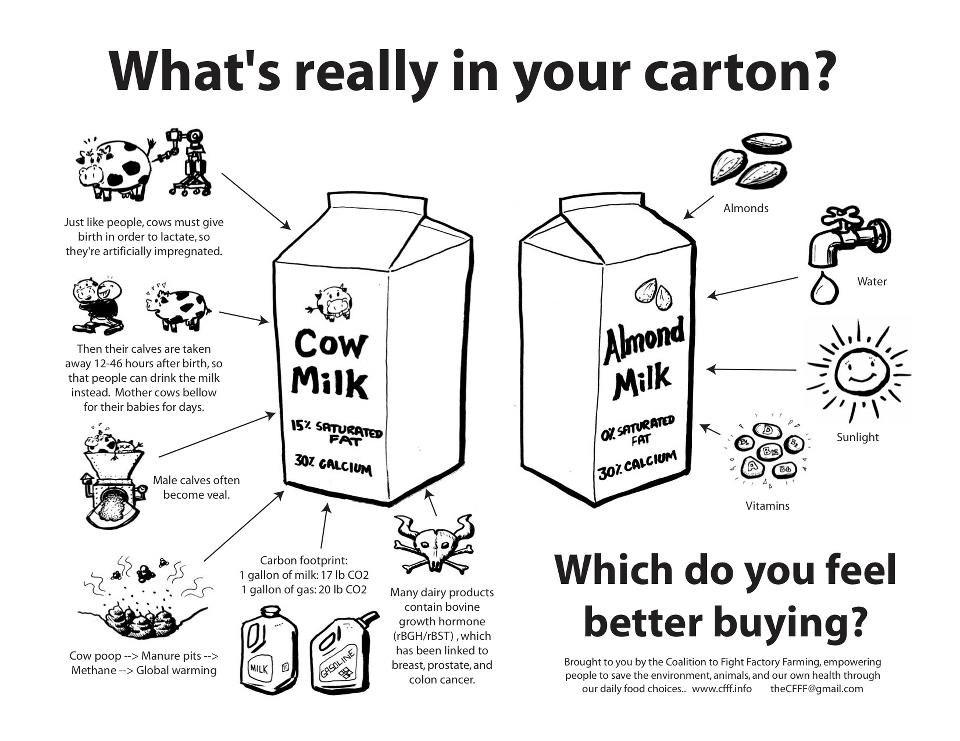
Non-dairy alternatives can be used for a child with a lactose intolerance or allergy, such as plant-based milk alternatives and plant-based yogurt alternatives. But it’s important to note that not all of these products have the same nutrients as their dairy equivalent.1
If you do choose a plant-based milk alternative, such as almondmilk or oatmilk, be sure the product is fortified with calcium and vitamin D.
Note that plant-based yogurt alternatives often have more added sugar and less protein than regular yogurt. Read nutrition fact labels and ingredient lists to ensure you’re providing your little one with foods that best meet their nutritional needs.
*While a plant-based milk alternative can be used in small amounts in baked or cooked foods, or plant-based yogurt alternative can be provided as a snack or part of a meal, babies under the age of 12 months should not be given cow’s milk nor a plant-based milk alternative to drink by the cup-full.11
These drinks do not contain all the nutrition your baby needs, and adding them in by the cup may take up valuable space in your baby’s tummy – edging out more nutritious foods, formula, and/or breastmilk.
Read more: What Type of Milk Should My Toddler Drink?
Reach out to your child’s healthcare providerIf you suspect that your child has lactose intolerance or a cow’s milk protein allergy, call their healthcare provider immediately for further support.
Wondering what might be the best choice for your baby or tot? Reach out to our team of registered dietitians and lactation consultants for free! They’re here to help on our free to live chat from Monday – Friday 8am - 6pm (EST). Chat Now!
Chat Now!
Pro Tip:
Some babies and toddlers will react to dairy ingredients that are “hidden” and not so obvious.10
Hidden dairy may be found in foods like breads, cereals, crackers, pancakes, waffles, soups, sauces, toppings, dressings, and deli meats. It’s important to read labels and avoid any foods that list “contains milk or milk ingredient.”10
The below meal plan, snack, and recipe ideas will help you choose the right foods for your baby when progressing from mostly single purees to more advanced textures and finger foods, while also excluding dairy.
Be sure to check all labels for both obvious and hidden sources of dairy.
Breakfast
Option 1: Scrambled eggs, clementine
Option 2: Dairy free yogurt such as soy, coconut, or almond, with sliced berries
Option 3: Strawberry Quinoa Cereal for Baby
Option 4: Whole grain French toast fingers with nut butter* and 100% fruit spread
Option 5: Banana pancakes (combine 1 ripe banana, 1 egg and 2 tbsp.
 whole wheat flour. Cook 3 minutes on each side over medium heat)
whole wheat flour. Cook 3 minutes on each side over medium heat)
Lunch
Option 1: Whole grain tortilla strips with mashed avocado dip
Option 2: Tuna sandwich cut into quarters, side of sliced peaches
Option 3: Chickpeas with soft cooked carrots
Option 4: Cubed and roasted butternut squash, with turkey slivers
Option 5: Mini Sweet Potato Chicken Meatballs with Cauliflower Rice and Steamed Broccoli
Dinner
Option 1: Black beans with soft cooked peppers
Option 2: Whole grain pasta with ground turkey, marinara, and roasted veggies
Option 3: Baked fish fingers with cubed and roasted sweet potato
Option 4: Mild Curry Chicken & Veggies with Brown Rice
Option 5: Lean hamburger cut into pieces with baked zucchini fries
Snacks:
Option 1: Soft cooked veggies with hummus
Option 2: Warm Peach Chunks with Nutmeg
Option 3: Hard-boiled egg, diced
Option 4: Fruited dairy free yogurt such as coconut, soy, or almond
Option 5: Applesauce mixed with small amount of nut* or seed butter
*Speak with your baby’s pediatrician before introducing allergenic foods
Let's Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday - Friday 8am - 6pm (Et).Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles:Does my Child Have a Food Allergy or a Food Intolerance?
Guidance When Raising a Child with Food Allergies
Introducing Major Food Allergens to your Infant
Our meal plans offer recipe and meal suggestions for your child. They are not designed to replace your doctor’s recommendations, nor do they take into account special nutritional needs, including allergies and intolerances, other than lactose intolerance and a cow’s milk protein allergy. The meal plans suggest serving sizes that may or may not be appropriate for your child. Please consult your doctor to determine what is best for your child.
Please consult your doctor to determine what is best for your child.
Sources
Your guide to dairy free baby food for cow's milk protein allergy
It is estimated that 1 in 14 children under the age of three will have some sort of food allergy, with the most common allergies to milk, eggs, peanuts, tree nuts, soya, fish and wheat.
Did you know that around 2% of babies have an allergy to milk or Cow’s Milk Protein Allergy (CMPA)?[1]
It’s the most common nutritional issue that babies have and it’s on the rise. Research hasn’t yet found a reason why, but as a paediatric dietitian, I am coming across more and more babies and children with CMPA.
If you would like a PDF version of this blog delivered directly to your inbox, pop your details below.
What is CMPA?Cow’s milk naturally contains a variety of nutrients, including protein. The proteins found in cow’s milk are called casein and whey. When some babies consume cow’s milk, their bodies react to these proteins and trigger an immune response releasing antibodies. These allergic reactions can happen immediately after eating any cows milk products – called an IgE mediated response, or can be delayed – called a non-IgE mediated response.
These allergic reactions can happen immediately after eating any cows milk products – called an IgE mediated response, or can be delayed – called a non-IgE mediated response.
Whatever type of milk allergy your baby has it is very important that they follow a completely dairy free diet. This doesn’t just mean avoiding cows milk but any foods that contain any cows milk products, such as butter, yoghurt, cheese, custard and ice-cream.
What about goats milk?As the proteins in cow’s milk are quite similar to the proteins of other mammalian milks, your child will also need to avoid milk from other animals too like goat’s milk, sheep milk and buffalo milk, which includes cheeses made from these milks.
What about traces of milk in manufactured foods?Milk or milk products are often used as an ingredient in lots of processed foods, like bread or flavourings, so it’s really important to check all food labels on any food products.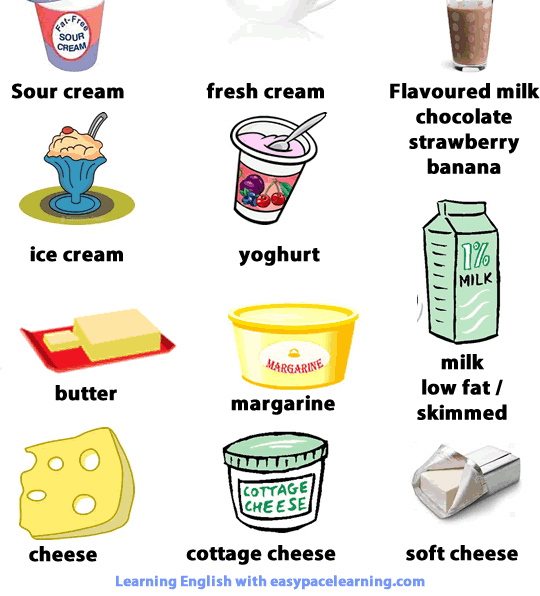 By law, if food contains any products in any form, they have to declare it prominently on the label. For example, many manufacturers display allergens in bold so it is easy to spot.
By law, if food contains any products in any form, they have to declare it prominently on the label. For example, many manufacturers display allergens in bold so it is easy to spot.
Until your dietitian tells you otherwise, you should avoid all traces of milk in foods including where the label says ‘may contain’ or ‘traces of milk’.
What are the symptoms of CMPA?Symptoms of an allergic reaction can be immediate (IgE) or delayed (non-IgE). The difference between an IgE and non-IgE reaction is the way that the reaction takes place using different parts of the immune system. Immediate means that they come on typically within 30 minutes after eating a food containing the allergen but they can take up to 2 hours. Delayed symptoms can take anywhere from two hours to several days later to show! Symptoms can include (but not limited to):
-
Eczema
-
Red skin
-
Hives
-
Swelling of the lips, tongue, mouth or body
-
Difficulty breathing
-
An itchy, runny nose
-
Tummy troubles such as vomiting, constipation or diarrhoea
-
Reflux
-
Tummy pain
-
Poor growth
-
Asthma
-
Anaphylaxis (in extreme cases)
If your baby shows any of the symptoms of CMPA, it is really important that they are seen by a healthcare professional such as your GP as soon as possible. If it’s an IgE reaction you will be referred to a paediatrician in your local hospital to confirm the diagnosis.
If it’s an IgE reaction you will be referred to a paediatrician in your local hospital to confirm the diagnosis.
IgE allergies are diagnosed in a hospital under the guidance of a Paediatrician. Your child may have skin prick tests where a small amount of the suspected allergen food is put on your baby’s skin. The surface of the skin is then scratched and the size of the ‘wheel’ it creates is measured.
They are notoriously inaccurate in babies under 1 where skin is sensitive and false positives are common.
Alternatively, a blood sample can be taken and sent off for further analysis, the results take several days to come back.
A very detailed allergen focussed history will be taken from you so it’s good to have a food diary and symptom record if possible. It is this coupled with the tests that will confirm the diagnosis.
Delayed onset reactionsIf it’s a non-IgE reaction your GP will take an allergen focussed history and may suggest an ‘exclusion diet and challenge. ’ Essentially this is a 2-4 week trial of a milk free diet to see if this improves their symptoms.
’ Essentially this is a 2-4 week trial of a milk free diet to see if this improves their symptoms.
If you are breastfeeding and you think that your little one is reacting to cow’s milk through your breastmilk, this will involve you avoiding dairy foods in your diet. If your baby is weaning, they will need to avoid cow’s milk too.
Your GP should organise a referral to a Registered Dietitian too as the diagnosis is only confirmed when your baby is ‘challenged’ i.e. when the food is reintroduced producing a return of their symptoms.
This can be carried out at home for most non-IgE babies, and best practice is to do this alongside a Registered Dietitian. You should be aware that access to an NHS dietitian can be scarce in some areas and an appointment may not be offered in time.
If this is the case, you are welcome to book an appointment with one of my fully qualified paediatric dietitians on the team. The link to book is here.
I’ve seen other tests I can buy online. Are these any good?
Are these any good? There are lots of alternative tests marketed to diagnose allergies such as IgG, vega testing, iridology, hair analysis, kinesiology or cytotoxic testing. These are widely available online and the costs can vary.
However, none have scientific evidence for their use and can’t diagnose an allergy or intolerance.
The only evidence based methods of diagnoses are the ones outlined above and all others should be avoided.
My baby reacted to milk challenges – what happens next?Once the diagnosis is confirmed, you will be advised to continue following the dairy free diet. You must be immediately referred to a Registered Dietitian with paediatric expertise if you haven’t already because by cutting out milk you are cutting out a key food group from your growing baby which if not appropriately replaced can result in poor growth and development and nutritional deficiencies, leading to health problems. It is essential that those missing nutrients are replaced with other foods in your little one’s diet.
You might have heard people use the phrase ‘cow’s milk protein intolerance’, however, this doesn’t actually exist. It’s a term that healthcare professionals have previously used to describe delayed onset or non-IgE milk allergy, but it sometimes is still used today.
What about lactose intolerance, is that different?This is not an allergy to dairy foods and is a separate condition. Lactose is the sugar that is found naturally in milk. Children with lactose intolerance have trouble breaking down the lactose in foods because they are missing the ‘lactase’ enzyme.
Often this is temporary following a nasty tummy bug, as the ‘lactase’ has been washed away. In rare cases, it is a genetic disorder where lactase isn’t produced by the body in sufficient amounts.
Lactose doesn’t cause an allergic reaction and there is no need for your baby to follow a dairy free diet. You can buy lactose free baby milk as well as lactose free versions of milk and yoghurt. Cheese is naturally low in lactose so it’s fine to have. Alternatively, you can add a couple of drops of the ‘lactase’ enzyme to normal milk.
Cheese is naturally low in lactose so it’s fine to have. Alternatively, you can add a couple of drops of the ‘lactase’ enzyme to normal milk.
Again, if you think your baby has lactose intolerance, it is really important to go see your healthcare professional for further advice.
I suspect my baby has CMPA, can I try a milk free weaning diet without seeing my GP?If you suspect that your baby/child has CMPA, you have to be very careful as by cutting out milk, your baby is at risk of being deficient in lots of nutrients, which will affect their growth and development. Below is a list of just some of the key nutrients a dairy free diet is at risk of being deficient in:
Milk and dairy foods are one of the five main food groups and contribute to a significant amount of your baby’s nutrition.
If your baby is breastfed, they will receive small amounts of dairy protein through breast milk and if formula fed, all of their nutrition comes from dairy as the majority of infant formula are derived from animal milks.
Once weaning starts, the amount of milk (and the nutrition coming from milk) gradually decreases as food intake goes up. However, milk and dairy foods still play a significant role in nourishing your little one right through their childhood.
Always seek the advice of a healthcare professional before you try a diet that avoids a whole food group as babies can become deficient in nutrients quite quickly which can impact on their future health and development.
Here is a quick list of foods a CMPA baby can have to replace some of those key nutrients:
Foods containing calcium:-
Fish with soft edible bones e.g. tinned sardines, tinned salmon and anchovies – it’s the bones that contain calcium so blend / mash them up well rather than picking them out
-
Oranges
-
Dried apricots, currants and figs
-
Nut butters such as peanut butter and almond butter
-
Tofu that has been set with calcium sulphate
-
Tahini and hummus
-
Fortified non-dairy breakfast cereals such as Ready-Brek
-
Fortified bread such as Kingsmill Vitamin Boost or Warburtons Milk Roll
-
Soya milks and yoghurts that have calcium added
-
Green veg such as kale and broccoli – however, it’s not so well absorbed by the body
-
Meat – particularly red meat such as beef or lamb for its iron content
-
Poultry – the darker meat is more nutritious
-
Fish
-
Eggs
-
Lentils
-
Beans and other pulses
-
Tofu and soya (if tolerated)
-
Nut butters
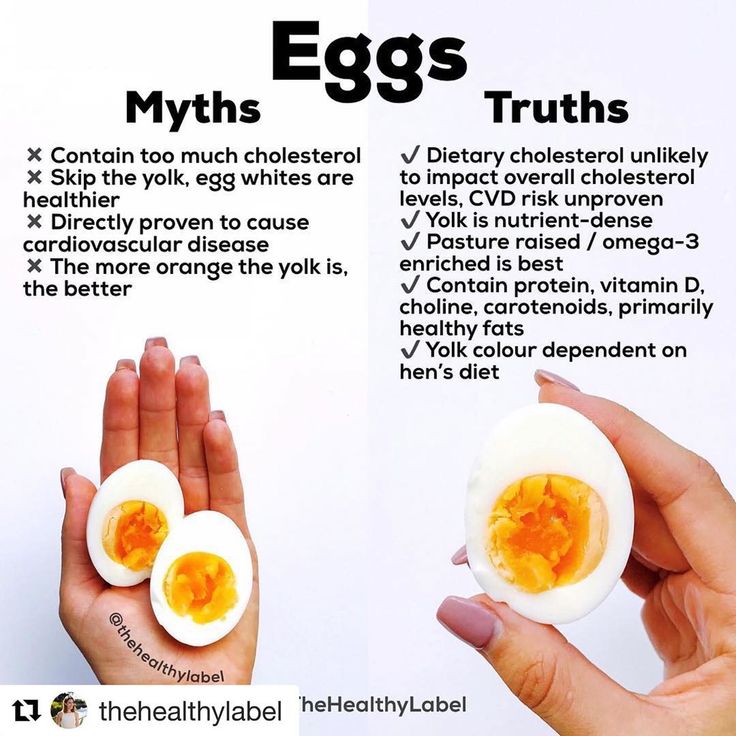
People often think that egg is a dairy food and therefore has to be avoided if your baby has CMPA. The good news is that unless your baby has a specific egg allergy, egg does not contain the same proteins as milk so your CMPA baby can enjoy eggs as part of their diet which, incidentally are an excellent source of nutrition.
The good news is that unless your baby has a specific egg allergy, egg does not contain the same proteins as milk so your CMPA baby can enjoy eggs as part of their diet which, incidentally are an excellent source of nutrition.
Seeing a Registered Dietitian is crucial because dietitians are the only nutrition professionals regulated by law that can advise you on how to manage a free-from diet without risks to your baby’s health.
Unfortunately, NHS dietitians are scarce in some areas and so it’s important to make arrangements to attend either a group or one-to-one appointment when it’s offered.
If you feel the waiting list is too long, you can also self-refer to a Registered Dietitian in private practice – look for one who is experienced in paediatrics and allergies.
What will the dietitian do?If you are breastfeeding, the dietitian will advise on the dietary changes you’ll need to make to your own diet. You don’t need to stop breastfeeding. As well as excluding dairy foods you will need to add in other foods in order to ensure your milk supply and milk quality isn’t affected. The dietitian will also be considering how your diet needs to look so that your own health is optimised.
You don’t need to stop breastfeeding. As well as excluding dairy foods you will need to add in other foods in order to ensure your milk supply and milk quality isn’t affected. The dietitian will also be considering how your diet needs to look so that your own health is optimised.
If you are formula feeding, the dietitian will assess your baby’s diet, growth, and allergy symptoms and advise the GP on which of the prescription dairy free formula would be best for your baby. There are currently 13 variants, all with their own unique formulation.
Your dietitian will decide on the most appropriate one for your baby’s unique needs.
I’m breastfeeding and my baby has CMPA – Do I need to cut milk out of my diet too?The short answer is maybe…We aren’t sure why, but CMPA is rare in breastfed babies by comparison to those on formula. One of the potential explanations is the immune benefits that breast milk contains, as well as the ‘microbiome’ or healthy gut bacteria that breastfed babies have [2].
It is important to note here that whilst CMPA is more commonly seen in formula fed babies, it can still occur in breastfed babies. Cow’s milk passes through breast milk at 100,000 times lower than that which is in cow’s milk.
What this means is that the amount of cow’s milk that gets to the baby through their mother’s milk is a lot lower than if they were to directly consume cows milk. Therefore most allergic babies are able to tolerate their mother’s milk. It also means that the vast majority of mums don’t need to follow a milk-free diet either.
However, if your baby is one of the rare ones who does react to your breastmilk, then you can try a milk free diet for a period of time (usually around 2-6 weeks) to see if the symptoms improve.
It’s essential to see a dietitian, as it is important the quality of mum’s diet doesn’t suffer, particularly their calcium intake, and also to ensure that the quality of the breast milk isn’t impacted.
It’s crucial that breastfeeding mums meet their daily calcium and vitamin D requirements.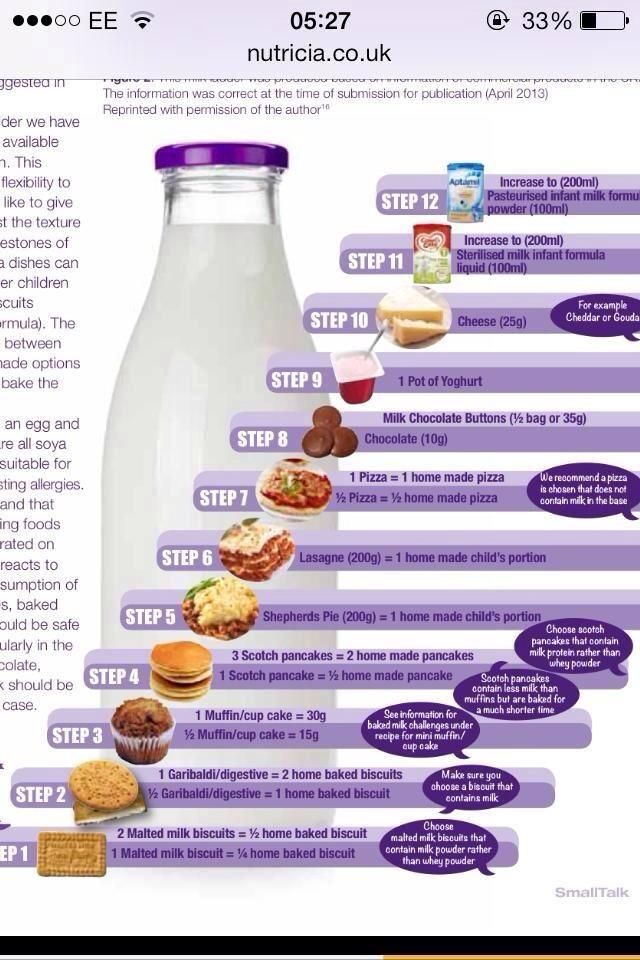 Did you know that as a breastfeeding mum, your calcium requirements increase from 700mg/day to 1250 mg/day whilst you are nursing?
Did you know that as a breastfeeding mum, your calcium requirements increase from 700mg/day to 1250 mg/day whilst you are nursing?
You will need approximately a litre of calcium enriched plant-based milk each day as well as a 10mcg vitamin D supplement just to meet your requirements.
If you don’t get enough calcium and vitamin D, it’s likely your own bone health will suffer as your baby will take the calcium and vitamin D they need from your stores instead.
If after a milk free diet your baby’s symptoms don’t improve, then your dietitian will be able to advise on what you need to do next.
Weaning on a Dairy Free DietStage 1 (around 6 months)
Research has shown that at the start of weaning it is best to start with single vegetables then fruits but progressing on to iron rich foods quite quickly. You can read more about this in my blog called ‘Why Food Before One is Just for Fun is Not True’. You don’t need to do anything differently at the start of weaning if your baby has CMPA as fruits, vegetables and all my suggested iron rich foods are dairy free.
If you need to thin down purees that are too thick, you can use expressed breast milk or some of the prescribed formula you have been given. If your dietitian has advised that your baby can have soya, you could use a little calcium and iodine fortified soya milk providing they are over 6 months old. Soya isn’t suitable for babies under 6 months.
Stage 2 onwards (7 months +)As weaning progresses and your baby is taking 3 meals a day, you will start to try and balance their meals by including protein foods such as eggs, meat, fish, beans and pulses and starchy carbohydrate foods alongside their fruits and vegetables.
However, you will need to ensure that your baby avoids all forms of milk, butter, cheese and yoghurt, and any foods that contain milk by checking all food labels to ensure foods do not contain milk.
Cross contamination can be a real problem when eating outside the home or at nursery. For example, when foods containing milk have been prepared in the same area, the milk proteins can occasionally contaminate dairy free foods and cause an allergic reaction if eaten. Do let restaurants know before you order and have a good long chat with your childcare provider before they start nursery.
Do let restaurants know before you order and have a good long chat with your childcare provider before they start nursery.
As weaning progresses and your baby starts to drop milk feeds, you need to be in close contact with your dietitian as most babies who follow a dairy-free diet need to take more breastmilk or formula than non-allergic babies in order to meet their nutritional requirements.
The dietitian will also advise on how best to balance your infant’s diet depending on what known allergies they have and also whether they require any supplements.
The limiting nutrients protein, fat, energy, calcium, iodine, vitamin A and certain B vitamins will be considered alongside your typical routine and family meals to help you plan a way of eating that meets your baby’s nutritional needs. The nutrients that your baby receives in the first two years of life affects their growth and development including their brain development and intellect [3].
When your baby has a food allergy, they are more likely to have another. This also includes little ones with severe eczema requiring regular steroid cream [4].
The advice is to introduce the other allergenic foods, one at a time between 4 months and 12 months of age. Delaying introduction of these foods beyond 12 months can actually make the likelihood of having an allergy greater [5].
It is advisable to start with egg and then peanut, after that the other allergens detailed on the list below can be offered. If you would like to know exactly how to introduce all of the allergens you can find out how in my mini online course ‘Introducing Allergens’.
Egg
Choose British red lion stamped eggs and offer both the white and the yolk together. Something like mashed or scrambled egg works well for spoon feeding or omelette strips as a finger food.
Peanuts
You mustn’t give your baby whole nuts due to the risk of choking, and peanut butter on a spoon can also pose the same risk. Puffed peanut snacks, peanut powder mixed into food or a small amount of smooth peanut butter warmed and thinned down with some of your baby’s usual milk or hot water are better options. You can add this thinned peanut butter to pureed fruits or vegetables.
Puffed peanut snacks, peanut powder mixed into food or a small amount of smooth peanut butter warmed and thinned down with some of your baby’s usual milk or hot water are better options. You can add this thinned peanut butter to pureed fruits or vegetables.
If your baby tolerates these foods without a reaction, continue offering them regularly as part of their normal diet. This repeated exposure has a protective effect.
Other allergenic foods
You can then start to offer the other common allergenic foods alongside other tolerated foods. Just offer one at a time (no more frequently than one new food per day) and just ¼ to ½ teaspoons worth, so that if your baby does react you know which one was the culprit.
-
Tree-nuts – almond, cashew, walnuts, brazil nuts, pecans, hazelnuts etc prepared in the same way as peanuts above.
-
Wheat – breakfast cereals, pasta, bread, couscous, breadsticks
-
Sesame – such as houmous which contains tahini (sesame paste)
-
Fish & seafood – cod, haddock, salmon, trout, tuna, prawns, crab, mussels
Again, if your baby tolerates them continue offering them regularly as part of their normal diet to capitalise on the protective effect of repeated exposure.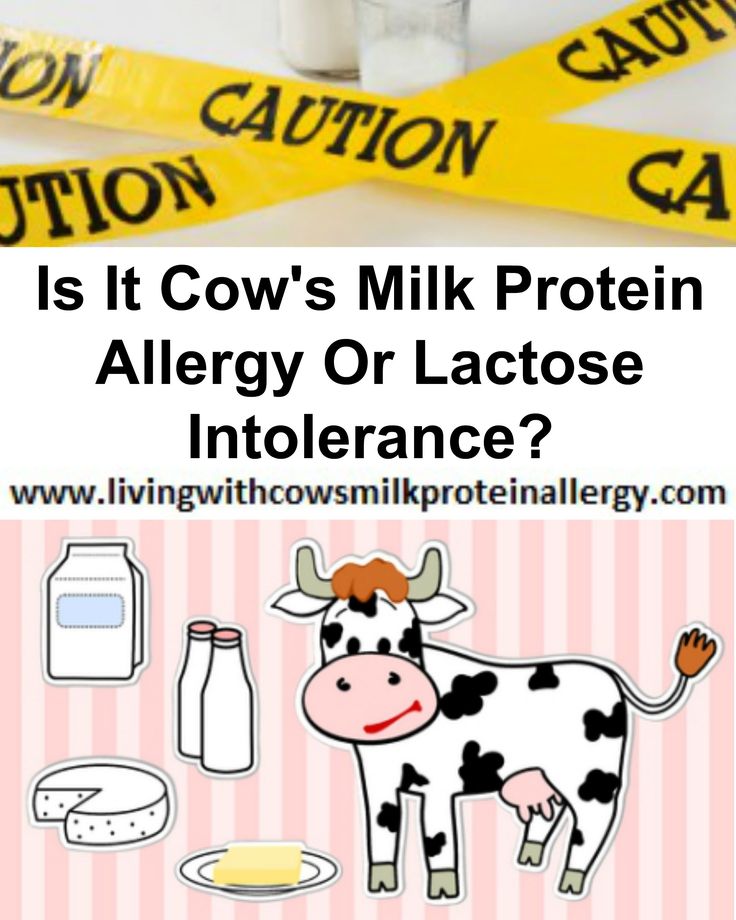
There are other foods that can cause allergic reactions when eaten, the Food Standards Agency (FSA) recognises 14 common allergens, which by Law must be declared prominently when they are an ingredient in any food.
It is possible that anyone can develop an allergy to anything, so it is very important to be aware of the symptoms of an allergic reaction.
If you are concerned that a certain food is causing a reaction to your baby, stop offering that food and seek medical advice from a health professional.
For more information on the 14 allergens please visit the FSA website.
The Food Standards Agency’s 14 allergensWhilst the list below is not exhaustive of all allergens (it is possible for anyone to be allergic to anything), this is the list of the 14 most common allergenic foods, that must be legally declared when they are used as an ingredient in food in the UK:
-
Celery
-
Cereals containing gluten – the protein found in wheat
-
Crustaceans – a type of seafood like prawns, crab and lobster
-
Eggs
-
Fish
-
Lupin – a flower that’s found in flour
-
Milk
-
Molluscs – shelled foods like mussels, whelks, snails
-
Mustard
-
Tree nuts
-
Peanuts
-
Sesame seeds
-
Soya
-
Sulphur dioxide – used as a preservative in dried fruits and some sausages
If your baby has IgE or immediate onset CMPA, there is no need to be concerned about them being allergic to soya.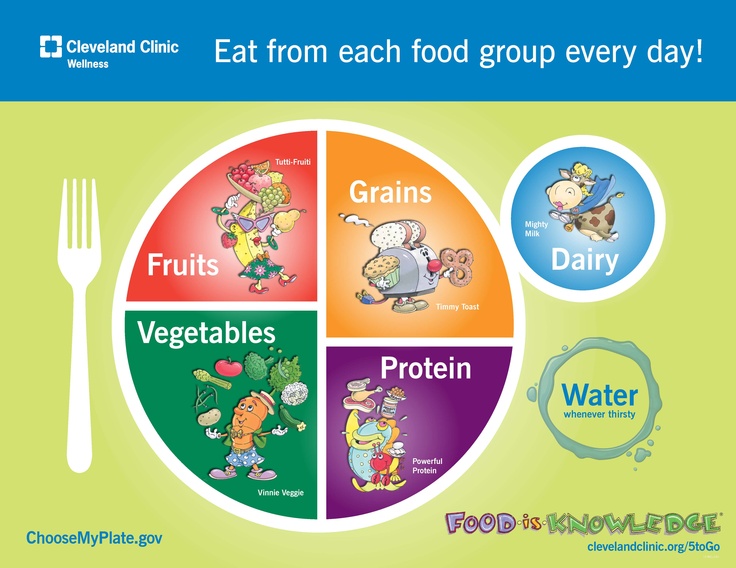
There is a link however between non-IgE or delayed onset CMPA where up to 50% of babies/children may also show a similar allergic reaction to the proteins found in soya [6]. The current advice would be to try introducing a small amount of soya once weaning is well established and use a stepwise soya ladder to increase quantities. Your dietitian will go through what this looks like with you.
I heard that soya was bad for babies and they should avoid it, is this true?It is recommended that babies under 6 months don’t have soya infant formula but this has nothing to do with allergies. Soya also contains phyto-oestrogens which are similar to female hormones. An old study in male marmoset monkeys found changes in male monkeys fertility when they were fed soya [7].
As a precaution, the NHS advises that babies should not have soya infant formula under 6 months of age but this can be given after 6 months when weaning has started and milk is no longer the sole source of nutrition.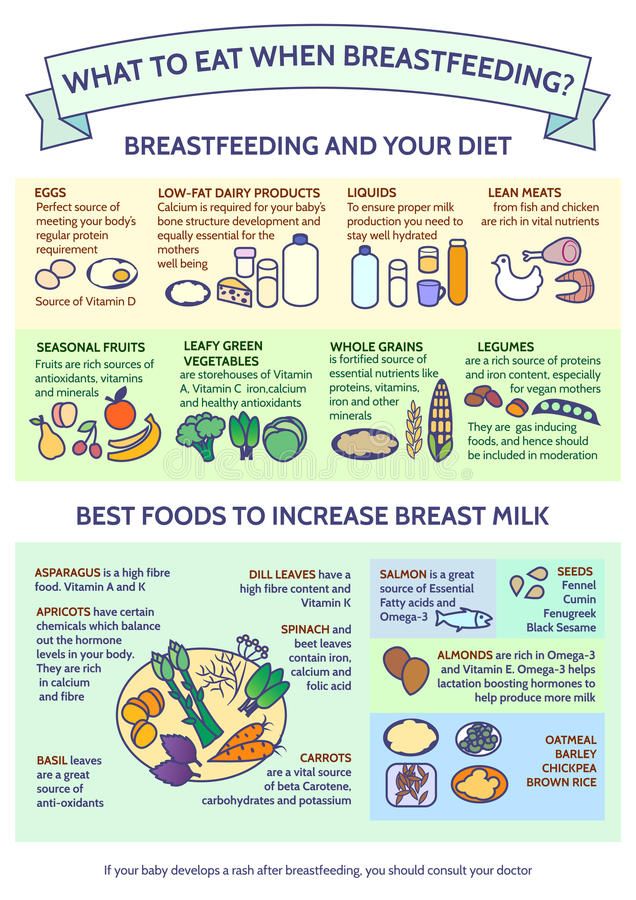
After reading this you might be worried that there’s not much left that your little one CAN eat. It can be so easy to focus on all of the foods that your little one needs to avoid that you forget about all of the wonderful foods that they can enjoy!
There are lots of foods that are naturally free from dairy. Fruits and vegetables, meats, fish and seafood, eggs, nuts and seeds, grains such as rice and couscous. The list really is endless. If you’re struggling to think of the foods that your little one can eat, have a chat with your dietitian who will be able to give you some more ideas.
How do I know if my baby has outgrown her milk allergy?If your baby has been symptom-free for 6 months and is older than 9 months of age they can undergo a stepwise challenge to see if they are still allergic. The Milk Ladder is a step by step approach that is carried out under the supervision of a dietitian if your baby has non-IgE delayed onset type of allergy.
For those who have an IgE or immediate onset milk allergy, the milk ladder is carried out in hospital under close medical supervision.
What is the milk ladder?The milk ladder is a six-step approach to re-introducing milk, initially in a baked form alongside other proteins as this is less allergenic and moving stepwise in increasing amounts, other proteins and less baking time as it progresses.
There are specific recipes to accompany the first 3 steps on the milk ladder and it’s important not to alter these recipes which have been created in a specific way to measure tolerance.
If your child doesn’t tolerate a certain step, they remain on the step before and include these foods in their diet until a date is arranged to try again.
Dairy free baby food recipes for weaning:Here are my top 10 dairy free baby food recipes for each stage of weaning:
Stage 1-
Carrot puree
-
Broccoli Puree
-
Trio of Root Veg
-
Courgette and pea mash
-
Apple and Beetroot puree
-
Carrot and spinach puree
-
Parsnip and Pear puree
-
Cauliflower, apple and sweet potato
-
Avocado smash with banana
-
Apple and apricot pudding
-
2 ingredient pancakes
-
Omelette fingers
-
Veggie Curry
-
Pork and paprika
-
Omega-3 rich quinoa balls
-
Pizza and Pasta sauce
-
Fish risotto with peas
-
Pork Casserole
-
Fruity chicken
-
Bolognese
My Baby’s First Birthday Cake recipe
-
Blueberry porridge
-
Moroccan Lamb with couscous
-
Jacket Potato with Bean Chilli
-
Chicken meatballs
-
Beef curry
-
Home made fish fingers
-
Lentil Dhal
-
Chicken coconut curry
-
Dairy free mini lasagnes
-
Baby’s 1st Birthday Cake (made with dairy free milk)
For younger babies there are 13 different variants and the one your baby needs will be determined by the dietitian, Essentially there are two main differences:
Extensively Hydrolysed FormulaThese are processed so that the protein within the cow’s milk is broken down into smaller parts so that they become hypoallergenic and are able to pass by the immune system without causing symptoms.
Examples include Althera, Nutramigen LGG 1&2, Pregestamil Lipil, Aptamil Pepti 1&2, Aptamil Pepti Junior, Infantrini Peptisorb and Simlac Alimentum.
Amino Acid FormulaThese are only prescribed in the most severe cases of food allergy. The proteins are completely broken down to amino acids and so are unrecognisable to your baby’s immune system.
Examples include Alfamino, PurAmino, Neocate LCP and Neocate Syneo.
Both extensively hydrolysed formula and amino acid formula will taste and smell differently to standard baby formula. For young babies, such as under 4 months, they tend to just get used to this and accept it. However, older babies who are used to the taste and smell of standard formula, are likely to struggle to accept the new formula.
Your dietitian can work with you to make this transition easier and increase the chances of your baby accepting the new milk.
If your baby is over 6 months of ageA soya based infant formula may be a suitable alternative to standard formula assuming your baby can tolerate soya.
It’s important not to give soya formula to babies under 6 months as the levels of oestrogens are too high for developing babies. You should also be aware that soya infant formula contains a type of sugar which isn’t good for your baby’s teeth.
How long should my baby stay on their special formula?In order to ensure your baby is getting all the nutrition they need, it is likely they will likely stay on their infant formula until around 2 years of age which is the current World Health Organisation Guideline, however if they eat a balanced and varied diet and are not fussy, your dietitian may suggest certain plant-based milk alternatives. It is important to follow their advice as not all plant milks are nutritionally equal.
If this is the case it’s likely that additional calcium and vitamin D in the form of a supplement will be needed.
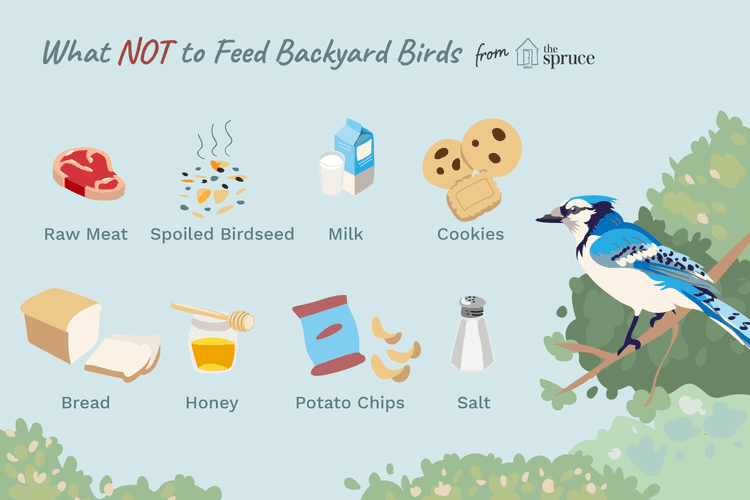
Could I not just give my CMPA plant milk to drink instead of formula?There are lots of plant-based milks available on the market such as almond milk, oat milk, hemp milk and pea milk. Whilst these do not contain any milk, they are a poor source of nutrition for your baby as they do not contain the right balance of nutrients, particularly calories, fat and protein as well as lots of other nutrients.
Whilst these do not contain any milk, they are a poor source of nutrition for your baby as they do not contain the right balance of nutrients, particularly calories, fat and protein as well as lots of other nutrients.
Calcium and iodine fortified unsweetened soya milk can be used in cooking, but should not replace breastmilk or formula or be given as a drink until at least 2 years of age. Your dietitian will advise if the other plant-based milks can be used in cooking with your individual baby.
Again, it’s not a one size fits all approach as the context of the rest of their diet has to be considered.
Rice milk is not suitable for children under 5 due to the naturally occurring high levels of inorganic arsenic.
How long does CMPA last?Research shows that most babies with CMPA will have outgrown their allergy by the age of three. However, it can last throughout childhood and even into adulthood in some rare cases.
It is possible to desensitise the body to milk using the milk ladder described above, so including milk containing foods at the level your baby reached on the milk ladder as part of their normal diet is important.
As eliminating milk from the diet is associated with nutritional risks, challenging your little one at regular intervals in encouraged.
Can probiotics help my baby with a milk allergy?Probiotics may help a baby with the symptoms of a cow’s milk protein allergy however the evidence that we have isn’t good enough to make this recommendation. We are still waiting on more research to see if these could help[8].
How do I access a dietitian?Your health visitor or GP can refer you to an NHS dietitian or you can find a private practice one here. Make sure your dietitian is a paediatric dietitian with experience in food allergies in order to support you fully.
How can I find out more about CMPA?There is information available on CMPA on the Allergy UK website
Are there any alerts I should sign up to?I would recommend signing up to the Food Standards Agency (FSA) allergy food alerts. You can receive email/text reminders whenever there is a food safety recall due to an allergen not being present on a food label and therefore a risk to anyone with a food allergy.
You can receive email/text reminders whenever there is a food safety recall due to an allergen not being present on a food label and therefore a risk to anyone with a food allergy.
You can follow me on Instagram and Facebook for daily tips and advice or you can join my Happy Healthy Weaning course where I will guide you every step of the way along your baby’s weaning journey.
Sarah Almond Bushell MPhil, BSc (Hons) RD MBDA – Registered Dietitian & Children’s Nutritionist
90,000 Silent diet for a child and adult: Food principles, permitted productsComplain
updated
Content:
When you need a silence diet
diets with acute intestinal infections
Diets for children at Rotavirus
Adult diet for any intestinal infection
Dairy-free diet for breastfeeding mothers
Dairy-free diet for a child up to 9 years0005
Dairy-free diet for 1-2 year olds
Dairy-free diet for 2-3 year olds
Prohibited foods
List of approved foods
Dairy-free diet is the elimination of dairy products for a certain period. It can last from three days - for example, after poisoning, or temporary restrictions will be lifelong in case of lactose intolerance. A well-designed diet will help to maintain a diet without health consequences.
It can last from three days - for example, after poisoning, or temporary restrictions will be lifelong in case of lactose intolerance. A well-designed diet will help to maintain a diet without health consequences.
Refusal of dairy products can be voluntary, for example, with vegetarianism, and forced - with problems with the absorption of milk.
Dairy-free diet means avoiding all dairy products
Indications:
- acute intestinal infections;
- intolerance to the milk protein casein during breastfeeding;
- lactose intolerance; nine0046
- irritable bowel syndrome during periods of exacerbation.
Despite the fact that there are few indications, a large number of people of different ages face them. Sometimes a diet is recommended to patients in the stage of exacerbation of an infectious disease.
Diet for acute intestinal infections
Intestinal infections are especially common in children under three years of age due to the immaturity of the gastrointestinal tract. A common cause of infection - rotavirus, requires mandatory exclusion of milk until complete recovery. nine0005
A common cause of infection - rotavirus, requires mandatory exclusion of milk until complete recovery. nine0005
Salmonellosis and food poisoning are more common in adults. Dairy products are excluded for three days to unload the digestive tract.
Principles of nutrition for intestinal infections:
- exclude dairy products;
- in the first days you can not have any vegetables and fruits;
- can be boiled low-fiber vegetables from the third day;
- in the early days, the basis of nutrition is rice and rice water;
- two weeks sparing diet without spices, raw vegetables and fruits. nine0046
Way of cooking - stewing, boiling, steaming.
It is very important to drink plenty of water when you are sick. In addition to pure water, you can drink chamomile tea, raisin decoction, rehydration solutions from a pharmacy. Fruit and vegetable juices are strictly prohibited!
Rotavirus diet for children
Diet plan for a small child with rotavirus infection:
- Day 1.
 Rice congee, boiled rice porridge without milk, sugar and salt. nine0046
Rice congee, boiled rice porridge without milk, sugar and salt. nine0046 - Day 2. Add dried white bread, pita bread to the diet.
- Day 3. Add boiled buckwheat porridge in water.
- Day 4. We introduce soups with lean meat and cereals into the diet.
- Day 5–6. You can eat drying, lean cookies, baked apples.
- Day 7. You can try fermented milk products - fermented baked milk, thermostatic yogurt without additives.
Gradually switch to the usual diet. Dairy products are introduced a week after recovery. nine0005
Breastfeeding does not need to be stopped; if the baby is formula fed, you can switch to lactose-free products and soy milk formulas for a while. If the child already has a common table and can do without the mixture, it is better not to give it until the stool normalizes.
In case of any intestinal infectious disease, consultation with a pediatrician is obligatory.
Adult diet for any intestinal infection
Diet for poisoning and intestinal infection for adults and children over 6 years old:
- Day 1.
 Only rice water.
Only rice water. - Day 2. Rice porridge, white bread crackers.
- Day 3–5. Dairy-free cereals, pasta, poultry meat, natural yoghurts.
- Day 6–7. Soups in vegetable broth, without cabbage and legumes, with lean meat, baked apples, bananas.
Gradually familiar products are also added. Milk and its derivatives are introduced after the normalization of the stool, but not earlier than three days after the onset of the disease. Such a diet, but less strict, can be followed for infectious diseases. nine0005
Dairy free diet for breastfeeding mothers
Allergy to the milk protein casein is a condition in newborns that presents with skin rashes, stool problems and bloating. Allergies must be confirmed by laboratory tests and a pediatrician. Most often in a child, it passes on its own by the age of three to five years.
While such a baby is breastfed, the mother is forced to follow a diet that excludes milk. This diet has certain features, because a woman especially needs a complete diet. nine0005
nine0005
Peculiarities of the diet of lactating women:
- the energy value of the diet is 2000–2200 calories;
- not less than 1 g of fat per 1 kg of weight;
- sufficient fluid intake - up to 2.5 liters per day;
- variety of products;
- enough fresh vegetables and fruits;
- Vitamin D supplement 6400 IU per day.
Restriction in dairy products is a serious dietary change, so it is important to ensure that a woman receives all the necessary macro and micronutrients. nine0005
Since the diet should be varied, consider the principles of compiling a menu for the week:
- exclusion of all dairy products, including yogurt, cottage cheese, kefir;
- portion of meat five times a week;
- serving of fish twice a week;
- at least three types of cereals;
- daily portion of fresh vegetables, at least five types of vegetables per week;
- at least one fruit daily, at least three types of fruit per week; nine0046
- Enough healthy fats – daily nuts, avocados, or olive/flaxseed oil.

Thanks to this diet, the absence of dairy products will not adversely affect the health of a woman.
Sample menu for the day:
- Oatmeal on the water with dried fruits and nuts.
- Banana.
- Soup with turkey meat and vegetables + tea with dryers or marshmallows.
- Fruit and berry jelly. nine0045 Steamed buckwheat with fish + green vegetable salad with olive oil.
- A glass of oat or soy milk.
The menu should be based on taste preferences and consist of allowed products.
Diet without milk for a child up to a year
A dairy-free diet is essential for babies with lactose intolerance or allergy to the milk protein casein. In both cases, dairy products, including sour-milk, should be excluded. These conditions may resolve on their own by 3 to 5 years of age. Lactose intolerance can persist for life. nine0005
If you are breastfeeding, don't stop! To correct lactose intolerance, the pediatrician will prescribe special drugs, and if the mother is allergic to casein, it is enough to follow a dairy-free diet.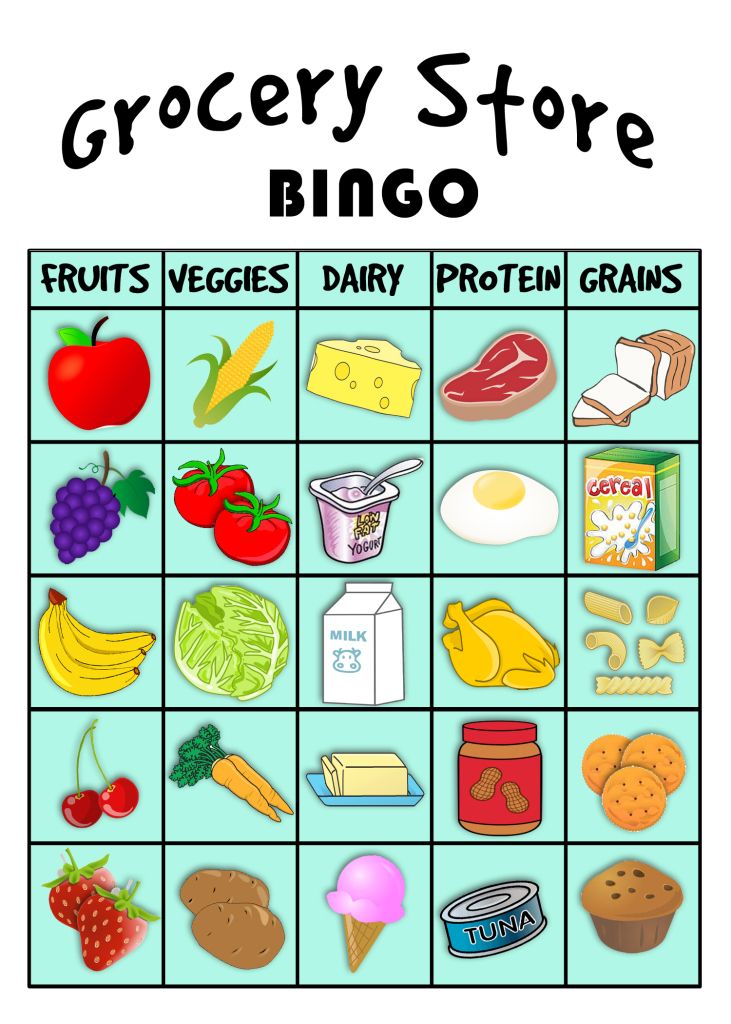
If you are allergic to protein in cow's milk, you need to choose the right formula for your child
A child under one year old only gets acquainted with the variety of food. The basis of his diet is mother's milk or a mixture. To feed children with an allergy to casein, special mixtures with protein hydrolyzate, mixtures with soy milk are used, in some cases mixtures with goat's milk are also suitable. For lactose intolerance, lactose-free mixtures are used. nine0005
Approximate scheme for introducing products:
- from 6 months: vegetable purees;
- from 7 months: dairy-free cereals;
- from 8 months: fruit purees;
- from 9 months: rabbit meat;
- from 10 months: turkey meat;
- from 11 months: vegetable soups with meat.
In children prone to allergies, complementary foods should be introduced very carefully - one food per week.
Dairy-free diet for children 1-2 years
Before the age of two, the child learns a variety of food and gradually prepares for the transition to a common table. Dishes become more complex, contain more components.
Dishes become more complex, contain more components.
When dieting without dairy products, it is important to monitor the amount of fat, calcium and take additional vitamin D.
Example of a daily diet:
- Porridge with water with a spoonful of olive or linseed oil.
- Formula or breastfeeding. nine0045 Soup with previously introduced vegetables and meat.
- Fruit, lean biscuits.
- Vegetable puree.
- Formula or breast milk at bedtime.
The rule of gradual introduction of complementary foods for a child with allergies is still observed: no more than one new product per week.
Dairy-free diet at 2-3 years of age
From the age of two, the child eats close to the common table, but the food should still be without spices, mushrooms, and a lot of salt. nine0005
Pediatricians recommend trying dairy products around three years of age, starting with cottage cheese or yogurt. If there is no reaction, then gradually increase the amount of the product. Whole milk can not be up to three years, and if intolerance does not pass - for life.
If there is no reaction, then gradually increase the amount of the product. Whole milk can not be up to three years, and if intolerance does not pass - for life.
Example of a daily diet:
- Porridge with vegetable oil and fruit.
- A handful of fresh berries.
- Formula or breast milk.
- Vegetable soup.
- Compote with lean biscuits or bagel. nine0046
- Steamed meat or fish puree.
Allowed foods are important to rotate during the week. It is necessary to continue taking vitamin D, calcium according to indications.
Prohibited products
To feel good on a diet, it is enough for a person to know the list of prohibited foods and take a multivitamin complex.
Not allowed:
- milk;
- butter and cream, sour cream; nine0045 fermented milk products: fermented baked milk, kefir, koumiss, ayran, yogurt, etc.;
- cottage cheese;
- baked goods containing milk: cakes, some biscuits, cakes, pies;
- milk chocolate and sweets.

Always check the ingredients of purchased products. In the presence of milk and its derivatives, these products are prohibited for you.
List of approved products
This list is very wide, you can make an excellent menu for every day from it - finding recipes without milk is not a problem. With any diet, it is better to think over meals in advance: it is easier to balance all the nutrients and vitamins. nine0005
Permitted products:
- cereals;
- pasta;
- meat and poultry;
- fish;
- vegetables;
- fruits;
- coconut, almond, soy, oat milk;
- nuts;
- mushrooms;
- seafood;
If there are contraindications to drinking milk, choose products from this list.
For many people, dairy products make up a large part of their diet, but this does not mean that the quality of life will decline without milk. Contraindications to the use of milk are just an excuse to reconsider and diversify your diet a little.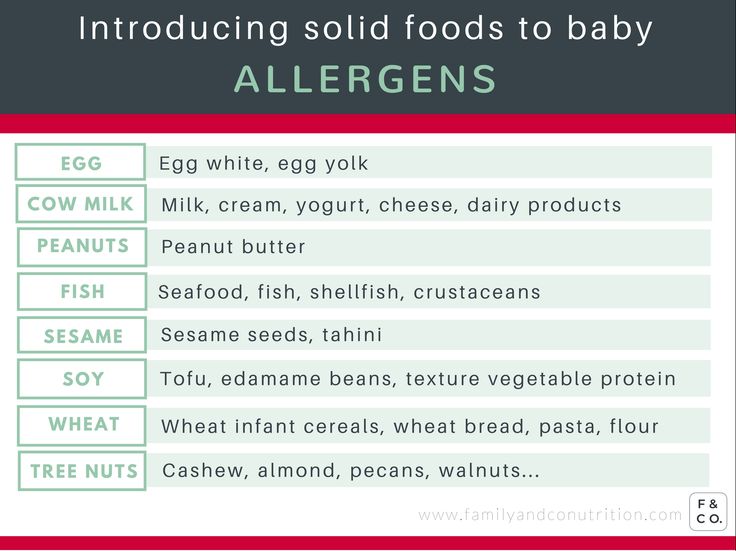 nine0005
nine0005
See also: diet for rotovirus
* The information provided cannot be used for self-diagnosis, treatment determination and does not replace a visit to a doctor!
HeadingNutrition for a nursing mother
The benefits and possible harm of breastfeeding bread for mother and child
How to eat after a cesarean section in the first days and when feeding a baby
You and your child grow through dreams. Encourage this in each other
Comments
Learn and participate
Baby.ru clubs are a treasure trove of useful information
New Year with the Krasny Oktyabr factory less noticeable scar after cesarean? TOP-25 Christmas gifts for children of all ages Assess the state of your child's immunity nine0005
Dairy-free menu for a child from 2 to 5 years old - 12 answers
Although, probably for any age)
At 2 years old, we got to a normal allergist.
Here I described in detail what we took and found the cause of our allergy - casein.
i.e. no dairy products of any kind.
As a result, now the child is 6 years old, there have been no rashes since 2.5 years. Free consumption of dairy products from the age of 5.5 (does not like it very much, but eats milk porridges, glazed curds, cheesecakes, cookies with cottage cheese, pastries with butter, pancakes and borscht with sour cream). nine0005
I must say right away that we told the child: you can't eat dairy products, the doctor forbade you! And they did not give anything that was impossible !!! Absolutely nothing!! Never!
1. Baking. There were basically 3 options
Dairy-free biscuits
Very tasty biscuits!
1 st. l. sunflower oil
1.5 tbsp. spoons of sugar (less possible, no sugar at all)
1 egg (no egg, no protein or yolk, if allergic)
a glass of flour
a little bit of baking powder (optional)
bake in a hot oven for 5 minutes!
I made different versions: with berries, apples, salty, cinnamon, raisins.
Dairy-free pies:
Pies were always berry (I froze a full freezer of berries in the summer) or fruit (less often)
They are all on vegetable oil with eggs (the child was not allergic to eggs)
For example:
- berries (nuts, fruits, cinnamon, raisins, dried apricots)
- 2 eggs
- 1 cup sugar
- 3/4 cup vegetable oil
- 1 tsp soda
- 2 cups flour
Sweets:
made like in our childhood sugar + water + lemon / berry (with a fun game) / jam and on fire.
photo from the Internet, I think that the essence is clear))
Porridges:
remidia was eaten up to 3 years, or even longer (all types of cereals, except semolina)
After 2.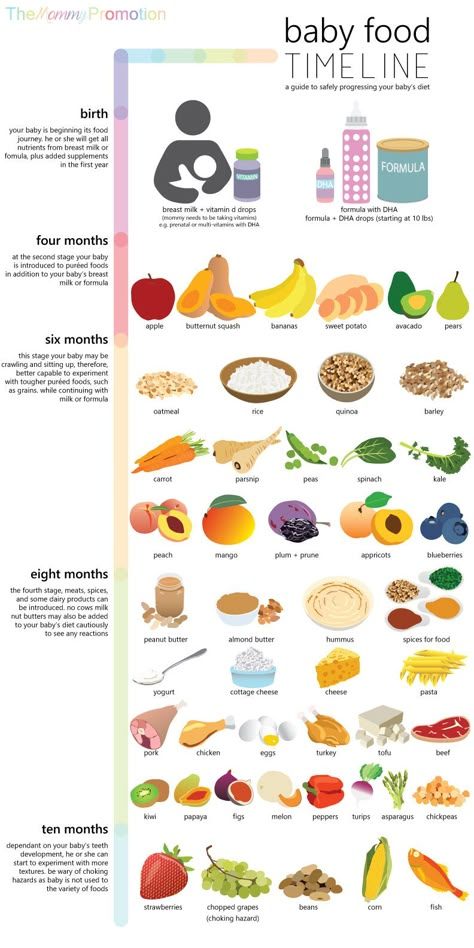 5 years ordinary cereals were boiled on water, including with the addition of dried fruits, berries and fruits (nuts were given very limited).
5 years ordinary cereals were boiled on water, including with the addition of dried fruits, berries and fruits (nuts were given very limited).
Vegetables:
Any in any form at any time of the day without restrictions!
Mostly there was broccoli, all types of cabbage (including Brussels sprouts, white cabbage, cauliflower), carrots, all types of beans (green, white, even grown their own), potatoes (soaked), beets, turnips, radishes, kohlrabi, cucumbers , tomatoes, peppers, all greens. nine0005
Meat:
The child was given only turkey and rabbit. We were not lazy and regularly went shopping at farmers' markets in the Moscow region (or even further)
We made the following dishes from meat:
Hedgehogs
lunch (minimum 4 hours), cook almost until ready
3. mix 1 and 2 in a bowl, I do not salt, but not essential
4. I throw the balls into boiling water + 2 leaves of lavrushka, with allergies, lavrushka is a thing! nine0343 5.