Do babies with pyloric stenosis vomit after every feeding
Pyloric Stenosis (for Parents) - Nemours KidsHealth
What Is Pyloric Stenosis?
Pyloric stenosis is a condition that can affect the gastrointestinal tract in babies. It can make a baby vomit forcefully and often, and can lead to other problems, such as dehydration. Pyloric stenosis needs medical care right away.
What Happens in Pyloric Stenosis?
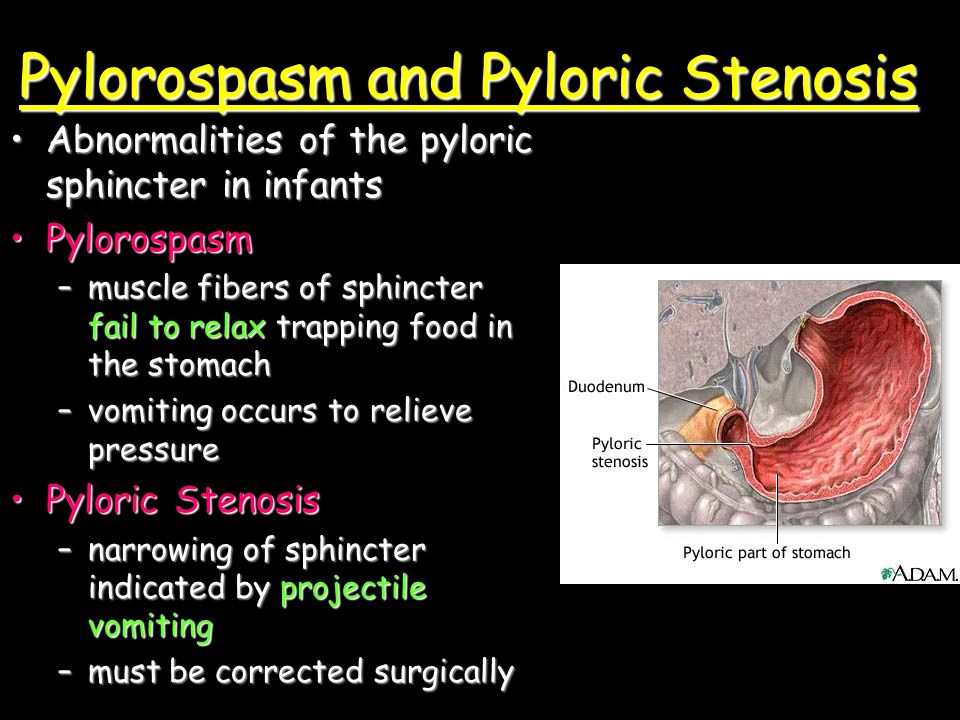
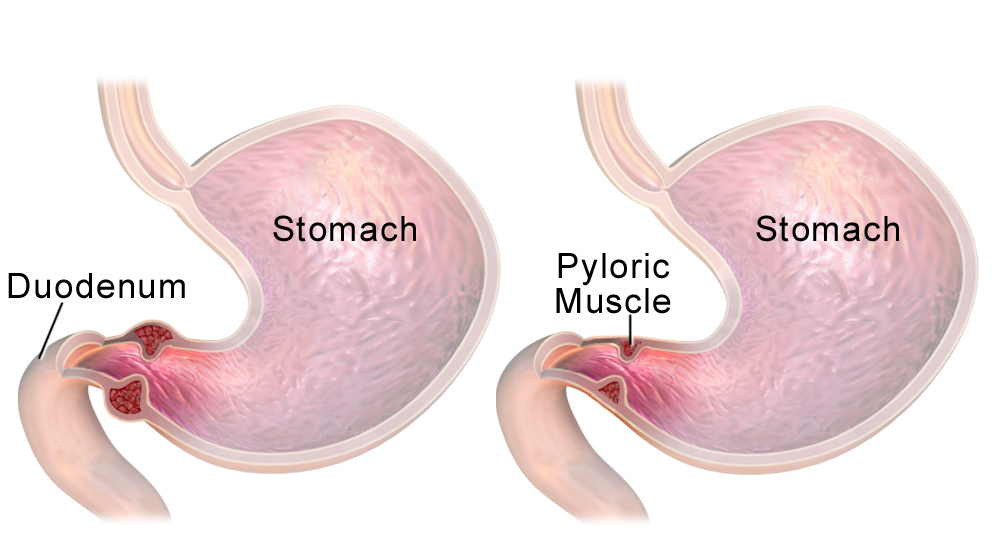
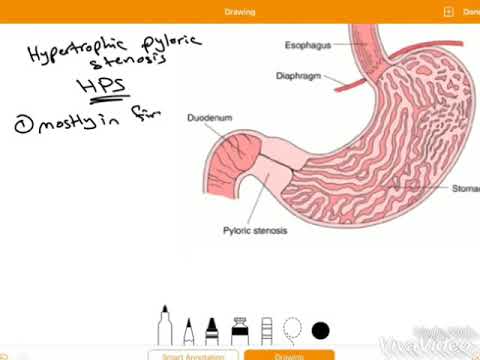
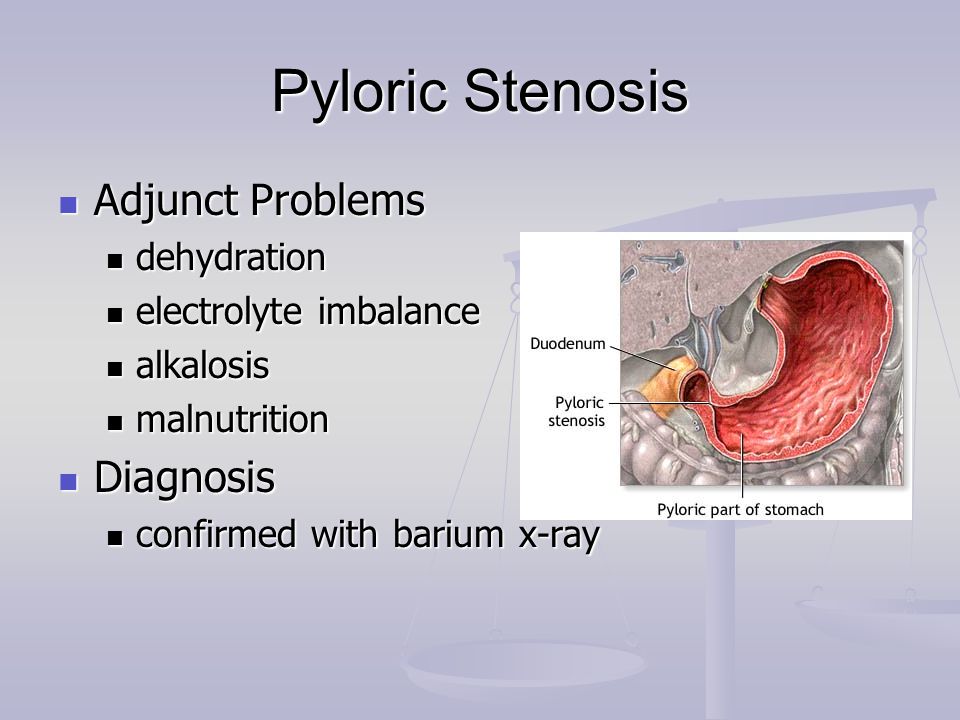
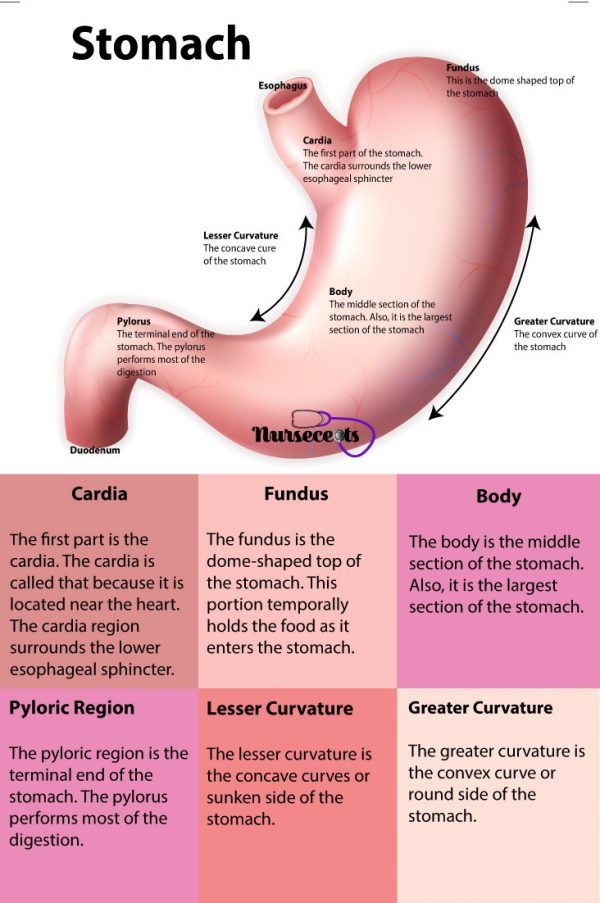
Food and other stomach contents pass through the pylorus, the lower part of the stomach, to enter the small intestine. Pyloric stenosis (pie-LOR-ik stih-NOE-sis) is a narrowing of the pylorus. When a baby has pyloric stenosis, this narrowing of the pyloric channel prevents food from emptying out of the stomach.
Pyloric stenosis (also called infantile hypertrophic pyloric stenosis) is a type of gastric outlet obstruction, which means a blockage from the stomach to the intestines.
Pyloric stenosis affects about 3 out of 1,000 babies in the United States. It's more likely to affect firstborn male infants and also runs in families — if a parent had pyloric stenosis, then a baby has up to a 20% risk of developing it. Most infants who have it develop symptoms 3 to 5 weeks after birth.
What Causes Pyloric Stenosis?
It's thought that babies who develop pyloric stenosis are not born with it, but have progressive thickening of the pylorus after birth. A baby will start to show symptoms when the pylorus is so thick that the stomach can't empty properly.
The cause of this thickening isn't clear. It might be a combination of several things. For example, use of erythromycin (an antibiotic) in babies in the first 2 weeks of life or antibiotics given to moms at the end of pregnancy or during breastfeeding can be associated with pyloric stenosis.
What Are the Signs & Symptoms of Pyloric Stenosis?
Symptoms of pyloric stenosis typically begin when a baby is around 3 weeks old. They include:
- Vomiting.
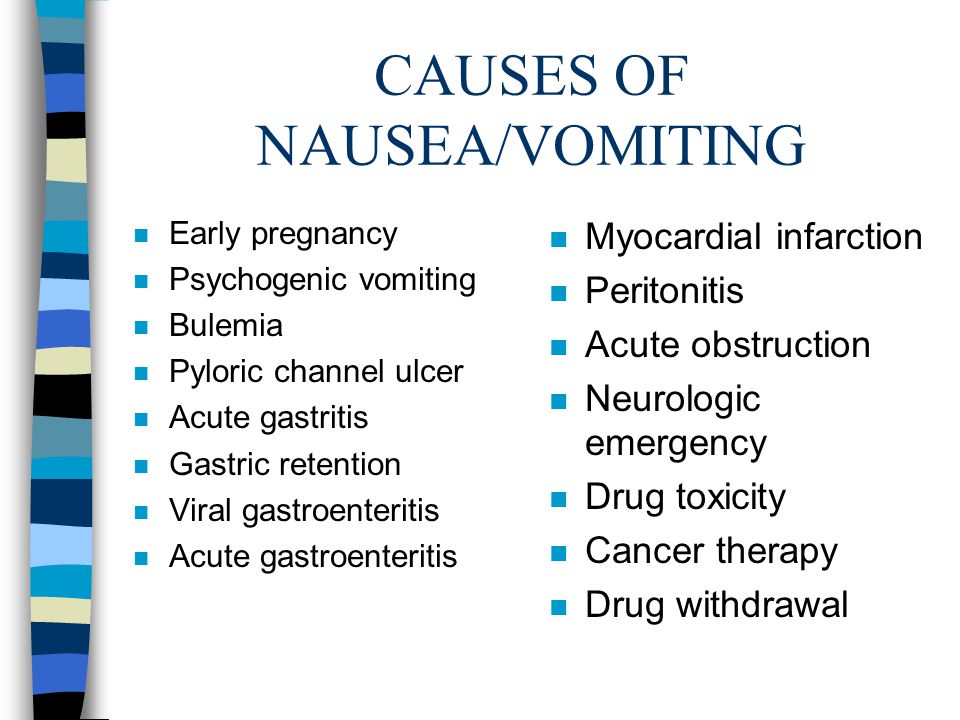
 The first symptom is usually vomiting. At first it may seem that the baby is just spitting up often, but then it tends to become projectile vomiting, in which the breast milk or formula is ejected forcefully from the mouth, in an arc, sometimes over a distance of several feet. Projectile vomiting usually takes place soon after the end of a feeding, although in some cases it can happen hours later.
The first symptom is usually vomiting. At first it may seem that the baby is just spitting up often, but then it tends to become projectile vomiting, in which the breast milk or formula is ejected forcefully from the mouth, in an arc, sometimes over a distance of several feet. Projectile vomiting usually takes place soon after the end of a feeding, although in some cases it can happen hours later.The vomited milk might smell curdled because it has mixed with stomach acid. The vomit will not contain bile, a greenish fluid from the liver that mixes with digested food after it leaves the stomach.
Despite vomiting, a baby with pyloric stenosis is usually hungry again soon after vomiting and will want to eat. It's important to know that even with the vomiting, the baby might not seem to be in great pain or at first look very ill.
- Changes in stools. Babies with pyloric stenosis usually have fewer, smaller stools (poops) because little or no food is reaching the intestines.
 Constipation or poop with mucus also can happen.
Constipation or poop with mucus also can happen. - Failure to gain weight or weight loss. Most babies with pyloric stenosis will fail to gain weight or will lose weight. As the condition gets worse, they might become dehydrated.
Dehydrated infants are less active than usual, and they may develop a sunken "soft spot" on their heads and sunken eyes, and their skin may look wrinkled. Because less pee is made, they can go more than 4 to 6 hours between wet diapers.
- Waves of peristalsis. After feeds, increased stomach contractions may make noticeable ripples, which move from left to right over the baby's belly as the stomach tries to empty itself against the thickened pylorus.
It's important to call your doctor if your baby has any of these symptoms.
Other conditions can cause similar problems. For instance:
- gastroesophageal reflux (GER) usually begins before 8 weeks of age. GER involves lots of spitting up (reflux) after feedings, which can look like vomiting.
 But most babies with GER don't have projectile vomiting, and while they might have trouble gaining weight, they usually have normal poops.
But most babies with GER don't have projectile vomiting, and while they might have trouble gaining weight, they usually have normal poops. - a milk protein allergy also can make a baby spit up or vomit, and have diarrhea. But these babies don't have projectile vomiting.
- gastroenteritis (inflammation in the digestive tract that can be caused by viral or bacterial infection) also can cause vomiting and dehydration. But babies with gastroenteritis usually also have diarrhea with loose, watery, or sometimes bloody stools. Diarrhea usually isn't seen with pyloric stenosis.
How Is Pyloric Stenosis Diagnosed?
The doctor will ask detailed questions about the baby's feeding and vomiting patterns, including what the vomit looks like. The doctor will do an exam, and note any weight loss or failure to maintain growth since birth.
The doctor will check for a lump in the abdomen. If the doctor feels this lump, which usually is firm and movable and feels like an olive, it's a strong indication that a baby has pyloric stenosis.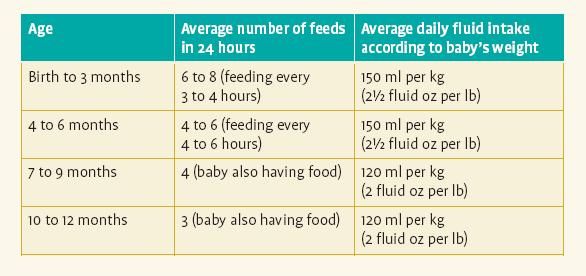
If pyloric stenosis seems likely, the doctor probably will order an abdominal ultrasound. The enlarged, thickened pylorus will show on ultrasound images. The doctor may ask that the baby not be fed for several hours before an ultrasound.
Sometimes doctors order a barium swallow instead of an ultrasound. Babies swallow a small amount of a chalky liquid (barium). Then, special X-rays are done that let the doctor check the pyloric area for any narrowing or blockage.
The doctor also might order blood tests to check levels of electrolytes (minerals that help keep fluids balanced and vital organs working properly). An electrolyte imbalance often happens due to the ongoing vomiting of stomach acid and dehydration, and needs to be corrected.
How Is Pyloric Stenosis Treated?
When an infant is diagnosed with pyloric stenosis, either by ultrasound or barium swallow, the baby will be admitted to the hospital and prepared for surgery. Any dehydration or electrolyte problems in the blood will be corrected with intravenous (IV) fluids, usually within 24 hours.
Doctors do a surgery called pyloromyotomy (pie-lor-oh-my-OT-uh-me) to relieve the blockage. Using a small incision (cut), the surgeon examines the pylorus and separates and spreads the thick, tight muscles. This relaxes and opens those muscles.
The surgery can also be done through laparoscopy. This technique uses a tiny scope placed through a small cut in the belly button, letting the doctor see the area of the pylorus. Using other small instruments placed in nearby incisions, the doctor can complete the surgery.
Most babies return to normal feedings fairly quickly, usually 3 to 4 hours after the surgery. Because of swelling at the surgery site, a baby may still vomit small amounts for a day or so. If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If you're breastfeeding, you might worry about continuing while your baby is hospitalized.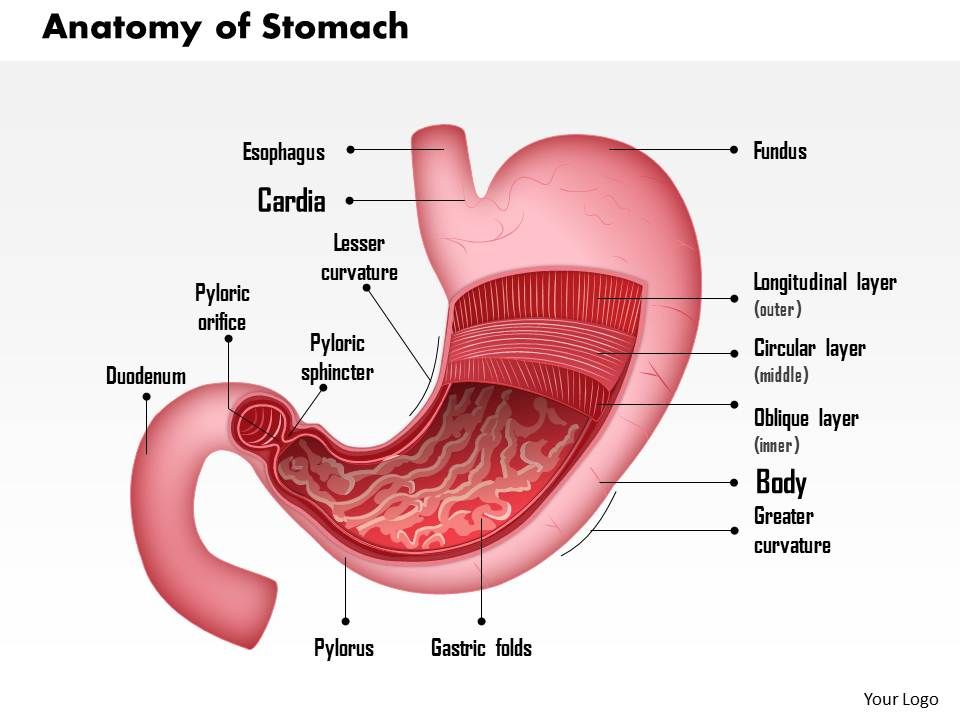 The hospital staff should be able to provide a breast pump and help you use it so that you can continue to express milk until your baby can feed regularly.
The hospital staff should be able to provide a breast pump and help you use it so that you can continue to express milk until your baby can feed regularly.
After a successful pyloromyotomy, your baby won't need to follow any special feeding schedules. Your doctor will probably want to examine your child at a follow-up appointment to make sure the surgical site is healing properly and that your baby is feeding well and maintaining or gaining weight.
Pyloric stenosis should not happen again after a pyloromyotomy. If your baby still has symptoms weeks after the surgery, there might be another medical problem, such as gastritis or GER, so let your doctor know right away.
When Should I Call the Doctor?
Pyloric stenosis is an urgent condition that needs immediate treatment. Call your doctor if your baby:
- has lasting or projectile vomiting after feeding
- is losing weight or not gaining weight as expected
- is less active than usual or is very sleepy
- has few or no stools (poops) over a period of 1 or 2 days
- show signs of dehydration, such as more than 4 to 6 hours between wet diapers, a sunken "soft spot" on the head, or sunken eyes
Pyloric Stenosis (HPS): Symptoms, Treatment & Tests
Overview
What is pyloric stenosis?
Pyloric stenosis is a thickening or narrowing of the pylorus, a muscle in the stomach. This problem happens to newborns. The full name of the condition is hypertrophic pyloric stenosis (HPS). Hypertrophy means thickening. Pyloric stenosis causes projectile vomiting and can lead to dehydration in babies.
This problem happens to newborns. The full name of the condition is hypertrophic pyloric stenosis (HPS). Hypertrophy means thickening. Pyloric stenosis causes projectile vomiting and can lead to dehydration in babies.
What happens in pyloric stenosis?
The pylorus is a muscular sphincter (muscle that opens and closes). It’s located at the end of the stomach, where the stomach meets the small intestine.
The pylorus contracts (closes) when food and liquid need to get digested in the stomach. It then relaxes (opens) to let food and liquid pass into the small intestine.
When the pyloric muscle is too thick, it narrows the passageway. Liquid and food can’t move from the stomach to the small intestine. Babies with pyloric stenosis often forcefully vomit since formula or breast milk can’t leave the stomach. Many babies have difficulty gaining weight because they have many episodes of vomiting.
Who is at risk for pyloric stenosis?
Risk factors for pyloric stenosis include:
- Sex of the baby: Full-term, first-born male babies are at higher risk.
 It’s less likely in baby girls.
It’s less likely in baby girls. - Race: It happens more to white infants, especially of European descent.
- Family history of pyloric stenosis: About 15% of infants with pyloric stenosis have a family history of it. The parent who had the condition before also matters. An infant’s risk is three times higher if the mother had pyloric stenosis, compared to the father.
- Smoking: Babies whose mothers smoked during pregnancy are at higher risk.
- Antibiotics: Some babies who needed antibiotics shortly after birth may be at higher risk. Babies whose mothers took certain antibiotics late in pregnancy may also have a higher risk.
- Approach to feeding: Some studies of babies drinking formula show an increased risk for pyloric stenosis. But it remains unclear if the risk comes from the bottle or the formula. If it comes from the bottle, it may also apply to bottles with breast milk.

When does pyloric stenosis occur?
Babies usually aren’t born with pyloric stenosis. The thickening of the pylorus starts to happen in the weeks after birth.
Pyloric stenosis symptoms usually start when the baby is 2 to 8 weeks old. But it can take up to five months for the symptoms to become apparent. If you notice symptoms, talk to your healthcare provider. It’s best to treat HPS before your baby becomes dehydrated and undernourished.
Can older children get pyloric stenosis?
In rare cases, older children can get a pyloric obstruction — something blocking the passage through the pylorus. Usually, a peptic ulcer is the cause in older children. Or perhaps a child has a rare disorder such as eosinophilic gastroenteritis, which inflames the stomach.
How common is pyloric stenosis?
Pyloric stenosis affects 3 out of every 1,000 babies born. It’s the most frequent condition requiring surgery in infants.
Symptoms and Causes
What are the symptoms of pyloric stenosis?
Symptoms start when babies are around 2 to 8 weeks old. Infants with pyloric stenosis may eat well but have these symptoms:
Infants with pyloric stenosis may eat well but have these symptoms:
- Frequent projectile vomiting (forceful vomiting), usually within a half hour to an hour after eating.
- Abdominal (belly) pain.
- Dehydration.
- Hunger after feedings.
- Irritability.
- Small stools.
- Wave-like stomach motion right after eating, just before vomiting starts. Occasionally a mass like a sausage can be felt in the stomach.
- Weight loss.
Most babies appear otherwise healthy. Parents may not notice something is wrong until babies get very dehydrated or undernourished. Babies may also start to get jaundice, when the skin and whites of the eyes become yellow.
Is spit-up a sign of pyloric stenosis?
Many babies spit up a little after they eat. These dribbles are common and usually nothing to worry about. Forceful or painful projectile vomiting is a sign of a more serious issue. Talk to your healthcare provider if your child vomits after eating.
Diagnosis and Tests
How is pyloric stenosis diagnosed?
Your healthcare provider will ask you about your child’s eating habits. Then your child will get examined. Sometimes, providers can feel an olive-sized lump in your child’s belly. That’s the thickened pyloric muscle.
Your provider may recommend a blood test as well. This test can tell if your child is dehydrated or has an electrolyte imbalance from vomiting. Electrolytes are minerals that keep the body working the way it should.
What tests might my child need to diagnose pyloric stenosis?
If the provider doesn’t feel the lump or wants to confirm the diagnosis, your child may need an abdominal ultrasound. During this painless procedure:
- Your provider places a probe (tool) gently against the belly.
- The probe uses sound waves to create images.
- Your provider can often see the thickened pyloric muscle in the images.
Sometimes, even a physical exam and ultrasound don’t show any problems. If this happens, your provider may recommend an upper gastrointestinal (GI) series:
If this happens, your provider may recommend an upper gastrointestinal (GI) series:
- Your child drinks a special liquid.
- The provider can see the liquid on an X-ray as it travels through the stomach toward the small intestine.
- Your provider can figure out if the liquid moves from the stomach through the pylorus. If it doesn’t, that indicates pyloric stenosis.
In some cases, an upper gastrointestinal series must be done if the physical exam and abdominal ultrasound do not reveal any abnormalities. This test requires that your child drink a special liquid. This liquid can be seen on an X-ray as it travels through the stomach and small intestine. The pediatric radiologist will be viewing the X-ray while your child drinks the liquid to determine whether or not the liquid is able to move out of the stomach through the pylorus.
Management and Treatment
What is pyloric stenosis treatment?
Surgery called pyloromyotomy treats pyloric stenosis. After diagnosing pyloric stenosis, your surgeon will discuss the surgery with you. It’s a safe surgery.
After diagnosing pyloric stenosis, your surgeon will discuss the surgery with you. It’s a safe surgery.
What happens before pyloric stenosis surgery?
Infants with pyloric stenosis often have dehydration because they vomit so much. Your provider will make sure your baby is properly hydrated before performing surgery. Your baby will probably need fluids through an IV which will be given at the hospital. A blood test to test hydration may be taken during this time to make sure it’s improving.
Your child won’t be able to have milk or formula starting six hours before surgery. Keeping them off these fluids reduces the risk of vomiting and aspiration (breathing in vomit) while under anesthesia.
What happens during pyloric stenosis surgery?
During pyloric stenosis surgery, the team will:
- Give your child general anesthesia. Your child will be asleep during the surgery and not feel any pain.
- Make a small incision (cut) on the left side of the abdomen, higher than the belly button.
- Perform a pyloromyotomy, making an incision in the thickened pylorus. This procedure allows food and liquid to travel from the stomach to the intestines.
How long is pyloric stenosis surgery?
The procedure usually takes less than an hour.
Can my child eat after pyloric stenosis surgery?
Your child will likely need to stay in the hospital for one to three days after surgery. Here’s what you can expect:
- Your child will start eating formula or breast milk a few hours after surgery. They’ll eat small amounts at first. Your surgeon will discuss your child’s feeding plan with you.
- If you use formula, the team will slowly increase the volume and concentration of the formula as your child can tolerate it.
- If you breastfeed, your child will have breast milk from a bottle for the first few feedings. It’s important to accurately measure the amount.
What if my child still vomits after surgery?
Babies can still vomit after pyloric stenosis surgery. It doesn’t mean they have the condition again. Vomiting may be because of:
It doesn’t mean they have the condition again. Vomiting may be because of:
- Anesthesia from the surgery.
- Lack of adequate burping after feedings.
- Too much food, too quickly.
If your child continues to vomit a lot, they may need more tests. Your care team will continue to work to correct any vomiting problems.
Prevention
Can I prevent pyloric stenosis in my baby?
There’s no way to prevent pyloric stenosis. If you know pyloric stenosis runs in your family, make sure to tell your healthcare provider. The provider can be on the lookout for any signs or symptoms of the condition.
Knowing the signs and symptoms of pyloric stenosis means you can get help as soon as possible. Getting treatment early helps prevent problems such as malnourishment and dehydration.
Outlook / Prognosis
What is the outlook for babies with pyloric stenosis surgery?
The outlook for babies with HPS is very good. Most children do not have long-term problems after successful pyloric stenosis surgery. They eat well, grow and thrive.
They eat well, grow and thrive.
Will my baby need a second pyloric stenosis surgery?
In rare cases, the pylorus is still too narrow after surgery. Surgeons may perform a second operation to cut it more.
Living With
How do I care for my child after pyloric stenosis surgery?
When you go home from the hospital:
- Your child will be eating normally, so you can feed them without a problem.
- Use medication such as acetaminophen (Tylenol®) if your child experiences any pain.
- Give your child a sponge bath the day after surgery. At three days post-surgery, you can bathe them in the tub.
- A small tape covers the incision, called a Steri-Strip™. Don’t pull it off yourself — it will fall off on its own. If it doesn’t, your provider will remove it at the follow-up appointment.
What happens at the follow-up appointment after pyloric stenosis surgery?
Bring your baby back to the provider around seven to 10 days after surgery.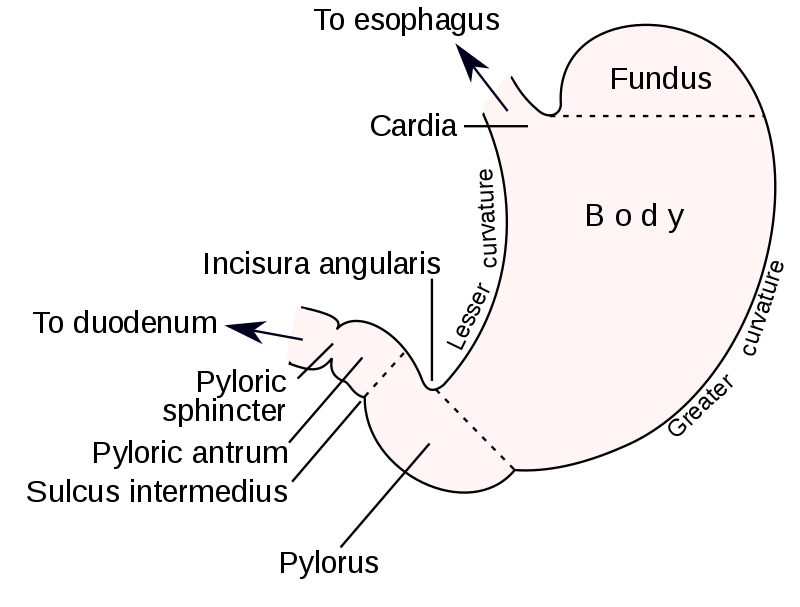 The provider will examine the surgical area and see how your child is recovering.
The provider will examine the surgical area and see how your child is recovering.
Are there activity restrictions after pyloric stenosis surgery?
Your child can go back to all regular activities. They can continue to have tummy time as well.
When should I call the healthcare provider?
Some normal swelling around the incision site is normal. But call your provider if your child has:
- Bleeding.
- Distended (swollen) or enlarged stomach.
- Excessive swelling around the surgical area.
- Fever.
- Fewer wet diapers than usual.
- Frequent vomiting.
- Vomiting that appears dark green or contains blood.
- Increased pain.
- Redness or drainage (leaking) from the incision.
A note from Cleveland Clinic
Contact your healthcare provider if your baby has frequent projectile vomiting. Your baby may have a thickened muscle at the end of the stomach. This condition, pyloric stenosis, makes it hard for food and liquid to pass through. Babies may then vomit and become dehydrated or malnourished. Surgery for pyloric stenosis usually provides relief. Called pyloromyotomy, the treatment opens the muscle to restore the food’s path. Babies who receive this surgery have good outcomes, with few complications.
Babies may then vomit and become dehydrated or malnourished. Surgery for pyloric stenosis usually provides relief. Called pyloromyotomy, the treatment opens the muscle to restore the food’s path. Babies who receive this surgery have good outcomes, with few complications.
ᐈ Pyloric stenosis ~【Symptoms and treatment in Kyiv】
The feeling of excessive satiety after each meal does not always indicate quality nutrition. And even more so when regular vomiting occurs after eating. Such symptoms may occur with the development of a specific disease of the gastrointestinal tract.
Pyloric stenosis is a narrowing of the gastric outlet between the pyloric part of the stomach (pylorus) and the initial part of the duodenum. A rather rare disease, most often affecting infants, although it can also occur in adults.
The pylorus is the lower segment of the stomach that connects it to the duodenum. Pathological changes form a thickened muscle layer in this critical area, which makes it impossible for food to pass.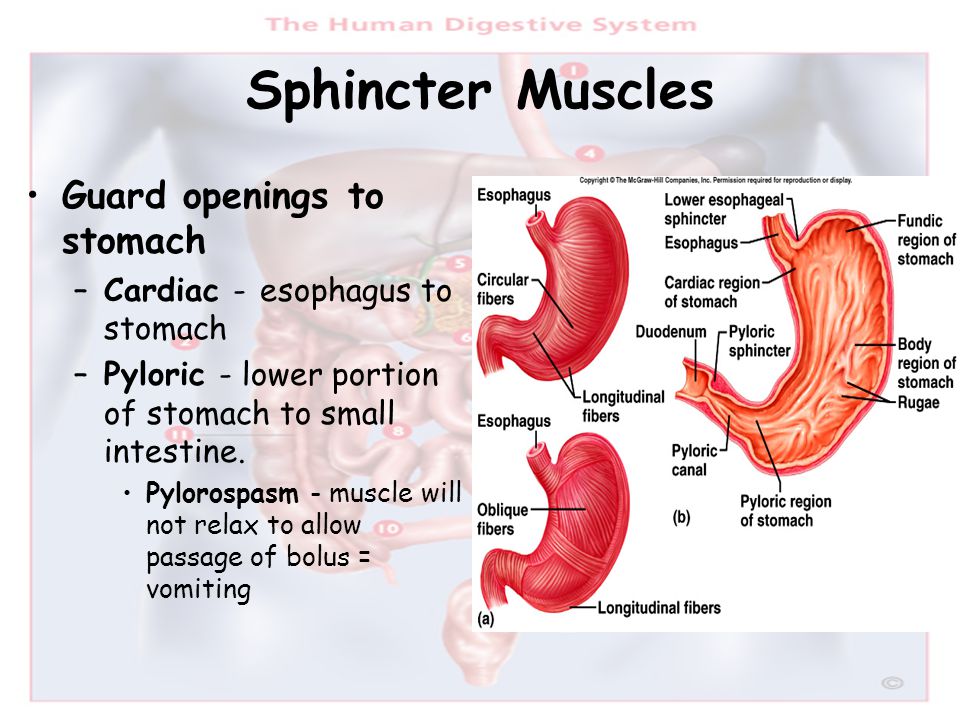
With thickening and pyloric stenosis, life-threatening complications such as dehydration and increased acidity of the blood with metabolic disorders appear within a short period. Immediate medical attention from a gastroenterologist and surgeon is required.
The most informative research method is esophagogastroduodenoscopy (EGDS) under anesthesia. This type of endoscopic examination is performed for adult patients in the hospital of the MEDICOM clinic. An ultrasound examination of the abdominal organs can also be performed on an outpatient basis to detect the disease in both adults and newborns.
Vidkriti Zgornuti
Classification of pyloric stenosis
The disease is divided into two types:
- congenital form of pyloric stenosis - associated with underdevelopment of the pylorus in newborns for various reasons, the development of the disease is influenced by hereditary factors and pregnancy, which proceeded with complications;
- Acquired pyloric stenosis - diagnosed in adults or adolescents.
In adult pyloric stenosis, the pathology may be primary or secondary.
Primary stenosis develops without involvement of other comorbidities and is usually asymptomatic. Its basis is hypertrophy of the pyloric muscles.
Secondary stenosis is caused by pyloric fibrosis, which is diagnosed as a result of:
- stomach or duodenal ulcer;
- benign or malignant neoplastic tumors;
- Lesniewski-Crohn disease leading to inflammation and adhesions in the pyloric region;
- sustained contraction of the pylorus caused by excessive activity of the vagus nerve, which is responsible for the functioning of the parasympathetic system, slowing down the motility of the gastrointestinal tract.
Vidkriti Zgornuti
Etiology
The causes of pyloric stenosis in infants remain unclear.
This is a birth defect that occurs more frequently in boys and children with a family history of stenosis. The disease can also be diagnosed in infants who took antibiotics during the first weeks of life or after the mother received antibiotic therapy in the last weeks of pregnancy.
The disease can also be diagnosed in infants who took antibiotics during the first weeks of life or after the mother received antibiotic therapy in the last weeks of pregnancy.
The cause of pyloric stenosis in children is hypertrophy of the muscle membrane, which causes its excessive contraction and prevents food from entering the duodenum.
There are certain risk factors, which include:
- Genetics.
Approximately 15% of infants with pyloric stenosis have a family history of the disease. - Race.
The disease most affects the population of northern European origin, less common in African Americans and Asians. - Smoking.
A bad habit during pregnancy almost doubles the chance of having a baby with pyloric stenosis.
Vidkriti Zgornuti
Pathogenesis
The pylorus is a muscle at the transition from the stomach to the duodenum. Its job, on the one hand, is to allow chyme to enter the intestines, and on the other hand, to prevent digested food from entering the stomach. Under the influence of adverse factors or genetic predisposition, the process of innervation in this area is disrupted, which causes signs of pyloric stenosis.
Its job, on the one hand, is to allow chyme to enter the intestines, and on the other hand, to prevent digested food from entering the stomach. Under the influence of adverse factors or genetic predisposition, the process of innervation in this area is disrupted, which causes signs of pyloric stenosis.
In case of stenosis, convulsions occur again and again in the annular muscle of the stomach. With impaired innervation, the blood supply to the site also suffers, which provokes dystrophy of muscle fibers. As a result, only a small part of the food enters the intestines. Most of the contents of the stomach with pyloric stenosis reflexively leave with vomiting. The longer the spasms of the pyloric muscle, the thicker it is. The symptoms of pyloric stenosis worsen as it progresses.
Vidkriti Zgornuti
Clinical manifestations of pyloric stenosis
Symptoms of pyloric stenosis in infants usually appear 3-6 weeks after birth, very rarely after 3 months of age.
When a child falls ill, the following is recorded:
- severe vomiting - at first small, with time it intensifies and spouts, occurs approximately 30 minutes after eating, sometimes it may contain blood due to irritation of the stomach;
- dehydration - diapers are lighter and less wet than usual, baby cries without tears;
- constant hunger and concomitant weight loss - due to the loss of food eaten, the child very often requires food, but this does not manifest itself in weight gain: he loses weight, growth retardation occurs;
- weak skin tone and turgor, reduced elasticity;
- constipation.
Abdominal cramps are caused by overexertion of the muscles that try to "push" food into the intestines, despite the fact that it is narrowed.
Vidkriti Zgornuti
Symptoms of pyloric stenosis in adults:
- bloating;
- nausea;
- weight loss to the point of exhaustion;
- early satiety after eating;
- vomiting of partially digested food (no bile) shortly after eating;
- frequent pain in the upper abdomen that subsides after vomiting;
- changes in biochemical parameters and the content of electrolytes (for example, potassium or sodium ions) in the blood, metabolic alkalosis (increased blood pH).
Vidkriti Zgornuti
Features of the course of the disease during pregnancy
During pregnancy, pyloric stenosis is rare. Most often it is formed against the background of other transferred diseases of the gastrointestinal tract. The clinical picture requires immediate diagnosis - gastroscopy or ultrasound.
The resulting pathology threatens with serious complications, so it is urgent to start treatment. With strong signs of pyloric stenosis, surgery is recommended. But this method of treatment is best used as a last resort during pregnancy. You should first treat the provoking disease and prescribe drugs that relax the muscles of the stomach.
Vidkriti Zgornuti
Peculiarities of pyloric stenosis in children
Congenital pyloric stenosis in a child is a disease that often leads to complete obstruction of the gastrointestinal tract. The frequency of the disease is estimated at 1:300-1:900 cases in newborns.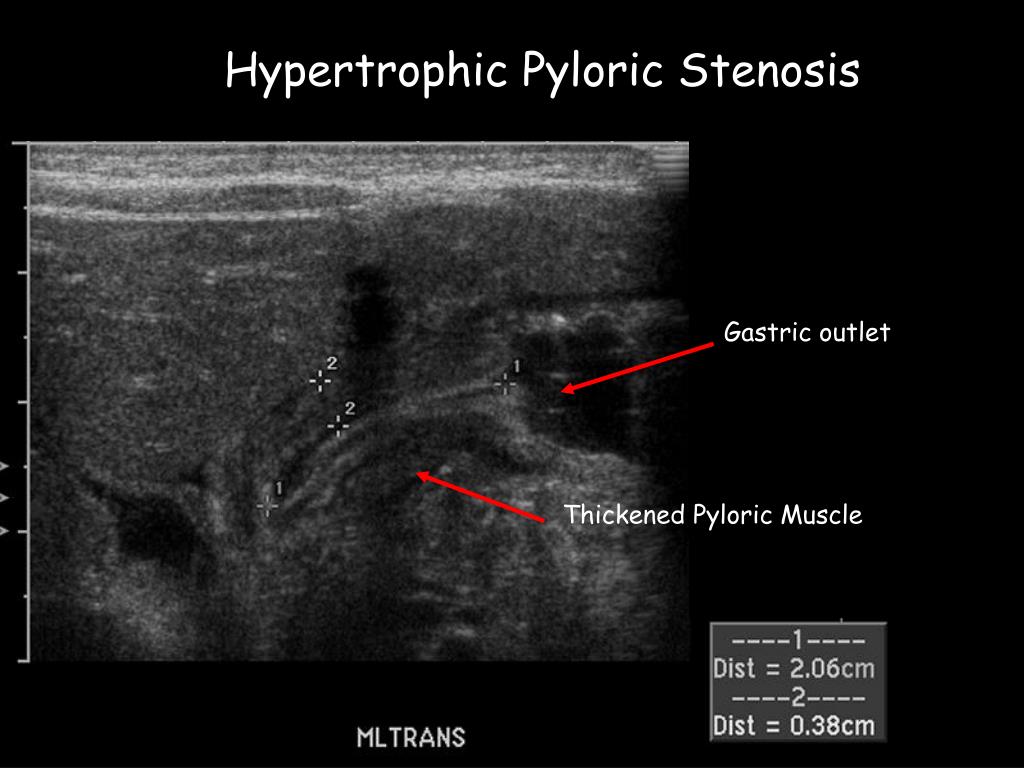 The characteristic symptoms of pyloric stenosis include vomiting that occurs during or immediately after eating. Bile is never detected in the returned contents. Palpation through the abdominal wall can sometimes reveal a tumor in the pyloric projection - an olive symptom.
The characteristic symptoms of pyloric stenosis include vomiting that occurs during or immediately after eating. Bile is never detected in the returned contents. Palpation through the abdominal wall can sometimes reveal a tumor in the pyloric projection - an olive symptom.
An important point in pediatrics is the difference between pyloric stenosis and pylorospasm. With pylorospasm, regurgitation of food by an infant is observed, which is due to disruption of the central nervous system. The cause may be high intracranial pressure, increased excitability and other factors. But with this pathology, the child still gains weight, and the amount of food during regurgitation is less than the amount of food consumed. A pediatric gastroenterologist must distinguish between these two conditions.
Vidkriti Zgornuti
Complications
The consequences of pyloric stenosis can be fatal, especially in infancy.
Typical complications include:
- frequent vomiting can cause dehydration and disruption of the mineral balance of electrolytes that help regulate many vital functions;
- yellowing of the skin and eyes - occurs in rare cases due to a substance secreted by the liver (bilirubin) that accumulates in the body;
- stomach irritation - repeated vomiting can irritate the baby's stomach and lead to easy bleeding;
- inability to grow and develop.

Vidkriti Zgornuti
Chronic lack of vitamins, minerals and electrolytes has an even more pronounced effect. This deficiency leads to metabolic imbalance, metabolic alkalosis. The pH level of the blood increases and the blood becomes more and more alkaline. As a result of alkalosis, cells absorb more potassium from the blood, and the concentration of this mineral in the blood falls. Without therapy, metabolic alkalosis is fatal.
The consequences of pyloric stenosis include anemia, decreased oxygen levels in the blood, and thickening of the blood.
Vidkriti Zgornuti
Diagnosis of pyloric stenosis
The clinical symptoms of pyloric stenosis in children are so characteristic that a diagnosis can be made based on the history of the disease. In addition, when examining a child, abdominal cramps are visible, and in the upper part you can feel an olive-shaped tumor - this is an overgrown pylorus. For accurate diagnosis of pyloric stenosis, an ultrasound examination of the abdominal cavity is performed. To assess the degree of dehydration, a blood test is performed - an assessment of biochemical parameters and electrolytes.
For accurate diagnosis of pyloric stenosis, an ultrasound examination of the abdominal cavity is performed. To assess the degree of dehydration, a blood test is performed - an assessment of biochemical parameters and electrolytes.
In adults, the diagnosis of pyloric stenosis is also based on interview, physical examination, ultrasound, and blood tests.
In addition, instrumental methods are used:
- X-ray of the abdominal cavity;
- upper gastrointestinal contrast test - the patient swallows a suspension of barite (contrast agent), which can visualize gastric distention and delayed emptying;
- computed tomography, thanks to which you can see the thickening of the pyloric wall and exclude the secondary nature of pyloric stenosis;
- videogastroscopy - thanks to the camera of the endoscope, you can examine the stomach from the inside and take samples of its mucous membrane to rule out gastric cancer.
Vidkriti Zgornuti
Treatment of pyloric stenosis
Pyloric stenosis needs treatment.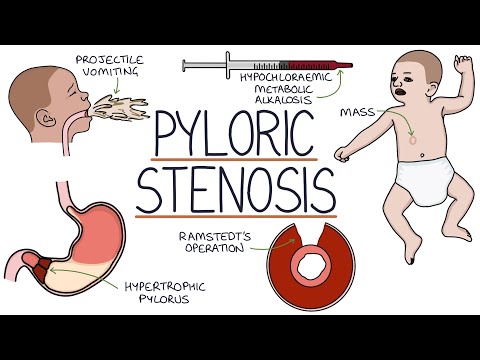 By itself, the condition will not improve. You will most likely need an operation called a pyloromyotomy.
By itself, the condition will not improve. You will most likely need an operation called a pyloromyotomy.
If surgery is not possible for health reasons, pyloric stenosis should be treated conservatively. This therapy concept aims to stimulate the pyloric muscle as little as possible. In addition, patients receive small meals, up to 12 times a day. In this case, it is necessary to sleep with a raised upper body.
Drug treatment of pyloric stenosis is treated with antispasmodic drugs. The biggest disadvantage of conservative treatment: sometimes it lasts for several weeks, which increases the risk of malnutrition, which must be compensated. Thus, pyloromyotomy has proven to be the best treatment for pyloric stenosis.
If the patient is dehydrated due to frequent and severe vomiting, they must be taken to the hospital and hydrated before surgery.
Vidkriti Zgornuti
Operations for pyloric stenosis
Laparoscopy is the main method of treatment in childhood, which is a dissection of the pyloric muscles.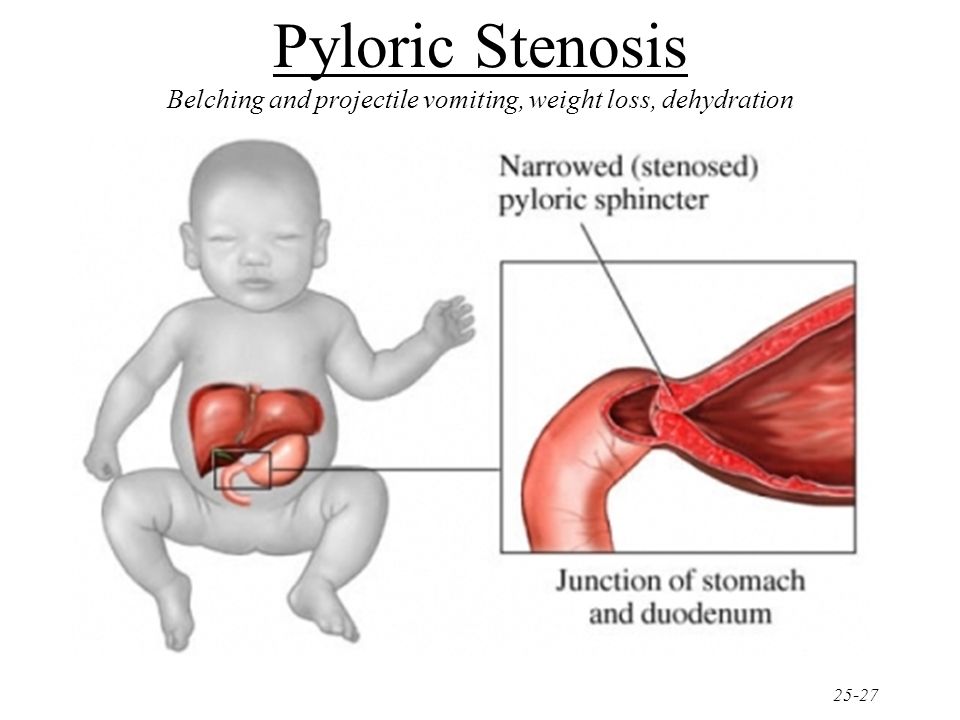 This is a minimally invasive operation in which a camera is inserted through a small incision into the child's abdomen, followed by an instrument that cuts the outer layers of the pyloric muscles.
This is a minimally invasive operation in which a camera is inserted through a small incision into the child's abdomen, followed by an instrument that cuts the outer layers of the pyloric muscles.
As a result, the narrowed area expands, and food can freely enter the intestines. This procedure is performed very quickly after diagnosis, sometimes even on the same day. The results of treatment with this procedure are very successful. The procedure carries a low risk of complications, the most common of which are bleeding and infection. Vomiting usually stops within a few days, and then the child begins to eat more food to "catch up". Most babies go home 48 hours after surgery and the recovery period is one week.
In adults, surgery is also performed for pyloric stenosis. In some cases, resection of part of the stomach (partial gastrectomy) is preferable because prolonged pyloric stenosis in adults increases the risk of stomach cancer. The pyloric lumen can also be enlarged with endoscopic surgery, but stenosis often recurs after this procedure.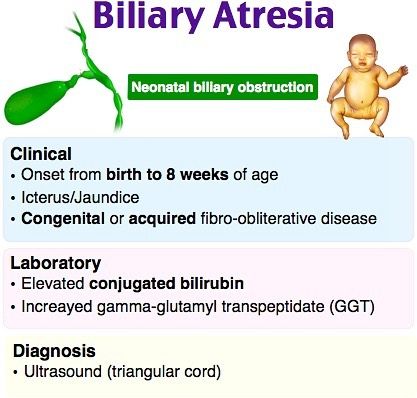
Vidkriti Zgornuti
Control of cure
If the disease is treated with surgery at an early stage, the prognosis is usually good even in severe cases. After the operation, the child can eat in 2-4 hours. With pyloric stenosis, there are usually no relapses, but visits to a gastroenterologist and periodic instrumental diagnostics are required. Thanks to prompt measures, the mortality rate is now well below one percent.
Vidkriti Zgornuti
Prevention of the disease
There are no preventive measures for this pathology. However, it is important that parents recognize the signs and symptoms of the disease so that the child receives medical attention as soon as possible. It can prevent dehydration, weight loss and malnutrition.
Prevention of pyloric stenosis may include consultation with a geneticist during pregnancy, especially if there is a history of the disease in the family. Also, a woman should not be in contact with infectious patients in order to avoid antibiotic treatment.
Also, a woman should not be in contact with infectious patients in order to avoid antibiotic treatment.
Vidkriti Zgornuti
Q&A
What can I eat with pyloric stenosis?
With pyloric stenosis, a liquid diet is recommended: soups, juices, broth, liquid and pureed cereals. During the consultation of a gastroenterologist, the optimal menu for the patient is selected. In the absence of the opportunity to take food in a natural way, feeding is done using a probe.
What causes pyloric stenosis?
Pyloric stenosis can be either congenital or acquired. In the first case, the disease occurs due to genetic disorders and is diagnosed in the first month of life. In adults, pyloric stenosis is most often provoked by chronic stomach ulcers. Less commonly, the disease occurs against the background of a perforated ulcer, chronic gastritis, a cancerous tumor, and a chemical burn.
How to identify pyloric stenosis?
The primary diagnostic method is ultrasound, which allows you to study the full stomach and the hypertrophied layer in the pyloric region. With the help of x-rays, an increase in the cavity of the stomach and its peristalsis is determined. With the introduction of contrast on fluoroscopy, the pyloric zone is clearly visible. Gastroscopy reveals a decrease in the contractile function of the stomach.
With the help of x-rays, an increase in the cavity of the stomach and its peristalsis is determined. With the introduction of contrast on fluoroscopy, the pyloric zone is clearly visible. Gastroscopy reveals a decrease in the contractile function of the stomach.
Vidkriti Zgornuti
The article is for informational purposes only. Please remember: self-medication can harm your health.
Vidkriti Zgornuti
Springs
- Mayo Clinic
- Medscape
Vidkriti Zgornuti
The author of the article:
Zaritskaya Yulia Mikhailovna
Gastroenterologist of the highest category
Expert in the direction:
Vasquez Abanto Anna Estuardovna
General practitioner, gastroenterologist
Which doctor treats pyloric stenosis?
Clinic MEDICOM has all the resources to carry out effective diagnosis and treatment of pyloric stenosis in Kyiv. Both for a child and for an adult patient, a consultation of a gastroenterologist and a surgeon will be held when drawing up an individual treatment plan. Surgical operation for an adult patient can be performed in the hospital of the MEDICOM clinic on Obolonskaya embankment, 9.
Both for a child and for an adult patient, a consultation of a gastroenterologist and a surgeon will be held when drawing up an individual treatment plan. Surgical operation for an adult patient can be performed in the hospital of the MEDICOM clinic on Obolonskaya embankment, 9.
And remember, if an adult can endure painful sensations for a long time, then it is necessary to respond immediately to the deterioration of the baby's well-being in order to preserve the health and life of the child. Call the 24-hour contact center to make an appointment without delay.
show more
Certificates
Reviews
02.11.2021 10:35
Nadiya Viktorivna
The following, authoritative article, the sons performed an operation on 2 different types of people, in good health, on the child himself.
09/21/2021 18:03
Tanya
Thank you for the information. My child is 1.5 months old, often spitting up, gaining weight poorly, the doctors talk about a treacherous person, they signed up for an ultrasound scan.
14.06.2021 13:54
Vita Omelchenko
The article is already good. We are getting ready for the operation, so they scared us. Now I want to sort it out.
leave feedback
Congenital pyloric stenosis. What is congenital pyloric stenosis?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Congenital pyloric stenosis is a malformation of the gastrointestinal tract, characterized by an organic narrowing of the pyloric section of the stomach adjacent to the duodenum. Congenital pyloric stenosis manifests itself on the 2nd-4th week of a child's life with "fountain" vomiting that occurs after feeding, a decrease in body weight and skin turgor, oliguria, and constipation. Methods for diagnosing congenital pyloric stenosis are ultrasound, X-ray and endoscopic examination of the stomach. Treatment of congenital pyloric stenosis is carried out only surgically and consists in performing pyloromyotomy.
Methods for diagnosing congenital pyloric stenosis are ultrasound, X-ray and endoscopic examination of the stomach. Treatment of congenital pyloric stenosis is carried out only surgically and consists in performing pyloromyotomy.
- Reasons
- Symptoms of congenital pyloric stenosis
- Diagnostics
- Treatment of congenital pyloric stenosis
- Forecast
- Treatment prices
General
Congenital pyloric stenosis is an anomaly in the development of the stomach, namely its pyloric (output) section, leading to a violation of its patency and difficulty in evacuating food. In pediatrics, congenital pyloric stenosis occurs with a population frequency of 1 in 300 newborns; boys are born 4 times more often with this defect. Congenital pyloric stenosis is the most common surgical pathology of the neonatal period, requiring immediate surgical treatment.
The pyloric part of the stomach (pylorus, pylorus) is the distal part of the stomach, directly adjacent to the duodenum and including the pylorus cave (antrum) and the pyloric canal.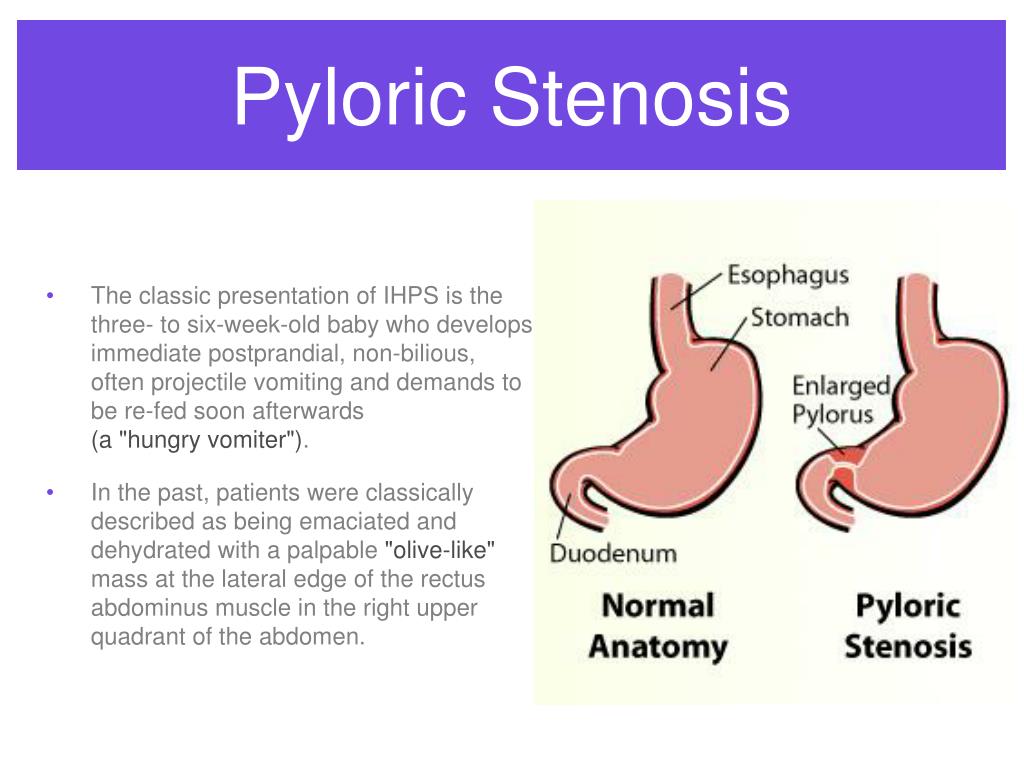 The antral part serves as a reservoir for the accumulation of partially digested food, and the pyloric canal (the narrowest part of the stomach) performs an evacuation function - transporting the contents of the stomach into the duodenum. With congenital pyloric stenosis, the passage of food through the pylorus is difficult, which leads to its accumulation in the stomach and the development of vomiting syndrome, which quickly leads to dehydration, alkalosis and exhaustion of the child.
The antral part serves as a reservoir for the accumulation of partially digested food, and the pyloric canal (the narrowest part of the stomach) performs an evacuation function - transporting the contents of the stomach into the duodenum. With congenital pyloric stenosis, the passage of food through the pylorus is difficult, which leads to its accumulation in the stomach and the development of vomiting syndrome, which quickly leads to dehydration, alkalosis and exhaustion of the child.
Congenital pyloric stenosis
Causes
Congenital pyloric stenosis is a malformation of the distal stomach, caused by hypertrophy of the muscular layer of the pylorus in embryogenesis, underdevelopment of the ganglia and insufficient peptidergic innervation of the pylorus, intrauterine delay in the opening of the pyloric canal. Currently, congenital pyloric stenosis is considered as a multifactorial pathology, the origin of which may involve family and hereditary factors and adverse effects on the developing fetus.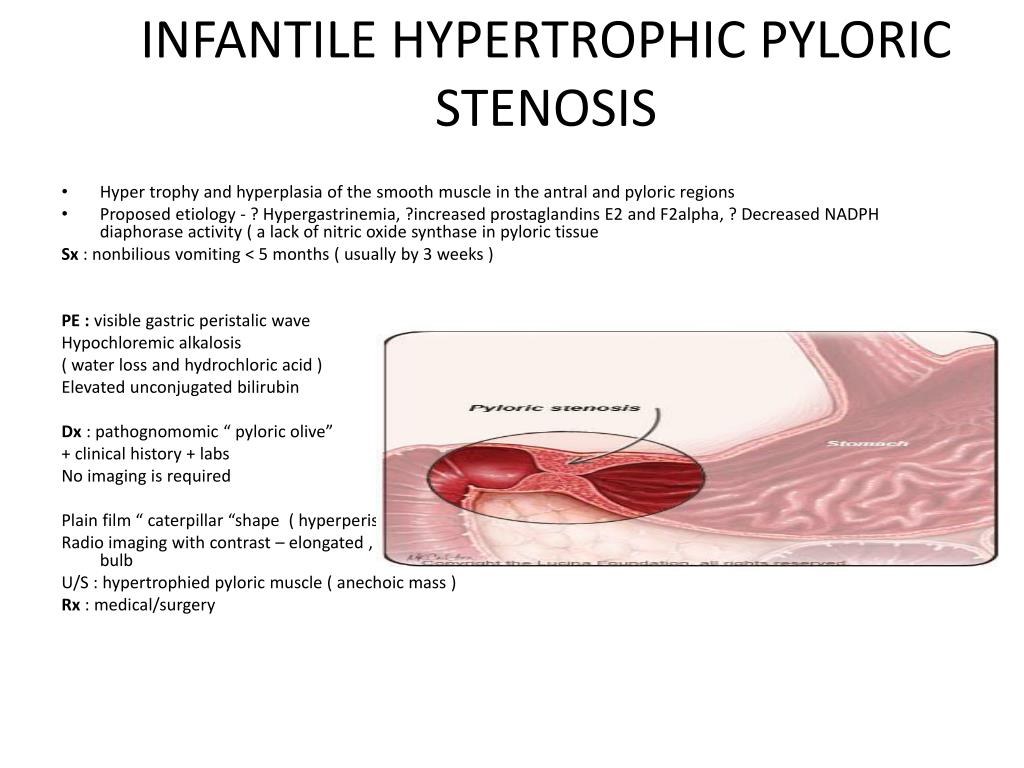
When studying the genetic aspect of congenital pyloric stenosis, cases of recessive, sex-linked and autosomal dominant inheritance have been described. It is known that if the father had congenital pyloric stenosis in the past, the risk of having a child with the same defect is 5% for boys and 2% for girls; if the mother suffered from pyloric stenosis in childhood, the probability of inheriting the disease for boys is 15%, and for girls - 6%.
The promoters of the development of congenital pyloric stenosis can be unfavorable exogenous factors: intrauterine infections (rubella, cytomegaly, herpes), increased maternal gastrin levels, treatment of the newborn with antibiotics (in particular, erythromycin) in the first 2 weeks of life.
Acquired pyloric stenosis in adults can develop as a complication of peptic ulcers of the stomach located close to the pylorus, with gastric cancer or pancreatic cancer. In this case, the pyloric canal narrows due to scar tissue or tumor infiltrate, which leads to the development of symptoms resembling congenital pyloric stenosis.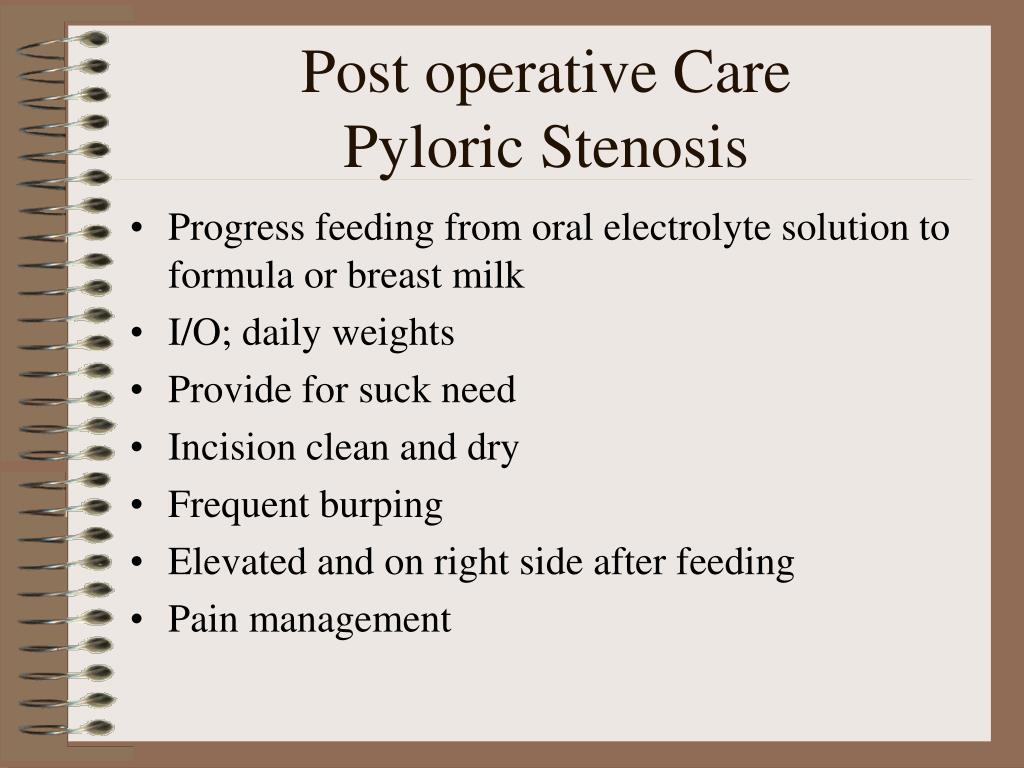
Macroscopically, there is a thickening of the wall of the pyloric canal up to 3-7 mm (at a norm of 1-2 mm), elongation and olive shape of the pylorus, its white color and cartilaginous density. Morphological examination of preparations reveals hypertrophy of circular muscle fibers, edema and sclerosis of the mucous and submucosal layers, impaired differentiation of connective tissue structures.
Symptoms of congenital pyloric stenosis
Depending on the clinical course, acute and protracted congenital pyloric stenosis is distinguished, which goes through compensated, subcompensated and decompensated stages. The degree of narrowing of the pyloric canal and the compensatory possibilities of the child's stomach affect the time of development and severity of symptoms of congenital pyloric stenosis.
In the first days of a child's life, regurgitation and infrequent vomiting are noted. A distinct clinic of congenital pyloric stenosis appears by the end of the second or beginning of the third week of a child's life.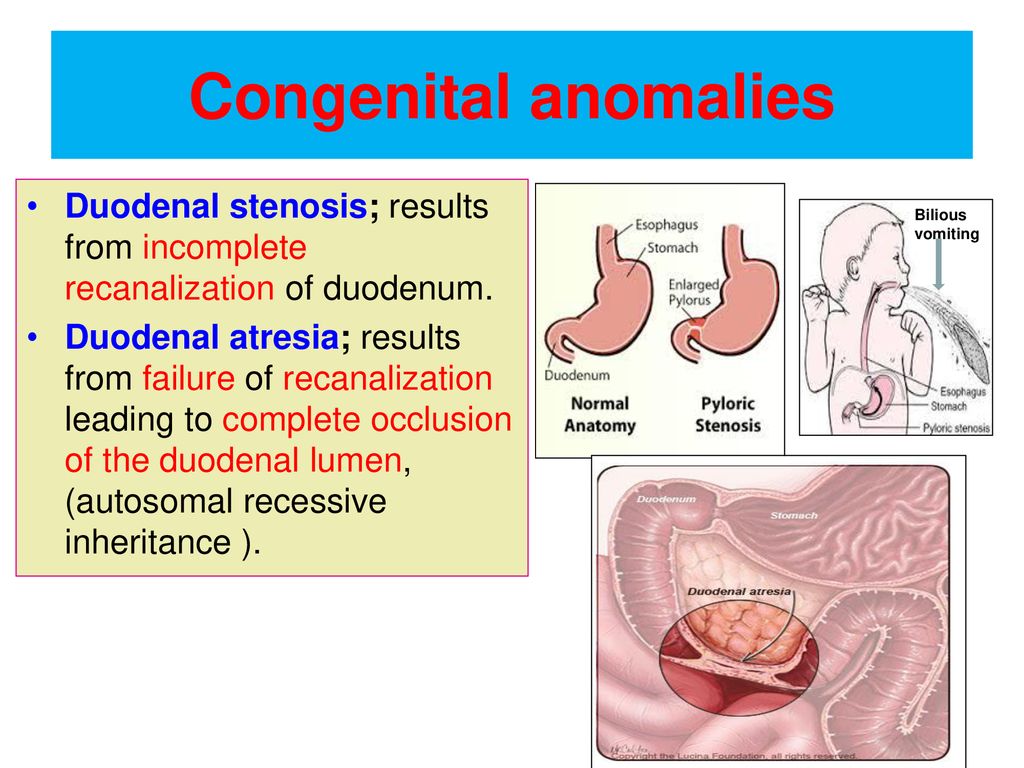 A typical sign of pyloric stenosis is vomiting "fountain" after almost every feeding. At the same time, the volume of vomit significantly exceeds the amount of milk sucked during the last feeding. The nature of the vomit is stagnant, in the form of curdled milk with a sour smell. An important differential diagnostic sign of congenital pyloric stenosis is the absence of bile impurities in the vomit.
A typical sign of pyloric stenosis is vomiting "fountain" after almost every feeding. At the same time, the volume of vomit significantly exceeds the amount of milk sucked during the last feeding. The nature of the vomit is stagnant, in the form of curdled milk with a sour smell. An important differential diagnostic sign of congenital pyloric stenosis is the absence of bile impurities in the vomit.
Against the background of constant vomiting in a child with congenital pyloric stenosis, dehydration and malnutrition rapidly progress, the frequency of urination decreases, and constipation appears. The child's stool has a dark green color due to the predominance of bile; urine becomes concentrated, leaves colored stains on the diapers.
Due to violations of the water-salt balance, severe metabolic and electrolyte disorders (hypovolemia, alkalosis), deficiency anemia, and blood clots develop. A complication of congenital pyloric stenosis can be a pyloric ulcer with perforation of the ulcer and gastrointestinal bleeding.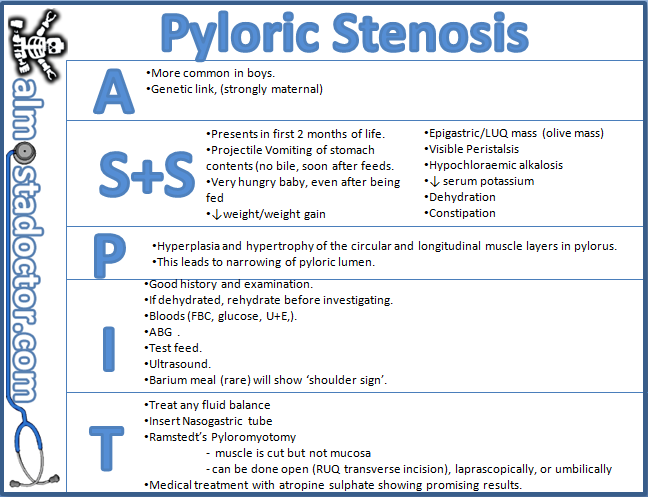 Vomiting syndrome can lead to asphyxia, eustachitis, otitis, aspiration pneumonia.
Vomiting syndrome can lead to asphyxia, eustachitis, otitis, aspiration pneumonia.
Diagnostics
A child with suspected congenital pyloric stenosis should be referred by a pediatrician to a pediatric surgeon. The diagnosis is confirmed by ultrasound, endoscopic, x-ray examination of the stomach.
When examining a child with congenital pyloric stenosis, swelling in the epigastric region is determined, visible peristalsis of the stomach (an hourglass symptom). In most cases, it is possible to palpate a hypertrophied pylorus, which has a dense consistency and a plum-like shape.
Laboratory analyzes (UAC, CBS of blood, biochemical analysis of blood) are characterized by an increase in hematocrit, metabolic alkalosis, hypokalemia, hypochloremia.
Children with suspected congenital pyloric stenosis are shown to have an ultrasound of the stomach with a water-siphon test. When examining the pyloric canal, its tight closure, thickening of the muscle pulp, and the absence of evacuation of the contents into the duodenum are noticeable.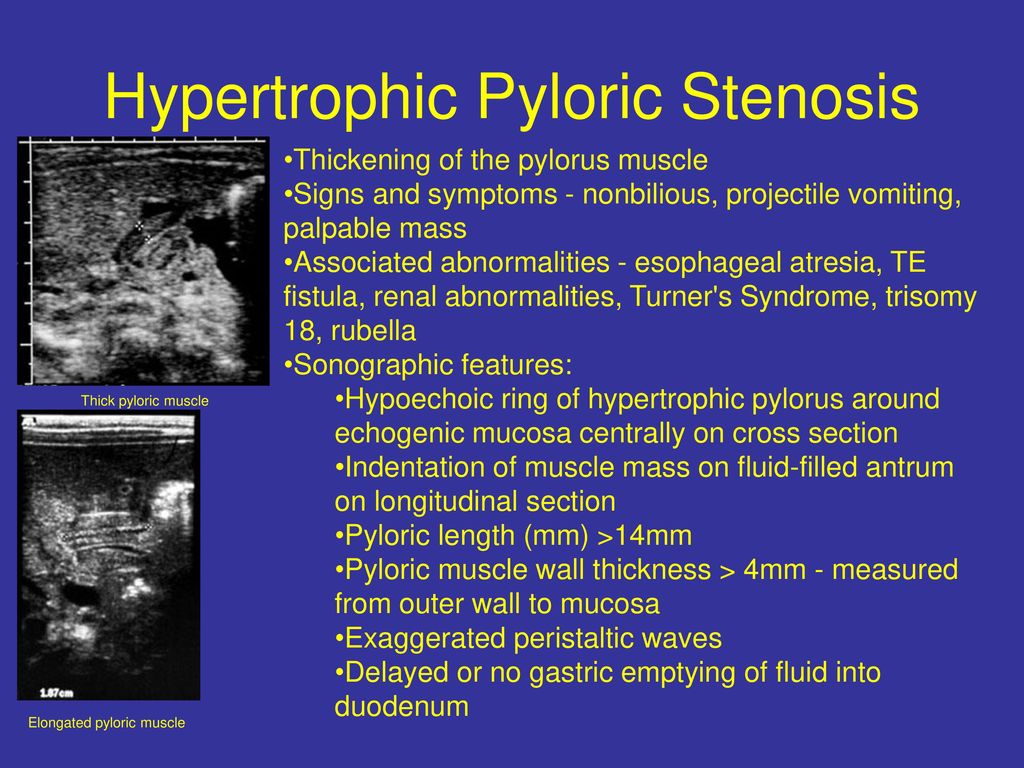 When conducting esophagogastroduodenoscopy, a child with congenital pyloric stenosis is determined by the expansion of the antrum and the narrowing of the lumen of the pylorus canal to the size of a pinhead. Unlike pylorospasm, in congenital pyloric stenosis, the pyloric canal does not open with air insufflation. According to endoscopic data, reflux esophagitis is often detected in congenital pyloric stenosis.
When conducting esophagogastroduodenoscopy, a child with congenital pyloric stenosis is determined by the expansion of the antrum and the narrowing of the lumen of the pylorus canal to the size of a pinhead. Unlike pylorospasm, in congenital pyloric stenosis, the pyloric canal does not open with air insufflation. According to endoscopic data, reflux esophagitis is often detected in congenital pyloric stenosis.
Plain radiography of the abdominal cavity demonstrates an increase in the size of the stomach, the presence of an empty stomach fluid level in it, and a decrease in gas filling of the intestinal loops. When performing radiography of the stomach with a barium suspension, segmenting peristalsis, a delay in contrast in the stomach and the absence of its evacuation into the duodenum 12 attract attention, in the lateral projection there is a symptom of the antropyloric "beak" (narrowing of the pyloric canal).
Differential diagnosis of congenital pyloric stenosis is carried out with pylorospasm, intestinal obstruction, hiatal hernia, duodenal atresia and stenosis, GERD.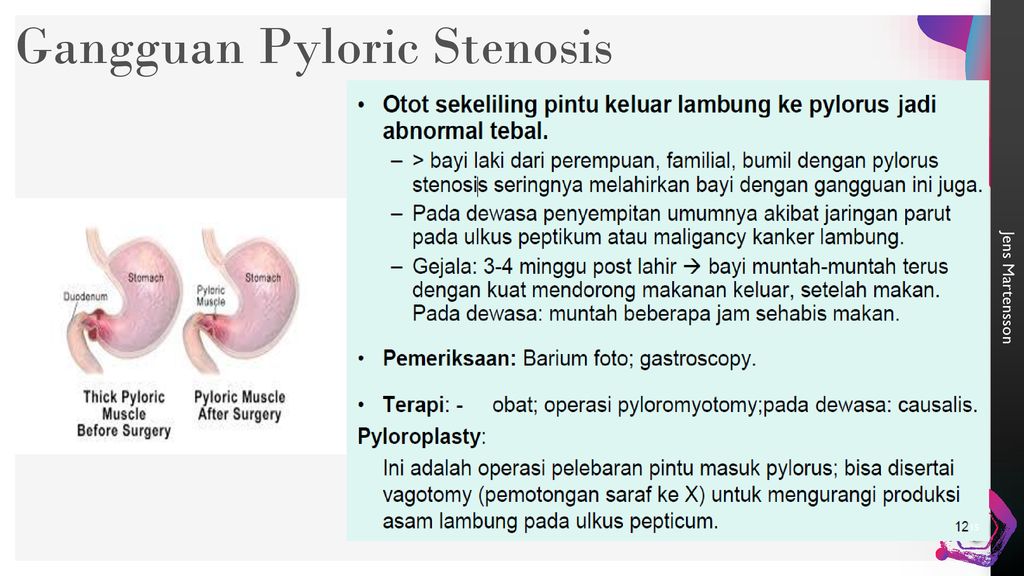
Treatment of congenital pyloric stenosis
The presence of congenital pyloric stenosis in a child requires active surgical tactics. Bougienage of the pyloric canal leads to its short-term opening and re-stenosis.
Surgical treatment of congenital pyloric stenosis is preceded by preoperative preparation of the child, including infusion therapy with glucose-salt and protein solutions, the use of antispasmodics, replenishment of fluid and nutrient deficiency with microclysters.
In congenital pyloric stenosis, Frede-Ramstedt pyloromyotomy is performed, during which the pyloric sero-muscular layer is dissected to the mucosa, thereby eliminating the anatomical obstruction and restoring the patency of the pyloric canal. The operation is performed by an open, laparoscopic or transumbilical method. In the postoperative period, dosed feeding is carried out, the volume of which is brought to the age norm by 8-9 days.