Do i burp baby after dream feed
What Is Dream Feeding? And How Do I Dream Feed? – Happiest Baby
By Dr. Harvey Karp, MD, FAAP
On This Page
- Dream Feeding: What It Is
- How to Dream Feed
- How to Get Your Baby Back to Sleep
- Dream Feeding Tips
- Dream Feeding Benefits
- Adding a Second Dream Feed
- When to Stop Dream Feeds
- Final Thoughts on Dream Feeds
Newborn babies eat a lot. Breastfed infants eat about every two to three hours and formula-fed babies hit the bottle every three to four hours…and that doesn’t stop when bedtime calls. In fact, bottle-fed babies often continue night feedings until they’re around 6 months old, whereas breastfed babies may continue up to a year. But that doesn’t mean that there’s nothing you can do to tame night-waking. If your little one wakes up hungry each night, it’s smart to increase daytime milk (research shows that infants who received more milk or solid feeds during the day are less likely to feed at night) and boost their evening calories by way of a dream feed. Think of a dream feed as topping off your car’s gas tank...so there's no need to refuel during the journey ahead. Offering your baby a dream feed will eliminate—or at least delay—one of the top reasons babies wake through the night: a rumbling tummy.
Dream feeding is when you rouse your baby—without fully waking them up—to feed them one more time before you turn in for the night. Babies who go to sleep between 6pm and 8pm often wake out of hunger in the middle of the night. But research has shown that sneaking in an extra feed between 10pm and midnight can reduce night wakings, helping babies stay asleep until a more “reasonable” time of the morning. This can become part of your little one’s regular sleep schedule.
Babies who go to sleep between 6pm and 8pm often wake out of hunger in the middle of the night. But research has shown that sneaking in an extra feed between 10pm and midnight can reduce night wakings, helping babies stay asleep until a more “reasonable” time of the morning. This can become part of your little one’s regular sleep schedule.
The goal of a dream feed is to offer your little one more meal before you hit the hay, so that you and your baby’s schedule sync better…and you both sleep better. Ready to try it? Follow these steps:
-
Step 1: Gently take your baby out of the bassinet or crib between 10pm and 12am, or whenever when you go to bed. Keep the room dim and quiet, except for white noise. Doing this during Baby’s more active REM sleep is ideal. During REM sleep your baby may flutter their eyelids, make little squeaks and squawks, or move around more than usual.
-
Step 2: Keep your baby swaddled. There’s no need to unswaddle—or change your baby’s diaper—if they’ll take the feed that way and their diaper isn’t soiled. (If your baby is super sleepy, you may need to rouse them a bit by gently tickling their toes.)
-
Step 3: Touch Baby’s cheek with your breast or bottle. Placing your breast or bottle on your baby's cheek or lower lip will wake up their rooting reflex and get your baby to start eating.
-
Step 4: Offer a brief feed. Encourage nursing for 5 to 10 minutes on each side. For bottle-fed babies, try for about 3 ounces.
-
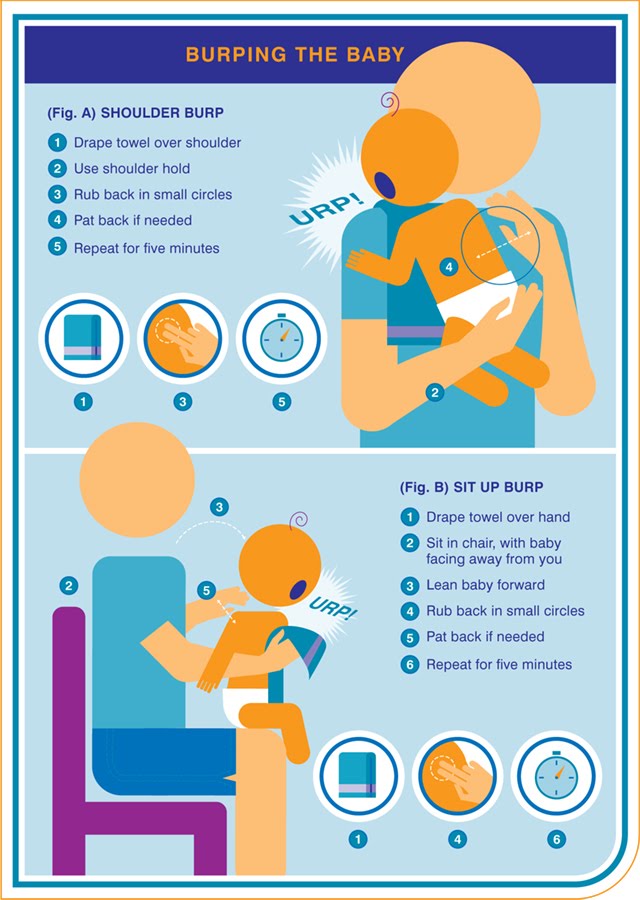
Step 5: Burp your baby. Many parents ask: Do you burp a baby after a dream feed? and the answer is always yes. You want to burp a baby after a dream feed—or any feed—before putting them back down on their back.
Oftentimes, a baby who has just enjoyed a dream feed can be returned to their bassinet with nary a wakeup. But if your little one has woken up during or after a dream feed, you can get them back down with the help of the 5 S’s: Swaddling, Side/Stomach, Shushing, Swinging, Sucking.
But if your little one has woken up during or after a dream feed, you can get them back down with the help of the 5 S’s: Swaddling, Side/Stomach, Shushing, Swinging, Sucking.
First, if you haven’t already, swaddle your baby and put on some rumbly white noise. I recommend playing white noise all night, but you can turn up the volume as you’re putting your baby back down. The most effective white noise for sleep is continuous, monotonous, and at a low-pitch, like my SNOO sounds download or SNOObear, Happiest Baby’s white noise lovey.
At the same time, gentle rhythmic motion can help lull babies to sleep. In fact, a 2019 study in the journal PLOS ONE found that the magical mix of swaddling, white noise, and rocking “evokes an immediate calming response” when caregivers soothe their infants and when they use SNOO, my responsive bassinet. SNOO uses womb-like white noise and motion (and a built-in swaddle!) to quickly settle babies back to sleep after a feed…usually adding sleep for the whole family.
Other time-tested tricks to help a baby sleep after a dream feed include rocking in a rocking chair, walking with your baby in your arms, bouncing on an exercise ball, and offering a pacifier, which fulfills the Sucking portion of the 5 S’s. As an added bonus, research suggests a bedtime paci helps lower the risk of sudden infant sleep death, or SIDS.
As you put your little one back into their bassinet, do my quick wake-and-sleep trick, which teaches your baby to fall asleep on their own. Here’s the gist: Right after you put your baby down, gently rouse them with a gentle tickle on their feet until they barely open their eyes. After a few seconds, they’ll close their eyes again and slide back to sleep. If your little one fusses, pick them up for a feed or a cuddle, then repeat the gentle-tickle-to-wake routine.
Set your baby up for dream feed success:As I mentioned earlier, the one-two punch of adding daytime calories and dream feeds can really work wonders to help babies sleep longer. Try offering cluster feeds from about 4pm till bedtime. Cluster feeds are a series of quick milky meals given to Baby every one to two hours. They’re meant to load your little one’s system with calories to keep them well stocked with nutrition through the night. At the same time, put your little one down for night-night safely swaddled with your trusted white noise on. Consider this another “dream team” to help Baby sleep better!
Try offering cluster feeds from about 4pm till bedtime. Cluster feeds are a series of quick milky meals given to Baby every one to two hours. They’re meant to load your little one’s system with calories to keep them well stocked with nutrition through the night. At the same time, put your little one down for night-night safely swaddled with your trusted white noise on. Consider this another “dream team” to help Baby sleep better!
A wonderful thing about dream feeding is that doesn’t interfere with your little one’s need to feed at night. Instead, dream feeding simply shifts your baby’s feeding schedule just a bit so that it’s more conducive to your sleep schedule, too. Plus, dream feeding means that…
- Your baby will get the extra calories they need to sleep better.
- Your baby is eating a meal at a convenient time, so you can sleep longer, too.
- You’re not responding to your baby’s crying with food, which is important because reacting to cries with a feed can inadvertently encourage your baby to eat more at night.

- Your baby will eat less during the night and therefore be hungrier in the morning, which will boost daytime eating.
If your baby frequently wakes around 3:30am despite having an earlier dream feed and using strong, rumbly white noise, consider setting your alarm and giving one more dream feed at 3am. Again, it’s best to keep the lights dim and to not talk or cuddle too much at this hour. You want to be loving when you feed your baby, but you don’t want your little one to think that it’s time to play! The idea is to pick up and feed your little one before they wake you, so you’re giving your baby the nourishment they need, but not rewarding them for waking and crying.
If you must do this early-morning dream feed, every three days, reduce the 3am feed a bit more by giving a little less milk than usual. If you’re nursing, just feed on one side for the second dream feed. If you’re bottle-feeding, you can try doubling the amount of water the formula directions suggest—for just ONE feeding and ONLY for a couple days. This is very important: It’s dangerous to dilute baby formula for meals. It can cause serious health problems. Diluting for this ONE wee-hour feed for a brief period of time is different. The purpose of the extra water is to fill your baby’s stomach with enough ounces, but fewer calories. This can help babies sleep through to morning…when they will be hungry and ready to eat their full bottle again. Again, this is a temporary fix only to be used for the 3am dream feed—and only for a couple of nights.
This is very important: It’s dangerous to dilute baby formula for meals. It can cause serious health problems. Diluting for this ONE wee-hour feed for a brief period of time is different. The purpose of the extra water is to fill your baby’s stomach with enough ounces, but fewer calories. This can help babies sleep through to morning…when they will be hungry and ready to eat their full bottle again. Again, this is a temporary fix only to be used for the 3am dream feed—and only for a couple of nights.
All babies are different, so there is no specific age recommendation for stopping a dream feed. My general rule is that you can bid adieu to the dream feed 2 to 4 weeks after your baby is sleeping well from the time of your dream feed on through to the morning. (Learn when your baby might start sleeping through the night.) Of course, if the dream feed isn’t working for you, there’s no need to continue!
Final Thoughts on the Dream Feed and Other Sleep TipsOffering a dream feed to your snoozing baby before you declare “lights out” may give you a chance to catch more precious ZZZs, which, of course, is fantastic! Giving a dream feed can also help train your sweet pea to stay asleep for longer stretches…and that skill can carry over to better night sleeps down the road, too. Beyond dream feeding, if your newborn baby is having difficulty sleeping, you may need a little extra help lulling them to dreamland. This is where I hope SNOO can help exhausted families by automatically soothing fussing with gentle rocking and white noise. You can learn more about SNOO and find other great sleep resources below:
Beyond dream feeding, if your newborn baby is having difficulty sleeping, you may need a little extra help lulling them to dreamland. This is where I hope SNOO can help exhausted families by automatically soothing fussing with gentle rocking and white noise. You can learn more about SNOO and find other great sleep resources below:
- SNOO Success Stories
- All About Your Baby’s Wake Windows
- What to Do When Your Baby Won't Sleep in a Bassinet
- How to Turn On Baby’s “On Switch” for Sleep
- Sleep Regression 101
About Dr. Harvey Karp
Dr. Harvey Karp, one of America’s most trusted pediatricians, is the founder of Happiest Baby and the inventor of the groundbreaking SNOO Smart Sleeper. After years of treating patients in Los Angeles, Dr. Karp vaulted to global prominence with the release of the bestselling Happiest Baby on the Block and Happiest Toddler on the Block. His celebrated books and videos have since become standard pediatric practice, translated into more than 20 languages and have helped millions of parents. Dr. Karp’s landmark methods, including the 5 S’s for soothing babies, guide parents to understand and nurture their children and relieve stressful issues, like new-parent exhaustion, infant crying, and toddler tantrums.
Dr. Karp’s landmark methods, including the 5 S’s for soothing babies, guide parents to understand and nurture their children and relieve stressful issues, like new-parent exhaustion, infant crying, and toddler tantrums.
View more posts tagged, feeding
Have questions about a Happiest Baby product? Our consultants would be happy to help! Connect with us at [email protected].
Disclaimer: The information on our site is NOT medical advice for any specific person or condition. It is only meant as general information. If you have any medical questions and concerns about your child or yourself, please contact your health provider.
How to Properly Dream Feed Your Baby
Skip to contentLearning how to dream feed baby is quite simple. Yay! Yet dream feeding is one of those terms that gets tossed around so much that everyone assumes that everyone else knows the exact meaning of the term. When you dig a little deeper, you see that people have WILDLY different definitions of the same exact term!
When you dig a little deeper, you see that people have WILDLY different definitions of the same exact term!
Last Updated Jan 27, 2021.
Photo Credit: Zach Lucero
So What Is a Dream Feed?
Just so everyone is on the same page…
A dream feed is when:
- a parent goes to their sleeping infant,
- picks them up to breastfeed
- or props them up either in their crib, or in a caregiver’s arms, to offer a bottle,
- feeds the child,
- and then puts them back down *asleep* without the baby ever having woken up.
A dream feed is NOT a dream feed if a child:
- opens their eyes at any point in the process,
- or if the feeding is in response to the baby waking up.
Generally speaking, a dream feed is done between the hours of about 9:30pm and 12:00am. Technically, if all other terms are met, but the feed is done outside of these hours, the feeding is still a dream feed.
The Right Age for Dream Feeding
Dream feeds are a great tool from birth (or a few weeks after, when babies are not quite so sleepy), through to when a baby is done being swaddled.![]() It is very challenging to dream feed a baby, even a very young one, without waking them up if they are not swaddled. Generally speaking, it’s wise to stop dream feeding around 14–16 weeks of age. After this age, babies become a lot more awake and aware, and dream feeds tend to disrupt the rest of their overnight sleep.
It is very challenging to dream feed a baby, even a very young one, without waking them up if they are not swaddled. Generally speaking, it’s wise to stop dream feeding around 14–16 weeks of age. After this age, babies become a lot more awake and aware, and dream feeds tend to disrupt the rest of their overnight sleep.
Check out my Newborn Sleep Program!
Benefits of Dream Feeding
Let me first dispel a myth. A dream feed does not necessarily prevent a baby from waking up to eat at night. Although, sometimes it does work. I like dream feeds for young babies because I appreciate the “insurance policy” of extra calories at night. As long as a baby is young enough that the dream feed itself does not wake them, and fracture their remaining nighttime sleep, a dream feed can insure as many calories as possible during each 24-hour period.
A gift to reflux-y babies!
Some babies respond beautifully to a dream feed. Especially those with reflux! From about 7pm on through to about 2 or 3am, the body is flooded with the hormone melatonin. Melatonin is responsible for many things. Chief amongst them is making the body feel drowsy, and relaxing the long muscles (abs, legs, and arms). Since the abdominal muscles are relaxed, it’s common for babies with a lot of reflux to tolerate a dream feed without spitting up. And even possibly negate the need to be burped, or held upright afterwards. I can speak to this from personal experience with my own extremely reflux-y, wholly unmedicated daughter. Since the concern for calorie intake is so high with reflux babies, dream feeds can be especially useful for them.
Melatonin is responsible for many things. Chief amongst them is making the body feel drowsy, and relaxing the long muscles (abs, legs, and arms). Since the abdominal muscles are relaxed, it’s common for babies with a lot of reflux to tolerate a dream feed without spitting up. And even possibly negate the need to be burped, or held upright afterwards. I can speak to this from personal experience with my own extremely reflux-y, wholly unmedicated daughter. Since the concern for calorie intake is so high with reflux babies, dream feeds can be especially useful for them.
Burping After a Dream Feed
If you feel your sleeping baby needs to be burped, go ahead and attempt to burp them as you normally would during the day. Check in with your pediatrician to ask how long to attempt a burp before giving up and putting baby back to sleep.
The bottom line is that a dream feed done correctly can benefit baby AND parents by offering an extra dose of nutrition, while also possibly helping baby sleep! (Which means YOU can get more sleep too! Win!)
If you like staying in the know with the most up-to-date information, and learning everything you can about your little one’s sleep, please sign up for my newsletter using the button below!
Sign up for my newsletter!
So remember, to properly dream feed your baby…
- Enter their room (keeping it dark!), and prop baby up either in their crib, or your arms, and immediately start feeding them the breast or bottle.

- Dream feed between 9:30pm-12:30am (or whenever you are heading to bed yourself!)
- Baby should NOT wake up AT ALL during the entire feeding. (Baby should be put back down in bed just as asleep as they were when you starting the feeding.)
- You should stop attempting dream feeds when baby starts to sleep unswaddled. (Or around 14-16 weeks old when these feeds can start to become disruptive to their nighttime sleep.)
If you want to learn everything I know about babies under 16 weeks, check out The Newborn Sleep Program. This program can help set up your newborn (and you) for the best possible sleep! And if your baby is older than 16 weeks old, and you’re looking for affordable, hands-on sleep training support, check out my online training series: The Baby Sleep Trainer Program + Support. Use the code DFbaby for 10% off either program.[/fusion_text][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]
Search for:
Articles by Age
Categories
- Naps
- Newborn
- Opinion
- Sleep FAQs
- Sleep Training
- Getting Started
- How To Be Successful
- Success Stories
- Troubleshooting
Frequent vomiting in babies: normal or not
Every caring parent is attentive to the health of their child, so as not to miss the first symptoms of serious diseases. If the child is the first, the reactions of his body, in particular regurgitation, cause concern. Most often it occurs for a physiological reason.
If the child is the first, the reactions of his body, in particular regurgitation, cause concern. Most often it occurs for a physiological reason.
There is a sphincter between the stomach and the esophagus. In children from birth to a year, it is underdeveloped and is not able to keep food in the stomach. Any careless movement leads to the fact that the contents of the stomach pour out through the esophagus, that is, the child burps. To avoid this, pediatricians recommend carrying the child in the “column” position for half an hour after eating. Even in this position, regurgitation is possible, since pressure on the chest and stomach of the child cannot be completely eliminated. There is nothing to worry about, but in some cases regurgitation indicates the presence of serious diseases.
What is normal
If the child spits up only a small part of the food, is active, feels good, there is no reason for concern. In the presence of temperature, capriciousness, lethargy, regurgitation can be one of the symptoms of the disease. For babies up to six months, the norm is spitting up small portions of food up to 6-8 times a day. The curdled consistency of regurgitation is not a cause for concern. This is milk curdled under the influence of a special enzyme contained in the gastric juice, and prepared for further digestion.
For babies up to six months, the norm is spitting up small portions of food up to 6-8 times a day. The curdled consistency of regurgitation is not a cause for concern. This is milk curdled under the influence of a special enzyme contained in the gastric juice, and prepared for further digestion.
The so-called "fountain" regurgitation should alert parents and force them to closely monitor the baby's condition. It is necessary to drink it with warm boiled water, for some time vilify vertically. If such regurgitation was a one-time occurrence, the crumbs do not have a temperature, you should not worry. If the situation recurs, you should consult a doctor.
Causes of regurgitation
Newborns do not realize how much food they need and often overeat. Parents misinterpret the crying of the baby, and begin to feed him on demand. The baby may not be hungry, but simply demand the attention of the mother, her warmth. Excess food is not retained in the stomach, and the child burps.
When breastfeeding, the baby sometimes does not grasp the nipple correctly, and swallows air along with milk. It will come out with a little milk. Another common cause of regurgitation is excess gas. Food moves to the intestines more slowly than necessary, and part of it is ejected through the esophagus.
Serious problems that are manifested by frequent regurgitation include congenital defects of the gastrointestinal tract and central nervous system, intestinal obstruction.
Troubleshooting
Most causes of spitting up are easy to fix, but the situation can be more serious. Some children suffer from lactose intolerance, which is genetically determined. The sooner this is detected and the necessary treatment is started, the better the child will develop. Lactose intolerance can be suspected if the baby spits up breast milk, and this problem is not observed when feeding with mixtures. Timely diagnosis of genetic lactose intolerance allows you to avoid a large number of child health problems in the future.
If parents are concerned about the frequent regurgitation of the baby, it is worth taking an analysis in one of the modern laboratories and consulting a doctor with its results. The modern level of laboratory diagnostics makes it possible to accurately determine the cause of the problem, and knowing it, the doctor will select the optimal treatment. No. 180035 Genetic lactose intolerance Savchenko Svetlana Petrovna
Expert in the field of laboratory diagnostics, healthcare organization, diagnostics and treatment of therapeutic diseases.
Article publication date: 02/16/2018
Updated: 08/19/2022
Why does the baby spit up after feeding?
search support iconSearch Keywords
Regurgitation is a common condition in newborns and infants and is most often a normal variant. However, it is not uncommon for parents to worry if their baby is spitting up frequently, believing that it is due to nutritional or health problems in general. Sometimes these fears are not unfounded, and regurgitation really has a pathological origin. What is its cause and when should you really consult a doctor about this?
However, it is not uncommon for parents to worry if their baby is spitting up frequently, believing that it is due to nutritional or health problems in general. Sometimes these fears are not unfounded, and regurgitation really has a pathological origin. What is its cause and when should you really consult a doctor about this?
Regurgitation - Return of a small amount of food (uncurdled or partially curdled milk) from the stomach up the digestive tract: into the esophagus and further into the oral cavity. According to statistics, at least 1 time during the day, at least 50% of babies from 0 to 3 months can spit up, more than 60% of children 3-4 months old, and 5% of children spit up until the year 1 .
Regurgitation in newborns is considered a physiological process. It is caused by a number of factors, including:
- Structural features of the upper digestive tract in babies
- In newborns and infants under one year old, the stomach has a spherical shape.
 It holds a small amount of food, besides, the release from it into the duodenum is slower in comparison with children after the year 2 .
It holds a small amount of food, besides, the release from it into the duodenum is slower in comparison with children after the year 2 . - Weakness of the lower esophageal sphincter that separates the esophagus from the stomach
- Normally, the lower esophageal sphincter should tightly "close" the esophagus, allowing food to pass into the stomach and not allowing it to enter back into the upper digestive tract. However, in young children (up to a year), the muscles of the esophageal sphincter are poorly developed, and it does not do its job very well 2 .
- Slow movement of food through the gastrointestinal tract
- The neuromuscular apparatus of newborns is immature. It does not ensure the proper movement of food through the esophagus, causing regurgitation.
One of the important risk factors contributing to regurgitation in newborns is aerophagia. This is the swallowing of large amounts of air during feedings. This happens when the baby is not properly attached to the breast, the mother has a lack of breast milk, or the bottle is in the wrong position in the child who receives the mixture. The size of the opening in the nipple also matters - if it is too large, the newborn swallows a lot of air 3 .
This happens when the baby is not properly attached to the breast, the mother has a lack of breast milk, or the bottle is in the wrong position in the child who receives the mixture. The size of the opening in the nipple also matters - if it is too large, the newborn swallows a lot of air 3 .
With aerophagia, the baby becomes capricious, restless immediately after feeding. Noticeable bloating. If the baby spits up immediately after a feed, the milk (or formula) remains practically fresh, uncurdled 3 .
Promotes post-feeding regurgitation and predominantly horizontal position of the baby during the day, combined with relatively high intra-abdominal pressure 4 . Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Regurgitation in many newborns can be provoked by other situations in which pressure in the abdominal cavity increases and stomach contents are thrown into the esophagus, in particular 3 :
- tight swaddling;
- stool disorders, in particular constipation;
- long, forced cry and some others.
Want to avoid common feeding problems?
Start with a baby bottle with an anti-colic system that helps avoid common feeding problems such as colic, gas and spitting up*
How can you tell the difference between normal spitting up and vomiting?
Sometimes regurgitation is considered a manifestation of disorders in the digestive tract of children. Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
If the mother is worried that her baby is spitting up often, keep track of when this happens and count the total number of spit ups per day. Normally, regurgitation usually occurs after eating (the child burps after each feeding), lasts no more than 20 seconds and repeats no more than 20-30 times a day. With pathology, the problem manifests itself at any time of the day, regardless of when the baby was fed. Their number can reach 50 per day, and sometimes more 1 .
The amount of discharge during regurgitation also matters. With normal, physiological regurgitation, it is approximately 5 - 30 ml. If this volume fluctuates between 50 and 100 ml, it is already defined as profuse vomiting. When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
Vomiting in babies is a warning sign. Doctors are especially alarmed by repeated vomiting, a fountain, with an admixture of bile, in combination with constipation. Vomiting can lead to the development of dehydration, acid-base imbalance and other consequences, therefore, if it occurs, you should urgently contact a pediatrician to find out the cause and begin treatment. A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
Physiological regurgitation: symptoms
Neonatal regurgitation, which is considered normal and not of concern to pediatricians 3 :
- usually lasts for a certain period of time;
- is characterized by slow, "passive" leakage; if the baby spits up a fountain, it is better to consult a doctor;
- has a sour smell of curdled milk;
- occurs without the participation of muscles - the baby does not strain during regurgitation;
- does not affect the general well-being of the baby.
How to help a newborn who spit up often?
If the baby is healthy, no medication is prescribed for spitting up. To help the child allow simple measures based on lifestyle changes and feeding.
. To improve the situation, it is recommended to feed the baby more often, avoiding oversaturation, best of all - on demand 5 . The AirFree valve prevents air from entering the baby's stomach. To allow air that has entered the digestive tract during meals to escape, it is important to keep the newborn upright for 10-20 minutes after feeding 4 . To reduce the negative impact of stomach acid on the esophagus, put your baby to sleep in a supine position. The side or prone position, which many pediatricians used to recommend, is no longer recommended. It was found to be associated with an increased risk of sudden infant death syndrome 5 . If parents notice alarming symptoms, such as spitting up too often or large volume, etc., it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy. 1 Zakharova I.
Every feeding, the mother must ensure that the baby does not swallow too much air during suckling. When sucking, there should be no loud, smacking, clicking sounds. You also need to control that the baby captures the nipple along with the areola.
If the newborn is bottle-fed and receiving formula, it is important to choose the right bottle and nipple. The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air New Anti-colic bottle with AirFree valve
References 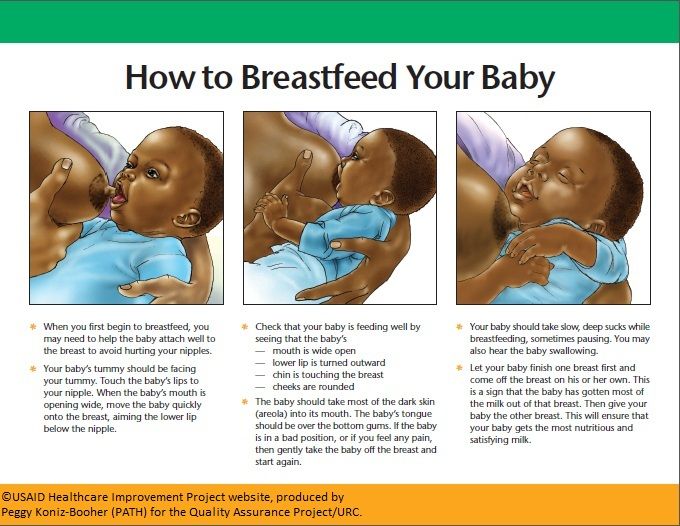 N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. Vol. 7. No. 4.
N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. Vol. 7. No. 4.
3 Zakharova IN Regurgitation and vomiting in children: what to do? //Pediatrics. Supplement to Consilium Medicum, 2009. No. 3. S. 58-67.
4 Zakharova I. N., Sugyan N. G., Pykov M. I. Regurgitation syndrome in young children: diagnosis and correction // Effective pharmacotherapy, 2014. No. 3. P. 18-28.
5 Vandenplas Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) //Journal of pediatric gastroenterology and nutrition.