Do i have to burp my baby after dream feed
How to Properly Dream Feed Your Baby
Skip to contentLearning how to dream feed baby is quite simple. Yay! Yet dream feeding is one of those terms that gets tossed around so much that everyone assumes that everyone else knows the exact meaning of the term. When you dig a little deeper, you see that people have WILDLY different definitions of the same exact term!
Last Updated Jan 27, 2021.
Photo Credit: Zach Lucero
So What Is a Dream Feed?
Just so everyone is on the same page…
A dream feed is when:
- a parent goes to their sleeping infant,
- picks them up to breastfeed
- or props them up either in their crib, or in a caregiver’s arms, to offer a bottle,
- feeds the child,
- and then puts them back down *asleep* without the baby ever having woken up.
A dream feed is NOT a dream feed if a child:
- opens their eyes at any point in the process,
- or if the feeding is in response to the baby waking up.
Generally speaking, a dream feed is done between the hours of about 9:30pm and 12:00am. Technically, if all other terms are met, but the feed is done outside of these hours, the feeding is still a dream feed.
The Right Age for Dream Feeding
Dream feeds are a great tool from birth (or a few weeks after, when babies are not quite so sleepy), through to when a baby is done being swaddled. It is very challenging to dream feed a baby, even a very young one, without waking them up if they are not swaddled. Generally speaking, it’s wise to stop dream feeding around 14–16 weeks of age. After this age, babies become a lot more awake and aware, and dream feeds tend to disrupt the rest of their overnight sleep.
Check out my Newborn Sleep Program!
Benefits of Dream Feeding
Let me first dispel a myth. A dream feed does not necessarily prevent a baby from waking up to eat at night. Although, sometimes it does work. I like dream feeds for young babies because I appreciate the “insurance policy” of extra calories at night. As long as a baby is young enough that the dream feed itself does not wake them, and fracture their remaining nighttime sleep, a dream feed can insure as many calories as possible during each 24-hour period.
As long as a baby is young enough that the dream feed itself does not wake them, and fracture their remaining nighttime sleep, a dream feed can insure as many calories as possible during each 24-hour period.
A gift to reflux-y babies!
Some babies respond beautifully to a dream feed. Especially those with reflux! From about 7pm on through to about 2 or 3am, the body is flooded with the hormone melatonin. Melatonin is responsible for many things. Chief amongst them is making the body feel drowsy, and relaxing the long muscles (abs, legs, and arms). Since the abdominal muscles are relaxed, it’s common for babies with a lot of reflux to tolerate a dream feed without spitting up. And even possibly negate the need to be burped, or held upright afterwards. I can speak to this from personal experience with my own extremely reflux-y, wholly unmedicated daughter. Since the concern for calorie intake is so high with reflux babies, dream feeds can be especially useful for them.
Burping After a Dream Feed
If you feel your sleeping baby needs to be burped, go ahead and attempt to burp them as you normally would during the day. Check in with your pediatrician to ask how long to attempt a burp before giving up and putting baby back to sleep.
Check in with your pediatrician to ask how long to attempt a burp before giving up and putting baby back to sleep.
The bottom line is that a dream feed done correctly can benefit baby AND parents by offering an extra dose of nutrition, while also possibly helping baby sleep! (Which means YOU can get more sleep too! Win!)
If you like staying in the know with the most up-to-date information, and learning everything you can about your little one’s sleep, please sign up for my newsletter using the button below!
Sign up for my newsletter!
So remember, to properly dream feed your baby…
- Enter their room (keeping it dark!), and prop baby up either in their crib, or your arms, and immediately start feeding them the breast or bottle.
- Dream feed between 9:30pm-12:30am (or whenever you are heading to bed yourself!)
- Baby should NOT wake up AT ALL during the entire feeding. (Baby should be put back down in bed just as asleep as they were when you starting the feeding.
 )
) - You should stop attempting dream feeds when baby starts to sleep unswaddled. (Or around 14-16 weeks old when these feeds can start to become disruptive to their nighttime sleep.)
If you want to learn everything I know about babies under 16 weeks, check out The Newborn Sleep Program. This program can help set up your newborn (and you) for the best possible sleep! And if your baby is older than 16 weeks old, and you’re looking for affordable, hands-on sleep training support, check out my online training series: The Baby Sleep Trainer Program + Support. Use the code DFbaby for 10% off either program.[/fusion_text][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]
Search for:
Articles by Age
Categories
- Naps
- Newborn
- Opinion
- Sleep FAQs
- Sleep Training
- Getting Started
- How To Be Successful
- Success Stories
- Troubleshooting
Dream Feeding for Babies — Heaven Sent Sleep
If you’ve been around the baby sleep world for a while, you might have heard the term “dream feeding. ”
”
This term was coined by The Baby Whisperer to describe a feeding you perform in the late evening hours while your baby is asleep. You simply rouse them gently enough that they take in a feeding before you go to bed, in order to improve their night sleep.
Babies will instinctually take in what they need during that feeding (either by breast or bottle).
If you have been wondering if a dream feeding is the answer to your infant’s night wakings, then this blog will cover all the information you need to try it out!
Some frequently asked questions we will cover are:
Is dream feeding necessary or effective?
How does dream feeding work?
How to dream feed/How to give a dream feeding/Dream feeding with breast or bottle feeding
How to start dream feeding?
How to stop dream feeding? When to stop dream feeding?
Is dream feeding safe or is dream feeding bad for baby?
Dream feed schedule
Burping when dream feeding
How much do you feed during a dream feed?
Dream feed pros and cons
How to wake a baby for the dream feed
Is dream feeding necessary or effective?
It certainly isn’t something you *have* to do and effectiveness really varies from child to child. It didn’t work with ANY of mine and actually made their sleep after the dream feeding WORSE. But it wouldn’t be a “thing” if it never worked for anyone.
It didn’t work with ANY of mine and actually made their sleep after the dream feeding WORSE. But it wouldn’t be a “thing” if it never worked for anyone.
It is certainly fine to try it a few times, at different ages, to see if it is something you want to continue doing!
How does dream feeding work?
Why would a dream feed work (or what is the theory behind it)? If your baby typically does a bedtime feeding around 7pm, then they may wake at 11pm, 12am, 1am to eat again. That means you may have only been asleep for an hour or 2 yourself!
By giving a feeding in the 10pm (or so) hour, you eliminate the waking out of true hunger and may allow baby to sleep longer (and you too)! In other words, it resets their feeding clock back to zero.
This essentially elongates the baby’s long stretch of sleep to align with parents so they are getting more sleep.
We are filling their tummy up before they have the chance to get hungry and wake you up in the middle of the night.
A dream feed can also be useful to temporarily implement when you begin sleep training. This way baby does not associate waking and crying with being fed. You can feed while they are asleep and comfort/soothe when they are awake.
Some may even consider this a tear-free way to night wean a little one.
Another way the term “dream feed” is used, is by bedsharing+breastfeeding moms. Most of the time a baby will only rouse a little bit, nurse, and fall back to sleep without waking and crying. Essentially they are eating in their sleep or very light sleep cycles.
You may find that the idea of the dream feed is more well known and popular than the actual results of the dream feed. It may even be the equivalent of an Urban Myth.
How to dream feed/How to give a dream feeding/Dream feeding with breast or bottle feeding
Ideally, we want the baby to stay asleep or doze during the dream feeding. Follow these steps to dream feed your little one:
Step one: Gently rouse your little one just enough that they latch onto the bottle or breast.
 They need to be alert enough to eat, but not so much that they wake up and are cranky. That could throw off the whole night!Some babies are roused enough just by taking them out of their sleeping space, others may need a little more!Pro tip: The best way to rouse them is to initiate the rooting reflex by stroking their cheek.
They need to be alert enough to eat, but not so much that they wake up and are cranky. That could throw off the whole night!Some babies are roused enough just by taking them out of their sleeping space, others may need a little more!Pro tip: The best way to rouse them is to initiate the rooting reflex by stroking their cheek.Step two: Feed the baby! Simple, right? Make sure their head is slightly elevated. If you’re having trouble getting them to latch, then they are not awake enough.
Do not give up! It may not work the first few times. Try to give it a consistent effort for a week before deciding if it works for your family.
It is important to note that there is very little (or none) evidence based research to prove whether a dream feed is effective or not. It is mostly anecdotal information.
How to start dream feeding?
If dream feeding is going to be effective, it’s usually at younger ages (think newborn to 4 months) though sometimes adding it later can work too! It really and truly is just an experiment since it isn’t an evidence based practice.
You can definitely introduce this concept at any age, however as a professional, I find it works best (if it is going to work) prior to 3-4 months of age when they already have multiple night feedings.
How to stop dream feeding? When to stop dream feeding?
It typically works best to try to wean the dream feeding before 6-9 months of age. After that, it can disrupt sleep even more than it helps.
Babies tend to become a lot more alert by that age and will fully wake up, wanting to play when you are trying to sneak in that extra feeding!
If you find that your little one is having a difficult time settling after you have done the dream feed, then that is usually a sign to stop the dream feed.
It is important to remember that this is a short term solution to night wakings and will eventually become a habit.
Some pediatricians will agree that babies do not need feedings in the night after 6 months of age, but every baby is different. so it's important to know what’s normal for night time wakings.
Since a dream feed is typically done to get a little one sleeping through the night, it is definitely best to check in with your pediatrician!
You will wait to drop the dream feeding until your baby is able to sleep from the dream feed to their normal morning wake up time, through any other night feedings.
You may choose to keep the dream feeding at that point, or you may want to wean it.
Once they are sleeping from the dream feeding to the morning wake up and have dropped any night feedings or early morning feedings, you will try to wait about 2 weeks before dropping the dream feed.
When you are ready to drop the feeding, you have a lot of options!
You could wean the amount of ounces you are feeding if you are bottle feeding (by ½ an ounce every second or third night; more if you are in a hurry)
You could wean the amount of time you are feeding if you are breastfeeding (so you would want to take note of how long the dream feed takes and then you can cut it by 1-2 minutes every second or third night)
You could also drop the feeding cold turkey and utilize a sleep training method to address any night wakings
The dream feed method book suggests dream feeding a newborn at 1 and 4am (give or take), and gradually moving those feedings earlier until you are down to one feeding and moving that one earlier until you no longer need it.
They also boast this will get your baby sleeping through the night by 4 months. As a professional, I believe this is a little bit ambitious, but if it helps families get more sleep (even if it does not mean sleeping through the night completely without feedings) then I am all for it!
As always, address this with your healthcare provider as they are able to assess your child’s growth and overall health!
It will also be easier to drop the dream feed if your child is already an independent sleeper at bedtime! Otherwise, when they wake up, they will need assistance getting back to sleep even if you are not feeding them.
Another important factor when working to drop a dream feed is to make sure you have a great day time routine.
This is important because:
This ensures they are getting an appropriate amount of sleep (so they are not waking because they are over or undertired at night)
Their nutritional needs are met (getting in nice, full feedings during the day and they are not skipping feeds)
Sets up their circadian rhythm/biological clock
Meeting their needs before they meltdown
A helpful practice to put into place is to offer soothing at every waking as opposed to feeding at every waking. You can implement a sleep training method (like pick up put down) or offer a pacifier and see if that soothes them back to sleep.
You can implement a sleep training method (like pick up put down) or offer a pacifier and see if that soothes them back to sleep.
Typically, you cannot soothe a hungry baby without a feeding! (No, this is not always the case so again, check in with your health care provider.)
It is also helpful to practice “le pause” for any wakings. If you are not familiar with “le pause”, you can read more about it here. Essentially, you stop, wait, and listen to what your child sounds like when they wake up.
If it is pretty mild fussing, grunting, etc and not full out crying, then you may be comfortable practicing that pause in order to let your little one settle back into their next sleep cycle.
If they are truly upset and need intervention, then you can step in for reassurance!
The worst case scenario with dropping the dream feed is that they continue to wake for it. In that case, you may choose to add it back in for a short period of time and try again later.
Pro tip: while introducing a dream feed, consider sizing up in diapers, using night time diapers, or inserting diaper booster pads as the extra intake may cause them to leak out of their diaper.
Is dream feeding safe or is dream feeding bad for baby?
Dream feeding is totally safe, when you feed just like you would during the day! It is not safe if you prop a bottle or feed the baby while they are lying flat as this is a choking hazard.
You also want to make sure you are alert while feeding your little one so that you do not risk falling asleep holding them while on an unsafe surface (like a recliner) or dropping them should you doze off.
To read more about safe sleep, check out this blog!
DREAM FEED SCHEDULEA dream feeding schedule would look something like:
6 or 7pm bedtime feeding
10 or 11pm dream feeding
3, 4, 5am night feeding (and this waking gets later and later as baby grows, develops their long stretch of sleep, and eventually sleeps through until their normal morning wake up!)
Without the dream feeding, it may look something like:
6 or 7pm bedtime feeding
12am night feeding
4am night feeding
Which means you are waking twice, instead of just once further fragmenting your night sleep as well as theirs.
Burping when dream feeding
Is it necessary to burp when dream feeding? Maybe! Burping is typically easier during the night when they are more relaxed. You will want to do this to avoid any discomfort waking your baby soon after you put them down.
This can also help to avoid them spitting up after the dream feeding. It is helpful to hold them upright for 10 or so minutes after the feeding to allow them time to digest, get the air out and relax back into a deeper sleep when you put them back down.
Some babies naturally take in less air during the dream feed because they are more relaxed. In this case, they may not burp but you should still try to get one out.
HOW MUCH DO YOU FEED DURING A DREAM FEEDING?There is no right or wrong answer to this one; you can do a small “snack” feeding of 2-3oz, you could do their normal 4-6oz, you could feed on one side if breastfeeding, or feed on both sides!
Some babies will only drink a tiny amount, some will take in the full feeding.
You know your baby best, so you can experiment and see what works!
DREAM FEED PROS AND CONSPros for the dream feeding:
Potentially extends their night sleep (and yours!)
Babies might sleep through with less disrupted sleep
Their sleep is hopefully more aligned with yours
May help a breastfeeding mom’s supply (or you could pump before you go to bed if you would rather and the dream feeding is not working!)
It can lessen the amount of time your baby cries by anticipating their need for food
Anticipates their need for food and takes the guesswork out of night wakings
Sleepy babies are cranky babies, so by ensuring baby wakes less frequently at night, baby may be less cranky during the day
For moms, knowing they may get a few extra hours of sleep instead of going to bed wondering when the next waking may be, will actually improve their sleep (even if it doesn’t actually work- kind of like a placebo effect)
May help baby avoid any pain associated with reflux after a feeding
If your little one is struggling with intake during the day, the night feed can get the extra calories in that they might have missed
Cons for the dream feeding:
You may have to stay up later to get it in
May not always work unfortunately (this means they may not sleep longer after it, or may wake more frequently because of it)
May disrupt their sleep (they may not go back to sleep easily after eating at that time)
Disrupts baby’s natural sleep cycle (and interrupts their most restorative sleep they will get during the night)
Can be difficult to drop it (it becomes habitual when we condition them to eating at that time)
Some will say this goes against “feeding on demand” and is forcing a meal on your little one they may not already want/need
It reinforces that food equals sleep, enforcing the brain and tummy connection.
 It just blows past feeding cues from our little ones
It just blows past feeding cues from our little ones It can overfill a baby’s tummy and cause sleep disruption plus gastrointestinal discomfort
According to care.com, “When baby becomes dependent on dream feeding, no learning is taking place, and it's possible that he'll lose his ability to suck purposely, says Potock. "My recommendation is to keep a balance between dream feeding and conscious suckling. That way, baby is soothed and comforted and may even fall asleep at the breast or toward the end of a bottle, but is still learning to suck-swallow-breathe with intention over time."
If your baby is having a hard time waking (just enough) to eat, then you can try a few different things:
You can try at a different time of the night. If your baby is in a deep sleep cycle, then you can wait until you see them in a light sleep cycle to feed; they may be easier to rouse at that point!
You can unswaddle them from the bottom and change their diaper (or use a Kyte BABY sleep bag which has a zipper at the bottom to make night time changes easier).
Rub a wet cloth or wet wipe on their cheek.
Tickle the bottom of their feet (annoying them just enough to get them to latch onto the bottle or breast).
Try changing the position you are holding baby in (switch sides for example).
Express some milk from the bottle or breast onto their lips; this may entice them to open their mouth enough to eat!
Pro tip: if you need light, use something soft, like a salt lamp. A salt lamp will not interrupt melatonin production which means you can go to sleep much easier after doing the dream feed.
“The great thing about babies is that they have a natural instinct to suck if they’re at a nipple,” says Jason Freedman, co-author of the book The Dream Feed Method.
Remember, this is a great way for dad to help out! If you are formula feeding, you can take shifts and dad can give the dream feed so that mom can get in a nice long stretch of sleep in the beginning of the night.
If you are breastfeeding, you could consider introducing a bottle, pumping some milk before you go to bed and allowing dad to give the bottle for the dream feeding-- again, giving mom a great long stretch of sleep!
For newly postpartum moms, sleep is so important! If you feel like you could be suffering from postpartum depression or anxiety, then use this list from the National Sleep Foundation to check in with yourself and see if the dream feed helps you rest better!
TAKEAWAYS ABOUT DREAM FEEDFirst, forget all the “rules.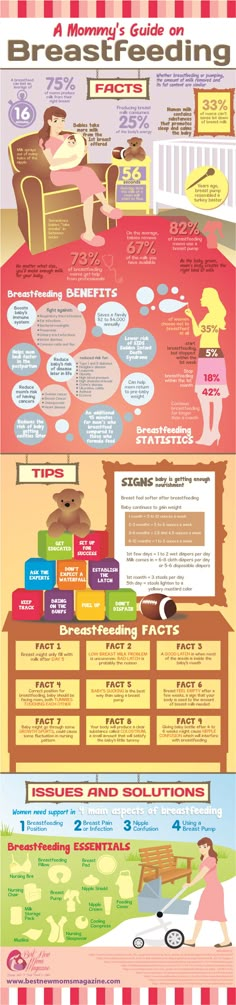 ” There are no hard and fast rules. You can try it at 9pm, 10pm, 11pm.
” There are no hard and fast rules. You can try it at 9pm, 10pm, 11pm.
You can swaddle or unswaddle. You can change their diaper or leave them as undisturbed as possible.
Do not panic if they wake up. Just keep the interactions low, lights down, and make it a relaxing feeding for you both.
Try not to stress if you attempt the dream feed and it does not work! It may not work right away and it is up to you if you would like to continue trying it, or let your baby lead the way with night feedings.
Either way is perfectly fine. Find what works for you and your baby! Do not get frustrated if it doesn’t work for your little one. There are a lot of other options out there to get you both better sleep!
We all know that new babies come with a certain level of sleep deprivation, and a dream feed can be one way to combat that.
There haven’t been any proper randomised, controlled studies into dream feeding so most of the pros and cons are based on anecdotal evidence and people’s opinions.
It definitely does not hurt to try it!
Best case, it buys you some extra hours of sleep and worse case, you wake at your normal feeding times.
How to help the baby when regulating
Support icon ofKeywords for searching
Home ›› How to help a child in sprinkling
Home Home ›!! how to help a child in regurgitation
↑ Verki
Breastfeed special time for mom and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagy. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
- Holding the child upright on your legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up during feeding.
 If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after. - When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.
Breastfeeding is a wonderful time to strengthen the bond between parent and baby. Every mom and every baby is different, so learning to help your newborn burp properly can take time and practice.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Preventive measures against regurgitation in children
08.03.2017
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes:
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile.
What causes physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed.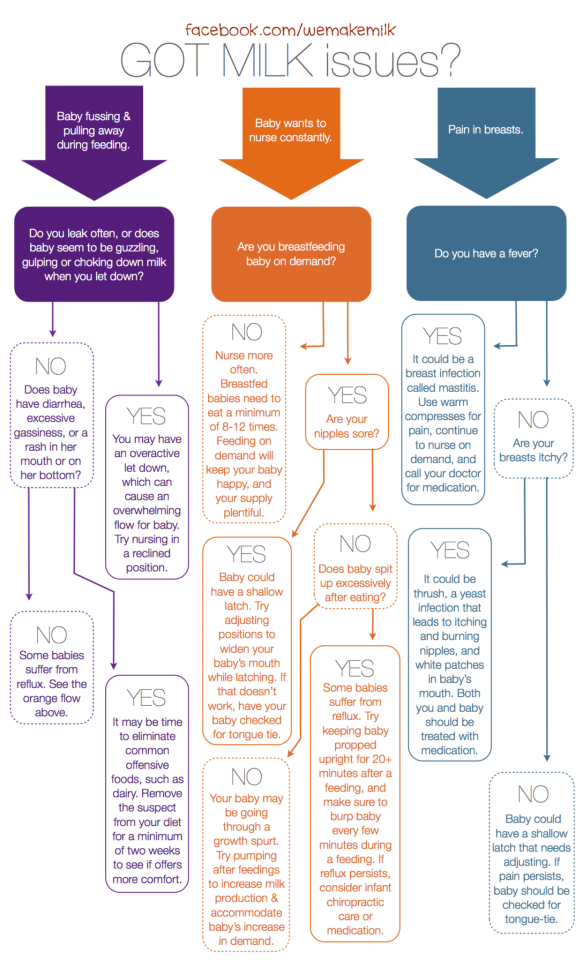 As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled.
-
Swallowing air during feeding (aerophagia).
 A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation.
A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm.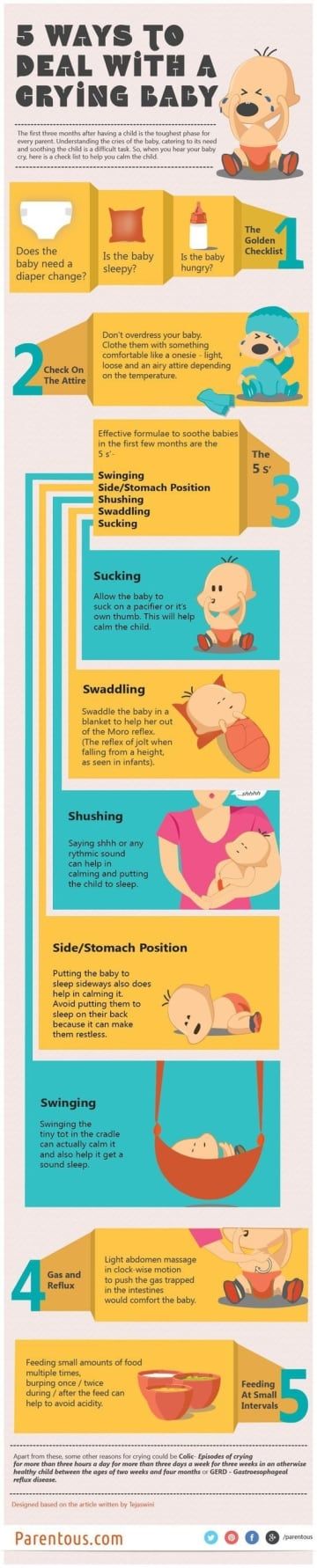 You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
Abnormal regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
-
increased intracranial pressure.
Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
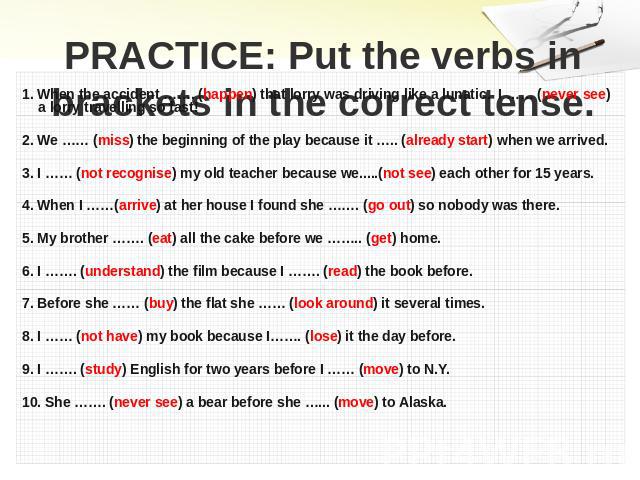
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case. It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air. Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again.
-
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency.