Feeding tubes for babies with reflux
Tube feeding - Part 1
What is it and why does it happen?
One of the lesser known (and obviously less frequent) consequences of severe gastroesophageal reflux disease (GORD) is the need to tube feed some children. Babies can learn very quickly that the act of feeding hurts and as a result will refuse to feed. Despite the notion that feeding should be instinctual, there are some instincts that take precedence, like preserving oxygen flow or avoiding pain. If stomach contents are being aspirated or are threatening to be aspirated into the lungs it can cause a child to instinctively protect their airways by pulling off the breast or bottle (often pulling their head sharply to the left to cut off the airways). Add pain into the mix and children will sometimes refuse to feed to the point where tube feeding is required. If your child is a feed refuser, tube feeding is not always the answer. Read our strategies and options for feed refusers.
What is tube feeding?
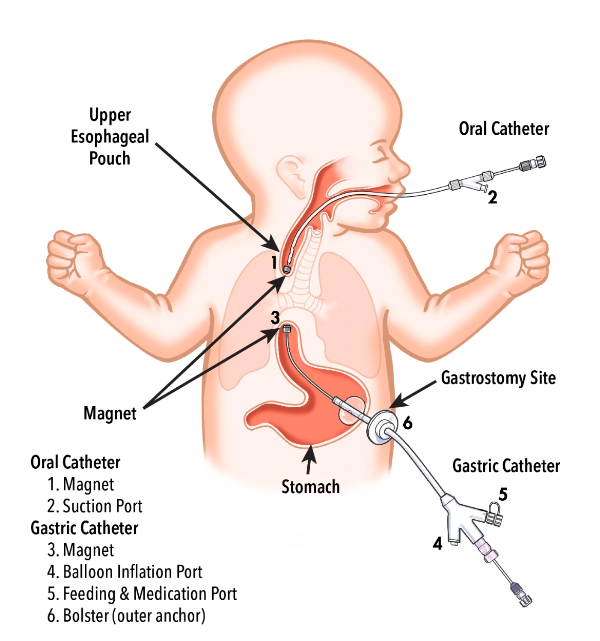
Tube feeding is where a small tube is passed either through the nose, down the oesophegus into the stomach called a nasal-gastric tube (NGT) or by gastric feeding where a small button is surgically placed through the abdominal wall directly into the stomach that will either permanently or periodically be attached to a tube through which feeds can be given. This is called a Percutaneous Endoscopic Gastrostomy (PEG). Ordinarily, a child will begin with a NGT until it becomes clear that tube feeding may be a longer term requirement, at which point a gastric tube will be considered. While the gastric tube sounds horrible, it does have advantages in that tape is not permanently affixed to the child’s face which is uncomfortable, inevitably irritates the skin and requires regular changing. Also, a gastric tube means that there’s no NGT running down the back of the child’s throat which can irritate and interfere with a child’s desire to eat – which is counter-productive in a child who is already feed averse.
A less common version of tube feeding is jejunal feeding known as a nasal jejunal tube (NJT) or jejunal tube (JT). This is where the tube is passed down either through the nose or through the abdominal wall the same way as above but the tube continues through the stomach to the second part of the intestine known as the jejunum. This means the tube has to pass through the pyloric sphincter and the deodenum (first part of the bowel) and feeds directly into the small intestine. It requires very delicate placement under x-ray usually and feeds must be given at a far slower rate due to the intestine not functioning as a receptacle in the same way the stomach can.
It requires very delicate placement under x-ray usually and feeds must be given at a far slower rate due to the intestine not functioning as a receptacle in the same way the stomach can.
How is a decision to commence tube feeding made?
Essentially, there are a couple of factors at play but as with all of these things, each case is different and your child’s specialists will make the decision based on best serving the needs of your particular child’s circumstances.
If the decision is being made on weight gain alone, it would generally be made where a considerable weight drop is demonstrated (over a few percentile bands) and where the child is not showing signs of being able to maintain their weight. Also, where a child’s weight is dangerously low to the point where they can’t maintain wet nappies or bowel movements or they appear to be fairly unresponsive and chronically malnourished.
A decision can also be made to tube feed where the airways are being significantly compromised by aspiration of stomach contents or an ineffective swallow that causes the child’s breathing to be critically (and often chronically) compromised. (These are obviously the reflux-related reasons for tube-feeding. There are, of course, other medical reasons for tube feeding.)
(These are obviously the reflux-related reasons for tube-feeding. There are, of course, other medical reasons for tube feeding.)
Why doctors don’t rush to tube feed
While the decision to put in a tube to feed a child is not one that any parent takes lightly, it can seem like the only solution to dealing with a child who is chronically feeding averse. The problem is that once a tube goes in, these children can fairly quickly become tube dependent. They are relieved by not having to feed and frequently the small level of feeding skills they already possess will be lost quite quickly. They will come to quickly rely on being fed by tube and be relieved at not having to go through the trauma of feeding so often or for as long.
This doesn’t happen with all children. Some children cope quite well with a tube, the tube is used to supplement their reasonable feeding skills and over a few months, the child is able to be weaned from the tube and resume a more normal feeding pattern.
What are the advantages of tube feeding?
It takes the fight away. Parents no longer need to battle their child at every meal (which can seem like all day, every day) and can concentrate on allowing them to play with food, experience new textures and sensations secure in the knowledge that if they actually don’t swallow anything, there’s another way of keeping them going. Surprisingly, it can be quite a relief for parents as well when a tube is placed. This will only seem like a normal response to those who have experienced it perhaps, but having fought your own child to feed continually just to keep them alive, having that pressure removed can be an immense relief.
Also, it allows you to concentrate on improving their feeding skills without the pressure of needing to get them to feed. They can chew on non-food items (like a rubber toothbrush) to experience a different texture without it needing to be associated with food – a good first step when needing to reintroduce a spoon for a child who’s scared of one.
Opinions to seek and options to explore before going down the tube feeding path
You may also wish to have your child assessed for a few other things that may be interfering with their desire to eat if time allows and commencing tube feeding is not strictly urgent. These include:
- lip or tongue ties (ABA page on lip & tongue ties)
- speech therapy assessment for swallow dysfunction
- allergy assessment by an immunologist – dairy, soy, gluten and other allergies and intolerances can cause gut pain and exacerbate feed refusal
- laryngomalacia particularly if stridor is present
- occupational therapy or speech therapy to assist with techniques in helping a child to feed
- lactation consultant to assess attachment and suck
- Ear Nose and Throat (ENT) specialist to assess whether enlarged tonsils, adenoids or other related ENT issues could be a causal factor
- Sleep specialist to assess whether there are any other causal factors at play (other than reflux) for disturbed sleep.

Conversations to consider before a tube is placed
Ask your medical team for a plan for the duration and removal of the tube:
- What are the circumstances under which the tube will be removed?
- What additional tests will be conducted to determine the cause of the child’s feeding aversion?
- When or has your child been assessed for:
- abnormal swallow
- abnormal gastric emptying
- lip or tongue ties
- constipation
- neurological issues
- food allergy or intolerance issues (or non-food related allergies)
- other physiologial causes eg hiatus hernia
Of course it is difficult for physicians to give you definite timeframes – they’re trying to find the answers too – but health systems are big and you don’t want your child getting lost in one because you assume people are thinking through the broad range of possible causes when they’re not. There are many variables for different children but it isn’t OK to place a tube with no plan to work towards removal unless there is evidence that it will be a long term requirement.
Remember: you are your child’s voice. You have to be your child’s advocate. If you are not a RISA member and you are on the cusp of tube feeding, we cannot recommend highly enough that you join. It will give you access to other parents who have been through this and can help you be the best advocate you can for your child.
Part 2 to this article coming soon and will deal with managing a child on a feeding tube.
Author: Joanne Matthews, RISA President.
Reviewed: Bianca Willis, BScience (Biomedical & Psychology), RISA Secretary
Last reviewed: March 2014
Back to March ’14 Newsletter
GERD (Gastroesophageal Reflux Disease) in Children
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is GERD in children?
GERD, or gastroesophageal reflux disease, is a long-term (chronic) digestive disorder. It happens when stomach contents flow back up (reflux) into the food pipe (esophagus) and cause symptoms or problems.
It happens when stomach contents flow back up (reflux) into the food pipe (esophagus) and cause symptoms or problems.
GERD is a more serious and long-lasting form of gastroesophageal reflux (GER).
GER is common in babies under 2 years old. Most babies spit up a few times a day during their first 3 months. GER does not cause any problems in babies. In most cases, babies outgrow this by the time they are 12 to 14 months old.
It is also common for children and teens ages 2 to 19 to have GER from time to time. This doesn’t always mean they have GERD.
When GER becomes GERD
Your baby, child, or teen may have GERD if:
- Your baby’s symptoms prevent him or her from feeding. These symptoms may include vomiting, gagging, coughing, and trouble breathing.
- Your baby has GER for more than 12 to 14 months
- Your child or teen has GER more than 2 times a week, for a few months
What causes GERD in a child?
GERD is often caused by something that affects the LES, the lower esophageal sphincter. The LES is a muscle at the bottom of the food pipe (esophagus). The LES opens to let food into the stomach. It closes to keep food in the stomach. When the LES relaxes too often or for too long, stomach acid flows back into the esophagus. This causes vomiting or heartburn.
The LES is a muscle at the bottom of the food pipe (esophagus). The LES opens to let food into the stomach. It closes to keep food in the stomach. When the LES relaxes too often or for too long, stomach acid flows back into the esophagus. This causes vomiting or heartburn.
Everyone has reflux from time to time. If you have ever burped and had an acid taste in your mouth, you have had reflux. Sometimes the LES relaxes at the wrong times. Often your child will just have a bad taste in his or her mouth. Or your child may have a short, mild feeling of heartburn.
Babies are more likely to have a weak LES. This makes the LES relax when it should stay shut. As food or milk is digesting, the LES opens. It lets the stomach contents go back up to the esophagus. Sometimes the stomach contents go all the way up the esophagus. Then the baby or child vomits. In other cases, the stomach contents only go part of the way up the esophagus. This causes heartburn or breathing problems. In some cases there are no symptoms at all.
Some foods seem to affect the muscle tone of the LES. They let the LES stay open longer than normal. These foods include:
- Chocolate
- Peppermint
- High-fat foods
Other foods can bring on symptoms because they are acidic. These foods include:
- Citrus foods
- Tomatoes and tomato sauces
Other things that may lead to GERD include:
- Being obese
- Medicines, including some antihistamines, antidepressants, and pain medicines
- Being around secondhand smoke
Which children are at risk for GERD?
GERD is very common during a baby’s first year of life. It often goes away on its own. Your child is more at risk for GERD if he or she has:
- Down syndrome
- Neuromuscular disorders such as muscular dystrophy and cerebral palsy
What are the symptoms of GERD in a child?
Heartburn, or acid indigestion, is the most common symptom of GERD. Heartburn is described as a burning chest pain. It begins behind the breastbone and moves up to the neck and throat. It can last as long as 2 hours. It is often worse after eating. Lying down or bending over after a meal can also lead to heartburn.
Heartburn is described as a burning chest pain. It begins behind the breastbone and moves up to the neck and throat. It can last as long as 2 hours. It is often worse after eating. Lying down or bending over after a meal can also lead to heartburn.
Children younger than age 12 will often have different GERD symptoms. They will have a dry cough, asthma symptoms, or trouble swallowing. They won’t have classic heartburn.
Each child may have different symptoms. Common symptoms of GERD include:
- Burping or belching
- Not eating
- Having stomach pain
- Being fussy around mealtimes
- Vomiting often
- Having hiccups
- Gagging
- Choking
- Coughing often
- Having coughing fits at night
Other symptoms may include:
- Wheezing
- Getting colds often
- Getting ear infections often
- Having a rattling in the chest
- Having a sore throat in the morning
- Having a sour taste in the mouth
- Having bad breath
- Loss or decay of tooth enamel
GERD symptoms may seem like other health problems. Make sure your child sees his or her healthcare provider for a diagnosis.
Make sure your child sees his or her healthcare provider for a diagnosis.
How is GERD diagnosed in a child?
Your child's healthcare provider will do a physical exam and take a health history. Other tests may include:
- Chest X-ray. An X-ray can check for signs that stomach contents have moved into the lungs. This is called aspiration.
- Upper GI series or barium swallow. This test looks at the organs of the top part of your child’s digestive system. It checks the food pipe (esophagus), the stomach, and the first part of the small intestine (duodenum). Your child will swallow a metallic fluid called barium. Barium coats the organs so that they can be seen on an X-ray. Then X-rays are taken to check for signs of sores or ulcers, or abnormal blockages.
- Endoscopy. This test checks the inside of part of the digestive tract.
 It uses a small, flexible tube called an endoscope. It has a light and a camera lens at the end. Tissue samples from inside the digestive tract may also be taken for testing.
It uses a small, flexible tube called an endoscope. It has a light and a camera lens at the end. Tissue samples from inside the digestive tract may also be taken for testing. - Esophageal manometry. This test checks the strength of the esophagus muscles. It can see if your child has any problems with reflux or swallowing. A small tube is put into your child’s nostril, then down the throat and into the esophagus. Then it measures the pressure that the esophageal muscles make at rest.
- pH monitoring. This test checks the pH or acid level in the esophagus. A thin, plastic tube is placed into your child’s nostril, down the throat, and into the esophagus. The tube has a sensor that measures pH level. The other end of the tube outside your child’s body is attached to a small monitor. This records your child’s pH levels for 24 to 48 hours. During this time your child can go home and do his or her normal activities.
 You will need to keep a diary of any symptoms your child feels that may be linked to reflux. These include gagging or coughing. You should also keep a record of the time, type of food, and amount of food your child eats. Your child’s pH readings are checked. They are compared to your child’s activity for that time period.
You will need to keep a diary of any symptoms your child feels that may be linked to reflux. These include gagging or coughing. You should also keep a record of the time, type of food, and amount of food your child eats. Your child’s pH readings are checked. They are compared to your child’s activity for that time period. - Gastric emptying study. This test is done to see if your child’s stomach sends its contents into the small intestine properly. Delayed gastric emptying can cause reflux into the esophagus.
How is GERD treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Diet and lifestyle changes
In many cases, diet and lifestyle changes can help to ease GERD. Talk with your child’s healthcare provider about changes you can make. Here are some tips to better manage GERD symptoms.
For babies:
- After feedings, hold your baby in an upright position for 30 minutes.
- If bottle-feeding, keep the nipple filled with milk. This way your baby won’t swallow too much air while eating. Try different nipples. Find one that lets your baby's mouth make a good seal with the nipple during feeding.
- Adding rice cereal to feeding may be helpful for some babies.
- Burp your baby a few times during bottle-feeding or breastfeeding. Your child may reflux more often when burping with a full stomach.
For children:
- Watch your child's food intake. Limit fried and fatty foods, peppermint, chocolate, drinks with caffeine such as sodas and tea, citrus fruit and juices, and tomato products.
- Offer your child smaller portions at mealtimes. Add small snacks between meals if your child is hungry. Don’t let your child overeat. Let your child tell you when he or she is hungry or full.
- If your child is overweight, contact your child’s provider to set weight-loss goals.

- Serve the evening meal early, at least 3 hours before bedtime.
Other things to try:
- Ask your child's provider to review your child’s medicines. Some may irritate the lining of the stomach or esophagus.
- Don’t let your child lie down or go to bed right after a meal.
- Always check with your baby’s provider before raising the head of the crib if he or she has been diagnosed with gastroesophageal reflux. Place all babies, including babies with GERD, on their backs for all sleeping until they are 1-year-old. This is for safety reasons and to reduce the risk for SIDS and other sleep-related infant deaths.
Medicines and other treatments
Your child’s healthcare provider may also recommend other options.
Medicines. Your child's provider may prescribe medicines to help with reflux. There are medicines that help reduce the amount of acid the stomach makes. This reduces the heartburn linked to reflux. These medicines may include:
This reduces the heartburn linked to reflux. These medicines may include:
- h3-blockers. These reduce the amount of acid your stomach makes by blocking the hormone histamine. Histamine helps to make acid.
- Proton pump inhibitors. These help keep your stomach from making acid. They do this by stopping the stomach's acid pump from working.
The provider may prescribe another type of medicine that helps the stomach empty faster if it's clear that your child has a stomach-emptying delay. If food doesn’t stay in the stomach as long as normal, reflex may be less likely to occur.
Calorie supplements. Some babies with reflux can’t gain weight because they vomit often. If this is the case, your child's healthcare provider may suggest:
- Adding rice cereal to baby formula
- Giving your baby more calories by adding a prescribed supplement
- Changing formula to milk- or soy-free formula if your baby may have an allergy
Tube feedings. In some cases tube feedings may be recommended. Some babies with reflux have other conditions that make them tired. These include congenital heart disease or being born too early (premature). These babies often get sleepy after they eat or drink a little. Other babies vomit after having a normal amount of formula. These babies do better if they are constantly fed a small amount of milk. In both of these cases, tube feedings may be suggested. Formula or breastmilk is given through a tube that is placed in the nose. This is called a nasogastric tube. The tube is then put through the food pipe or esophagus, and into the stomach. Your baby can have a tube feeding in addition to a bottle feeding. Or a tube feeding may be done instead of a bottle feeding. There are also tubes that can be used to go around, or bypass, the stomach. These are called nasoduodenal tubes.
In some cases tube feedings may be recommended. Some babies with reflux have other conditions that make them tired. These include congenital heart disease or being born too early (premature). These babies often get sleepy after they eat or drink a little. Other babies vomit after having a normal amount of formula. These babies do better if they are constantly fed a small amount of milk. In both of these cases, tube feedings may be suggested. Formula or breastmilk is given through a tube that is placed in the nose. This is called a nasogastric tube. The tube is then put through the food pipe or esophagus, and into the stomach. Your baby can have a tube feeding in addition to a bottle feeding. Or a tube feeding may be done instead of a bottle feeding. There are also tubes that can be used to go around, or bypass, the stomach. These are called nasoduodenal tubes.
Surgery. In severe cases of reflux, surgery called fundoplication may be done.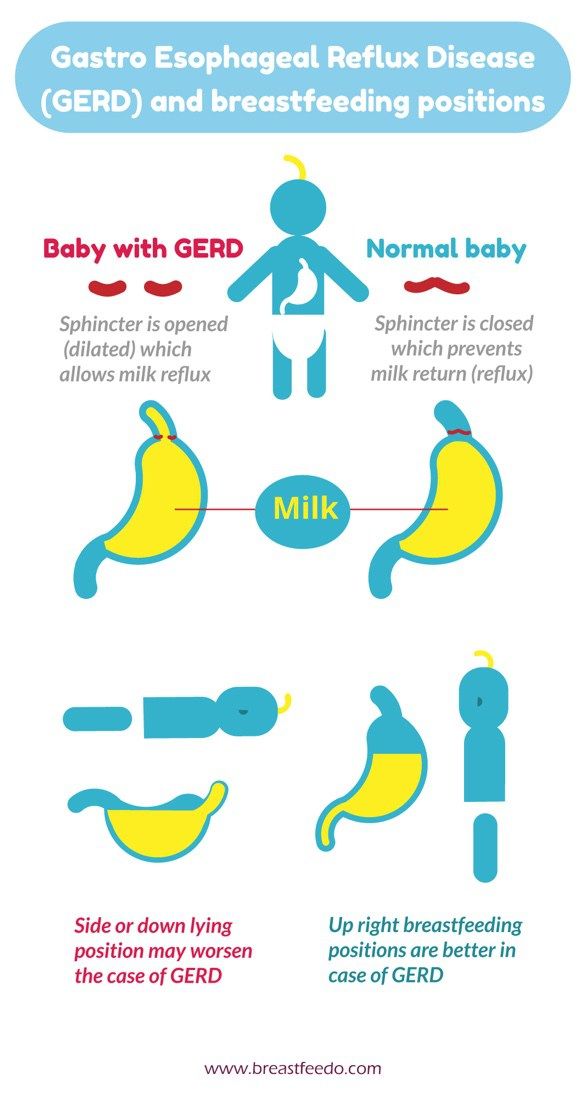 Your baby’s provider may recommend this option if your child is not gaining weight because of vomiting, has frequent breathing problems, or has severe irritation in the esophagus. This is often done as a laparoscopic surgery. This method has less pain and a faster recovery time. Small cuts or incisions are made in your child’s belly. A small tube with a camera on the end is placed into one of the incisions to look inside. The surgical tools are put through the other incisions. The surgeon looks at a video screen to see the stomach and other organs. The top part of the stomach is wrapped around the esophagus. This creates a tight band. This strengthens the LES and greatly decreases reflux.
Your baby’s provider may recommend this option if your child is not gaining weight because of vomiting, has frequent breathing problems, or has severe irritation in the esophagus. This is often done as a laparoscopic surgery. This method has less pain and a faster recovery time. Small cuts or incisions are made in your child’s belly. A small tube with a camera on the end is placed into one of the incisions to look inside. The surgical tools are put through the other incisions. The surgeon looks at a video screen to see the stomach and other organs. The top part of the stomach is wrapped around the esophagus. This creates a tight band. This strengthens the LES and greatly decreases reflux.
What are the complications of GERD in a child?
Some babies and children who have GERD may not vomit. But their stomach contents may still move up the food pipe (esophagus) and spill over into the windpipe (trachea). This can cause asthma or pneumonia.
The vomiting that affects many babies and children with GERD can cause problems with weight gain and poor nutrition. Over time, when stomach acid backs up into the esophagus, it can also lead to:
Over time, when stomach acid backs up into the esophagus, it can also lead to:
- Inflammation of the esophagus, called esophagitis
- Sores or ulcers in the esophagus, which can be painful and may bleed
- A lack of red blood cells, from bleeding sores (anemia)
Adults may also have long-term problems from inflammation of the esophagus. These include:
- Narrowing, or stricture, of the esophagus
- Barrett’s esophagus, a condition where there are abnormal cells in the esophageal lining
How can I help my child live with GERD?
Many babies who vomit outgrow it by the time they are about 1 year old. This happens as the LES gets stronger. For other children, taking medicines and making lifestyle and diet changes can reduce reflux, vomiting, and heartburn.
When should I call my child's healthcare provider?
Call you child's healthcare provider if your baby or child:
- Has reflux and is not gaining weight
- Has signs of asthma or pneumonia.
 These include coughing, wheezing, or trouble breathing.
These include coughing, wheezing, or trouble breathing. - Has vomiting that continues or is vomiting blood
Key points about GERD in children
- GERD is a long-term (chronic) digestive disorder.
- It happens when stomach contents come back up into the food pipe (esophagus).
- Heartburn or acid indigestion is the most common symptom of GERD.
- Vomiting can cause problems with weight gain and poor nutrition.
- In many cases, GERD can be eased by diet and lifestyle changes.
- Sometimes medicines, tube feedings, or surgery may be needed.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests.
 Also write down any new instructions your provider gives you for your child.
Also write down any new instructions your provider gives you for your child. - Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Feeding through a tube and gastrostomy
The article describes the types of gastrostomy, the care of these devices, as well as the rules for feeding a child with SMA through a gastrostomy.
Who needs a gastrostomy?
In palliative pediatrics, a gastrostomy may be placed for a variety of reasons. For example, if a child eats very little and cannot overpower all the necessary amount of food and water, because of this, he does not gain weight, does not grow, and is dehydrated. Or if one feeding takes a long time (for example, one and a half hours), and 5-6 such meals are needed per day. Or if the child does not swallow well and choke, there is a danger of throwing into the respiratory tract and the development of aspiration pneumonia.
If the above conditions are temporary, a nasogastric tube is placed. If it continues for more than 4-8 weeks without a clear improvement, the need and possibility of installing a gastrostomy should be discussed.
Why can't the probe stand for more than two months?
Prolonged use of a nasogastric tube can lead to various complications: bedsores, infections of the paranasal sinuses, eyes, ear from the side of the probe, reflux of stomach contents into the esophagus, oral cavity and lungs due to a partially open esophageal-gastric opening, aspiration pneumonia. In addition, a rigid probe can permanently injure the gastric mucosa and even cause erosive-ulcerative changes or gastric bleeding in the patient.
In addition, a rigid probe can permanently injure the gastric mucosa and even cause erosive-ulcerative changes or gastric bleeding in the patient.
What is a gastrostomy
A gastrostomy is an opening in the abdominal cavity through which a special tube is inserted that connects the outer surface of the abdominal wall and the inner surface of the stomach. This tube is the device through which the child can receive food and water in the right amount and not experience any problems with nutrition and the presence of fluid in the body.
Types of gastrostomy
Photo by Pixabay.com
Balloon and bumper gastrostomy tubes available. All gastrostomies have a range of sizes and diameters, so each child can choose the most suitable one.
Gastrostomy balloon tubes vary in length. Some have a long "tail", others do not have it and are called "low profile". For feeding, a special "tail" is attached to the low-profile gastrostomy tube - an extension for attaching a syringe or feeding system.
The balloon gastrostomy has one important advantage. You can change it yourself at home without anesthesia. Therefore, if the disease progresses in a child, and parents are thinking about how the child will withstand anesthesia next time, then you need to think about a balloon tube.
The bumper gastrostomy also has its advantages. For example, it is cheaper, it can be delivered for one and a half to two years or more. If the child has hope for an improvement in his condition, then you can put a bumper. Or, on the contrary, there are children with severe scoliosis and difficulties in installing a balloon. They may be shown the installation of a bumper gastrostomy tube.
In any case, the type of gastrostomy tube should be chosen together with the doctor, taking into account the characteristics of the child.
Photo by Pixabay.com
Gastrostomy feeding
Proper gastrostomy feeding requires boiled water and body temperature food (special food, homogenized porridge or milk formula). The main requirement for food is a liquid consistency, the absence of fibers and lumps, so as not to clog the gastrostomy tube.
The main requirement for food is a liquid consistency, the absence of fibers and lumps, so as not to clog the gastrostomy tube.
From the equipment - two syringes (for food and for water). All things must be clean, they must be prepared in advance and put on a diaper or towel.
If the child has a tail type gastrostomy tube, we feed through it. If it is low profile, you cannot feed directly through it, you must first attach the extension cord.
Next, you need to open the "tail" or extension and insert a syringe into it.
If it is a Janet syringe, then you insert it into the wide part of the gastrostomy tube or extension.
Photos from open sources
For medicines or liquids, a Luer type syringe is used, but the volume of the syringe must be at least 10 ml. Otherwise, the gastrostomy tube can be damaged by the increased pressure created by the smaller syringe. A Luer-type syringe is inserted into the narrow spout of a gastrostomy tube or extension. Do not confuse it with the exit point for refilling the cylinder.
Do not confuse it with the exit point for refilling the cylinder.
Photos from open sources
If the food being filled into the syringe has a thick consistency, then a syringe with a wide nozzle of the Genet type and a wide opening on the gastrostomy tube is used.
Before you start feeding, you need to open the tube itself to check how much food is left in the stomach after the last feeding. And, if there is air, then let it out. If everything is done correctly, then the tube will contain either clear, yellowish, gastric juice, or nothing at all if the child has digested everything.
Next, rinse the gastrostomy tube itself (minimum 10 ml of water), draw up the mixture into the syringe and inject it very slowly into the gastrostomy tube. The minimum feeding time is 15-20 minutes, otherwise reflux, vomiting or belching may occur after eating. If necessary, the feeding time can be increased up to 40 minutes, an hour, etc.
For convenience, it is better to use conventional syringe pumps, infusion pumps, gravity systems for feeding and water. Or equipment that is specifically designed for feeding. This allows you to free up time and hands of those who are nursing, and the child can even walk in a stroller on the street.
Or equipment that is specifically designed for feeding. This allows you to free up time and hands of those who are nursing, and the child can even walk in a stroller on the street.
Any gastrostomy insertion should be painless for the child and should not cause any discomfort.
After feeding, it is necessary to take a syringe with boiled water at body temperature (36-37 degrees) and rinse the gastrostomy tube from food. The volume of liquid depends on the age of the child and how he tolerates the volume of liquid. If he is less than a year old, then, as a rule, 10-20 ml are used, if the child is large and he tolerates a sufficient volume of liquid - 30-40 ml.
Flushing is needed to prevent clogging of the tube: food debris is removed from the inside of the tube and from the outside of the stomach. Rinsing should also be done slowly. After that, the gastrostomy tube is closed and wiped with a clean cloth.
Low profile gastrostomy tube feeding has its own challenges.
First fill the empty extension tube with water to prevent air from entering the stomach. To do this, attach the syringe, open the clamp on the extension, fill the extension with water, close the clamp, attach the extension to the gastrostomy tube, open the clamp and flush the tube, close the clamp, attach the syringe or feeding system, open the clamp.
Further feeding is carried out as described above.
After finishing feeding, flush the gastrostomy tube through the extension (see above), closing the clamp when disconnecting the feeding system, attaching the extension to the syringe, disconnecting the extension from the gastrostomy. The clamp closes to prevent the contents of the extension from spilling out. Close the gastrostomy tube.
Any gastrostomy insertion should be painless for the child and should not cause any discomfort.
What can not be done when feeding through a gastrostomy?
Do not use inhomogeneous (non-homogeneous) mixtures for feeding through the gastrostomy tube. Sometimes parents try to grind something on a blender: meat, potatoes, vegetables, and feed the child, if it is an inhomogeneous mixture of an unnecessary consistency, then it can clog the tube, and you will have to change it to a new one. If there is a balloon tube, then replacing it is quite simple. If bumper, then you have to change under anesthesia in the hospital.
Sometimes parents try to grind something on a blender: meat, potatoes, vegetables, and feed the child, if it is an inhomogeneous mixture of an unnecessary consistency, then it can clog the tube, and you will have to change it to a new one. If there is a balloon tube, then replacing it is quite simple. If bumper, then you have to change under anesthesia in the hospital.
Do not fill the balloon with various liquids that contain salts, medicines, do not fill with air, because the balloon will deflate too quickly. You must use boiled or distilled (purified water, practically free of impurities and impurities. Obtained by distillation in special apparatus) water.
How to give medication through the gastrostomy?
If medicine is to be given to a child, it must be in liquid form. There are special preparations intended for use through a gastrostomy tube - solutions, syrups, suspensions. If there is no such form, you need to crush the tablet and inject it through the tube, you must be sure that this tablet-water mixture will not clog it. There are drugs that are contained in a capsule in the form of granules. And these granules can settle on the tube wall and clog it. Such drugs cannot be used and cannot be picked out of the tube. If a blockage occurs, you should try to rinse the tube with boiled water, but in no case pick out the granules and do not try to break through the cork with some sharp object.
There are drugs that are contained in a capsule in the form of granules. And these granules can settle on the tube wall and clog it. Such drugs cannot be used and cannot be picked out of the tube. If a blockage occurs, you should try to rinse the tube with boiled water, but in no case pick out the granules and do not try to break through the cork with some sharp object.
The article was prepared on the basis of a video clip by a pediatrician, Ph.D. director for methodological work Natalya Nikolaevna Savva of the Children's Palliative Charitable Foundation “Feeding through a gastrostomy. Helping parents."
This material is for informational purposes only and cannot serve as advertising. Recommendations regarding the individual use of any drug or treatment should be obtained from your doctor.
Feeding through a gastrostomy. To help parents - Pro Palliative
PRO PALLIATIV uses cookies for statistics and analytics to make this website as user-friendly as possible. By staying on the site, you confirm your consent to the use of cookies.
By staying on the site, you confirm your consent to the use of cookies.
Based on a video from the SMA Families Foundation, this article explains the types of gastrostomy, how to care for them, and how to feed a child with SMA through a gastrostomy.
Who needs a gastrostomy?
Gastrostomy is usually placed if the child eats very little, and one feeding takes an hour and a half, and 5-6 meals are needed per day. As a result, such children do not grow, do not develop, and in order to avoid such a scenario, they need special devices for nutrition - a gastrostomy or a nasogastric tube.
A gastrostomy is also needed for a child with a swallowing problem if the problem persists for more than four to eight weeks, as placing the tube for such a long period may cause additional problems for a patient with a swallowing problem.
Gastrostomy is needed for children with SMA, as well as children after serious injuries, with organic damage to the central nervous system, or with impaired patency of the esophagus.
Why can't the probe stand for more than two months?
Prolonged use of a nasogastric tube can lead to various complications: bedsores, infections of the paranasal sinuses, eye, ear from the side of the probe, reflux of stomach contents into the esophagus, mouth and lungs due to a partially open esophageal-gastric opening, aspiration pneumonia. In addition, a rigid probe can permanently injure the mucosa and even cause erosive-ulcerative changes or gastric bleeding in the patient.
What is a gastrostomy
A gastrostomy is an opening in the abdominal cavity through which a special tube is inserted: it connects the outer surface of the abdominal wall and the inner surface of the stomach. Through this device, the child can receive food and water in the right amount and not experience any problems with nutrition and the presence of fluid in the body.
Nutrition for spinal muscular atrophy: brochure excerpt Evaluation of nutrition in children with SMA, tube feeding considerations, formula selection
Gastrostomy types
There are two types of gastrostomy: bumper and used allon . They differ in devices that are inside the stomach of a child: if it is a balloon gastrostomy, then in the stomach there is a balloon, if it is a bumper one, then a bumper that does not deflate or swell. A balloon gastrostomy is usually installed for six months, a bumper gastrostomy for a longer period.
They differ in devices that are inside the stomach of a child: if it is a balloon gastrostomy, then in the stomach there is a balloon, if it is a bumper one, then a bumper that does not deflate or swell. A balloon gastrostomy is usually installed for six months, a bumper gastrostomy for a longer period.
Both devices are very gentle, they do not injure the child's gastric mucosa.
The balloon gastrostomy has one advantage: you can change it yourself at home, without anesthesia. Therefore, if the child's disease progresses, and parents think about how he will withstand anesthesia next time, then it is better to put a balloon.
Balloon Gastrostomy
The Bumper Gastrostomy also has its advantages. It is installed if there is hope for an improvement in the child's condition - a bumper gastrostomy can be placed for one and a half to two years.
Doctor Natalia Savva demonstrates a bumper gastrostomy
In any case, the choice of gastrostomy type should be made together with the doctor, taking into account the child's condition.
Gastrostomy also differ in length. Some have a long "tail", others do not and are called " low profile ". For feeding, a special "tail" - a tube - is attached to the low-profile gastrostomy.
Gastrostomy feeding
Proper gastrostomy feeding requires:
- boiled water,
- special food/porridge/milk formula,
- two syringes (for food and for water).
All of these items must be clean, prepared in advance and placed on a diaper or towel.
All nutrition must pass through the gastrostomy tube.
You need to open the gastrostomy tube and insert a syringe into it. If it is Janet's syringe, then you insert it into the wide part of the gastrostomy tube.
Syringe Janet
A Luer-type syringe is used for drugs or liquids, but the volume of the syringe must be at least 10 ml, otherwise the gastrostomy may be damaged.
Luer Syringe
If the food being filled into the syringe has a thick consistency, a syringe with a wide nose and a wide opening on the gastrostomy tube is used.
Place the baby horizontally before feeding. Before starting to feed, it is necessary, by opening the tube itself, to check how much food is left in the stomach after the last feeding. And, if there is air, then let it out. If everything is done correctly, then the tube will contain either clear, yellowish, gastric juice, or nothing at all if the child has digested everything.
Then rinse the gastrostomy tube with 10 ml of water, draw up the puree or mixture into a syringe and inject it very slowly into the gastrostomy tube so that the child with SMA has time to digest it. The minimum feeding time is 15-20 minutes, otherwise reflux or belching may occur after eating. If necessary, you can enter food in 40 minutes, but in this case it is better to use special syringe pumps or pumps.
Important
Any insertion through the gastrostomy tube should be painless for the child and should not cause any discomfort.
After feeding, it is necessary to fill the syringe with boiled water at body temperature (36-37 degrees) - always check that the water is neither hot nor very cold. After that, air is released from the syringe, it is inserted into the gastrostomy tube, and flushing with the required volume of fluid begins.
After that, air is released from the syringe, it is inserted into the gastrostomy tube, and flushing with the required volume of fluid begins.
The amount of fluid depends on the age of the child. If he is less than a year old, then 10-12 milliliters will suffice; if the baby is large and tolerates a sufficient amount of fluid, then up to 40 milliliters can be administered after feeding.
Spinal muscular atrophy (SMA): what is it? SMA is a rare genetic disease requiring the involvement of palliative care professionals. What degrees of SMA are, what each characterizes, what equipment patients need - read in article
the device will always be passable and will not clog. Rinsing should also be done slowly. After that, the gastrostomy tube is closed and wiped with a clean cloth moistened with boiled water.We talked about the care of the gastrostomy in detail in the video instructions.
If the device has an extension set, the feeding procedure changes slightly. First you need to fill the tube itself with water so that there is no air in it and air does not enter the stomach. The water-filled tube is then inserted into the gastrostomy tube. Then food is introduced very slowly (at least 20 minutes). After the end of feeding, you need to click everything again, disconnect the syringe and close the gastrostomy. Then the extension tube is washed with a small amount of water (10-20 milliliters). After that, you can close the tube and disconnect, and close the gastrostomy itself.
First you need to fill the tube itself with water so that there is no air in it and air does not enter the stomach. The water-filled tube is then inserted into the gastrostomy tube. Then food is introduced very slowly (at least 20 minutes). After the end of feeding, you need to click everything again, disconnect the syringe and close the gastrostomy. Then the extension tube is washed with a small amount of water (10-20 milliliters). After that, you can close the tube and disconnect, and close the gastrostomy itself.
What should not be done when feeding through a gastrostomy?
Do not use inhomogeneous formulas for feeding through the gastrostomy tube. Sometimes parents try to grind something on a blender - meat, potatoes, vegetables - and feed the child. But if it is an inhomogeneous mixture that does not have the desired consistency, it may clog the tube and have to be changed. If there is a balloon tube, then replacing it is quite simple, and the bumper tube will have to be changed in a hospital under anesthesia.
Important
Do not fill the balloon with various liquids that contain salts, medicines, do not fill it with air, because the balloon will deflate too quickly. You should use boiled or distilled purified water that is practically free of impurities and foreign matter.
How to give medication through the gastrostomy?
If medicine is to be given to a child, it must be in liquid form. There are special preparations intended for administration through a gastrostomy tube - solutions, syrups, suspensions. If this form is not available, crush the tablet and inject it through the tube, making sure that this mixture of tablet and water does not clog the tube.
By the way, you can read about how parents can get medicines for their child free of charge here. Anna Povalikhina, legal adviser of the Vera Foundation, tells.
There are drugs that are contained in a capsule in the form of granules, these granules can settle on the wall of the tube and clog it.