Food for baby with diarrhoea
When your child has diarrhea: MedlinePlus Medical Encyclopedia
Diarrhea is the passage of loose or watery stools. For some children, diarrhea is mild and will go away within a few days. For others, it may last longer. It can make your child lose too much fluid (dehydrated) and feel weak.
The stomach flu is a common cause of diarrhea. Medical treatments, such as antibiotics and some cancer treatments can also cause diarrhea.
This article speaks of diarrhea in children over 1 year of age.
It is easy for a child with diarrhea to lose too much fluid and become dehydrated. Lost fluids need to be replaced. For most children, drinking the kinds of fluids they normally have should be enough.
Some water is OK. But too much water alone, at any age, can be harmful.
Other products, such as Pedialyte and Infalyte, may help keep a child well-hydrated. These products can be bought at the supermarket or pharmacy.
Popsicles and Jell-O can be good sources of fluids, especially if your child is vomiting. You can slowly get large amounts of fluids into children with these products.
You may also give your child watered-down fruit juice or broth.
Do not use medicines to slow down your child's diarrhea without talking to a doctor first. Ask your child's health care provider if using sports drinks is OK.
In many cases, you can continue feeding your child as usual. The diarrhea will normally go away in time, without any changes or treatment. But while children have diarrhea, they should:
- Eat small meals throughout the day instead of 3 big meals.
- Eat some salty foods, such as pretzels and soup.
When necessary, changes in the diet may help. No specific diet is recommended. But children often do better with bland foods. Give your child foods such as:
- Baked or broiled beef, pork, chicken, fish, or turkey
- Cooked eggs
- Bananas and other fresh fruits
- Applesauce
- Bread products made from refined, white flour
- Pasta or white rice
- Cereals such as cream of wheat, farina, oatmeal, and cornflakes
- Pancakes and waffles made with white flour
- Cornbread, prepared or served with very little honey or syrup
- Cooked vegetables, such as carrots, green beans, mushrooms, beets, asparagus tips, acorn squash, and peeled zucchini
- Some desserts and snacks, such as Jell-O, popsicles, cakes, cookies, or sherbet
- Baked potatoes
In general, removing seeds and skins from these foods is best.
Use low-fat milk, cheese, or yogurt. If dairy products are making the diarrhea worse or causing gas and bloating, your child may need to stop eating or drinking dairy products for a few days.
Children should be allowed to take their time returning to their normal eating habits. For some children, a return to their regular diet can also bring a return of diarrhea. This is often due to mild problems the gut has while absorbing regular foods.
Children should avoid certain kinds of foods when they have diarrhea, including fried foods, greasy foods, processed or fast foods, pastries, donuts, and sausage.
Avoid giving children apple juice and full-strength fruit juices, as they can loosen stool.
Have your child limit or cut out milk and other dairy products if they are making diarrhea worse or causing gas and bloating.
Your child should avoid fruits and vegetables that can cause gas, such as broccoli, peppers, beans, peas, berries, prunes, chickpeas, green leafy vegetables, and corn.
Your child should also avoid caffeine and carbonated drinks at this time.
When children are ready for regular foods again, try giving them:
- Bananas
- Crackers
- Chicken
- Pasta
- Rice cereal
Call your child's provider if your child has any of these symptoms:
- Much less activity than normal (not sitting up at all or not looking around)
- Sunken eyes
- Dry and sticky mouth
- No tears when crying
- Not urinated for 6 hours
- Blood or mucus in the stool
- Fever that does not go away
- Stomach pain
Easter JS. Pediatric gastrointestinal disorders and dehydration. In: Bakes KM, Buchanan JA, Moreira ME, Byyny R, Pons PT, eds. Emergency Medicine Secrets. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 65.
Kotloff KL. Acute gastroenteritis in children. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 366.
21st ed. Philadelphia, PA: Elsevier; 2020:chap 366.
Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
Diet for Diarrhea Only (Infant/Toddler)
The main goal while treating diarrhea is to prevent dehydration. This is the loss of too much water and minerals from the body. When this occurs, body fluids must be replaced. This is done by giving your child small amounts of liquids often. You can also give oral rehydration solution. Oral rehydration solution is available at pharmacies and most grocery stores. Don't use sports drinks—they are not good enough. In general, for mild diarrhea, the child can continue to eat.
In general, for mild diarrhea, the child can continue to eat.
If your baby is breastfed:
Keep breastfeeding. Feed your child more often than usual.
If diarrhea is severe, give oral rehydration solution between feedings.
As diarrhea decreases, stop giving oral rehydration solution and resume your normal breastfeeding schedule.
If your baby is bottle-fed:
Give small, frequent amounts of fluid. An ounce or two (30 to 60 mL) every 30 minutes may improve symptoms. Start with 1 teaspoon (5 mL) every 5 minutes and increase gradually as tolerated.
Give full-strength formula or milk. If diarrhea is severe, give oral rehydration solution between feedings.
If giving milk and the diarrhea is not getting better, stop giving milk. In some cases, milk can make diarrhea worse. Try soy or rice formula.
Don’t give apple juice, soda, or other sweetened drinks. Drinks with sugar can make diarrhea worse.
 Sports drinks are not the same as oral rehydration solutions. Sports drinks have too much sugar and not enough electrolytes to correct dehydration.
Sports drinks are not the same as oral rehydration solutions. Sports drinks have too much sugar and not enough electrolytes to correct dehydration.If your child is doing well after 24 hours, resume a regular diet and feeding schedule.
If your child starts doing worse with food, go back to clear liquids.
If your child is on solid food:
Keep in mind that liquids are more important than food right now. Don’t be in a rush to give food.
Don’t force your child to eat, especially if he or she is having stomach pain and cramping.
Don’t feed your child large amounts at a time, even if he or she is hungry. This can make your child feel worse. You can give your child more food over time if he or she can tolerate it.
If you are giving milk to your child and the diarrhea is not going away, stop the milk. In some cases, milk can make diarrhea worse. If that happens, use oral rehydration solution instead.

If diarrhea is severe, give oral rehydration solution between feedings.
If your child is doing well after 24 hours, try giving solid foods. These can include cereal, oatmeal, bread, noodles, mashed carrots, mashed bananas, mashed potatoes, applesauce, dry toast, crackers, soups with rice noodles, and cooked vegetables.
Don't feed your child high fat foods.
Don't feed your child high sugar foods including fruit juice and sodas.
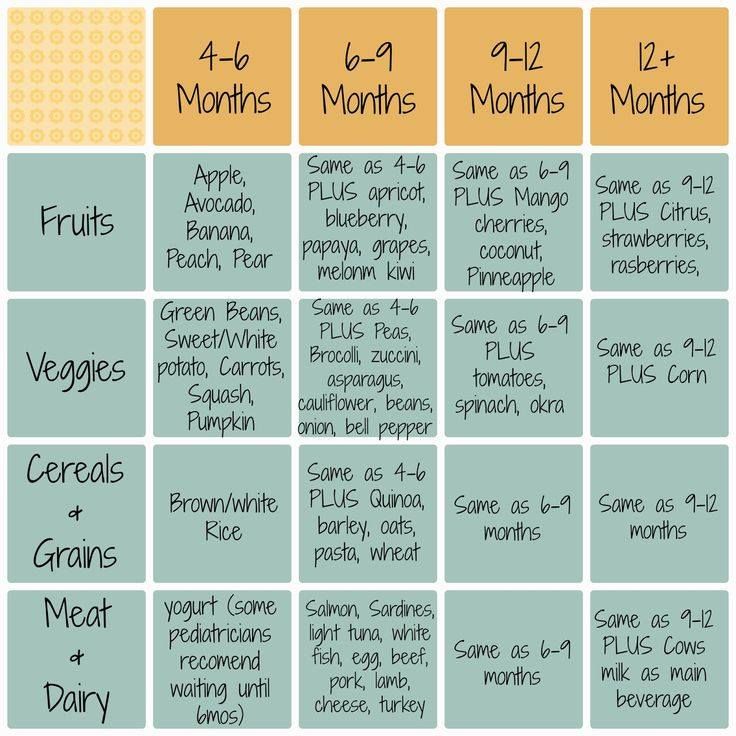
For babies over 4 months, as they feel better, you may give cereal, mashed potatoes, applesauce, mashed bananas, or strained carrots during this time. Babies over 1 year may add crackers, white bread, rice, and other starches.
If your child starts doing worse with food, go back to clear liquids.
You can resume your child's normal diet over time as he or she feels better. If at the diarrhea or cramping gets worse again, go back to a simple diet or clear liquids.

Follow-up care
Follow up with your child’s healthcare provider, or as advised. If a stool sample was taken or cultures were done, call the healthcare provider for the results as instructed.
Call 911
Call 911 if your child has any of these symptoms:
When to seek medical advice
Call your child’s healthcare provider right away if any of these occur:
Belly pain that gets worse
Constant lower right belly pain
Repeated vomiting after the first two hours on liquids
Occasional vomiting for more than 24 hours
Continued severe diarrhea for more than 24 hours
Blood in stool
Refusal to drink or feed
Dark urine or no urine, or dry diapers, for 4 to 6 hours in an infant or toddler, or 6 to 8 hours in an older child, no tears when crying, sunken eyes, or dry mouth
Fussiness or crying that cannot be soothed
Unusual drowsiness
New rash
More than 8 diarrhea stools within 8 hours
Diarrhea lasts more than one week on antibiotics
Fever (see Children and fever, below)
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer.
Never use a mercury thermometer.
For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
Ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead (temporal artery) temperature of 100.4°F (38°C) or higher, or as directed by the provider
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the provider
Child age 3 to 36 months:
Rectal, forehead (temporal artery), or ear temperature of 102°F (38.
 9°C) or higher, or as directed by the provider
9°C) or higher, or as directed by the providerArmpit temperature of 101°F (38.3°C) or higher, or as directed by the provider
Child of any age:
Repeated temperature of 104°F (40°C) or higher, or as directed by the provider
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
Was this helpful?
Yes No
Tell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.![]()
I still don't know what to do next.
Other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
Thank You!
© 2000-2020 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Start New Patient Education Search
Diet for diarrhea in a 1-year-old child
When a child is sick, it is always a serious test for a family. Moreover, if the baby has vomiting, frequent loose stools, fever, he refuses to eat. In such cases, parents naturally face the question: what to do?
The first thing to do is to see a doctor. In most cases, this condition is associated with an acute intestinal infection and can lead to serious consequences for the baby. And timely treatment allows you to quickly deal with the problem.
The second significant issue facing the parents of a sick child is the issue of proper nutrition. Unfortunately, you can still find recommendations to stop feeding a child during diarrhea, but this should not be done categorically.
Important!
It has been proven that "water-tea" breaks and starvation diets significantly weaken the protective functions of the child's body and lead to a delay in recovery processes in the intestines. Therefore, at present, most pediatricians insist on the mandatory continuation of the child's nutrition in case of acute intestinal infections, but with the obligatory consideration of the latest achievements in nutrition.
Therefore, at present, most pediatricians insist on the mandatory continuation of the child's nutrition in case of acute intestinal infections, but with the obligatory consideration of the latest achievements in nutrition.
The main principles for managing the nutrition of a child with diarrhea should be:
| Phased | The development of the disease has a staging, each stage must correspond to certain approaches to diet therapy |
| Accounting for the age of the child | Each age should have its own products and its own schemes for their purpose |
| Accounting for the severity of the disease |
There are three main stages of diet therapy. The first stage corresponds to the acute period of the disease, when the maximum manifestations of the disease are noted (vomiting, loose stools, fever), and the child may refuse his usual diet. During this period, proper nutrition is an integral part of treatment. And the success of treatment largely depends on the correct organization of diet therapy in a child.
During this period, proper nutrition is an integral part of treatment. And the success of treatment largely depends on the correct organization of diet therapy in a child.
The second stage is the recovery period. There are no longer those manifestations of the disease that were noted in the baby in the acute period, the child has an appetite, he becomes more active, but it must be remembered that any acute intestinal infection leads to significant changes in the child's body. This is a violation of the microflora of the gastrointestinal tract, and dysfunction of enzyme systems, bile secretion and other digestive processes. It takes time to restore the correct functioning of the gastrointestinal tract, which requires a sparing diet at this stage. Violation of the diet during this period can lead to the formation of a chronic pathology of the gastrointestinal tract.
The third stage of diet therapy is aimed at a gradual transition to the usual diet for this baby. Breastfed babies should continue to breastfeed. If the baby is bottle-fed, the doctor will prescribe a formula that matches the baby's condition. In children older than one year, it is necessary to exclude whole milk from the diet, they are also shown the appointment of fermented milk products as a diet therapy, the favorable properties of which are due to a number of positive qualities: the presence of lactic acid gives the product pronounced bactericidal properties and inhibits the growth of pathogenic microflora, the positive effect of these products on intestinal microbiocenosis, the secretory function of the digestive glands and intestinal motility, and they also have immunomodulatory properties.
If the baby is bottle-fed, the doctor will prescribe a formula that matches the baby's condition. In children older than one year, it is necessary to exclude whole milk from the diet, they are also shown the appointment of fermented milk products as a diet therapy, the favorable properties of which are due to a number of positive qualities: the presence of lactic acid gives the product pronounced bactericidal properties and inhibits the growth of pathogenic microflora, the positive effect of these products on intestinal microbiocenosis, the secretory function of the digestive glands and intestinal motility, and they also have immunomodulatory properties.
One of the important components of diet therapy is the use of dairy-free cereals with pro- and synbiotics. Clinical studies have shown that the appointment of this diet therapy contributes to a more rapid relief of the main symptoms of intestinal dysfunction, as well as the restoration of intestinal microflora.
Choose foods for the diet
It is most correct to start with rice porridge, as it has pronounced sorption properties and helps to stop diarrhea. As the child recovers, oatmeal and buckwheat porridge can be included in the diet.
As the child recovers, oatmeal and buckwheat porridge can be included in the diet.
Vegetables and fruits are an important component in the first stage of diet therapy. Preference should be given to products that contain pectin (baked apple, boiled carrots), as they contribute to the sorption of pathogens and their toxins. At the first stage of diet therapy, the use of fresh vegetables and fruits, as well as juices, is not shown.
The second stage - the patient's condition improves, the child becomes active, appetite improves, and in some children it even becomes elevated, which is often perceived by parents as a signal for increased nutrition. It is absolutely impossible to do this, since the child's body has not yet recovered from the disease. During this period, it is necessary to continue eating sour-milk, lactose-free and low-lactose products. An obligatory component of diet therapy is the use of nutrition with probiotics.
The third stage is the gradual expansion of the diet according to the age of the child. At this stage, the most justified is the widespread use of probiotic foods in order to restore and maintain the function of the gastrointestinal tract and its microbiocenosis.
At this stage, the most justified is the widespread use of probiotic foods in order to restore and maintain the function of the gastrointestinal tract and its microbiocenosis.
What to feed a child with diarrhea at first?
- freshly cooked rice;
- bananas;
- natural apple juice;
- boiled potatoes;
- boiled chicken meat;
- crackers and stale bread;
- lean fish;
- weak tea.
What can you eat with diarrhea in a child and an adult | Diet for diarrhea
Co-author, editor and medical expert - Klimovich Elina Valerievna.
Number of views: 2 814 937
Date last updated: 09/27/2022
Average read time: 4 minutes0003 What can you eat if you have diarrhea? It is very important to adjust your diet and eating habits to help your body cope with the problem as effectively as possible. Top of page Top of page Drink at least a glass of fluid after each bout of diarrhea to prevent dehydration. In case of intestinal upset, drink water, weak tea, apple juice, low-fat broth. A liquid diarrhea diet does not burden the digestive tract with heavy work and helps prevent irritation. Back to Contents Try not to smoke or drink alcohol.
What to drink with diarrhea?
What should I avoid if I have diarrhea?
What is diarrhea and how to treat it  If you do not know what to eat with diarrhea, use our recommendations.
If you do not know what to eat with diarrhea, use our recommendations. What can you eat with diarrhea?

What to drink with diarrhea?
What Should I Avoid When I Have Diarrhea?