Foods to avoid for babies with acid reflux
Feeding A Baby With Reflux | Parenting Blog | Babocush Limited
It may seem like it was just yesterday when you brought home your little bundle of joy then just like that, it’s time to wean your baby off of milk and introduce solid foods. This process might feel overwhelming, especially if your child is still experiencing baby reflux.
What are the symptoms of baby reflux?
It is important to note the symptoms. Repeated crying, vomiting or spitting up, arching of the back or neck during or after feeds, recurrent ear infections, incapacity to sleep or frequent waking, irritability and lastly, frequent hiccups. Babies typically grow out of reflux within the first two years of their life. With that being said, there are still some foods that can aggravate reflux and others that can ease it.
If your baby suffers with reflux, you may feel more comfortable consulting your doctor before you wean your baby off milk and transition them onto solid foods. As a general rule of thumb, you should avoid giving your baby solid food before they’re four months old.
It’s important that you start the weaning process with purees and baby led weaning.The best foods to feed a baby with reflux are purees of vegetables, particularly root vegetables like potatoes, carrots, pumpkin, swede, parsnips and sweet potato. You can also feed your baby any non-acidic fruits. You should avoid citrus fruits like oranges, apples and grapes, tomatoes, peppers, courgettes, cucumbers and aubergines. In addition to that, you should also avoid any foods that have cow’s milk proteins as well as spicy foods.
How to introduce solid foods?
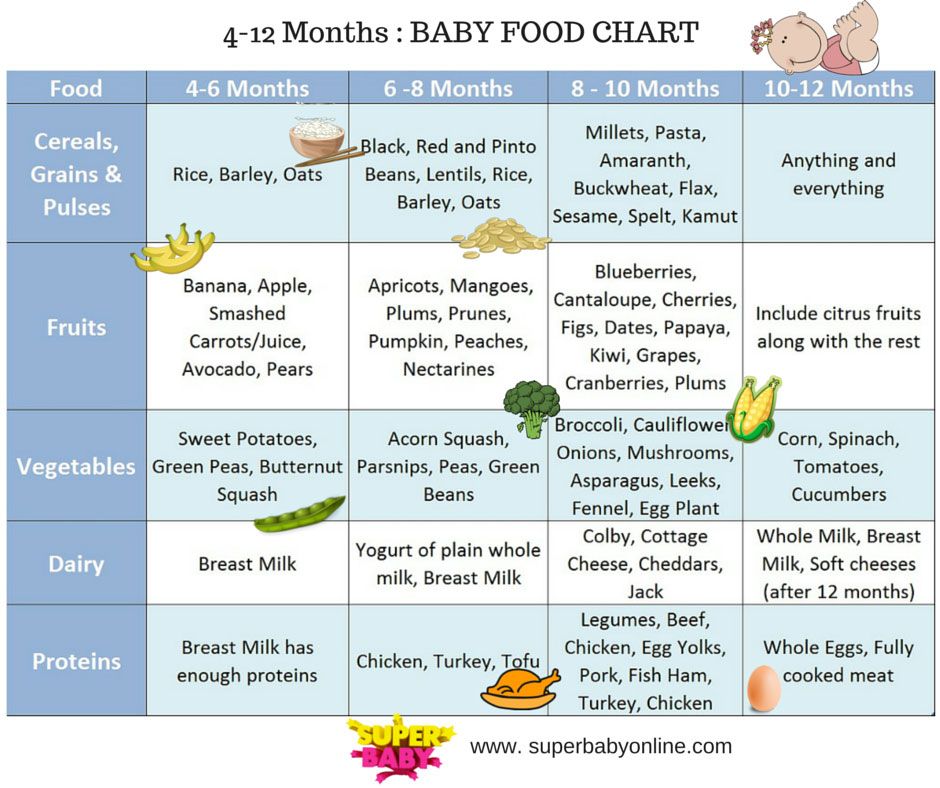
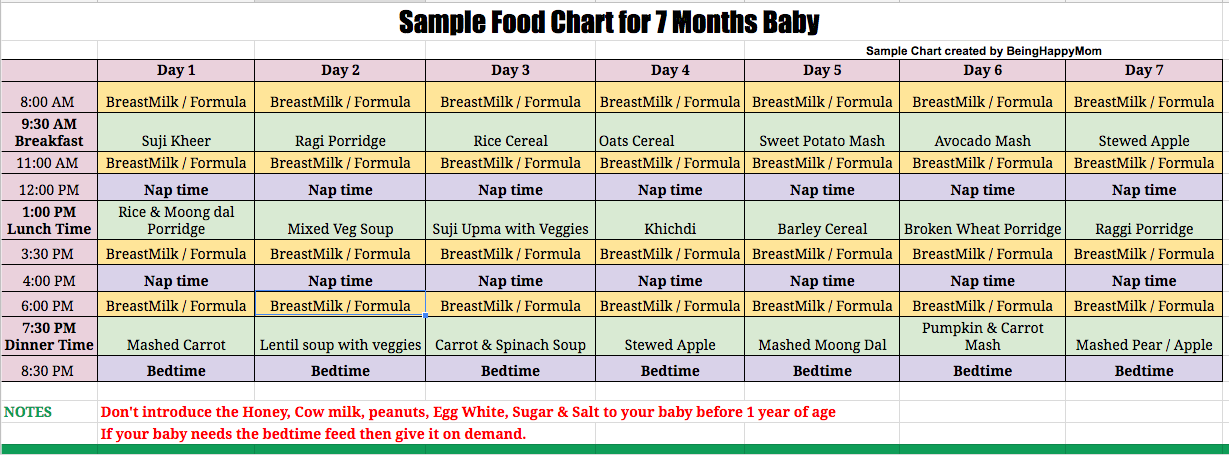
By the time your little one is 4 to 6 months old, you'll probably have your breastfeeding or formula drill down to an art. However, don’t get too comfortable - your baby will soon be ready for "real" food. When it comes to giving your baby solid food, there are a few tips you can follow that can make the process much easier…
Wean your baby slowly
As a general rule of thumb, you should wean your baby slowly and let them take the lead on how much food they need.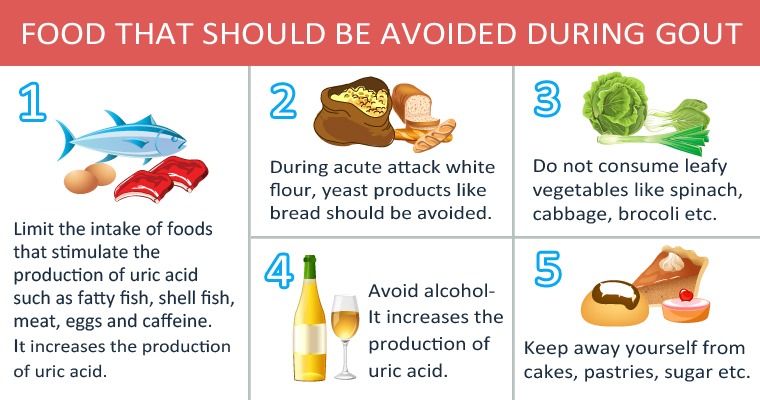 Don’t hurry meal times, allowing plenty of time for food to settle in your baby’s tummy.
Don’t hurry meal times, allowing plenty of time for food to settle in your baby’s tummy.
Start with smooth foods
You should also start your baby on food that is completely smooth. The textures of different kinds of foods can be a trigger for your infant to spit it up. That is not to say you can never introduce different textures, just make sure that you do so slowly. You should also make sure that you sit your baby upright when feeding them.
Watch out for allergies
You can include any foods that are a part of your family’s diet during complementary feeding. As a precaution, you could introduce foods one at a time for three days at first and, if your baby has no issues, the next new food should be added.
This way, any problematic food would be easier to recognise in the unlikely event that an acute or delayed form of allergic reaction occurs. Once potential allergens, such as eggs and peanuts, have been introduced it is recommended that you continue to include them in your baby’s diet, ideally at least twice a week, to ensure that your baby remains tolerant to that particular food.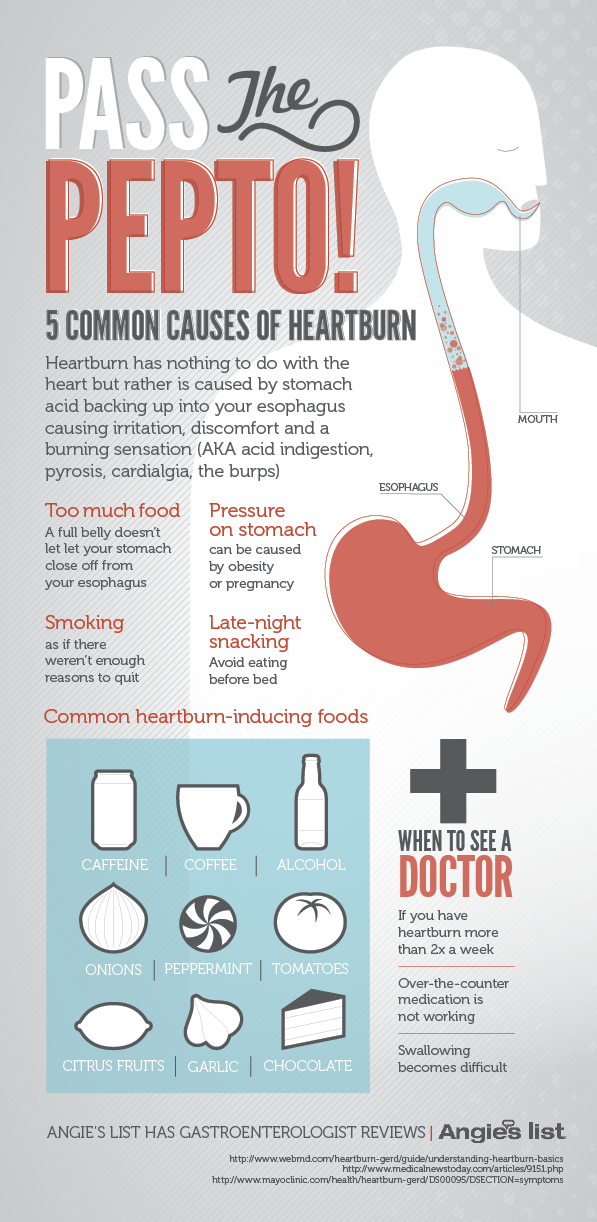
Spacing the time in between introducing new foods will give you the opportunity to discover the foods your baby likes and dislikes. Although your baby’s reflux can make introducing solid foods a challenge, it’s by no means impossible.
Related Blogs:
- Why Do Babies Hiccup?
- How To Burp A Baby
What Foods to Avoid When Breastfeeding Baby with Reflux
Sharing is caring!
- Share
Is your breastfed baby suffering from acid reflux? It can be so stressful to see your baby go through this, even though it is a common problem with newborns. If your baby is having acid reflux, there are lots of things you can do to improve their condition such as changing feeding position, burping after feeding and being aware of food to avoid when breastfeeding.
Acid reflux usually happens when the acid in the stomach moves back into the esophagus or the food pipe, resulting in the irritation of the lining of the food pipe and heartburn.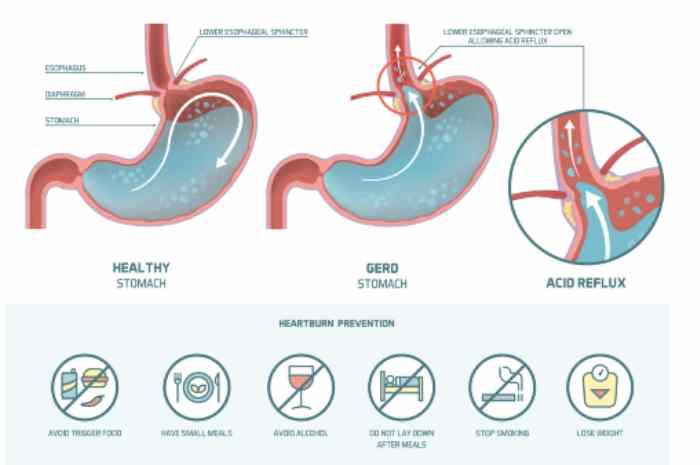 But many new moms do not realize that if you are nursing it can also be a problem for your baby. The good thing is it is not as dangerous as it sounds.
But many new moms do not realize that if you are nursing it can also be a problem for your baby. The good thing is it is not as dangerous as it sounds.
If your baby has reflux after nursing, you may need to consider eliminating the food or drink that you consumed within a few hours or so before nursing.
Keeping a food journal of everything you eat and drink with the date and time you consumed it can be very helpful for pin pointing the foods that may be triggering your newborn’s reflux.
Remember what you eat or drink, will affect your baby. So, a well-balanced breastfeeding diet is important for your health as well as your baby’s health.
In most cases, there is no need to medicate your baby for reflux. Diet changes will provide great results for your baby and you. After all, it is very disturbing to see your baby in distress. By removing acid foods, foods that trigger reflux, and overeating you will see the desired results quickly.
Make sure to pin this post for later!
{Disclosure: This post contains affiliate or referral links.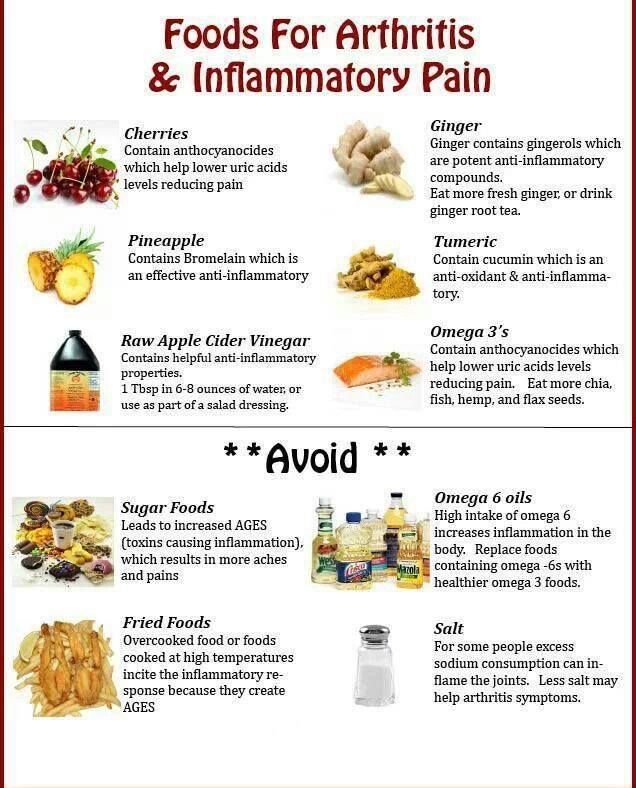 Read more about that here.}
Read more about that here.}
List of Foods to Eliminate to help control your baby’s reflux
There are some foods that commonly can cause acid reflux for breastfed babies. It can be hard to “give up” some of these foods so it’s important to focus on what you can eat while breastfeeding, just as much as the foods to avoid.
While many of these foods are good for you normally, while breastfeeding it can be helpful to eliminate these foods to aid in relieving your baby’s acid reflux.
The advice included in this article is meant for informational purposes only. Please consult your care provider before making any decisions regarding your pregnancy.
Tomatoes
Tomatoes contain citric acid, malic acid and trace amounts of oxalic acid. People who have acid reflux triggered by these acids may well have acid reflux from eating tomatoes, their by-products, such as pizza or ketchup, or drinking tomato juice. That’s a lot of acid!
Tomatoes may not cause you to have reflux, but it may be the culprit that is causing your baby to spit up after nursing.
Coffee, Tea, and Carbonated Beverages
These drinks are all caffeinated and should be avoided while nursing a baby that has reflux. They also contain different amounts of acid which may cause you distress to your baby’s tummy. They may be high in sugar as well.
Alcohol
Beer, wine, and liquor can relax the lower esophageal sphincter. Alcohol also stimulates the production of stomach acid. Many alcoholic beverages can be high in sugar as well. It’s best to avoid alcohol while nursing if you baby has acid reflux.
Citrus Fruits
Citrus fruits such as oranges, lemons, limes, and grapefruits contain more acid than other fruits that may lead to reflux. They also relax the lower esophageal sphincter. Enjoy other fruits while nursing.
High Fat Dairy
Try to substitute high fat milk, cheese, yogurt, and other dairy products for low fat options. Try coconut, oat, cashew or almond milk if cow milk is not tolerable for your nursing baby.
Read What to Eat While Breastfeeding for ideas of what to eat instead of dairy.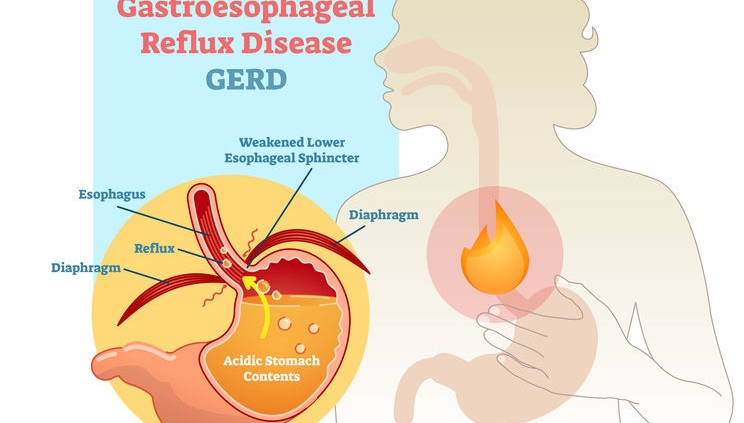
Mint
There is a big debate about mints such as peppermint and spearmint products. In some people it seems to cause heartburn and acid reflux. So, to be on the safe side, do not chew mint gum or eat mint foods while nursing.
Peppermint is known to be among the herbs that decreases milk supply also.
Spicy Foods
Spicy foods are a part of everyday life for most people. But eating spicy foods such as chili and peppers may cause reflux for your nursing baby.
Consider eliminating spicy foods while nursing and see if it helps your baby’s reflux.
High Fat Foods and Fried Foods
Foods high in fat such as fried chicken, milkshakes, sauces, cakes, and other rich foods should be avoided when nursing. These foods worsen acid reflux and can cause weight gain because of high in calories.
Check out 5 ways to lose the postpartum belly here.
Red Meat
Red meat is high in acid and fat content that can cause reflux. Do you need to totally avoid red meat? No! Just consider substituting fatty cuts for leaner cuts of meat while you are breastfeeding your baby with reflux.
Do you need to totally avoid red meat? No! Just consider substituting fatty cuts for leaner cuts of meat while you are breastfeeding your baby with reflux.
Processed Grain and Flour
Most of these foods are classified “junk food”. Some included are breads, hamburgers, cakes, cookies, and there are many more. Avoid these foods, they may cause reflux or gas for your nursing baby.
Look into making your own healthy breastfeeding snacks like these.
Garlic and Onions
Garlic and onions are known to cause heartburn or acid reflux in some people. Your baby may be one those people. So be careful consuming these when you are breastfeeding and test out eliminating this food if your newborn’s acid reflux persists.
Cruciferous Vegetable
Vegetables like broccoli, cauliflower and cabbage may cause gas in many breastfed babies which can lead to reflux for your baby. You may want to eliminate these as well if they effect your nursing baby.
Chocolate
Chocolates contain cocoa and theobromine, which are known to increase the acidity in the stomach. This is a hard one to give up, but you may have to forgo chocolate bars, hot chocolate, chocolate milk, and other chocolate products until after nursing if your baby is suffering from reflux.
Don’t worry, this time of having to watch what you eat does not last long. Generally by 6 months most babies out grow their digestive sensitivities to food you eat while breastfeeding and you can go back to a normal diet.
It is always best to consult your baby’s pediatrician if reflex continues. But changing your diet, controlling your weight, avoiding irritating foods, and generally taking care of yourself will in turn, keep your breastfeed baby healthy too.
More Breastfeeding Resources
Here at Birth Eat Love our goal is to make healthy eating easier for busy Moms during postpartum and breastfeeding.
Homemade breastfeeding snack recipes – this ebook has some great recipes that are low in sugar and dairy free for boosting milk supply.
Wondering what foods you can eat that will help increase your milk supply? This post has 11 real foods that you can eat today to make more milk and includes recipes, supplements and product suggestions.
Do you have a colicky or super fussy breastfed baby? There are some foods you may be eating that could be making your baby uncomfortable. Read about a few foods to avoid while breastfeeding here.
Looking for breastfeeding recipes that can help support your milk production? Here are 9 breastfeeding soups that you can make in the slow cooker or instant pot.
Interested in making freezer meals so you can have easy dinners? Check out this freezer meal ebook that has 12 recipes specifically designed to support breastfeeding and postpartum recovery.
Tired of trying to decide what to eat while breastfeeding? Reduce the thinking and stressing about meal time with this simple breastfeeding meal plan.
Trying to find a way to cope with the summer heat? Look no further with These refreshing iced teas
Sharing is caring!
- Share
Proper nutrition for GERD - Clinic on Leninsky
The key to solving many problems with the gastrointestinal tract is proper nutrition. Gastroenterologist at the Clinic on Leninsky Katerina Chesskaya tells what you can and should eat for those who suffer from reflux disease.
What is GERD?
Gastroesophageal reflux disease (GERD) is a chronic relapsing disease in which there is a spontaneous, regularly repeated reflux of stomach contents into the esophagus. As a result, the lower esophagus is affected. The reflux of stomach contents into the esophagus is considered normal if it occurs occasionally and is not accompanied by negative factors. The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.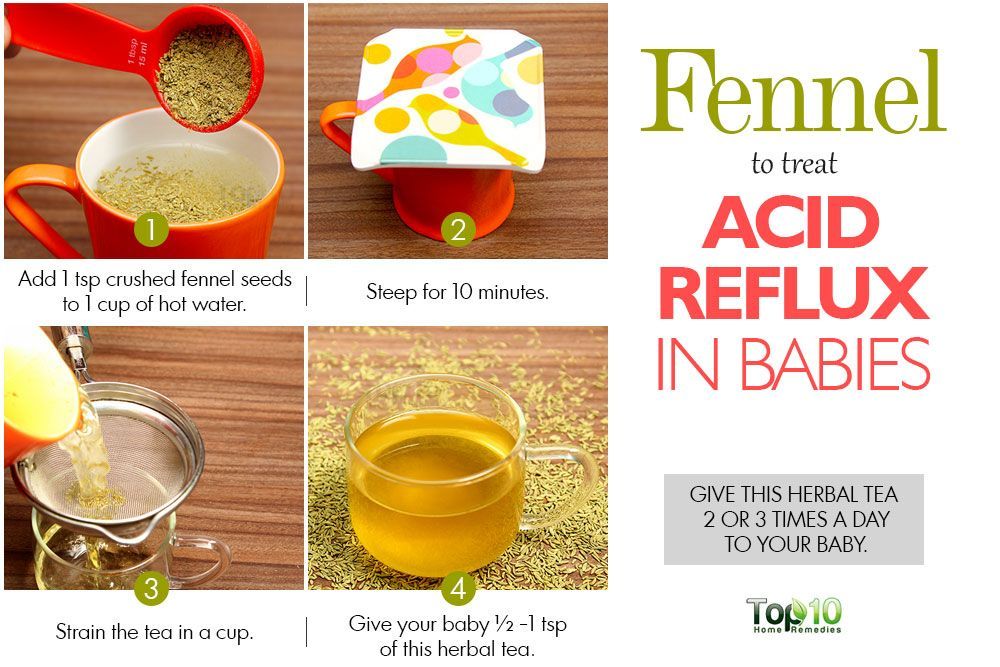 nine0005
nine0005
GERD is usually manifested by belching and heartburn after eating or bending forward, and also at night. Another indication of the presence of GERD is pain behind the sternum, extending to the interscapular region, lower jaw, and the left half of the chest. There are also signs of GERD that are not directly related to the esophagus - a cough, shortness of breath, often occurring when lying down, hoarseness, dry throat, rapid satiety, and bloating. The cause of chronic inflammatory diseases of the nasopharynx (pharyngitis, laryngitis, sinusitis, tonsillitis) in 30% of cases is GERD. It has been proven that against the background of GERD there is a risk of developing obstructive pulmonary diseases, including bronchial asthma. nine0005
Proper nutrition for GERD
As in the case of many other diseases of the gastrointestinal tract, the main principle of the treatment of GERD is proper nutrition. There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter. nine0005
These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter. nine0005
Here is a list of foods to consider when planning your menu for the day.
Delete:
1. Bread: fresh rye bread, tarts and pancakes.
2. Meat: stewed and fried meat dishes from fatty meat, poultry.
3. Fish: fatty fish, fried, smoked, salty dishes.
4. Vegetables: white cabbage, turnip, rutabaga, radish, sorrel, spinach, onion, cucumbers, salted, pickled and pickled vegetables, mushrooms.
5. Fruit: Raw, sour, unripe fruit, dried fruit puree. nine0021 6. Cereals: millet, pearl barley, barley and corn grits, legumes.
7. High acidity dairy products, spicy and salty cheeses.
8.:max_bytes(150000):strip_icc()/what-can-i-eat-if-i-have-a-peptic-ulcer-1742154-01-ec37a34d14c44195999f8d44372f820b.png?resize=1060%2C707&ssl=1) Sweet: halva, chocolate, ice cream, cakes.
Sweet: halva, chocolate, ice cream, cakes.
9. Drinks: sour, carbonated, fruit drinks, strong tea, coffee and alcohol.
Recommended:
1. Bread: from wheat flour of the first or highest grade, yesterday, dry, uncomfortable baking.
2. Meat: Beef, veal, chicken, rabbit, turkey, all in the form of cutlets, meatballs, soufflés, mashed potatoes and quenelles. nine0021 3. Fish: boiled river fish - zander, pike, perch, any low-fat varieties.
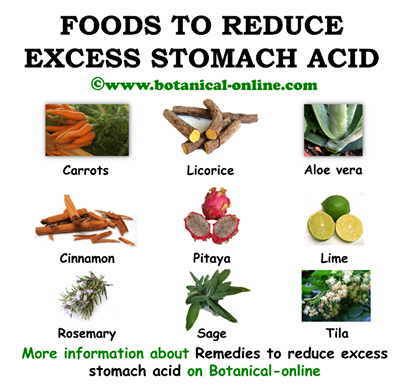
4. Vegetables: carrots, cauliflower, potatoes, beets, squash and squash.
5. Fruits: Sweet berries, ripe fruits. Preferably mashed or baked.
6. Cereals: oatmeal, semolina, buckwheat (mashed), rice porridge, on the water with the addition of milk, boiled vermicelli.
7. Dairy products: milk, lean cheese and low-fat sour cream. Cottage cheese dishes made from pureed cottage cheese, for example, cheesecakes, casseroles. nine0021 8. Sweet: jam, marshmallows, honey, marshmallow, cream and milk puddings.
9. Drinks: weak tea or cocoa with milk, sweet juices and decoctions.
Drinks: weak tea or cocoa with milk, sweet juices and decoctions.
It is also important to adhere to the diet:
— Fractional meals in small amounts and often up to 5-6 times a day.
- Do not lie down immediately after eating, the last meal is 2-3 hours before bedtime.
- Do not work in a slope, exclude the "gardener" pose.
- Do not wear tight belts and limit abdominal exercise. nine0021 - Obese people need to normalize body weight.
Remember that only a gastroenterologist can make a diagnosis of GERD (however, like any disease), to accurately determine the patient's condition. At the appointment, the doctor, together with the patient, will find the cause of the disease, outline a treatment plan and further supportive therapy in order to avoid relapses.
At the Clinic on Leninsky, an appointment is being made:
- pediatric gastroenterologist Natalya Medvedeva;
- gastroenterologist Ekaterina Chesskaya. nine0064
You can make an appointment with a gastroenterologist at the Clinic on Leninsky
by calling +7 (495) 668-09-86 .
Moscow, Leninsky prospect, building 67, building 2
Tel. .-Fri. 7:30–20:00 Sat-Sun 9:00–18:00
Treatment and prevention of gastroesophageal reflux disease (GERD)
Gastroesophageal reflux disease (GERD) common, but rarely detected and therefore untreated since GERD usually responds well to treatment.
GERD is treated gradually. The doctor will help you choose the right course of treatment. If the disease is mild, it will be enough for the patient to follow a certain diet, give up certain activities, and sometimes take over-the-counter medications. nine0005
In cases where the symptoms are more persistent (daily heartburn, symptoms that come on at night), prescription medication may be required. Surgery is a reasonable alternative to permanent medication, especially if the disease is acquired at an early age.
Surgery is also recommended if medication does not help. However, today there is a new generation of drugs that can effectively control gastroesophageal reflux. nine0005
If symptoms are still uncomfortable after taking strong drugs, GERD is most likely not the cause. Most gastroenterologists and surgeons do not recommend surgery in such cases, since the symptoms still continue to disturb after it.
Lifestyle changes
Gastroesophageal reflux treatment begins with lifestyle changes. First you need to understand what affects the occurrence of symptoms. nine0005
If you have symptoms of GERD, use the following tips:
- Avoid foods and drinks that stimulate the lower esophageal sphincter to relax, such as foods flavored with mint, chocolate, and alcohol.
- Lose weight if you are overweight. Being overweight and obese contributes to GERD because being overweight increases pressure on the stomach and lower esophageal sphincter, causing acidic stomach acid to reflux into the esophagus and irritate the esophageal mucosa.
 nine0064
nine0064
- Do not lie down for at least two or three hours after eating. After eating it is good to take a walk. This not only prevents the onset of GERD symptoms, but also burns extra calories.
- Avoid foods that trigger GERD symptoms. Do not eat fatty or fried foods, creamy sauces, mayonnaise or ice cream. Other foods that may exacerbate symptoms include coffee, tea, sodas, tomatoes, and citrus fruits. nine0064
- Stop smoking. Smoking disrupts the digestive system and, according to some studies, relaxes the lower esophageal sphincter. Smoking also reduces the amount of bicarbonate in saliva and reduces its ability to protect the esophagus from stomach acid. Some types of nicotine replacement therapy (nicotine patch, nicotine gum) can cause indigestion, stomach pain, and vomiting. Talk to your doctor about possible side effects of these products before use. nine0064
- Do not wear clothes that put pressure on your belly, such as tight belts, tight jeans, and elastic waistbands that put pressure on your stomach and lower esophageal sphincter.

- Raise the head of the bed 15 to 20 cm or use a wedge pillow to force acid into the stomach by gravity.
- Do not bend over after eating. If you need to pick something up from the floor, it's better to squat on half-bent knees and try not to bend at the waist. Do not engage in sports and physical labor after eating. nine0064
- Check your medications. Some medications can make symptoms worse. These drugs include theophylline, calcium channel blockers, alpha and beta blockers, anticholinergics that may be present in drugs used to treat Parkinson's disease, asthma, and some over-the-counter cold and cough medicines. If you think a drug you are taking is affecting your symptoms, talk to your doctor about alternatives. Do not interrupt the prescribed treatment without consulting a doctor. nine0064
Medication for gastroesophageal reflux
Your doctor may prescribe medication for GERD.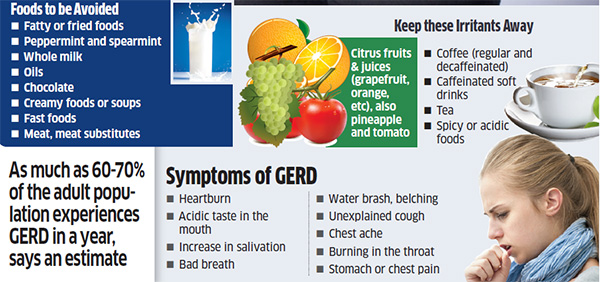 Because GERD is often a chronic condition, you will need to take medication for the rest of your life. In some cases, long-term treatment is not required.
Because GERD is often a chronic condition, you will need to take medication for the rest of your life. In some cases, long-term treatment is not required.
Be patient, it takes time to find the right drug and dosage. If the symptoms do not go away even after taking the drugs, or if they reappear immediately after completing the course, consult your doctor. If GERD symptoms appear during pregnancy, contact your obstetrician before starting medication. nine0005
The following is information about drugs commonly prescribed to treat GERD:
Over-the-counter antacids
These drugs help with mild and rare symptoms. Their action is to neutralize the acidic gastric juice. Antacids are usually fast-acting and can be taken as needed. Because they do not last long, they do not prevent heartburn and are less effective for symptoms that often occur. nine0005
Most antacids contain calcium carbonate (Maalox) or magnesium hydroxide. Sodium bicarbonate, or baking soda, helps with heartburn and indigestion. It should be mixed with at least 120 ml of water and taken one to two hours after meals so as not to overload a full stomach. Talk to your doctor about the need for this treatment. Do not use this method for more than two weeks and use it only in extreme cases, since soda can lead to metabolic disorders (pH) and the formation of erosions in the esophagus and stomach. Before using it on children under 12 years of age, consult a doctor. nine0005
Another type of antacid contains alginate or alginic acid (eg Gaviscon). The advantage of such an antacid is that it does not allow fluid to seep back into the esophagus.
Antacids can interfere with the body's ability to absorb other drugs, so if you are taking other drugs, check with your doctor before taking antacids.
Ideally, you should take antacids at least 2-4 hours after taking other drugs to minimize the chance of them not being absorbed. People with high blood pressure should avoid taking high sodium antacids (Gaviscon). nine0005
Finally, antacids are not a reliable treatment for erosive esophagitis, a disease that must be treated with other drugs.
Hydrochloric acid suppressants
These drugs reduce the amount of acid produced by the stomach and are available both with and without a prescription. Usually, the same drugs are dispensed on prescription, but in a larger dosage. They may help those who are not helped by antacids. Most patients get better if they take drugs that suppress the production of hydrochloric acid and make lifestyle changes. nine0005
The mechanism of action distinguishes between two groups of such drugs:
-Blocks H 2 -gistamine reticators
-Proton pump inhibitors
Most likely, the doctor recommends taking the drug within a few weeks in a standard dose, and then if it is not possible to achieve the desired effect, prescribe a drug with a higher dosage.
Traditional h3 blockers include:
- nizatidine (Axid AR Axid AR)
- famotidine (Pepcid AS Pepcid AC)
- cimetidine (Tagamet HB Tagamet HB)
- ranitidine 75 (Zantac 75)
Pepcid Complete is a combination of famotidine, calcium carbonate and magnesium hydroxide found in antacids.
Conventional proton pump inhibitors include:
- lansoprazole (Prevacid)
- omeprazole (Prilosec, Prilosec)
- rabeprazole (AcipHex, AcipHex, Pariet)
- pantoprazole (Protonix Protonix, Nolpaza Nolpaza)
- esomeprazole (Nexium) , Nexium)
- omeprazole + sodium bicarbonate ("Zegeride" Zegerid)
- dexlansoprazole ("Dexilant" Dexilant)
Proton pump inhibitors (PPI) also reduce acidity, but are more powerful than h3- blockers. Proton pump inhibitors are most commonly prescribed to treat heartburn and acid reflux. nine0005
These drugs block the secretion of acid from the cells of the gastric mucosa and significantly reduce the amount of stomach acid. They don't work as fast as antacids, but they can relieve reflux symptoms for hours.
They don't work as fast as antacids, but they can relieve reflux symptoms for hours.
PPIs are also used to treat inflammation of the esophagus (esophagitis) and erosions of the esophagus. Studies have shown that the majority of patients with esophagitis who took these drugs recovered after 6-8 weeks. It is likely that your doctor will re-evaluate your health after 8 weeks of taking proton pump inhibitors and, according to the results, reduce the dosage or stop treatment. If symptoms do not return within three months, you will only need to take medication occasionally. People with liver disease should consult their doctor before taking these drugs. nine0005
Prokinetics
Prokinetics e.g. They also increase the contractions of the esophagus and stomach to some extent, so that the stomach is emptied more quickly. These drugs may be used as an adjunctive treatment for people with GERD.
GERD surgery
Surgery is an alternative to conservative treatment of GERD. Surgery is most commonly performed on young patients (because they would otherwise require long-term treatment) with typical GERD symptoms (heartburn and belching) who are helped by medication but are looking for an alternative to daily medication.
Surgery is most commonly performed on young patients (because they would otherwise require long-term treatment) with typical GERD symptoms (heartburn and belching) who are helped by medication but are looking for an alternative to daily medication.
Patients with atypical symptoms or patients who are not responding to medical treatment should only have surgery if there is no doubt about the diagnosis of GERD and the relationship between symptoms and reflux is confirmed by research. nine0005
Fundoplication is used in most cases. During this operation, the upper part of the stomach is wrapped around the lower esophageal sphincter, which increases its tone. These days, minimally invasive (laparoscopic) techniques are commonly used instead of traditional "open" surgery. One of the benefits of a fundoplication is that the hiatal hernia can also be repaired during the operation.
Surgery is not always effective and some patients still need to take medication after surgery. The results of this surgery are usually positive, but complications can still occur, such as difficulty swallowing, bloating and gas, difficult recovery after surgery, and diarrhea that occurs due to damage to the nerve endings that are adjacent to the stomach and intestines. nine0005
The results of this surgery are usually positive, but complications can still occur, such as difficulty swallowing, bloating and gas, difficult recovery after surgery, and diarrhea that occurs due to damage to the nerve endings that are adjacent to the stomach and intestines. nine0005
Prevention of GERD
First of all, you need to pay attention to lifestyle and avoid situations that can trigger the onset of the disease.
Remember that GERD happens when stomach acid backs up into the esophagus, which connects the throat to the stomach.
To keep the lower esophageal sphincter functioning properly, follow these guidelines:
Avoid bending over or other physical exercises that increase pressure on the abdominal cavity. Don't exercise on a full stomach. nine0005
Do not wear clothes that are tight around the waist, such as elastic waistbands and belts, which can increase pressure on the stomach.
Do not lie down in the field of food.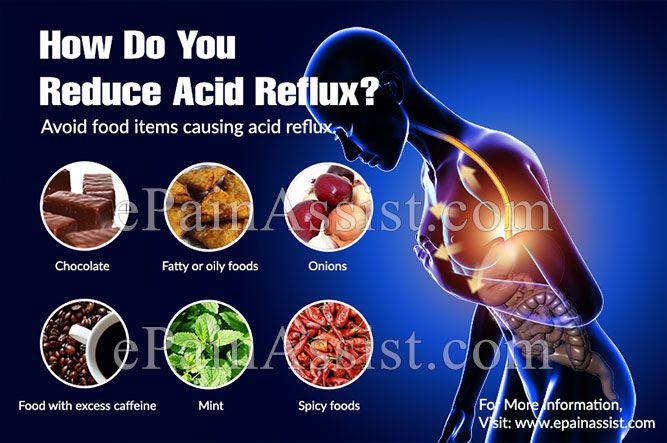 If you lie on your back after a large meal, it will be easier for the contents of the stomach to pass into the esophagus. For a similar reason, don't eat before bed. The head of the bed should rise 15-20cm so that gravity keeps the acid in the stomach where it should be while you sleep. nine0005
If you lie on your back after a large meal, it will be easier for the contents of the stomach to pass into the esophagus. For a similar reason, don't eat before bed. The head of the bed should rise 15-20cm so that gravity keeps the acid in the stomach where it should be while you sleep. nine0005
Do not overeat. Due to the fact that there is a large amount of food in the stomach, pressure on the lower esophageal sphincter increases, as a result of which it opens.
To keep your lower esophageal sphincter and esophagus functioning properly, follow these tips:
Quit smoking and avoid products containing tobacco. Smoking relaxes the lower esophageal sphincter, reduces the amount of acid-neutralizing saliva in the mouth and throat, and damages the esophagus. nine0005
Avoid foods that aggravate symptoms, such as tomato sauces, mints, citrus fruits, onions, coffee, fried foods, and carbonated drinks.
Do not drink alcoholic beverages. Alcohol causes the lower esophageal sphincter to relax, and the esophagus may begin to contract unevenly, causing acid to reflux into the esophagus and cause heartburn.
Alcohol causes the lower esophageal sphincter to relax, and the esophagus may begin to contract unevenly, causing acid to reflux into the esophagus and cause heartburn.
Check your medications. Some medications can make symptoms worse. Do not interrupt the prescribed treatment without consulting your doctor. Drugs that have this effect include asthma and emphysema drugs (such as theophylline), anticholinergics for Parkinson's disease and asthma, sometimes found in over-the-counter drugs, some calcium channel blockers, alpha blockers, and beta-blockers to treat heart disease or high blood pressure, some drugs that affect the nervous system, iron supplements. nine0005
While some drugs exacerbate GERD symptoms, others can cause drug-induced esophagitis, a condition that causes the same symptoms as GERD but is not due to reflux. Drug esophagitis happens when a pill is swallowed but does not reach the stomach because it sticks to the wall of the esophagus. Because of this, the mucous membrane of the esophagus is corroded, chest pain, esophageal ulcers and pain during swallowing occur.