Foods to avoid if baby has milk protein allergy
Milk Allergy Diet | Johns Hopkins Medicine
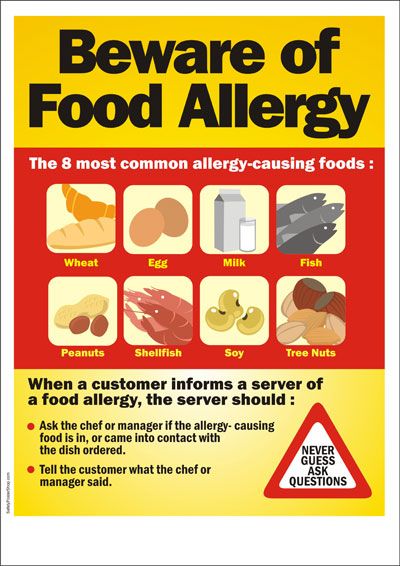
The key to an allergy-free diet is to avoid foods or products containing the food to which you are allergic. The items that you are allergic to are called allergens. Milk allergy is most common among infants and young children. Obvious forms of milk are cream, cheese, butter, ice cream, and yogurt. Milk and milk products may also be used as ingredients in many other foods. To avoid foods that contain milk and milk products, it is necessary to read food labels.
| Foods | Allowed | Not allowed |
|---|---|---|
| Beverages |
|
|
| Breads |
|
|
| Cereals |
|
|
| Desserts |
|
|
| Eggs |
|
|
| Fats |
|
|
| Fruits |
|
|
| Meats, fish, poultry, and cheese |
|
|
| Potatoes |
|
|
| Soups |
|
|
| Sweets |
|
|
| Vegetables |
|
|
| Miscellaneous |
|
|
Artificial butter flavor
Butter, butter fat, butter oil
Casein, casein hydrolysates
Caseinates (ammonium, calcium, magnesium, potassium, sodium)
Cheese, cottage cheese
Cream
Custard, pudding
Ghee
Half and Half
Hydrolysates (casein, milk protein, protein, whey, whey protein)
Lactalbumin, lactalbumin phosphate
Lactoglobulin, lactoferrin
Lactose, lactulose
Milk
-
Derivative, protein, solids, malted, condensed, evaporated, or dry
-
Whole, low-fat, nonfat, skim
-
Goat's milk and milk from other animals
Nisin
Nougat
Recaldent
Rennet casein
Sour cream or sour cream solids
Whey (delactosed, demineralized, protein concentrate)
Yogurt
Cow’s Milk Alternatives: Parent FAQs
By: Anthony Porto, MD, MPH, FAAP & Rachel Drake, MS, RD, CSO, CSP, CDN
Milk is a grocery list staple for many families.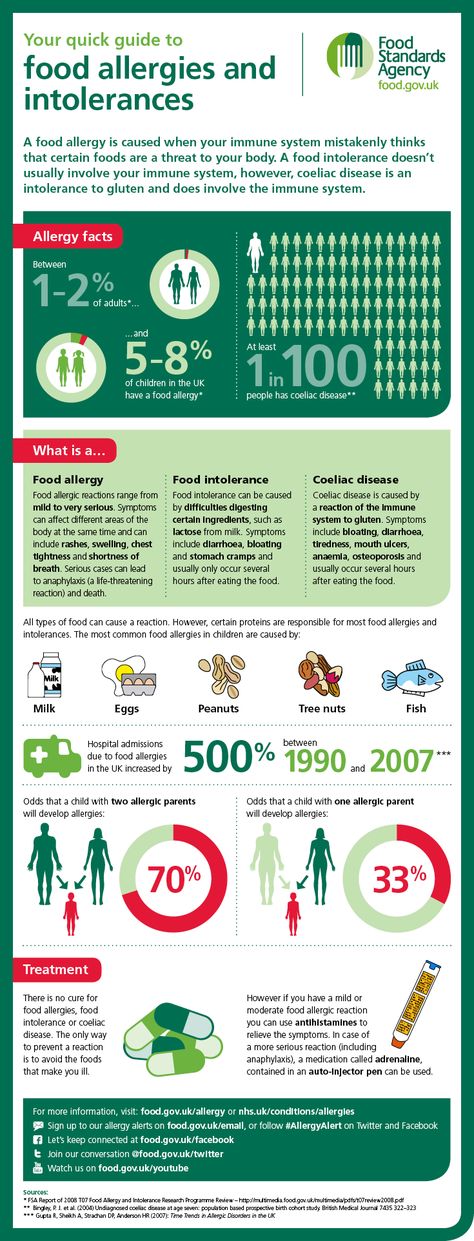 But some avoid it because of milk protein allergies or other health concerns. Some kids simply don't like the taste. These families may choose from a growing array of cow's milk alternatives that now fill the dairy aisle.
But some avoid it because of milk protein allergies or other health concerns. Some kids simply don't like the taste. These families may choose from a growing array of cow's milk alternatives that now fill the dairy aisle.
The nutritional content in the various dairy alternative products is important for parents to be aware of when shopping. Choices range from other animal-based beverages (such as goat's milk) to products made from nuts (such as almond milk), beans (such as soy milk), grains (such as oat) and other plants.
The American Academy of Pediatrics (AAP) knows that deciding what's best for your family can be confusing. To help you sort it all out, here are frequently asked questions from parents about cow's milk alternatives.
When do I introduce cow's milk into my baby's diet?
The AAP recommends
breast milk as the sole source of nutrition for your baby for about the first 6 months. If a baby is breastfed by a mother who is drinking cow's milk, or is formula fed with traditional infant formula, they have already been exposed to cow's milk protein. Most babies can begin consuming dairy foods around 6 months of age—after a few first
solid foods have been introduced. Plain, whole-fat or whole Greek yogurt is a good first form of cow's milk protein for babies to try. Avoid the added sugar commonly found in yogurt marketed to babies and toddlers.
If a baby is breastfed by a mother who is drinking cow's milk, or is formula fed with traditional infant formula, they have already been exposed to cow's milk protein. Most babies can begin consuming dairy foods around 6 months of age—after a few first
solid foods have been introduced. Plain, whole-fat or whole Greek yogurt is a good first form of cow's milk protein for babies to try. Avoid the added sugar commonly found in yogurt marketed to babies and toddlers.
Once a baby is developmentally able to eat finger foods, other dairy—such as pieces of cheese—can be added. The AAP recommends that whole cow's milk and low-iron formulas not be used during the first year of life, because babies' digestive systems under age one year old may not tolerate the cow's milk protein in large quantities. Low-iron formulas can also lead to anemia. Note: Low-iron formulas are no longer marketed routinely in the United States.
What if my baby is allergic to cow's milk?
If your formula-fed baby has a cow's milk allergy, ask your pediatrician about switching to a non-cow's milk, protein-based formula. Hypoallergenic formulas are cow's milk based; only soy formulas are not. Discuss these options with your child's pediatrician before switching.
Hypoallergenic formulas are cow's milk based; only soy formulas are not. Discuss these options with your child's pediatrician before switching.
According to a study published in Pediatrics, there is not enough evidence for breastfeeding mothers to routinely avoid allergenic foods—like cow's milk—while breastfeeding.
If your pediatrician diagnoses your baby with a cow's milk protein allergy, then they may recommend you remove cow's milk from your diet while breastfeeding. Be aware that it can take several weeks for the milk protein to disappear entirely. The AAP does not currently have an official recommendation on this issue.
After your baby's first birthday, they may begin using cow's milk alternatives or occasionally change to a toddler version of the formulas mentioned above. Many infants diagnosed with allergic colitis caused by cow's milk protein, including healthy babies with rectal bleeding, may safely begin cow's milk at a year or so of age. Your pediatrician can help you make this decision.
Your pediatrician can help you make this decision.
What kinds of cow's milk alternatives are available?
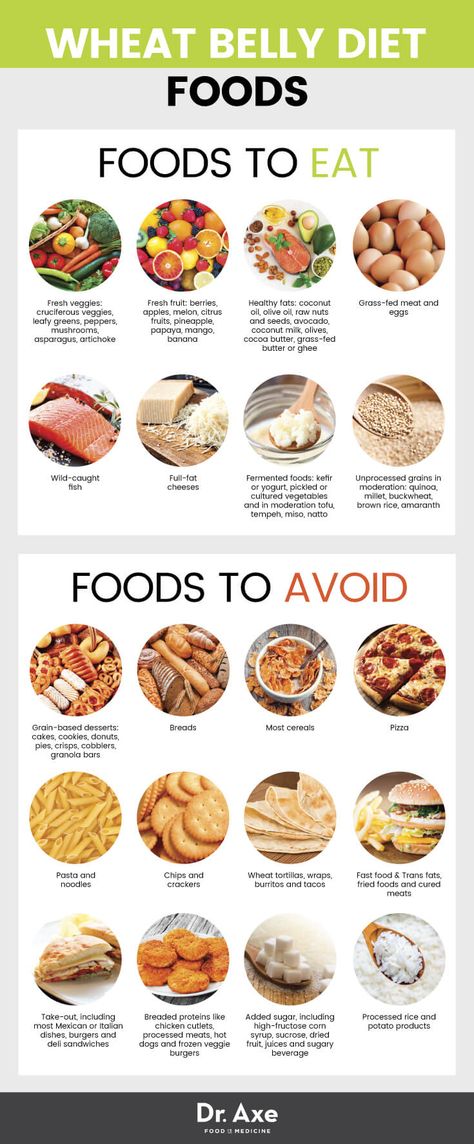
While soy milk has traditionally been the most commonly used cow's milk alternative, there are many options available. In addition, soy protein should also be avoided if your child is diagnosed with an allergy to cow's milk protein. This is because 50% of infants with cow's milk protein allergy may also have cross reactivity with the soy protein.
Use of tree nut milk, including almond and cashew milks, have become increasingly popular. Rice and oat milk, as well as hemp milk, are also possible alternatives. Some of these alternatives are flavored, for example with chocolate and vanilla. Keep in mind that these often contain added sugar and calories. It is best to avoid sugar-sweetened beverages for children under 2 years of age, and also limit them for older children as much as possible.
What are the differences among cow's milk alternatives?
Cow's milk alternatives often contain less protein and less calories in comparison to cow's milk. Most are fortified with vitamin D and calcium. It is important to
check labels since protein and vitamin content may differ among brands.
See the chart for a comparison of common unflavored milk alternatives.
Most are fortified with vitamin D and calcium. It is important to
check labels since protein and vitamin content may differ among brands.
See the chart for a comparison of common unflavored milk alternatives.
Comparison of common unflavored milk alternatives | ||||||||
|
Whole Milk (1 cup) |
Rice Milk (1 cup) |
Soy Milk (1 cup) |
Coconut Milk (1 cup) |
Almond Milk (1 cup) |
Oat Milk (1 cup) |
Hemp Milk (1 cup) | Pea Milk (1 cup) | |
Energy (kcal) | 149 | 115 | 105 | 76 | 37 | 130 | 70 | 80 |
Protein (g) | 7. | 0.68 | 6.34 | 0.51 | 1.44 | 4 | 3 | 8 |
Total fat (g) | 7.93 | 2.37 | 3.59 | 5.08 | 2.68 | 2.5 | 5 | 4.5 |
Saturated fat (g) | 4.55 | 0 | 0.5 | 5.083 | 0 | 0 | 0.5 | 0.5 |
Cholesterol (mg) | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Carbohydrate (g) | 11. | 22.37 | 12 | 7.12 | 1.42 | 24 | 1 | < 1 |
Calcium (mg) | 276 | 288 | 300 | 459 | 481 | 350 | 300 | 440 |
Iron (mg) | 0.07 | 0.49 | 1.02 | 0.73 | 0.85 | 1.8 | 1.8 | 0 |
Vitamin D (IU) | 128 | 96 | 108 | 96 | 96 | 100 | 100 | 110 |
Note: Homemade almond milk or other homemade milk alternatives do not contain the same number of vitamins, because they are not fortified. | ||||||||
How much dairy is recommended for my child?
Infants' diets primarily consist of dairy to help them meet their caloric needs for growth. In addition, dairy provides enough fat needed for brain and eye development.
At one year, babies should consume approximately 2 servings of dairy per day, or about 16 to a maximum of 24 ounces of whole milk per day. Whole-fat milk is recommended for children at this age, unless there is a family history or risk for obesity or heart disease. Talk with your child's pediatrician about which milk they recommend for your one-year-old child.
Between two and three years old, children should consume 2.5 servings of dairy per day. The AAP recommends that children stay on whole milk until they are two years of age—unless there is a reason to switch to low-fat milk sooner. Whole milk contains approximately 4% milk fat. It may help to gradually switch your child from whole milk to a lower-fat milk.
 Therefore, many pediatricians recommend that children get reduced fat (2%) milk for a few weeks before switching them to low fat (1%) or no fat (skim) milk. If your child cannot drink cow's milk, they can meet their dairy requirements by eating yogurt and cheese. However, they may need a vitamin D supplement since not all yogurts are fully supplemented with vitamin D. Talk with your child pediatrician before giving your child any supplements.
Therefore, many pediatricians recommend that children get reduced fat (2%) milk for a few weeks before switching them to low fat (1%) or no fat (skim) milk. If your child cannot drink cow's milk, they can meet their dairy requirements by eating yogurt and cheese. However, they may need a vitamin D supplement since not all yogurts are fully supplemented with vitamin D. Talk with your child pediatrician before giving your child any supplements.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age. Here is a breakdown of the recommended dietary allowances (RDA) for calcium and
vitamin D.
Recommended Dietary Allowances for Calcium and Vitamin D | ||
| Age |
Amount of Calcium Per Day |
Amount of Vitamin D Per Day |
0 to 6 months | 200 mg | 400 IU |
7 to 12 months | 260 mg | 400 IU |
1 to 3 years | 700 mg | 600 IU |
4 to 8 years | 1000 mg | 600 IU |
9 to 18 year | 1300 mg | 600 IU |
More information
-
Infant Allergies and Food Sensitivities
- Why Formula Instead of Cow's Milk?
- Where We Stand: Soy Formulas
- Choosing a Formula
- Lactose Intolerance in Infants & Children: Parent FAQs
- Ask the Pediatrician:
My preschooler refuses to drink milk.
 What should we do?
What should we do? - The Use of Soy Protein-Based Formulas in Infant Feeding (AAP Policy Statement)
About Dr. Porto:
Anthony Porto, MD, MPH, FAAP is a board-certified pediatrician and board-certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's
Real Answers, and is the co-author of
The Pediatrician's Guide to Feeding Babies and Toddlers. |
About Ms. Drake:Rachel Drake, MS, RD, CSO, CSP, CDN is a is a registered dietitian-nutritionist practicing in Connecticut. She is a board-certified specialist in pediatric nutrition through the Academy of Nutrition and Dietetics and the former Chair of the Failure to Thrive, Gastroenterology & Allergy specialty group within the
Pediatric Nutrition Practice Group of the Academy of Nutrition and Dietetics. In 2015, Ms. Drake was honored by the Academy of Nutrition and Dietetics as the
Recognized Young Dietitian of the Year for the state of Connecticut. She lives in Connecticut with her husband and young daughter. |
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.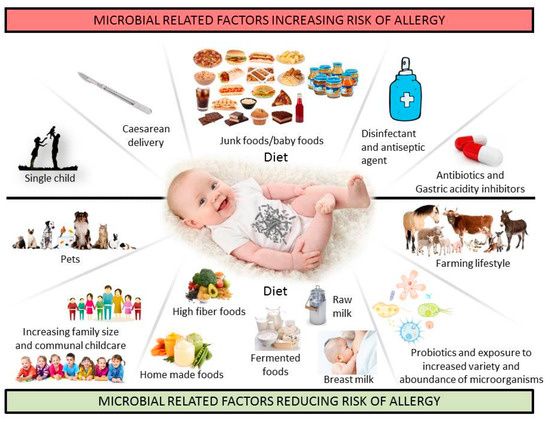
Diet for milk allergy
Cow's milk and products containing it are excluded from the diet. Although cow's milk and goat's milk are similar in antigenic composition, some patients with cow's milk allergy tolerate goat's milk. In order to avoid the use of ready-made products containing cow's milk, you should always study their composition on the packaging.
Some products containing milk:
- Skimmed milk powder
- Powdered milk
- Oil
- Whey
- Curd
- Lactose
- Margarine
- Casein
- Casein hydrolyzate
- Ice cream
- Cheese
Since the composition of any product is subject to change, it is necessary to study the packaging even of previously consumed products.
Dishes excluded from the diet:
1. Soups - Puree soups and other soups based on or containing milk.
2. High protein foods - Cheese, cottage cheese, sausages (e.g. sausages, smoked sausage) containing milk and milk components, beef, fish, poultry (breaded or with white sauce), egg dishes with the addition of dairy products.
3. Potatoes and other side dishes - Any food containing milk and its components (eg mashed potatoes, macaroni and cheese).
4. Vegetables - Any vegetable products with the addition of milk and its components (for example spinach puree).
5. Bakery products - Any bakery products with the addition of milk and its components:
- donuts
- pancakes
- pancakes
- wafers
- dry biscuits
- biscuit rolls
- biscuits
6. Cereal dishes — Dishes prepared with milk, prepared foods with the addition of milk or its components.
Cereal dishes — Dishes prepared with milk, prepared foods with the addition of milk or its components.
7. Fats - Butter, cream, salad dressings, mayonnaise and margarine containing milk or milk ingredients.
8. Sweet dishes — Any sweet dishes containing milk or its components, ready-made pies, cakes, biscuits, puddings, ice cream, sherbets, yoghurts, dry mixes.
9. Milk Whole cow's milk, skimmed milk, skimmed milk powder, sweetened or unsweetened condensed milk, yoghurt, cow's milk infant formula, cocoa with milk.
10. Beverages — Beverages with added milk:
- cocoa
- milkshakes
- alcoholic drinks with cream
11. Other products — Milk chocolate, cream sauce, whey, cottage cheese, products fried in butter, fried in breadcrumbs, cheese, dough, low quality chocolate. ⠀
⠀
what causes it, how it manifests itself, how to replace milk
Do you think that the body somehow reacts to milk incorrectly? Perhaps you don't think so! We tell you what a milk allergy is, how to detect it and what to do next.
Ksenia Yakushina
Tags:
Health
Nutrition
Shutterstock
How does a milk allergy occur, is there a difference between it and lactase deficiency, and what if you can't eat dairy products at all? We understand in this article.
Table of Contents
Milk allergy is second only to peanut and tree nut allergies. It happens to both adults and children, although the latter quite often outgrow it. This type of allergy is based on a disruption in the functioning of the immune system: it regards the components of milk as substances dangerous to the body and, accordingly, attacks them, destroying them, and the classic allergy symptoms appear along the way. Approximately every 50th child suffers from an allergy to milk components, in adults the incidence is lower - about 1%, but even 1-2% is millions of people. Most often, an allergy occurs to cow's milk proteins, however, sheep, goat, and other types of milk can also cause allergies. The only completely hypoallergenic milk is breast milk, if a baby develops an allergy to breast milk, then most likely some substances from the food that the mother consumed got into it. The danger of many products is greatly exaggerated, but the main milk protein - casein - is really able to penetrate into breast milk.
Approximately every 50th child suffers from an allergy to milk components, in adults the incidence is lower - about 1%, but even 1-2% is millions of people. Most often, an allergy occurs to cow's milk proteins, however, sheep, goat, and other types of milk can also cause allergies. The only completely hypoallergenic milk is breast milk, if a baby develops an allergy to breast milk, then most likely some substances from the food that the mother consumed got into it. The danger of many products is greatly exaggerated, but the main milk protein - casein - is really able to penetrate into breast milk.
Causes of milk allergy
In total, mammalian milk contains more than 20 major proteins, each of which the immune system can respond to. The casein already mentioned above is the cause of most cases of allergy to dairy products, the concentration of casein proteins in these products is higher than in all others, respectively, and the reaction to them occurs more often. Also, there is often an allergy to milk proteins contained in whey: lactoglobulin or albumins. By the way, whey proteins can contain not only milk, but also meat, so if you are allergic to them, then you may have to give up steaks or tartare. In case of an allergy to whey proteins, the patient is a little easier: when heated, these proteins break down, respectively, you can drink, for example, boiled milk. It doesn't work with casein. The safest component of milk is lactic acid, but it can sometimes cause problems. A reaction can occur only to a certain type of milk, or maybe to the milk of all mammals except humans. That is why - in order to avoid allergies - whole milk is introduced to children quite late and it is recommended to feed only breastfeeding for at least six months.
Also, there is often an allergy to milk proteins contained in whey: lactoglobulin or albumins. By the way, whey proteins can contain not only milk, but also meat, so if you are allergic to them, then you may have to give up steaks or tartare. In case of an allergy to whey proteins, the patient is a little easier: when heated, these proteins break down, respectively, you can drink, for example, boiled milk. It doesn't work with casein. The safest component of milk is lactic acid, but it can sometimes cause problems. A reaction can occur only to a certain type of milk, or maybe to the milk of all mammals except humans. That is why - in order to avoid allergies - whole milk is introduced to children quite late and it is recommended to feed only breastfeeding for at least six months.
ADVERTISING - CONTINUED BELOW
It is definitely necessary to separate allergy to milk and lactase deficiency - these two diseases have a completely different nature.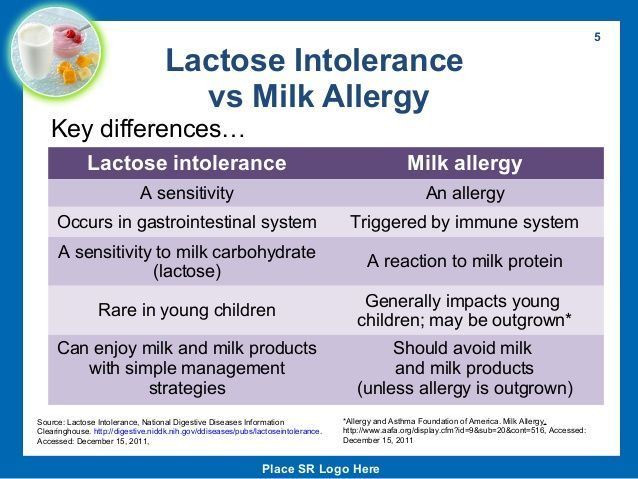 Allergies are based on an immune reaction, when cells of the immune system try to destroy proteins supposedly hostile to the body, releasing histamines (they are the ones that provoke symptoms). Lactase deficiency, or milk intolerance, appears due to a lack of an enzyme that breaks down lactose, milk sugar. This enzyme is called lactase, and its job is to produce galactose and glucose from lactose, which must then be absorbed in the intestines.
Allergies are based on an immune reaction, when cells of the immune system try to destroy proteins supposedly hostile to the body, releasing histamines (they are the ones that provoke symptoms). Lactase deficiency, or milk intolerance, appears due to a lack of an enzyme that breaks down lactose, milk sugar. This enzyme is called lactase, and its job is to produce galactose and glucose from lactose, which must then be absorbed in the intestines.
If there is not enough or no lactase at all, lactose remains unchanged in the body. It is actively consumed by microorganisms living in the intestines, and at the same time produce gas, as well as excess lactose creates excessive pressure in the gastrointestinal tract. As a result, flatulence, diarrhea, abdominal pain and other symptoms occur. In part, these manifestations are similar to the likely signs of allergy to cow's milk proteins, allergies to goat's milk and milk of other animal species, however, in fact, the causes of lactase deficiency have nothing to do with allergic reactions. However, in both cases, genetics plays a certain role, for example, among Europeans, lactase deficiency is not very common, but among people with Asian or Indian roots, the majority suffers from it.
However, in both cases, genetics plays a certain role, for example, among Europeans, lactase deficiency is not very common, but among people with Asian or Indian roots, the majority suffers from it.
Since we are talking about what can increase the risk of developing the disease, let's clarify this for allergies. So, increase the likelihood that you or your child is allergic to milk:
- the presence of other allergies. There are very frequent situations when a person is allergic to both milk and something else, but it happens that a reaction to dairy products first develops, and only then to something else;
- atopic dermatitis. This is a risk factor for food allergies in general, especially in children;
- heredity. If the parents have some kind of allergies, then the likelihood that the child will also have them increases. This applies to any allergic reactions, say, if the father has eczema and the mother has hay fever, their son or daughter may have a food allergy, including milk;
- age.
 Children are more likely to react to milk than adults because it is difficult for their bodies to process it. Over time, the allergy may disappear;
Children are more likely to react to milk than adults because it is difficult for their bodies to process it. Over time, the allergy may disappear; - immunosuppressed;
- prematurity - in this case, not all body systems can function correctly, including allergic reactions;
- stress, adverse environmental conditions - these factors can also affect the body.
- disorders of the gastrointestinal tract.
How milk allergy manifests itself
Like other food allergies, a reaction to milk can occur immediately, within minutes, or it can be delayed for several hours or even days. An allergy to milk in an adult, on average, manifests itself earlier than in a child.
An immediate reaction immediately following consumption of milk may be:
- hives;
- wheezing;
- itching around the mouth;
- swelling of lips, tongue, throat;
- cough;
- shortness of breath;
- vomiting.

Delayed reaction may look like this:
- diarrhea, loose stools, sometimes with blood;
- abdominal cramps and pains;
- runny nose;
- increased tearing;
- rash;
- lethargy;
- babies can get colic.
In the long term, allergies can turn into eczema or asthma. Young children may experience growth retardation.
Infrequent, subtle symptoms include joint pain, fatigue and inability to lose weight - this can also be due to milk.
It is important to know that an immune reaction to milk can cause anaphylactic shock: severe laryngeal edema prevents a person from breathing, hypoxia develops, blood pressure drops, loss of consciousness is possible. In these cases, it is necessary to immediately call an ambulance, in 10-20% of cases, anaphylactic shock is fatal. Thus, the answer to the question whether a milk allergy can be dangerous is unambiguous: yes, maybe it can even kill a person, so it’s absolutely impossible to joke with it.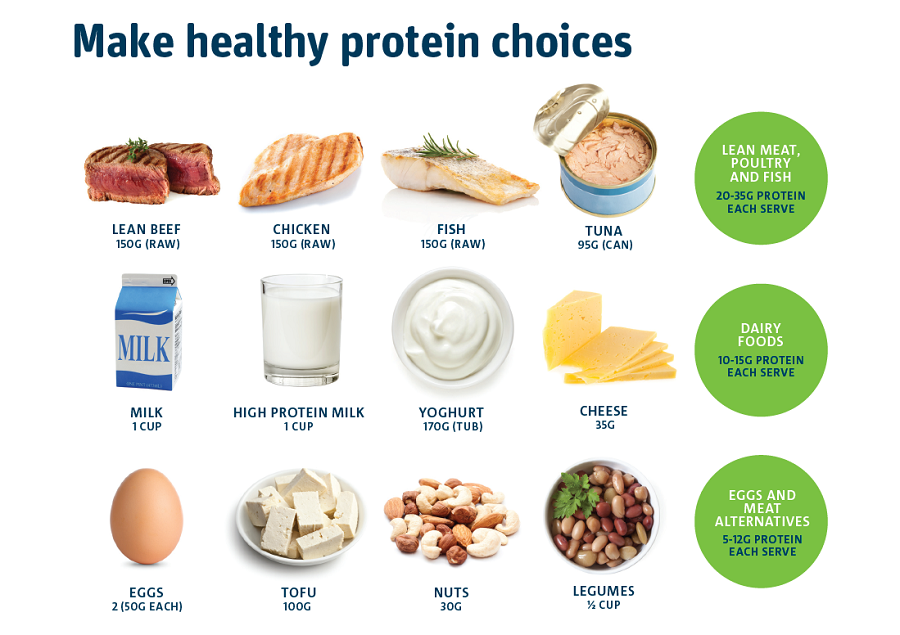
Allergic reaction to milk: diagnosis and treatment
If you suspect a milk allergy in yourself or a child, contact an allergist. The doctor will ask you:
- Have there been cases of allergies in the family, what, who?
- What exactly did you or your child eat (what food), when, in what quantities?
- What specific allergy symptoms did you notice, when did they start and how long did they last?
- What did you or your child take to help relieve the condition?
In addition, the doctor may refer a probable allergic person to skin tests, recommend taking an IgE antibody test, making an immunogram, conducting a provocative test - ingesting a little allergen and observing the reaction (of course, if before that milk did not cause strong reactions, such as anaphylactic shock, no one will risk the patient's life).
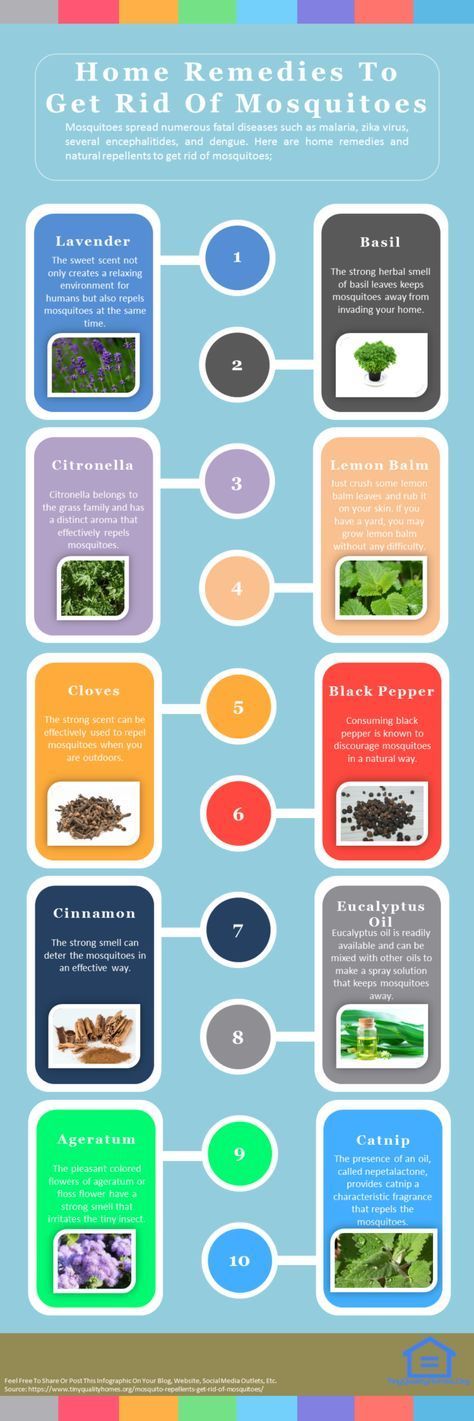
Depending on how the allergy to cow's milk (or the milk of other animals) manifests itself, different treatment regimens are used. First of all, all dairy products are excluded: not only whole milk, but also everything that is produced from it. At the same time, you need to not only stop buying dairy products, but also carefully study the composition of absolutely any food, because milk can be anywhere. Antihistamines, sorbents that help remove excess substances from the body, probiotics and, in case of severe allergies, hormonal preparations are prescribed as drug therapy.
First of all, all dairy products are excluded: not only whole milk, but also everything that is produced from it. At the same time, you need to not only stop buying dairy products, but also carefully study the composition of absolutely any food, because milk can be anywhere. Antihistamines, sorbents that help remove excess substances from the body, probiotics and, in case of severe allergies, hormonal preparations are prescribed as drug therapy.
Milk allergy: menu
If milk causes allergies, certain foods may need to be completely eliminated from the diet:
- milk itself;
- butter and ghee;
- cheese;
- yogurt;
- cottage cheese;
- cheese and milk sauces;
- milk powder;
- condensed milk;
- ice cream;
- cream;
- milkshakes;
- anything with cream in it;
- puddings.
Milk may not be listed in the composition of some products, but nevertheless it is often present, so you need to be careful with them:
- chocolate and chocolates;
- pastries and any products in dough;
- cereals, instant soups;
- chewing gum;
- margarine;
- various coffee additives;
- mashed potatoes;
- semi-finished products;
- nougat;
- salad dressings;
- sausages and related products;
- sherbet.
Some ingredients may also indicate the presence of milk proteins. These are, for example:
- any ingredients containing "lacto" in the name;
- Kurdish;
- casein or caseinates;
- ghee;
- hydrolysates;
- serum.
The cheesy flavor of some snacks may also be based on milk proteins.
Of course, these lists are incomplete, since it is simply impossible to provide comprehensive information on all possible ingredients. Over time, you will learn to isolate the information you need from the composition of products. Try not to eat unfamiliar foods until you are sure that they do not contain anything that causes you a negative reaction.
Thus, if the question arises of what to feed yourself or a child with an allergy to milk, you can focus on the composition of the products and the above stop lists. What can replace milk for allergies? Since the reaction is most often to protein, almost any plant-based substitutes will do: soy, rice, oat, almond milk.

 69
69 71
71
 Follow him on Instagram
@Pediatriciansguide.
Follow him on Instagram
@Pediatriciansguide.