Baby led weaning food allergies
Baby-Led Weaning & Early Introduction of Top Allergens – Managing Peanut Allergies
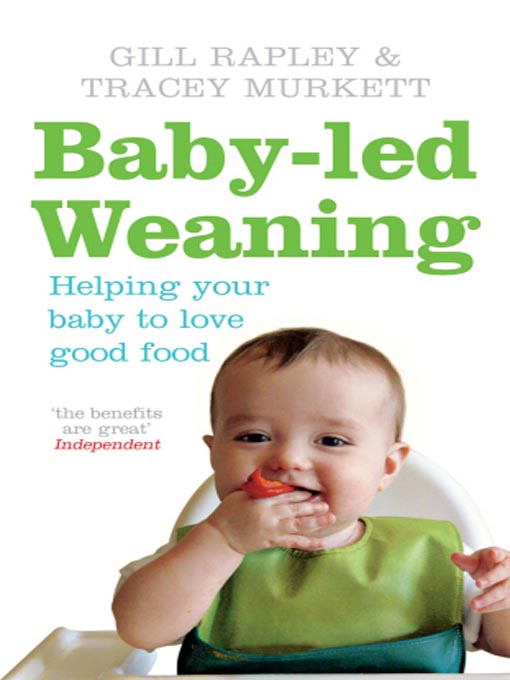
The way we feed babies has changed dramatically over the past twenty years or so. While not a new approach to the introduction of solid foods, “baby-led weaning” (BLW) has become more mainstream and understood as a beneficial and viable option with evidence-based short- and long-term benefits.
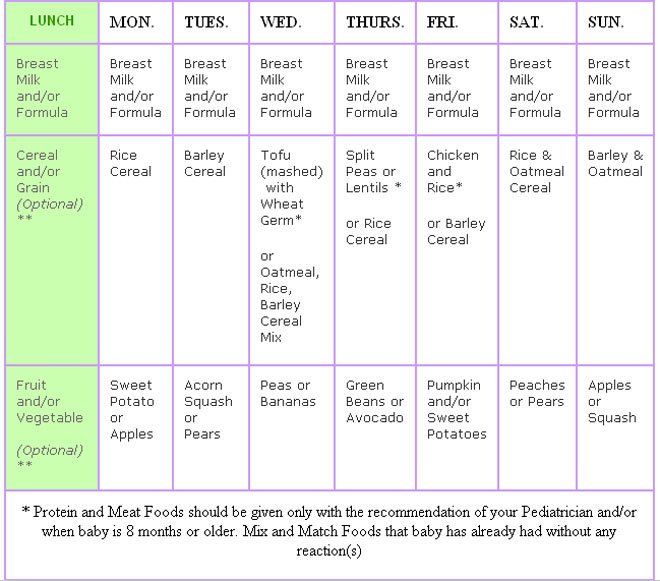
Scientific evidence supporting the early introduction of top allergenic foods during infancy for the prevention of food allergies has also grown. In fact, the new 2020-2025 Dietary Guidelines for Americans recommend offering top allergens (egg, peanut, tree nut, cow’s milk, fish, shellfish, soy, and wheat) early and often starting at about 6 months of age when babies are showing signs of readiness for complementary foods (in conversation with the pediatrician if babies are at high risk for food allergies).[vii]
The good news is that BLW is incredibly compatible with the early introduction of top allergens and can ease the process of offering these foods during infancy.
BLW is defined as the process of starting a baby on complementary foods using appropriately sized and textured finger-foods for self-feeding, starting at about 6 months of age with signs of readiness. It offers many advantages, however what makes it so unique is the “baby-led” aspect. As opposed to being passively spoon-fed, babies self-feed and decide whether and how much to eat, strengthening their own internal self-regulation systems, and boosting fine motor skills.[i] BLW promotes an earlier integration of babies into family meals, less picky eating in early childhood, healthier overall food preferences, and more adventurous eating.[ii],[iii],[iv],[v] Easier in general for caregivers, it saves both money and time, as babies can eat the family meal with some minor adjustments (such as reserving a portion for baby before adding salt), reducing the need to purchase baby food and/or prepare separate meals.
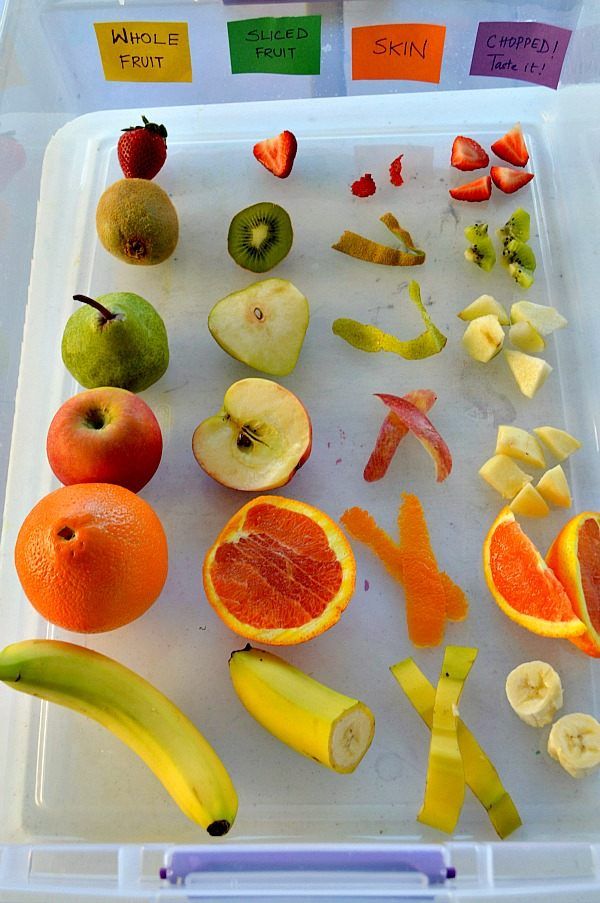
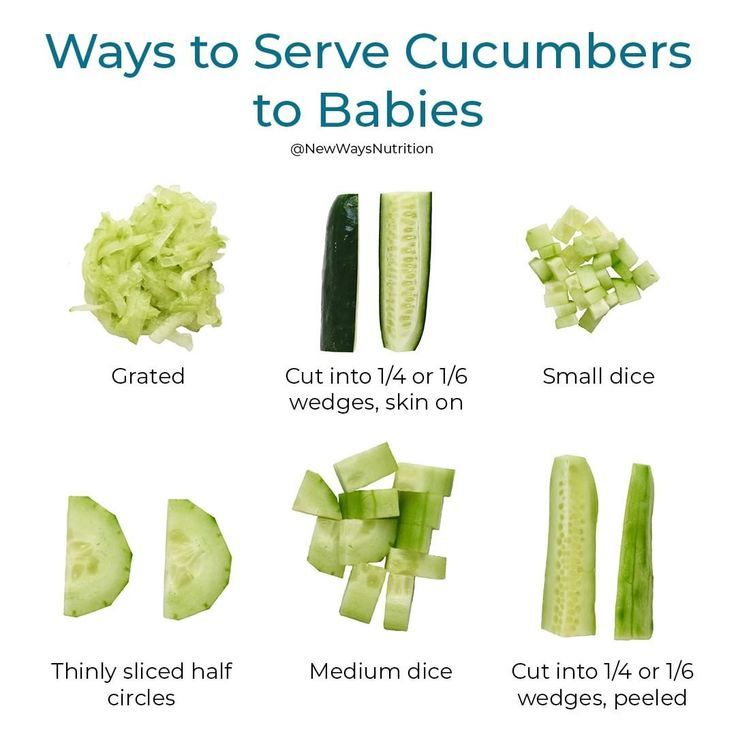
A common misconception about BLW is that offering finger foods during infancy increases choking risk, however studies actually show that when parents are educated on food sizing and texture, BLW does not increase the likelihood of choking. [vi] Additionally, how we size finger foods for babies does not depend on the baby’s age or number of teeth, but rather which type of developmental grasp they use to pick up pieces of food. At about 6 months, most babies use a palmar grasp and stick-shaped foods the size of an adult pinky-finger or larger are best. Usually by about 9 months of age (although babies each develop on their own timeline) most start using a pincer grasp and small chickpea-sized bites work best. Regardless of food size, the texture of foods should be soft and easily smashible between the fingers. This makes foods more manageable in the baby’s mouth and reduces overall choking risk.
[vi] Additionally, how we size finger foods for babies does not depend on the baby’s age or number of teeth, but rather which type of developmental grasp they use to pick up pieces of food. At about 6 months, most babies use a palmar grasp and stick-shaped foods the size of an adult pinky-finger or larger are best. Usually by about 9 months of age (although babies each develop on their own timeline) most start using a pincer grasp and small chickpea-sized bites work best. Regardless of food size, the texture of foods should be soft and easily smashible between the fingers. This makes foods more manageable in the baby’s mouth and reduces overall choking risk.
Another common misconception about BLW is that purees are not allowed. Purees are an important texture for babies to learn and can be served in a way that supports self-feeding by offering on a pre-loaded spoon. Further, there is no evidence that taking a combined approach and using both BLW and spoon-feeding is detrimental. In the end, it comes down to what works best for the caregivers and baby.
In the end, it comes down to what works best for the caregivers and baby.
Practical ways to build top allergenic foods into a baby’s diet during BLW include offering:
- Pieces of scrambled or hard-boiled egg and strips of frittata or quiche (eggs are an excellent, nutrient-dense first food for babies with a soft texture that lends itself to infant feeding)
- Peanut or tree nut butters stirred into yogurt, thinned with breast milk or water, cooked into muffins or pancakes, or spread in a thin layer on a finger of toast (note that whole tree nuts, peanuts and globs of any type of nut butter are a choking hazard for babies)
- Peanut powder – delicious in apple fritters (see recipe!) and peanut snacks such as Mission Mighty Me, Bamba and Puffworks
- Full-fat yogurt and low-sodium softer cheeses such as ricotta, mascarpone and mozzarella which offer baby-friendly ways to introduce cow’s milk
- Fish and/or shellfish cooked into fritters or shredded and served in a sauce for pasta
- Tender-cooked, smashed edamame for babies using a pincer grasp, or tofu cut into strips
- Wheat offered in soft fingers of pancake, toast or waffle, baked into muffins, or stirred into yogurt or applesauce in the form of wheat germ
Ultimately, how to feed a baby is a personal choice. The caregiver can rest in the knowledge that throughout baby’s first year, breast milk/formula will continue to be the main source of nutrients while self-feeding skills develop. If there is any concern about a food allergy, caregivers should always consult the pediatrician and/or allergist who will guide next steps. Regardless of the feeding method used – traditional, BLW or a combination of both – caregivers can help set their babies on a long-term healthy path by recognizing, listening and responding to the baby’s cues for hunger and fullness, diversifying the baby’s diet and offering a wide variety of foods, reducing the baby’s risk of developing food allergies by building top allergenic foods into meals early and often, and finding the joy and connection in eating together.
The caregiver can rest in the knowledge that throughout baby’s first year, breast milk/formula will continue to be the main source of nutrients while self-feeding skills develop. If there is any concern about a food allergy, caregivers should always consult the pediatrician and/or allergist who will guide next steps. Regardless of the feeding method used – traditional, BLW or a combination of both – caregivers can help set their babies on a long-term healthy path by recognizing, listening and responding to the baby’s cues for hunger and fullness, diversifying the baby’s diet and offering a wide variety of foods, reducing the baby’s risk of developing food allergies by building top allergenic foods into meals early and often, and finding the joy and connection in eating together.
Recipe: Peanut Apple Fritters
Soft, juicy and without added sugar or salt, these peanut apple fritters offer an easy and nutrient-dense way to serve peanuts to babies who are at least 6 months of age and showing signs of readiness for solid foods.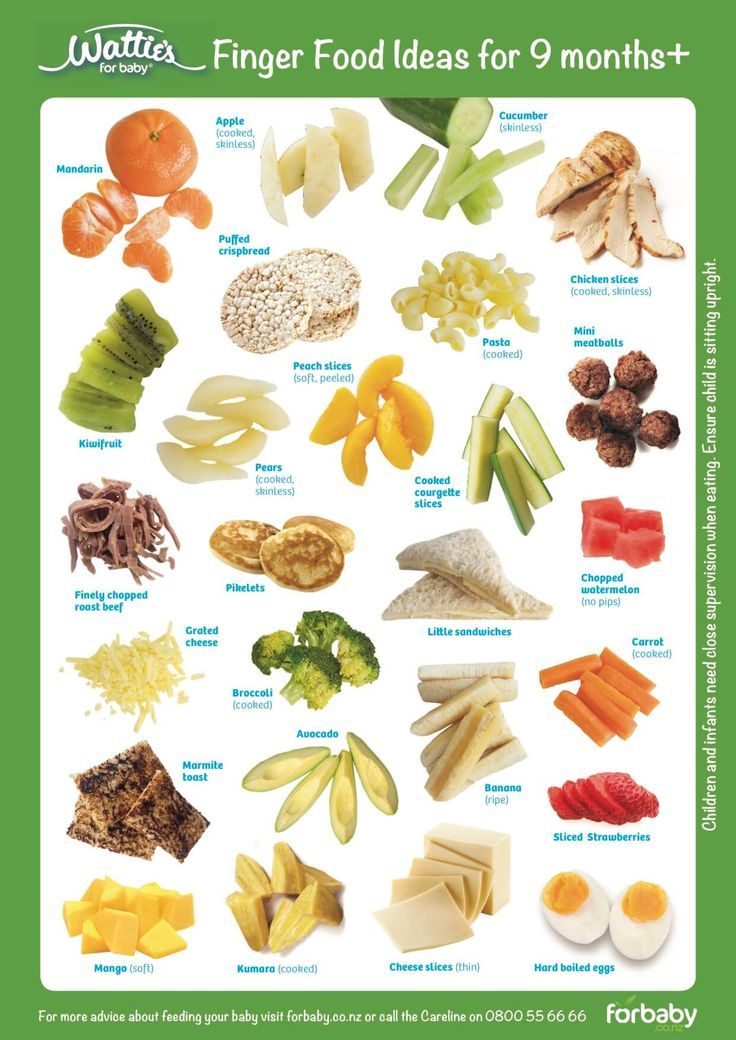 Cut fritters into strips for babies using a palmar grasp (usually 6-9 months of age), or small chickpea-sized bites for babies using a pincer grasp (usually 9-12 months of age).
Cut fritters into strips for babies using a palmar grasp (usually 6-9 months of age), or small chickpea-sized bites for babies using a pincer grasp (usually 9-12 months of age).
Prep time: 10 minutes
Freeze time: 10 minutes
Ingredients
- 1/2 cup peanut flour
- 1/2 cup oat flour
- 2 teaspoons baking powder
- 2 teaspoons lemon juice
- 2 large eggs at room temperature
- ¼ cup whole milk
- 2 large apples, peeled and diced
- Peanut (or vegetable) oil for frying
Directions
- Wash, peel, core and dice apples, place in a medium bowl and toss with lemon juice to prevent browning.
- In a separate medium bowl, whisk together the flour and baking powder.
- Add eggs and milk to the flour mixture and whisk until combined.
- Fold in the diced apples.
- In a cast iron or other frying pan, add ¼ inch oil and heat over medium-high heat until oil reaches a temperature of about 375°F using an instant read thermometer.

- Drop about ¼ cup batter into oil and fry until golden brown, then flip and fry the other side until golden brown as well. (Test doneness by inserting a small knife into the center of a fritter. If it does not come out clean, fry a little longer.)
Note: Fritters last for up to 5 days in the refrigerator. Reheat for about 5 minutes in the toaster oven. They also freeze well and can last for up to 2 months in the freezer when wrapped tightly in plastic wrap and stored in an airtight freezer bag or container.
Recipe: Mascarpone Peanut Butter Melts
Love this easy way to offer babies flavor, teething relief, an interesting texture that melts in the mouth, an early exposure to two top allergenic foods (peanut and cow’s milk) and lots of nutrients babies need, like protein, fat, fiber, vitamins & minerals! These are best for babies who are at least 6 months of age and using a pincer grasp. (The pincer grasp usually emerges around 9 months but can show up before and/or after; babies are each on their own developmental timeline!) If still using a palmar grasp, they may get frustrated if they can’t pick up the melt. Don’t skip the spices – the more flavors babies experience during infancy, the more likely they will be accepting of a wide range of flavors down the road.
Don’t skip the spices – the more flavors babies experience during infancy, the more likely they will be accepting of a wide range of flavors down the road.
Prep time: 10 minutes
Freeze time: 2 hours
Ingredients
- 1/2 cup mascarpone cheese
- 1/2 banana
- 1 pinch allspice
- 1 pinch ground cloves
- 1 pinch cinnamon
- 1 tablespoon smooth peanut butter
Directions
- In a small bowl, mash the banana with a fork until it is liquified – a few lumps are ok
- Add the mascarpone cheese and spices and mix until well combined
- Add the peanut butter into the mixture and stir well so that the peanut butter is completely incorporated into the mixture
- Using a 1/2 teaspoon measuring spoon, drop dime-sized spoonfuls of the mixture on a parchment-paper lined sheet pan that will fit into your freezer and freeze for at least 2 hours
- Remove from freezer and serve immediately as a finger food for babies using a pincer grasp
Note: Melts will last for up to 2 months in the freezer.
References:
[i] Morison, Brittany, Rachael Taylor, Jillian J. Haszard, Claire J. Schramm, Liz Williams Erickson, Louise J. Fangupo, Elizabeth A. Fleming, et al. “How Different Are Baby-Led Weaning and Conventional Complementary Feeding? A Cross-Sectional Study of Infants Aged 6-8 Months.” BMJ Open 6, no. 5 (May 2016): e010665 doi.org/10/1136/bmjopen-2015-010665
[ii] Morison, Brittany, Rachael Taylor, Jillian J. Haszard, Claire J. Schramm, Liz Williams Erickson, Louise J. Fangupo, Elizabeth A. Fleming, et al. “How Different Are Baby-Led Weaning and Conventional Complementary Feeding? A Cross-Sectional Study of Infants Aged 6-8 Months.” BMJ Open 6, no. 5 (May 2016): e010665 doi.org/10/1136/bmjopen-2015-010665
[iii] Taylor, Rachael W., Sheila Williams, Louise J. Fangupo, Benjamin John Wheeler, Barry J. Taylor, Lisa Daniels, Elizabeth A. Fleming, et al. “Effect of a Baby-Led Approach to Complementary Feeding on Infant Growth and Overweight: A Randomized Clinical Trial. ” JAMA Pediatrics 171, no.9 (September 2017): 838-46. Doi.org/10.1001/jamapediatrics.2017.1284.
” JAMA Pediatrics 171, no.9 (September 2017): 838-46. Doi.org/10.1001/jamapediatrics.2017.1284.
[iv] Van der Horst, Klazine, and Ester F. C. Sleddens. “Parenting Styles, Feeding Styles and Food-Related Parenting Practices in Relation to Toddlers’ Eating Styles: A Cluster-Analytic Approach.” PLOS ONE 12, no. 5 (May 2017): e0178149. Doi.org/10.1371/journal.pone.0178149.
[v] Townsend Ellen, Nicola Pitchford. “Baby Knows Best? The Impact of Weaning Style on Food Preferences and Body Mass Index in Early Childhood in a Case–Controlled Sample.” BMJ Open 2, no. 1 (January 2012): e000298. doi.org/10.1136/bmjopen-2011-000298.
[vi] Brown, Amy E. “No Difference in Self-Reported Frequency of Choking Between Infants Introduced to Solid Foods Using a Baby-Led Weaning or Traditional Spoon-Feeding Approach.” Journal of Human Nutrition and Dietetics 31, no. 4 (December 2017): 496-504. Doi.org/10.1111/jhn.12528.
[vii] https://www. dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
Research & Allergies - Baby Led Weaning Ideas
Human milk provides virtually all the protein, sugar, and fat your baby needs to be healthy, and it also contains many substances that benefit your baby’s immune system, including antibodies, immune factors, enzymes, and white blood cells. These substances protect your baby against a wide variety of diseases and infections not only while he is breastfeeding but in some cases long after he has weaned. (read more here)
- Infants should be breastfed exclusively during the first 6 months of life.
- From 6 months of age, breast milk should be complemented with a variety of adequate, safe and nutrient dense complementary foods. Salt and sugars should not be added to complementary foods.”
- Breastfeeding is recommended for at least 6 months or ranging up to 2 years of age and beyond, for as long as mother and infant wish to continue.
- There is no consistent evidence that breastfeeding is effective for the prevention of allergic disease. However, breastfeeding is recommended for the many benefits it provides to mother and infant.
- Breastfeeding during the period that solid foods are first introduced to infants from around 6 months may help reduce the risk of the infant developing allergies, although evidence for this is low.
- If breastfeeding is not possible, a standard cow’s milk based formula can be given. There is no evidence that soy or goat’s milk formula reduce the risk of allergic disease when used in preference to standard cow’s milk based formula.
- Based on a recently published review of studies, there is no consistent convincing evidence to support a protective role for partially hydrolysed formulas (usually labelled ‘HA’ or Hypoallergenic) or extensively hydrolysed formulas for the prevention of eczema, food allergy, asthma or allergic rhinitis in infants or children.
- Regular cow’s, goat’s milk (or other mammal derived milks), soy milk, nut and cereal beverages are not recommended for infants as the main source of milk before 12 months of age.
Ref: ASCIA 2019 guidelines (this information is still current and will be updated on an annual bases ‘if guidelines change’, 2020)
Ref: WHO reference
- Solid foods can be introduced to your baby around 6 months (not before 4 months) and when your baby is ready. If possible, breastfeed your baby while you are giving them solid foods. This advice is for all babies, even if they have severe eczema and/or food allergy, or if a parent or sibling has allergies.
- Studies show that introducing common allergy causing foods by 12 months may reduce the chance of babies developing food allergy. These foods include egg, peanut, cow’s milk (dairy), tree nuts, soy, sesame, wheat, fish and other seafood.
- Solid foods should be in a form suited for your baby’s age, such as small amounts of well cooked egg and smooth peanut butter/paste.
 Giving new solid foods in the day rather than at night allows you to watch your baby and respond if they have an allergic reaction.
Giving new solid foods in the day rather than at night allows you to watch your baby and respond if they have an allergic reaction.
- You can rub a small amount of food inside your baby’s lip to start with. If there is no allergic reaction after a few minutes, start giving small amounts of the food. Never smear or rub food on your baby’s skin, as this will not help to identify possible food allergies.
- If you need guidance, mix a small amount (¼ teaspoon) of hard-boiled egg or smooth peanut butter/paste into your baby’s usual food (such as vegetable puree). If there is no allergic reaction, gradually increase the amount, such as ½ teaspoon the next time.
- Continue to give the foods to your baby regularly (twice weekly) as part of a varied diet, to maintain tolerance. Trying a food and then not giving it regularly may result in food allergy development.
- Even if you follow this advice some babies may still develop a food allergy.
 If your baby has an allergic reaction (which mostly occur within minutes) stop giving that food and seek advice from your doctor.
If your baby has an allergic reaction (which mostly occur within minutes) stop giving that food and seek advice from your doctor.
- If your baby already has food allergies, see your doctor for advice, testing, treatment and an action plan. Babies with cow’s milk, wheat or multiple food allergies should also be seen by a dietitian to help maintain healthy food intake. Avoiding these foods can affect your baby’s growth and development.
ASCIA Fast Facts Introducing foods allergy prevention 2019313.65 KB
For more information visit www.allergy.org.au/patients/allergy-prevention ; www.preventallergies.org.au
Allergy & Anaphylaxis Australia www.allergyfacts.org.au and Allergy New Zealand www.allergy.org.nz are patient support organisations that offer updates and advice for people with allergies.
Nut Butters
According to the recent guidelines from the American Academy of Allergy, Asthma and Immunology, potentially allergenic foods like nuts are safe to introduce to babies as young as 6 months of age, once they have had exposure to a few typical first foods like cereals, fruit and vegetables. This is great news because nuts and nut butters like peanut, cashew, and almond are nutrition powerhouses, providing protein, beneficial fatty acids, vitamin E and minerals like manganese, potassium and iron. Lumps of nut butters are a choking hazard for small babies so try mixing it in foods or spread a thin layer over a long strip of toast to serve as a finger food.
This is great news because nuts and nut butters like peanut, cashew, and almond are nutrition powerhouses, providing protein, beneficial fatty acids, vitamin E and minerals like manganese, potassium and iron. Lumps of nut butters are a choking hazard for small babies so try mixing it in foods or spread a thin layer over a long strip of toast to serve as a finger food.
Eggs
Eggs are a great first food! They are easily digestible, and they offer the important nutrition your baby needs including iron, folate and choline, high-quality protein, plus vitamins A, D and E. Eggs are also a quick and easy meal to prepare. Just hard-cook an egg, make eggy bread, your could also mash the yolk and thin it with breast milk make it a dressing over foods etc. Hard-boiled and chopped egg white is a perfect finger food, as are scrambled eggs or omelets cut into thin strips.
Wheat Products i.e. Bread and Crackers
There are some parents that may think to limit gluten in their baby’s diet in the hope to reduce risk of developing celiac disease later in life. But although more research is needed on how to prevent celiac disease, there is now some evidence that keeping wheat away from babies is not helpful and may even increase their risk for this autoimmune disorder.
But although more research is needed on how to prevent celiac disease, there is now some evidence that keeping wheat away from babies is not helpful and may even increase their risk for this autoimmune disorder.
Cold-water Fish
Introducing fish to your baby is simple, you can bake it, pan fry it or steam a boneless fillet. Cold-water fish including salmon, herring, canned salmon, canned tuna light or sardines are a great source of DHA in a babies diet. DHA plays a crucial role in retinal and brain development and is especially important for children in the first two years of life. (note: ensure all bones are removed from fish as they may be a choking hazard).
The Environemental Defense Fund (one of the world’s largest environmental organizations, with more than 1.5 million members and a staff of 500 scientists, economists, policy experts, and other professionals around the world) looks at safety of canned tuna and fish. There are two main kinds of canned tuna: chunk light and solid or chunk white (albacore). Most canned white tuna is albacore. Its mercury levels are almost three times higher than the smaller skipjack, used in most canned light tuna.
Most canned white tuna is albacore. Its mercury levels are almost three times higher than the smaller skipjack, used in most canned light tuna.
The following are recommendations based on EPA guidance and estimates of mercury in the most popular canned tunas:
- Canned white, or albacore (0.32 parts per million of mercury). Children under six can eat up to one 3-ounce portion a month; children from 6–12, two 4.5-ounce portions a month. Adults, including pregnant women, can safely eat it up to three times a month (women, 6-ounce portions; men, 8-ounce portions).
- Canned light— the safer choice (0.12 parts per million of mercury). Children under six can eat up to three 3-ounce portions per month. Older children and adults can safely eat it once a week. But look out for “gourmet” or “tonno” labels. They are made with bigger yellowfin tuna and can contain mercury levels comparable to canned white.
- A better alternative is canned salmon(mostly sockeye or pink from Alaska), which is low in contaminants and high in heart-healthy omega-3s.
 It’s also sustainably caught in Alaska and similarly priced, making it a great choice all around.
It’s also sustainably caught in Alaska and similarly priced, making it a great choice all around.
Governing authorities & bodies around the world:
- World Health Organisation (WHO)
- American Academy of Pediatrics (AAP)
- The Murdoch Children’s Research Institute
- Australiasian Society of Clinical Immunology and Allergy (ASCIA)
- National Health Serve UK (NHS)
References & articles:
- 2019 ASCIA Infant Food Allergy Guidelines (Note: The Infant Feeding guidelines on the ASCIA website are the current versions (updated in 2019). The ASCIA resources are reviewed annually, however the documents will only be updated if there are changes in the literature).
- UK guidelines for baby led weaning
- What to feed your kids so they don’t get food allergies
- New Foods to Feed Babies
- AAP article Breastfeeding Benefits your babies immune system
- Mercury Levels in Canned Tuna
- ASCIA guidelines on this webpage are for parents and health professionals.

- Food service providers (such as childcare centres) should refer to the ASCIA guidelines for prevention of anaphylaxis in schools, preschools and childcare services: www.allergy.org.au/schools-childcare
Combat readiness - articles from the specialists of the clinic "Mother and Child"
What is an allergy?
Allergy - increased sensitivity of the body to certain substances. So, for example, some people can stroke a cat without consequences, while others sneeze or suffocate from contact with wool - this is how the body reacts to the allergen. An allergic reaction can be expressed in different ways: in the form of itchy redness on the skin, shortness of breath, sneezing, runny nose, digestive problems. The list of allergens is extensive: plant pollen (trees and grasses), animal hair, food, dust, bacteria, viruses and fungi, various chemicals.
Types of allergies in children
The most common in children:
• Food allergy - manifests itself in the form of skin itching, dermatitis, indigestion.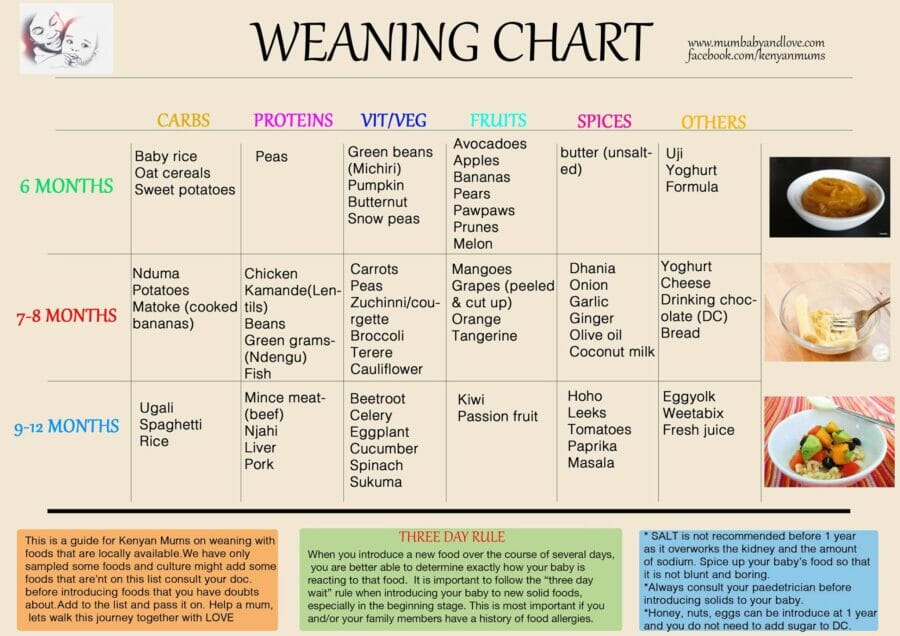
• Drug allergy - reaction to medication is expressed in skin irritation, itching, rashes, urticaria. There may be attacks of bronchial asthma, and in severe cases - anaphylactic shock.
• Pollinosis - occurs annually, during the flowering of plants. Hay fever is characterized by inflammation and itching in the eyes, shortness of breath, runny nose (allergic rhinitis).
• Cold allergy is a reaction to cold, which is manifested by a reaction of the skin (redness, itching), sometimes difficulty in breathing.
• Allergy to the sun - develops with prolonged exposure to ultraviolet rays on the skin.
• Quincke's edema - an acute allergic reaction that may occur in response to exposure to food allergens, after taking medication, after an insect bite.
Marina Vladimirovna explains: “The number of allergic reactions in children is increasing today. Most likely, this is due to the deterioration of the environmental situation and the quality of food. Animals receive hormonal supplements and antibiotics with feed, and pastures and crops are treated with chemicals, growth stimulants, and fertilizers. In addition, more household chemicals and medicines are now being used.”
Animals receive hormonal supplements and antibiotics with feed, and pastures and crops are treated with chemicals, growth stimulants, and fertilizers. In addition, more household chemicals and medicines are now being used.”
How to prevent
If polyunsaturated fats (Omega-3) are regularly present in the diet of the expectant mother, that is, foods such as fish, nuts, spinach, flaxseed oil, they have a positive effect on the immune system of the unborn child, reducing the risk of allergies. But if you already have allergies, you should follow a hypoallergenic diet! Smoking, including passive smoking, is very harmful: the risk of developing bronchial asthma and atopic dermatitis increases in the future baby. Breastfeeding is an excellent allergy prevention: studies show that cow's milk allergy is seven times more common in formula-fed babies, and breast milk significantly reduces the risk of allergies in the first years of life. As long as the baby eats only breast milk, his contact with food allergens is minimal. Both the immune and digestive systems of a child in the first six months of life are still immature: it is protected by mother's antibodies obtained in the womb and then from breast milk. Introducing complementary foods too early can cause allergies.
Both the immune and digestive systems of a child in the first six months of life are still immature: it is protected by mother's antibodies obtained in the womb and then from breast milk. Introducing complementary foods too early can cause allergies.
We treat wisely
Allergy treatment is complex and it is possible only after the discovery of the allergen! To begin with, the doctor will ask the mother to analyze the baby’s nutrition (and her own if the baby is breastfed): keeping a food diary will help identify the foods that caused the reaction. In addition to nutrition, other factors should be assessed: how do you wash bed linen and clothes? Is there too much dust in the apartment (or, for example, carpets, soft toys, open bookshelves)? Is there mold in the bathroom? How long have the air conditioners been cleaned? Does the child have reactions to pets or their food? A reaction to chlorine in tap water is also possible. In this case, installing a filter will help.
If a child is allergic to house dust or dust mites, you will have to give up carpets (especially those made of natural wool), and store soft toys in resealable containers and buy only those that are easy to wash. Blankets and pillows for children with allergies are suitable with artificial filling, which is easy to wash. In addition, air purifiers and humidifiers help - the humidity in the room should be at least 60%.
If the allergen cannot be experimentally identified, then the doctor will suggest that children over five years of age do skin tests for the most common irritants.
Doctors recommend moisturizing and anti-itch products that restore the protective functions of the skin, as well as hormonal ointments to eliminate skin rashes. They are safe for children, are not absorbed into the blood and allow you to quickly get rid of dermatitis. Most likely, the doctor will prescribe sorbent preparations - they remove harmful substances from the body, strengthening the immune system and restoring the microflora. Calcium preparations are also used for treatment - it reduces the permeability of the walls of blood vessels, prevents the penetration of allergens into the blood and enhances the effect of antihistamines.
Calcium preparations are also used for treatment - it reduces the permeability of the walls of blood vessels, prevents the penetration of allergens into the blood and enhances the effect of antihistamines.
Currently, the SIT-therapy method is widely used - "vaccinations" against allergies. This is a treatment method in which the body is "accustomed" to the allergen. Small doses of a substance are injected under the skin, which, upon contact, causes a certain reaction. At first, these are very small doses, then they gradually increase. SIT therapy allows you to minimize the manifestations of allergies - but only when the allergen is known and confirmed by research.
“This method is called immunotherapy, as it aims to develop resistance of the body's immune system to the effects of an allergen. This vaccination is given to people aged 5 to 50 years. The method is used primarily for respiratory allergies - for example, allergies to pollen, mold fungi, house dust mites and other household allergens, which manifests itself in the form of hay fever, conjunctivitis, atopic bronchial asthma. "Vaccination" is very effective as a prevention of serious allergic reactions to insect bites. It is carried out in the so-called “cold” period - when there is no exacerbation, ”explains Marina Vladimirovna.
"Vaccination" is very effective as a prevention of serious allergic reactions to insect bites. It is carried out in the so-called “cold” period - when there is no exacerbation, ”explains Marina Vladimirovna.
Prevention on holiday
Of course, it is impossible to avoid exposure to all allergens while traveling, but it is possible to reduce their harmful effects. Keep windows closed during pollination, do not open car windows. Give up trips to picnics and hiking - it is better to relax by the sea, where there is much less pollen. Be sure to follow the rules of being in the sun: avoid direct sunlight and be on the beach only before 11.00 and after 17.00. Remember that clouds are not an obstacle to mid-wave UV radiation. After bathing in salt water, be sure to rinse your baby in the shower and dry the skin: water drops and salt crystals are small lenses that enhance the effect of the sun. Apply sunscreen with an SPF (at least 45-50) after every swim or every two hours. And be careful with local exotic fruits, seafood and delicacies - the body's reaction to them can be unpredictable.
And be careful with local exotic fruits, seafood and delicacies - the body's reaction to them can be unpredictable.
If mom and dad have allergies, the child will develop it with a probability of 80%. If one of the parents, the risk is halved.
Food allergy: a familiar stranger | Paracelsus
What does the term "food allergy" mean? How can it manifest itself? Are there any age-related features (patterns)?
S.N. : - You are right: it is important to navigate in terminology. Reactions to food products can be divided into 2 large groups:
- toxic (for example, poisoning with mushrooms, nitrate vegetables, etc.)
- non-toxic:
1. Food allergy (FA) - reactions of varying strength to food protein, with the participation of immune mechanisms. An example is reactions with rashes, swelling, difficulty breathing to fish or peanuts, food anaphylaxis.
2. Food intolerance - for example, in case of insufficiency of digestive enzymes, diseases of the intestines, liver, pancreas. The most characteristic symptoms are those of the digestive system. An example is a disorder of the stool with lactase deficiency; celiac disease
3. Histamine liberation - reactions in the form of a release of histamine in response to a provocation with a non-protein food substance, without immune memory and depending on the dose of food eaten. An example is itchy rashes after a New Year's "tangerine punch" or drinking red wine.
The good news is that the actual prevalence of PA in the population is 10 times less than "allergy sufferers" believe: 2-3% according to scientists' estimates versus 20-30% according to population surveys. Thus, the true PA is 7-10% in the structure of allergic diseases and PA is the cause of Atopic dermatitis in children in 20-40% (in 10-15% in adults). As you can see, the role of PA decreases with age. Therefore, not many strict lifelong dietary restrictions are justified even for allergy sufferers!
Therefore, not many strict lifelong dietary restrictions are justified even for allergy sufferers!
How is food allergy inherited and developed in children?
S.N. : - The predisposition to allergic reactions is genetically transmitted from both the maternal and paternal side, and may sooner or later be realized: the risk reaches 80%. But science has not yet learned to predict which allergens a reaction will develop (food or inhaled or contact).
- Does it happen that the parents have never had allergies, and the child is allergic?
S.N. : - With detailed data collection, allergy or asthma reveals itself in previous generations of the family, lateral branches of the family tree (aunt, uncle), and sometimes it could not be recognized. So even when the parents themselves are not prone to allergies, there is a risk for the child (15%).
- What should parents of children with food allergies or a predisposition to it be wary of?
S. N. : - Factors provoking food allergies - pathology in the third trimester of pregnancy, complications in childbirth and delay in the first application to the breast (not in the first 30-40 minutes), passive smoking *, air pollution with pollutants, high-protein diet of the mother, viral infections at an early age , diseases and pathologies of the gastrointestinal tract, early transfer to artificial / mixed feeding.
N. : - Factors provoking food allergies - pathology in the third trimester of pregnancy, complications in childbirth and delay in the first application to the breast (not in the first 30-40 minutes), passive smoking *, air pollution with pollutants, high-protein diet of the mother, viral infections at an early age , diseases and pathologies of the gastrointestinal tract, early transfer to artificial / mixed feeding.
What foods are the most common allergens? Which ones are not allergic?
S.N. : - Most often, allergies are caused by dairy products, eggs, fish and seafood, soy, wheat, nuts, peanuts. This "big eight" is responsible for more than 90% of food allergies in any region of the globe. More than 160 food allergens have been described: anyone can be in this role in this or that person - and even a harmless zucchini, alas ...
Citrus fruits, chocolate, "sweet and red", food additives - even without being allergens, contribute to the release of histamine from our own cells, with this scenario, the dose eaten and the age of the eater are important.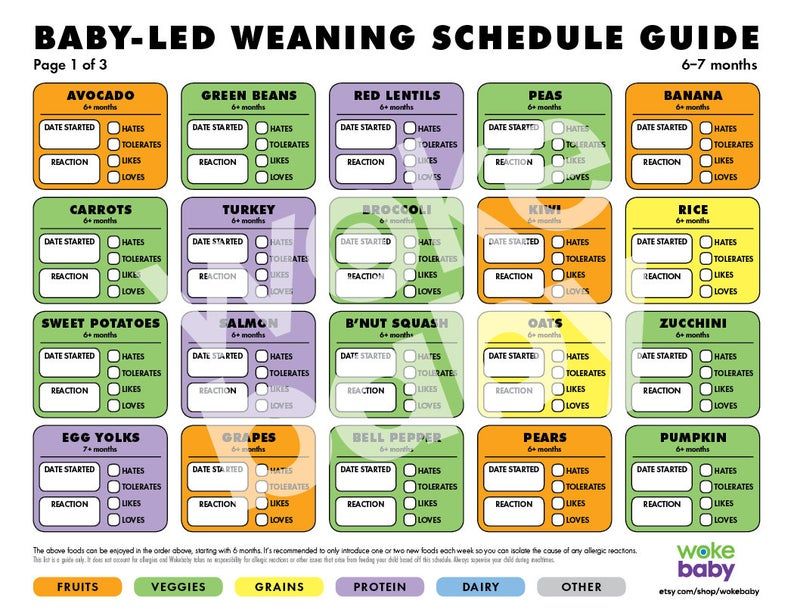
Can food allergies be prevented?
S.N.: - To date, effective methods of preventing PA include only balancing the nutrition of a pregnant woman and a nursing mother (varied! The role of dietary fiber!) And maintaining breastfeeding for at least 6 months, competent introduction of complementary foods, exclusion from the child's diet "food chemistry" at least up to 5-7 years.
- Very often there are disputes on the forums about the possibility or impossibility of developing an allergy to breast milk?
S.N. : - Breast milk is not an allergen, and this is one of the few indisputable statements in children's allergology J. Moreover, it contains many substances and factors that prevent the formation of PA and contribute to the maturation of the intestine, the formation of normal microflora in an infant. Mother's milk is still irreplaceable. Therefore, with an early start of PA, a special diet is recommended for a nursing mother, but not weaning the baby from the breast!
- Can food allergies occur in adults or is it the prerogative of childhood?
S. N. : - Cross food allergy with pollen allergy - yes. In this case, it usually appears in the mouth, sore throat, rashes around the mouth when eating fresh fruits, raw carrots, nuts and seeds (even if a person calmly consumed these products before the onset of hay fever).
N. : - Cross food allergy with pollen allergy - yes. In this case, it usually appears in the mouth, sore throat, rashes around the mouth when eating fresh fruits, raw carrots, nuts and seeds (even if a person calmly consumed these products before the onset of hay fever).
How can food allergens be identified?
S.N. : - Our Center has in its arsenal a large number of different allergy examination methods that allow at any age and with any symptomatology to identify the presence of sensitivity to a huge number of foods. In particular, the study using the Immunocap method allows you to determine even the initial level of allergy and - in time to exclude the food product from the diet, and then track the timing of the introduction of the guilty food product.
Immunocap is currently the gold standard for allergy diagnostics in the world, a reference laboratory method. The technique is fully automated, which eliminates the human factor. Immunocap data, combined with an analysis of the clinical picture, gives 99. 8% confidence in the correct diagnosis (remember the joke that medicine is an inexact science? we don’t have 100%)
8% confidence in the correct diagnosis (remember the joke that medicine is an inexact science? we don’t have 100%)
Our center also presents innovative molecular diagnostics that allows you to identify allergies to individual components of food products and find out prognostic risks, in particular, whether it is possible to use the guilty allergen in a thermally processed form, whether PA is true or cross, what is the prognosis for recovery.
How is PA treated?
S.N. : - diet + symptom control. In some cases, a diet without a “guilty” product is required for life, and this must be taken with all responsibility (for example, fish, nuts, peanuts).
Why is PA dangerous if it is not treated and who should treat it?
S.N. : - The risks associated with PA are, firstly, the development of an "atopic march": first, dermatitis, after a few years, rhinitis, conjunctivitis, bronchial asthma, and sometimes all these conditions do not replace each other sequentially, but are present in the same person for years and decades, seriously complicating the life of him, his entire family and his doctor.