Formula feeding a breastfed baby
How to combine breast and bottle feeding
It can take several weeks for you and your baby to feel happy and confident with breastfeeding.
Once you've both got the hang of it, it's usually possible to offer your baby bottles of expressed milk or formula alongside breastfeeding.
This is sometimes called mixed or combination feeding.
Why combine breast and bottle?
You may want to combine breastfeeding with bottle feeding if you:
- are breastfeeding and want to use a bottle to offer your baby some expressed breast milk
- want to breastfeed for some of your baby's feeds, but give bottles of formula for 1 or more feeds
- are bottle feeding your baby and want to start breastfeeding
- need to leave your baby and want to make sure they have some milk while you're away
Introducing formula feeds can affect the amount of breast milk you produce. There is also a small amount of evidence to show babies may not breastfeed as well because they learn to use a different kind of sucking action at the bottle than at the breast.
These things can make breastfeeding more difficult, especially in the first few weeks when you and your baby are still getting comfortable with breastfeeding.
Your breastmilk supply will usually not be affected if you start bottle feeding your baby when they are a bit older, you are both comfortable with breastbeeding, and you breastfeed every day.
Introducing formula feeds
If you're combining breastfeeding with formula feeds both you and your baby can carry on enjoying the benefits of breastfeeding.
If you choose to introduce infant formula:
- it's best to do it gradually to give your body time to reduce the amount of milk it makes – this helps lower your chance of getting uncomfortable, swollen breasts, or mastitis
- if you're going back to work, start a few weeks beforehand to give both of you time to readjust
- if your baby is 6 months old or more and can drink milk from a cup, you may not need to introduce a bottle at all
For more information, see drinks and cups for babies.
Giving your baby their first bottle
It may take a while for a breastfed baby to get the hang of bottle feeding, because they need to use a different sucking action.
- it usually helps to give the first few bottles when your baby is happy and relaxed – not when they're very hungry
- it may help if someone else gives the first bottle feeds, so that your baby is not near you and smelling your breast milk
- you might want to try using a different position for bottle and breastfeeding
See more advice on how to bottle feed.
Restarting breastfeeding
If you want to start breastfeeding more and give your baby fewer bottles, it's a good idea to ask your midwife, health visitor or breastfeeding supporter for support.
These tips may help too:
- Hold and cuddle your baby as much as possible, ideally skin to skin. This will encourage your body to make milk and your baby to feed.

- Express your breast milk regularly. Expressing releases the hormone prolactin, which stimulates your breasts to make milk. About 8 times a day, including once at night is ideal. It may be easier to express by hand to begin with – your midwife, health visitor or breastfeeding supporter can show you how.
- Try bottlefeeding while holding your baby skin to skin and close to your breasts.
- If your baby is latching on, feed little and often. Do not worry if your baby does not feed for long to begin with. See tips on how to get your baby properly positioned and attached.
- Choose times when your baby is relaxed, alert and not too hungry, and do not force your baby to stay at the breast.
- Decrease the number of bottles gradually, as your milk supply increases.
- Consider using a lactation aid (supplementer). A tiny tube is taped next to your nipple and passes into your baby's mouth so your baby can get milk via the tube as well as from your breast.
 This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
See more tips on boosting your milk supply.
Help and support with mixed feeding
If you have any questions or concerns about combining breast and bottle feeding:
- talk to your midwife, health visitor or breastfeeding supporter
- call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm, every day)
- find breastfeeding support near you
Video: why combine breast and bottle feeding?
In this video, 3 mothers discuss ways to combine breast and bottle feeding.
Media last reviewed: 22 March 2020
Media review due: 22 March 2023
Page last reviewed: 8 October 2019
Next review due: 8 October 2022
Breastfeeding vs.
 Formula Feeding (for Parents)
Formula Feeding (for Parents)Choosing whether to breastfeed or formula feed their baby is one of the biggest decisions expectant and new parents will make.
Healt experts believe breast milk is the best nutritional choice for infants. But breastfeeding may not be possible for all women. For many, the decision to breastfeed or formula feed is based on their comfort level, lifestyle, and specific medical situations.
For moms who can't breastfeed or who decide not to, infant formula is a healthy alternative. Formula provides babies with the nutrients they need to grow and thrive.
Some mothers worry that if they don't breastfeed, they won't bond with their baby. But the truth is, loving mothers will always create a special bond with their children. And feeding — no matter how — is a great time to strengthen that bond.
The decision to breastfeed or formula feed your baby is a personal one. Weighing the pros and cons of each method can help you decide what is best for you and your baby.
All About Breastfeeding
Nursing can be a wonderful experience for both mother and baby. It provides ideal nourishment and a special bonding experience that many mothers cherish.
A number of health organizations — including the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the World Health Organization (WHO) — recommend breastfeeding as the best choice for babies. Breastfeeding helps defend against infections, prevent allergies, and protect against a number of chronic conditions.
The AAP recommends that babies be breastfed exclusively for the first 6 months. Beyond that, breastfeeding is encouraged until at least 12 months, and longer if both the mother and baby are willing.
Here are some of the many benefits of breastfeeding:
Fighting infections and other conditions. Breastfed babies have fewer infections and hospitalizations than formula-fed infants. During breastfeeding, antibodies and other germ-fighting factors pass from a mother to her baby and strengthen the immune system. This helps lower a baby's chances of getting many infections, including:
This helps lower a baby's chances of getting many infections, including:
- ear infections
- diarrhea
- respiratory infections
- meningitis
Breastfeeding also may protect babies against:
- allergies
- asthma
- diabetes
- obesity
- sudden infant death syndrome (SIDS)
Breastfeeding is particularly beneficial for premature babies.
Nutrition and ease of digestion. Often called the "perfect food" for a human baby's digestive system, breast milk's components — lactose, protein (whey and casein), and fat — are easily digested by a newborn.
As a group, breastfed infants have less difficulty with digestion than do formula-fed infants. Breast milk tends to be more easily digested so that breastfed babies have fewer bouts of diarrhea or constipation.
Breast milk also naturally contains many of the vitamins and minerals that a newborn requires. One exception is vitamin D — the AAP recommends that all breastfed babies begin receiving vitamin D supplements during the first 2 months and continuing until a baby consumes enough vitamin D-fortified formula or milk (after 1 year of age).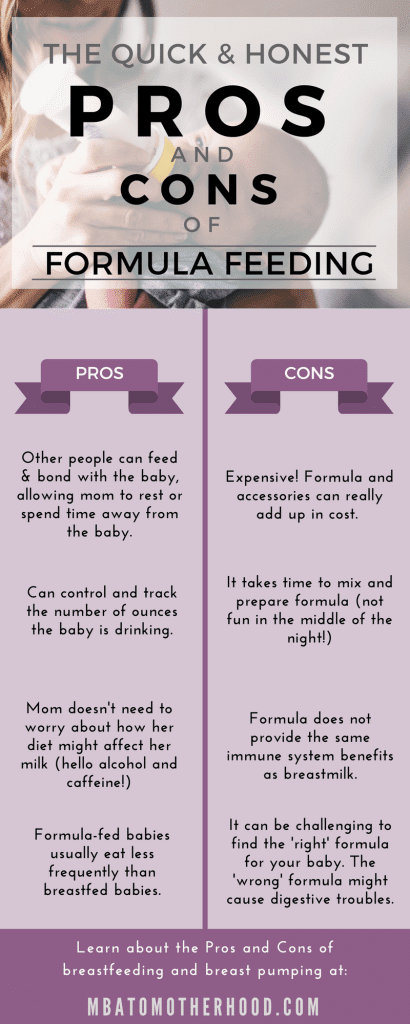
The U.S. Food and Drug Administration (FDA) regulates formula companies to ensure they provide all the necessary nutrients (including vitamin D) in their formulas. Still, commercial formulas can't completely match breast milk's exact composition. Why? Because milk is a living substance made by each mother for her individual infant, a process that can't be duplicated in a factory.
Free. Breast milk doesn't cost a cent, while the cost of formula quickly adds up. And unless you're pumping breast milk and giving it to your baby, there's no need for bottles, nipples, and other supplies that can be costly. Since breastfed babies are less likely to be sick, that may mean they make fewer trips to the doctor's office, so fewer co-pays and less money are paid for prescriptions and over-the-counter medicines.
Different tastes. Nursing mothers usually need 300 to 500 extra calories per day, which should come from a wide variety of well-balanced foods. This introduces breastfed babies to different tastes through their mothers' breast milk, which has different flavors depending on what their mothers have eaten. By tasting the foods of their "culture," breastfed infants more easily accept solid foods.
This introduces breastfed babies to different tastes through their mothers' breast milk, which has different flavors depending on what their mothers have eaten. By tasting the foods of their "culture," breastfed infants more easily accept solid foods.
Convenience. With no last-minute runs to the store for more formula, breast milk is always fresh and available whether you're home or out and about. And when women breastfeed, there's no need to wash bottles and nipples or warm up bottles in the middle of the night.
Smarter babies. Some studies suggest that children who were exclusively breastfed have slightly higher IQs than children who were formula fed.
"Skin-to-skin" contact. Many nursing mothers really enjoy the experience of bonding so closely with their babies. And the skin-to-skin contact can enhance the emotional connection between mother and infant.
Beneficial for mom, too. The ability to totally nourish a baby can help a new mother feel confident in her ability to care for her baby. Breastfeeding also burns calories and helps shrink the uterus, so nursing moms may be able to return to their pre-pregnancy shape and weight quicker. Also, studies show that breastfeeding helps lower the risk of breast cancer, high blood pressure, diabetes, and cardiovascular disease, and also may help decrease the risk of uterine and ovarian cancer.
Breastfeeding also burns calories and helps shrink the uterus, so nursing moms may be able to return to their pre-pregnancy shape and weight quicker. Also, studies show that breastfeeding helps lower the risk of breast cancer, high blood pressure, diabetes, and cardiovascular disease, and also may help decrease the risk of uterine and ovarian cancer.
p
Breastfeeding Challenges
Breastfeeding can be easy from the get-go for some mothers, but take a while to get used to for others. Moms and babies need plenty of patience to get used to the routine of breastfeeding.
Common concerns of new moms, especially during the first few weeks and months, may include:
Personal comfort. Initially, many moms feel uncomfortable with breastfeeding. But with proper education, support, and practice, most moms overcome this.
Latch-on pain is normal for the first week to 10 days, and should last less than a minute with each feeding. But if breastfeeding hurts throughout feedings, or if their nipples and/or breasts are sore, it's a good idea for breastfeeding mothers to get help from a lactation consultant or their doctor. Many times, it's just a matter of using the proper technique, but sometimes pain can mean that something else is going on, like an infection.
Many times, it's just a matter of using the proper technique, but sometimes pain can mean that something else is going on, like an infection.
Time and frequency of feedings. Breastfeeding requires a big time commitment from mothers, especially in the beginning, when babies feed often. A breastfeeding schedule or the need to pump breast milk during the day can make it harder for some moms to work, run errands, or travel.
And breastfed babies do need to eat more often than babies who take formula, because breast milk digests faster than formula. This means mom may find herself in demand every 2 or 3 hours (maybe more, maybe less) in the first few weeks.
Diet. Women who are breastfeeding need to be aware of what they eat and drink, since these can be passed to the baby through the breast milk. Just like during pregnancy, breastfeeding women should not eat fish that are high in mercury and should limit consumption of lower mercury fish.
If a mom drinks alcohol, a small amount can pass to the baby through breast milk.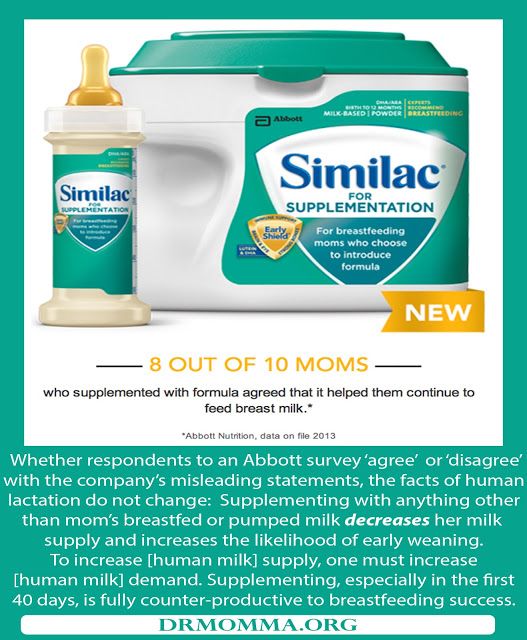 She should wait at least 2 hours after a single alcoholic drink to breastfeed to avoid passing any alcohol to the baby. Caffeine intake should be kept to no more than 300 milligrams (about one to three cups of regular coffee) or less per day because it can cause problems like restlessness and irritability in some babies.
She should wait at least 2 hours after a single alcoholic drink to breastfeed to avoid passing any alcohol to the baby. Caffeine intake should be kept to no more than 300 milligrams (about one to three cups of regular coffee) or less per day because it can cause problems like restlessness and irritability in some babies.
Maternal medical conditions, medicines, and breast surgery. Medical conditions such as HIV or AIDS or those that involve chemotherapy or treatment with certain medicines can make breastfeeding unsafe. A woman should check with her doctor or a lactation consultant if she's unsure if she should breastfeed with a specific condition. Women should always check with the doctor about the safety of taking medicines while breastfeeding, including over-the-counter and herbal medicines.
Mothers who've had breast surgery, such as a reduction, may have difficulty with their milk supply if their milk ducts have been severed. In this situation, a woman should to talk to her doctor about her concerns and work with a lactation specialist.
p
All About Formula Feeding
Commercially prepared infant formulas are a nutritious alternative to breast milk, and even contain some vitamins and nutrients that breastfed babies need to get from supplements.
Manufactured under sterile conditions, commercial formulas attempt to duplicate mother's milk using a complex combination of proteins, sugars, fats, and vitamins that aren't possible to create at home. So if you don't breastfeed your baby, it's important to use only commercially prepared formula and not try to make your own.
Besides medical concerns that may prevent breastfeeding, for some women, breastfeeding may be too difficult or stressful. Here are other reasons women may choose to formula feed:
Convenience. Either parent (or another caregiver) can feed the baby a bottle at any time (although this is also true for women who pump their breast milk). This allows mom to share the feeding duties and helps her partner to feel more involved in the crucial feeding process and the bonding that often comes with it.
Flexibility. Once the bottles are made, a formula-feeding mother can leave her baby with a partner or caregiver and know that her little one's feedings are taken care of. There's no need to pump or to schedule work or other obligations and activities around the baby's feeding schedule. And formula-feeding moms don't need to find a private place to nurse in public.
Time and frequency of feedings. Because formula is less digestible than breast milk, formula-fed babies usually need to eat less often than breastfed babies.
Diet. Women who opt to formula feed don't have to worry about the things they eat or drink that could affect their babies.
page 7
Formula Feeding Challenges
As with breastfeeding, there are some challenges to consider when deciding whether to formula feed.
Lack of antibodies. None of the antibodies found in breast milk are in manufactured formula. So formula can't provide a baby with the added protection against infection and illness that breast milk does.
Can't match the complexity of breast milk. Manufactured formulas have yet to duplicate the complexity of breast milk, which changes as the baby's needs change.
Planning and organization. Unlike breast milk — which is always available, unlimited, and served at the right temperature — formula feeding your baby requires planning and organization to make sure that you have what you need when you need it. Parents must buy formula and make sure it's always on hand to avoid late-night runs to the store.
And it's important to always have the necessary supplies (like bottles and nipples) clean, easily accessible, and ready to go — otherwise, you will have a very hungry, very fussy baby to answer to. With 8-10 feedings in a 24-hour period, parents can quickly get overwhelmed if they're not prepared and organized.
Expense. Formula can be costly. Powdered formula is the least expensive, followed by concentrated, with ready-to-feed being the most expensive. And specialty formulas (such as soy and hypoallergenic) cost more — sometimes far more — than the basic formulas. During the first year of life, the cost of basic formula can run about $1,500.
And specialty formulas (such as soy and hypoallergenic) cost more — sometimes far more — than the basic formulas. During the first year of life, the cost of basic formula can run about $1,500.
Possibility of producing gas and constipation. Formula-fed babies may have more gas and firmer bowel movements than breastfed babies.
Making a Choice
Deciding how you will feed your baby can be a hard decision. You'll really only know the right choice for your family when your baby comes.
Many women decide on one method before the birth and then change their minds after their baby is born. And many women decide to breastfeed and supplement with formula because they find that is the best choice for their family and their lifestyle.
While you're weighing the pros and cons, talk to your doctor or lactation consultant. These health care providers can give you more information about your options and help you make the best decision for your family.
Breast milk and formula: what do they have in common?
1 Cribb VL et al.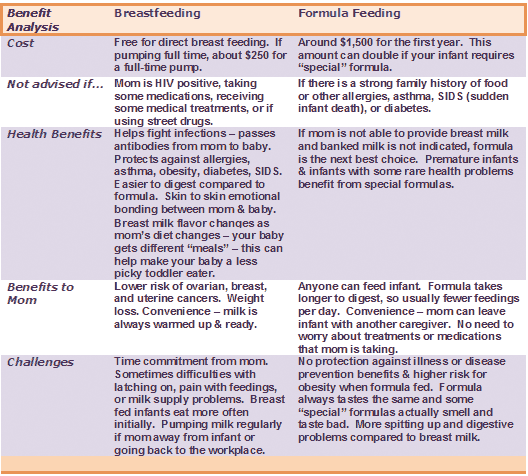 Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Clean Nutr. 2012;66(1):104.
Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Clean Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity. " Int J Pediatrician Endocrinol. 2009;2009:327505.
" Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv Nutr. 2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
- Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development. " J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
" J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR. Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
- Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child. 2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263.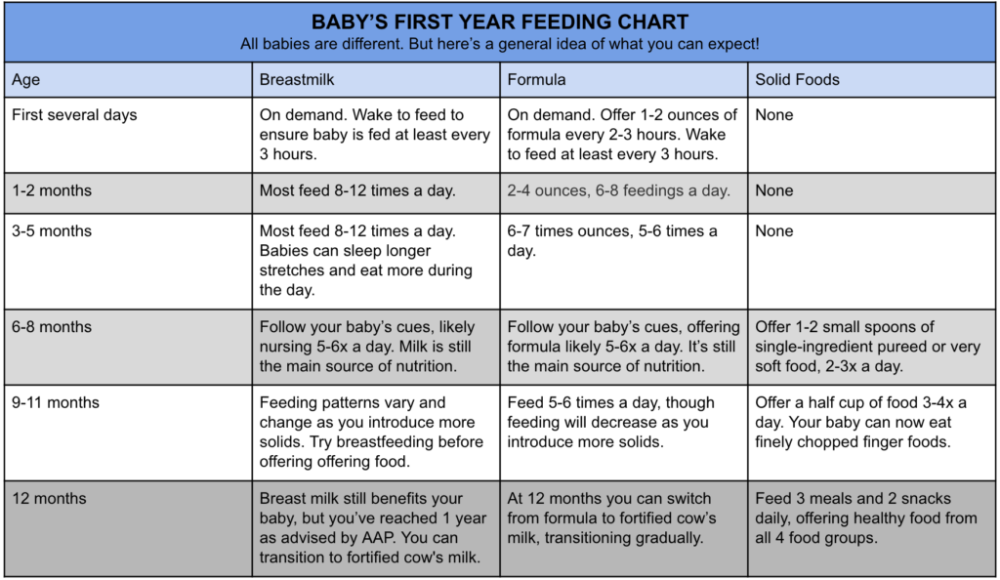 - Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: the MIDIA study ". Diabitis Care. 2015;38(2):257-263.
- Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: the MIDIA study ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review. JAMA Pediatr . 2015;169(6): e 151025. - Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrician. 2015;169(6):e151025.
25 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatric. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginecol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas G Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
31 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
32 Doan T et al. Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs . 2007;21(3):200-206. - Dawn T. et al., "Breastfeeding increases parental sleep duration." G Perinat Neonatal Nurs. 2007;21(3):200-206.
33 Menella JA et al. Prenatal and postnatal flavor learning by human infants. Pediatrics . 2001;107(6): E 88. - Menella J.A. et al., Prenatal and Postnatal Taste and Smell Recognition in Children. Pediatrix (Pediatrics). 2001;107(6):e88.
34 Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance.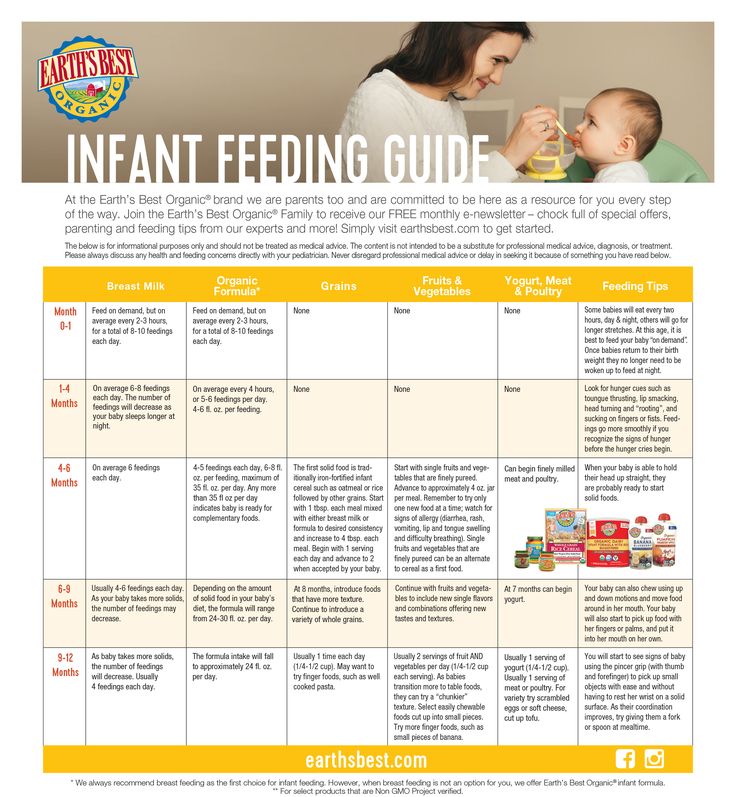 Pediatrics . 2007;120(6):1247-1254. - Forestell S.A., Mennella J.A., "The First Signs of Readiness to Taste Fruits and Vegetables." Pediatrix (Pediatrics). 2007;120(6):1247-1254.
Pediatrics . 2007;120(6):1247-1254. - Forestell S.A., Mennella J.A., "The First Signs of Readiness to Taste Fruits and Vegetables." Pediatrix (Pediatrics). 2007;120(6):1247-1254.
is it possible to stop breastfeeding
These are comments from Community readers. Collected into one material, carefully edited and formatted according to editorial standards.
Julia Konyakhina
studied the opinion of readers
Author profile
According to WHO, only 40% of children under six months of age are exclusively breastfed. The rest are on artificial or mixed feeding.
We asked readers to tell us which way of feeding they have chosen for their children and why. A discussion unfolded in the comments: there were arguments both in defense of artificial mixtures and in favor of breastfeeding. We carefully studied the opinions of readers and chose arguments for switching to mixtures and against.
👍 For: mixtures help out when mom is not around
Evgeny Kulakov
experienced father
In October 2020, when the youngest child was six months old, the wife contracted the coronavirus and was admitted to the hospital for 10 days. And the mixture saved me, if not my life, then my nervous system for sure. Although the baby was already given complementary foods, he was not yet weaned from the breast. I had to urgently order a mixture, or rather a lot of a mixture. So he got off his chest.
And the mixture saved me, if not my life, then my nervous system for sure. Although the baby was already given complementary foods, he was not yet weaned from the breast. I had to urgently order a mixture, or rather a lot of a mixture. So he got off his chest.
The eldest himself refused breast milk at six months. The doctor recommended that we switch to a mixture to avoid a lack of vitamins.
/papa-mozhet/
How can a man go on maternity leave
As for the pros and cons of formulas for children, no difference was noticed with breast milk. And the family benefited from not breastfeeding. Despite the restrictions during the pandemic, we became more mobile with the younger one: we were able to travel long distances and walk longer in nature.
👎 Against: breast milk is healthier for the baby
Zhenya
fed two
She breastfed two daughters, although both times were not easy. The older one could not be properly attached to the chest. It was very painful, the milk stagnated in the ducts, the child did not gain weight well. She called breastfeeding specialists to the house: they helped, showed me how to feed properly. She fed her daughter for up to a year and seven months, then she quite easily refused to breastfeed.
It was very painful, the milk stagnated in the ducts, the child did not gain weight well. She called breastfeeding specialists to the house: they helped, showed me how to feed properly. She fed her daughter for up to a year and seven months, then she quite easily refused to breastfeed.
I don't regret choosing to breastfeed. My daughter was a little sick, now she also easily tolerates SARS. Initially, she was anxious, and breastfeeding helped her calm down and fall asleep.
There was a lot of milk from the youngest, and I again suffered from severe lactostasis. Again she called a specialist: they strained her chest, albeit through tears. But then everything was perfect, fed up to a year and a half. There was a moment when the child tried to refuse the breast, but we managed to overcome it.
It seems inconvenient to me to feed with mixtures: you need to fiddle with jars, sterilize them, and heat them up. You may be allergic to the mixture. Breastfeeding is much easier: I put on a special apron and fed anywhere. I believe that mixtures are an extreme measure that can be taken only out of hopelessness.
I believe that mixtures are an extreme measure that can be taken only out of hopelessness.
Verunchik Gavrikova
passed the GV course
Initially, she was determined to breastfeed her baby. I read a lot, watched videos on YouTube about the best position to feed, how to properly attach the baby to the breast, what to do in case of lactostasis, mastitis, how to decant in an emergency with your hands. My friends gave me breast pumps, I bought absorbent breast pads.
I chose the GV-friendly maternity hospital, where after giving birth a consultant came to me and showed me how to apply the baby. I also took a special training course: it was not only about feeding, but also about the features of caring for children.
I can’t say that I am a fan of breastfeeding, but I think that this is the best option for a child. Nature has provided that the composition of milk varies depending on the age and needs of the baby. Through milk, he receives antibodies. That is, if a mother gets sick with SARS, the child will be protected. After all, it's free, it's the bond between mother and child. At night, mom can sleep while the baby eats while sleeping together. As a result, everyone gets enough sleep.
That is, if a mother gets sick with SARS, the child will be protected. After all, it's free, it's the bond between mother and child. At night, mom can sleep while the baby eats while sleeping together. As a result, everyone gets enough sleep.
/spi-moya-radost/
How to solve baby sleep problems
Evgewa
breastfed for 2 years
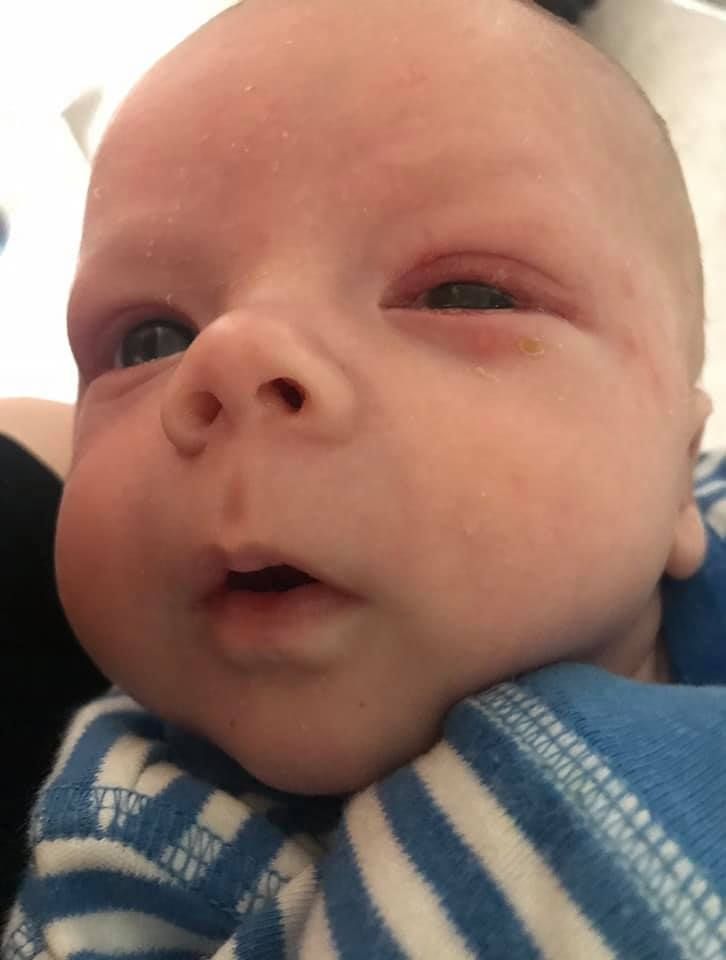
There was not even a choice how to feed. She knew that there would be only breastfeeding, despite the fact that the child was born prematurely and spent a total of a month on nursing, of which one week was in intensive care.
The neonatologist said that at least a drop, but you need to give breast milk to the child. For several weeks, until it was impossible to go to the ward with him, I pumped every three hours and carried the milk. She did not feed only during the resuscitation period, where the child got two weeks after birth.
After discharge, already at home, feeding was established, which lasted up to two years without a single problem. I remember this time as the happiest.
I remember this time as the happiest.
👍 For: when there is not enough milk, with a mixture the child is more satisfying, and the mother is calmer
Lera Kotova
for the child to be full
In my family, all the women had little milk. Therefore, I prepared for the fact that I would have the same. She breastfed the eldest for up to five months, squeezing some miserable drops out of herself, and at the same time supplemented her with formula. I fed the younger one for a month and a half, but then I got tired of lying for hours with a breast in my mouth and no visible effect, so I switched him to a mixture in a week, and everyone felt good and satisfying.
Elena Goncharova
switched to the mixture and does not regret
I fed my son formula. It didn't work out for me with breastfeeding. I don’t know how it really is, but it felt like there wasn’t enough milk in the first week. I drank and lactation pills, and tea with milk, and ate often, but my chest quickly became empty, my son hung on it for an hour and a half and, as it seemed to me, did not eat enough.
I expressed some crumbs, got nervous, cried that I couldn't feed my son. It still hurt. Although it seemed like she tried to apply, as they taught in the maternity hospital. In the end, looking at my suffering, my sister said a very correct phrase: “Your task is to feed the child. And what is a secondary question. So we switched to a mixture. I don't regret.
We fed our son together with her husband: sometimes he, sometimes me. Walked longer, slept better. Until almost two years old, the child did not get sick with anything, constipation, and did not suffer from allergies. The only negative was only the price of the mixture. It turned out that a good one is not cheap.
/baby-cost-calc/
Calculator: How much will you spend per child in the first year
Perhaps with the second child I will immediately begin to feed the mixture, or maybe I will try breastfeeding again. But this will be my personal decision, I will not listen to anyone else on this issue.
👎 Against: contact with a child is priceless
Olga Rulich
had no problems with breastfeeding
It turned out to be difficult for me to wean the children from the breast. With the first child, this happened at two years and two months, with the second - at one year and eight months.
The process of establishing feeding and feeding itself was problem-free. I did not take medicines, there were no force majeure. Contact with the baby during feeding is invaluable.
👍 Pros: formula feeding is more convenient
Polina Kalmykova
weighed all the pros and cons and chose the mixture
Both children spent the first weeks after birth in the hospital. In order not to lose breastfeeding, I had to work hard: first, around the clock every three hours, go to the intensive care unit and express into the syringe, then sit in the hospital in the breast pumping room with ten more of the same mothers and prepare food. All this was bleak: they don’t even give a child in their arms, after giving birth emotions rage, and here you are sitting - either you cry, or a neighbor.
All this was bleak: they don’t even give a child in their arms, after giving birth emotions rage, and here you are sitting - either you cry, or a neighbor.
After the hospital, my son did not want to breastfeed, she still suffered with breastplates: I remember, to be honest, all this with a shudder. As a result, I breastfed him for up to a year, and my daughter refused at four months: I was forced to switch to treatment that was incompatible with breastfeeding, and after a bottle, my daughter stopped breastfeeding. Probably, it was possible to find a consultant, try to fix something, but I had no particular desire.
A month before, a gastroenterologist from a polyclinic put me on the most rigid diet literally without anything, because my daughter had reflux. I decided it would be best for everyone to switch to a special blend. Later, however, it turned out that reflux absolutely fit into the physiological norm and there was no need to torment me like that.
Community 22. 06.21
06.21
How to eat healthy while breastfeeding?
Now my daughter is already a year old and I can compare breastfeeding and formula. Brief conclusion: the mixture is much more convenient. My daughter very quickly switched to a full night's sleep. Sometimes, of course, he wakes up at night, but this cannot be compared with how his son slept on GV: he woke up three to five times during the night. It is also easier to put to bed: the daughter easily falls asleep with a bottle, and the son's connection "HV - sleep" quickly ceased.
Weaning our son from GV was also stressful for us: I tried to turn it all over for more than a month. With my daughter, there are no problems with weaning from the bottle. My children and I often go to different public places, and, of course, bottle feeding there is much easier than breastfeeding: you don’t have to look for feeding rooms, wrap yourself in snoods, or prepare for public censure. I am no longer ready to pump into a bottle after weeks in the hospital.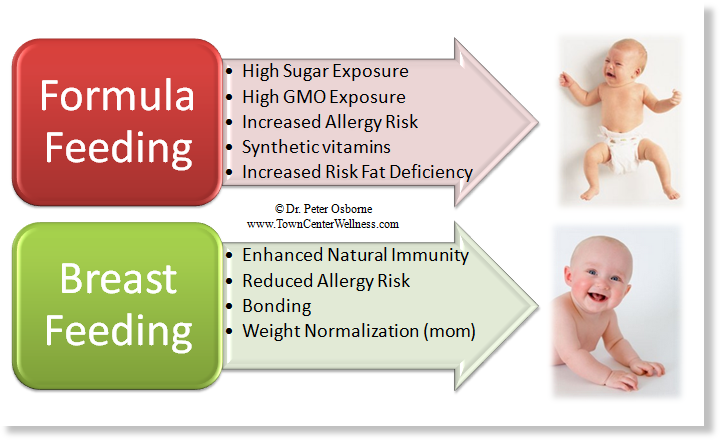 Well, in general, it’s more comfortable for me to live when there is no milk in my breast: nothing presses, nothing swells, nothing leaks.
Well, in general, it’s more comfortable for me to live when there is no milk in my breast: nothing presses, nothing swells, nothing leaks.
True, I also noticed the disadvantages. It seems that breastfeeding really has a better effect on the child's immunity: the son did not get sick at all in the first year, the daughter fell ill several times, once she even ended up in the hospital with bronchitis. Another point is cost. We used a can of 600 g of not the most expensive mixture in a few days, a month it turned out from 10,000 R and more. GV, of course, is much more economical.
👎 Against: breastfeeding is more physiological and cheaper0021
She breastfed both daughters. At first there were difficulties, but I struggled with them. Thanks to perseverance, she overcame all problems.
Feed each for over a year. I believe that this process is inherent in us by nature, and it is better not to interfere in the affairs of nature. I did not feel any inconvenience or deprivation due to breastfeeding.