Formula feeding at baby friendly hospital
My “Baby Friendly” Hospital Harmed My Baby: How Hospitals Can Do Better
The author and her daughter shortly after delivery
The decision to breast- or formula-feed is a highly personal one, with the right answer varying parent to parent. But this is not an article about the benefits of breastfeeding or about concerns that previous studies may have exaggerated those benefits. This isn’t an overview of the long coercive history of formula companies or the Trump administration’s politically motivated refusal to endorse a 2018 World Health Organization resolution promoting breastfeeding. Nor is it a discussion of the feminist case for formula-feeding made by Hanna Rosin and others.
Rather, this is a story about what happens when good information isn’t enough to overcome bad systems. But first, some background. I’m white, middle-class, and well-educated—with all of the status and privilege that affords. This is my third child, I work in health policy, and I already had a pretty good sense of the medical literature on breastfeeding when I walked into the maternity ward. Before joining the National Women’s Health Network, I spent a decade as a senior aide to two members of Congress so I’ve had a lot of experience telling powerful people why they’re wrong. In short, there aren’t many patients better positioned to stand up for themselves and their children.
And yet, I didn’t. Or at least not until my daughter was so dehydrated she couldn’t give enough blood to fill a pen cap.
Arrival of the "Baby Friendly" HospitalsWhen I gave birth for the first time, the “baby friendly hospital” movement was still in its infancy in the United States. It wasn’t until 2010 that the U.S. Department of Health and Human Services endorsed its ten principles, including:
#7 “practice rooming in” (the term for when a baby sleeps in the mother's hospital room during her recovery instead of in the hospital nursery),
#9 “give no pacifiers or artificial nipples to breastfeeding infants,” and
#6 “give infants no food or drink other than breast-milk, unless medically indicated. ”
”
(The WHO formally dropped their prohibition on pacifiers in a 2018 update, but as of this writing, the Americans haven’t caught up.)
However well-intentioned, these principles—imposed on exhausted parents by hospital staff and backed up by a tangle of bureaucratic rules and incentives—can quickly turn coercive in practice.
As the Washington Post reported in 2014, “If a mom wants to send her newborn [to the nursery], staff members often have to ask why and then fill out paperwork explaining the reason. ... Formula may be provided, but only on request, and only after, in some instances, mothers sign a waiver acknowledging that using a bottle could impede breast-feeding. Lactation consultants roam the floor.” [emphases mine]
“full compliance with the 10 steps of the initiative may inadvertently be promoting potentially hazardous practices”
Writing in JAMA Pediatrics in 2016, pediatricians Joel L. Bass, Tina Gartley, and Ronald Kleinman warned that “there is now emerging evidence that full compliance with the 10 steps of the initiative may inadvertently be promoting potentially hazardous practices and/or having counterproductive outcomes.”
Bass, Tina Gartley, and Ronald Kleinman warned that “there is now emerging evidence that full compliance with the 10 steps of the initiative may inadvertently be promoting potentially hazardous practices and/or having counterproductive outcomes.”
The article highlighted the dangers of mandatory rooming-in and unsupervised skin-to-skin contact when mothers are exhausted or medicated and called into question the practice of banning pacifiers when pacifiers have been shown to reduce the incidence of sudden infant death syndrome (SIDS). It also raised concerns about coercing mothers into exclusive breastfeeding.
Starving My BabyI first noticed things weren’t right 24 hours after giving birth. My daughter was too sleepy to nurse longer than a few weak tugs on my breast and none of the lactation consultant’s tricks would rouse her. With my other children, I’d satisfactorily supplemented nursing with formula during my hospital stay so I asked for a bottle.
Click to enlarge
The nurse was stern and disapproving. If I wanted to “give up” on breastfeeding, I’d have to sign a waiver acknowledging all of the risks associated with my terrible choice. “Reasons for supplementation” listed on the form include “mothers who are critically ill,” have “intolerable pain during feeding unrelieved by interventions,” or have “breast pathology.”
For mothers who simply choose to supplement, the form makes clear: “The American Academy of Pediatrics says that routine supplements of formula for breastfed newborns should not be used.”
Recovering from a C-section, I was dependent on hospital staff for my food and pain medication, and even assistance using the bathroom. Interrupted every hour for two straight days by a seemingly endless parade of doctors, residents, nurses, techs, and support staff—all with their own, uncoordinated schedule of rounds—I had the jellied zombie brain of a torture victim.
I signed their form, but then I didn’t use the formula! Maybe I’d better speak to the pediatrician first, I thought, see if I’m overreacting to my baby’s listlessness before I give her an allergy, destroy my milk supply, or risk any of the other horrors of formula supplementation described on the waiver. I asked to see the pediatrician but the nurses sent me the lactation consultant instead.
I asked to see the pediatrician but the nurses sent me the lactation consultant instead.
And so I delayed for another day, with a signed form and a pack of ready-made formula within reach but too cowed to go against the hospital staff who controlled every aspect of my existence. Looking back now, it’s incomprehensible to me. Dehydration in newborns can lead to blood clots, strokes, brain swelling, permanent brain damage, and death. I should have fed my baby right away, and I knew it, and yet somehow I didn’t do it.
"Cut, squeeze, repeat, while she screamed in pain and I watched helplessly."
Fortunately for the two of us, jaundice set in first, and with it the need to draw blood for a bilirubin test. The nurses cut my daughter’s heel, she screamed weakly, they squeezed her little foot to express the blood, and collected a single drop. Then the cut quickly clotted closed.
So they had to do it again. And again. And again.
And again.
Cut, squeeze, repeat, while she screamed in pain and I watched helplessly.
They only needed to collect a tiny vial’s worth, but she was far too dehydrated. She’d lost 15% of her birthweight by then. After twenty agonizing minutes, they handed my tiny girl back to me. I flung open the cabinet and attached nipple to bottle with shaking hands. With that first sip, her eyes shot wide open and her tiny hands flew instinctively to the sides of the bottle. She responded like a starving person eating for the first time in her life. Which, of course, she was.
It Doesn't Have to Be This WayIn the months since leaving the hospital, I’ve I thought a lot about how the hospital’s systems were structured, intentionally or not, to strip me of my own decision-making power. Good information is a necessary component of good health outcomes, but it’s not sufficient so long as patients aren’t empowered to follow through. As Laura Dorwart wrote in The Week about her own experience in a “baby-friendly” hospital, the issue is one of “parental consent within a medical context that too often presents itself as a top-down hierarchy: hospital administration, doctor, nurse, baby — and mother last. Dead last.”
Dead last.”
It doesn’t have to be this way. To ensure the well-being of both mother and child, hospitals should:
- coordinate routine nighttime schedules to better support patient recovery since sleep-deprived patients can’t advocate for themselves as effectively
- scrap policies that implicitly or explicitly punish staff—say, with extra paperwork—when a parent asks to use the nursery or wants to formula feed, ensuring instead that policies are bureaucratically neutral and let the patient lead
- eliminate misleading and coercive forms and materials that exaggerate the harms of formula feeding while dismissing the potential harms of breastfeeding
- prioritize the parent's mental health and physical recovery as highly as maintaining breastfeeding exclusivity
Back at work, I related my own experience to the NWHN’s work on reproductive coercion, particularly our leadership on long-acting reversible contraceptives (LARCs) and sterilization.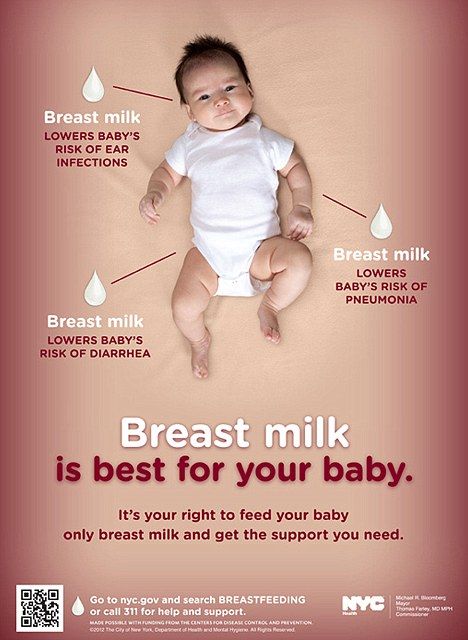 In addition to providing women with good information, we also work towards systemic reform so that women are supported in making those well-informed choices without coercion.
In addition to providing women with good information, we also work towards systemic reform so that women are supported in making those well-informed choices without coercion.
In 1979, we recognized that too many doctors were trying to take advantage of women at their most vulnerable to enforce a racist or classist agenda, and we fought for policy changes to safeguard against sterilization coercion. In 2019, we continue to push funders and providers to drop coercive contraceptive policies and quotas and we train providers, counselors, and policymakers on how to build patient-centered systems that help women end up with the sexual and reproductive health care that’s right for them.
In my professional work, I train health providers on the need to listen to their patients to avoid the pitfalls of coercion. But it wasn’t until I fed my starving child for the first time that I really understood.
Sarah Christopherson, MA, is the Legislative Director for the social justice campaign, Americans for Tax Fairness, and the NWHN’s former Policy Advocacy Director. Her 10 years working for Congress and her deep knowledge of health policy and consumer protection make her the NWHN’s issue area expert on federal health reform implementation and defense, drug and device safety and efficacy, and sexual and reproductive health.
Her 10 years working for Congress and her deep knowledge of health policy and consumer protection make her the NWHN’s issue area expert on federal health reform implementation and defense, drug and device safety and efficacy, and sexual and reproductive health.
Read more from Sarah Christopherson.
The continued availability of external resources is outside of the NWHN’s control. If the link you are looking for is broken, contact us at [email protected] to request more current citation information.
6 "Rules" About Hospitals Offering Formula That Every New Mom Should Know
Life
polkadot/Fotolia
by Steph Montgomery
If you're pregnant, you've probably already thought about how you'll inevitably feed your baby. It's natural to wonder how the hospital you deliver at might play a roll in that decision, too. If you plan to formula-feed from the start, or simply want to have formula available in case breastfeeding doesn't work out or you want to supplement, you might be surprised to learn that there are actually "rules" about hospitals offering formula. At some hospitals, getting formula to feed your baby isn't as easy as asking for it or checking a box on an intake form.
If you plan to formula-feed from the start, or simply want to have formula available in case breastfeeding doesn't work out or you want to supplement, you might be surprised to learn that there are actually "rules" about hospitals offering formula. At some hospitals, getting formula to feed your baby isn't as easy as asking for it or checking a box on an intake form.
According to Baby-Friendly USA, U.S. hospitals that have received a Baby-Friendly Hospital Initiative (BFHI) designation must follow certain rules about when and how they offer formula to new parents. Designed to promote exclusive breastfeeding, they follow the World Health Organization's (WHO) "Ten Steps to Successful Breastfeeding," which, as SELF reports, might limit a new parent's ability to use formula to feed their babies in these specific hospitals after childbirth. According to the 2016 BFHI guidelines, all babies are to be considered breastfeeding unless, after receiving breastfeeding counseling and education, their moms state otherwise. This means that, at some hospitals, nurses are not allowed to offer formula unless it's requested, or, as reported by the Fed Is Best Foundation, new moms have signed a waiver acknowledging the so-called risks of formula-feeding. Other hospitals will allow formula only with a doctor's prescription.
This means that, at some hospitals, nurses are not allowed to offer formula unless it's requested, or, as reported by the Fed Is Best Foundation, new moms have signed a waiver acknowledging the so-called risks of formula-feeding. Other hospitals will allow formula only with a doctor's prescription.
If you decide to supplement with formula, the BFHI recommends that you not use a bottle, because they believe it might interfere with breastfeeding. Instead, some BFHI hospitals have new moms use a syringe, cup, spoon, supplemental nursing system, or even their finger and some tubing to give their baby formula when needed. So with that in mind, here's a few formula-feeding rules some hospitals abide by that all parents should be aware of:
No Free Formula Samples
According to Baby-Friendly USA, BFHI hospitals are required to follow the World Health Organization's "International Code of Marketing of Breast-Milk Substitutes," which means that they can't give out free samples of formula or related supplies, like bottles or nipples to new parents.
They Can't Offer Formula
In order to promote exclusive breastfeeding, BFHI hospitals are not allowed to offer formula unless it is requested. According to their 2016 Guidelines and Evaluation Criteria, "Breast milk should be the standard for infant feeding. All infants in the facility should be considered to be breastfeeding infants unless, after giving birth and being offered help to breastfeed, the mother has specifically stated that she has no plans to breastfeed."
Only If Medically Necessary
According to Baby-Friendly USA, hospitals are allowed to offer formula if it is medically necessary. In practice, however, the process can be a bit more complex. As mom Julisa Gendren told Romper via email, "I had to sign my name eight times to give my daughter formula. I asked for a lactation consultant, but there weren't any available because it was the weekend. It was the middle of the night. I had been nursing for two hours straight, and [my daughter] was inconsolable. She had lost seven percent of her body weight on day two of her life."
She had lost seven percent of her body weight on day two of her life."
Only If Mom Signs A Waiver
Adventist Health BakersfieldAccording to the Fed is Best Foundation, some hospitals require moms who want to use formula to sign a waiver, acknowledging the "risks" of formula feeding, which they claim are not based on facts or scientific evidence. Romper corresponded with one new mom, K, via email who went through this process at a BFHI hospital in Bakersfield, California when her second child was born eight weeks ago.
"It was the night I had given birth. I had been breastfeeding for hours on and off," she says. "I knew [my son] needed some formula, and I needed a break. I hadn’t slept in days. I called the nurse, asked for formula, and when she came back with it she said, 'I have to have you sign this before I can give you this formula.' I was exhausted and alone and completely unable and unwilling to argue even though I felt it was unfair."
Only With A Prescription
As mom of two, Victoria Lopez-Garrett learned that some hospitals even require a prescription for formula. She told Romper via email, "I had to bring a prescription for formula, since I wanted to formula-feed from birth with my second. With my first I was denied formula because I didn’t have a prescription. The next day at her pediatrician's office, we found out she had lost over a pound. She was starving. I had been instructed to starve her."
She told Romper via email, "I had to bring a prescription for formula, since I wanted to formula-feed from birth with my second. With my first I was denied formula because I didn’t have a prescription. The next day at her pediatrician's office, we found out she had lost over a pound. She was starving. I had been instructed to starve her."
You Can't Use A Bottle
When she had her son two years ago, first-time mom Whitney was shocked to learn that bottles weren't allowed at her hospital. She told Romper via email, "Formula was never offered, not even after my son was readmitted with dangerous bilirubin levels. As a first time mom I was too nervous to ask for it, and the lactation consultant told me it wasn’t necessary and that I just needed to nurse, pump, and then finger feed every two hours, because bottles weren't allowed."
According to the BFHI Guidelines, "any fluid supplementation (whether medically indicated or following informed decision of the mother) should be given by tube, syringe, spoon, or cup in preference to an artificial nipple or bottle. "
"
What does Baby Friendly Hospital status mean
We use cookies
to improve!
Good
Author: Ekaterina Mokshankina
April 7, 2022
697 Views
In 1990 WHO adopted the Declaration, Promotion and Support of Breast Frecking, - Specialists of the Organization talked about the need to create the conditions under which mothers will feed the mother children only by breastfeeding, if there are no contraindications for this in the women themselves and their children. To consolidate the principles of this declaration, in 19In 1991, WHO, together with UNICEF, developed the Baby Friendly Hospital initiative.
Baby-friendly hospital is an international designation given by WHO and UNICEF to hospitals for supporting breastfeeding. First of all, the initiative concerned maternity hospitals, but in 2003 antenatal clinics and children's clinics joined it. Today, 23,000 hospitals around the world are considered child-friendly. According to the Russian Association of Physicians in Support of Breastfeeding, as of March 1, 2013, 288 maternity hospitals, 153 antenatal clinics and 197 children's polyclinics.
According to the Russian Association of Physicians in Support of Breastfeeding, as of March 1, 2013, 288 maternity hospitals, 153 antenatal clinics and 197 children's polyclinics.
We emphasize that this initiative was born in 1991. Today, experts say that breastfeeding is the best nutritional option for a child's health, but not the only possible one. Not all women breastfeed, even if they have milk: for some it is simply painful to do this, for others they need to go to work faster. And children also have allergies, and until doctors find out what exactly, a woman has to sit on buckwheat and water or switch to mixtures. Women can choose how they feed their baby, and formula can be a safe and healthy option.
Editorial by Kuprum:
In this article, we will talk about the WHO initiative and its principles. This does not mean that breastfeeding is the only sure way to feed a child, and only bad mothers feed their babies with formula. If you are uncomfortable or do not like breastfeeding your baby, you do not need to force it and suffer. If a child is not breastfed, this does not mean that he will definitely grow up less healthy.
If you are uncomfortable or do not like breastfeeding your baby, you do not need to force it and suffer. If a child is not breastfed, this does not mean that he will definitely grow up less healthy.
In the 1970s, formula milk became popular in America and later in the less developed countries of Asia and Africa. For example, the Nestlé company distributed them among the poor with the label "humanitarian aid".
The World Health Association and UNICEF noted that infant mortality has increased in underdeveloped countries with the spread of formula milk. In addition to problems with immunity, others arose when refusing breast milk due to improper preparation of mixtures. According to the instructions, the mixture must be diluted in clean drinking water, which not all families have access to, and some mothers saved the powder and diluted less than recommended. As a result, children were malnourished and lacked nutrients.
In 1981, the WHO developed a code for formula manufacturers, which prohibited open advertising in maternity hospitals, for example, it was not possible to give free samples to mothers of newborns.
In the 1991 declaration, WHO also called on all countries to follow the principles of supporting breastfeeding in order to reduce child mortality.
The initiative is based on the document "10 Steps to Successful Breastfeeding", which lists the principles of operation of maternity facilities. Here is what these principles look like in the 2018 revision of the document.
- The health facility has written policies on breastfeeding practices that all staff are made aware of.
- Employees are taught about breastfeeding.
- Staff teaches patients about breastfeeding and its benefits for mother and baby.

- In the first 60 minutes after birth, the baby is placed next to the mother for skin-to-skin contact: this is how the “golden hour” rule is implemented, during which the child must recognize and remember the mother, and the woman must realize motherhood.
From the editors of Kuprum:
Maternal instinct does not exist. After childbirth, the mother may not only not feel attachment to the child, but also feel hostility - this is a normal reaction of the body to experienced stress.
- Breastfeeding specialists teach women how to breastfeed properly and how to keep lactating if they are separated from their baby.
- They try to leave breast milk as the only source of nutrition for newborns, and milk formulas are not given without medical indications. Reasons to give formula are listed in the WHO document "Acceptable Reasons for Using Breast-milk Substitutes", last revised 2009of the year.

- Mother and child must be in the same room around the clock.
- Breast should be given to the child not on schedule, but on demand.
- In the maternity hospital, children are not given products that soothe them or imitate breasts.
- Doctors of the medical institution consult women by hotline or in groups on various resources.
At first, the WHO compiled manuals for staff training, which were issued jointly with regional doctors, then the hospital submitted an application to UNICEF, and the organization sent an employee for certification. In 2019In 1999, the initiative to coordinate statuses with UNICEF was suspended: now regional health organizations should designate child-friendly hospitals.
It is important to understand that a hospital's lack of such status does not mean that it is opposed to breastfeeding.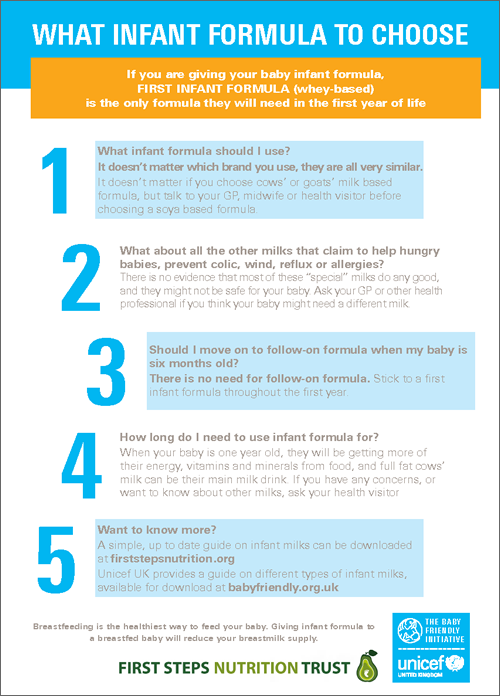 This status is nominal and does not give the maternity hospital and the clinic any privileges, and certification, as we have already said, is optional, that is, even if the hospital management does not seek to get a postscript to the name, the staff can still support breastfeeding without any manuals.
This status is nominal and does not give the maternity hospital and the clinic any privileges, and certification, as we have already said, is optional, that is, even if the hospital management does not seek to get a postscript to the name, the staff can still support breastfeeding without any manuals.
Moreover, breastfeeding is not a dogma to be followed fanatically.
The American Academy of Pediatrics states that breastfeeding is important for a child's immune system and protects against a number of illnesses, including:
- diarrhea;
- respiratory infections;
- necrotizing enterocolitis - a violation of the intestinal microflora, which leads to perforation of the intestinal wall;
- otitis media;
- urinary tract infections;
- late sepsis in premature babies;
- lymphoma, leukemia and Hodgkin's disease is a malignant disease of lymphoid tissue.

Breastfeeding has been shown to reduce the risk of developing allergies, asthma, obesity and type 2 diabetes. However, more research is needed to confirm this.
Breastfeeding also benefits the mother by reducing postpartum bleeding, helping the uterus recover faster, and reducing the risk of breast and ovarian cancer.
Breast milk also contains polyunsaturated fatty acids, which are not found in milk mixtures - they are responsible for the development of the retina and gray matter of the brain. However, there are disadvantages to breastfeeding without supplements, for example, the baby may not get enough vitamin D.
Moreover, there are times when breastfeeding is not enough for good nutrition.
In February 2012, Gillian Johnson's baby went into cardiac arrest from malnutrition and dehydration because doctors at the hospital insisted on breastfeeding and the mother had no milk. Gillian said that the nurses refused to give her son complementary foods, and instead advised her herbal infusions so that she would have milk. The child was connected to a life support machine, but two weeks later, due to irreversible changes in the brain, he had to be turned off.
Gillian said that the nurses refused to give her son complementary foods, and instead advised her herbal infusions so that she would have milk. The child was connected to a life support machine, but two weeks later, due to irreversible changes in the brain, he had to be turned off.
Dr. Michelle Castillo-Hegy experienced a similar attitude from the medical staff: she gave birth in the clinic and breastfed her baby for the first week, but there was not enough milk. The child's blood sugar level dropped and body weight decreased, but the medical staff kept silent about this and did not offer complementary foods. The child was saved in intensive care, but this affected his further development. After that, Michelle created the volunteer organization Fed is Best, which advocates for the rejection of the idea of the exclusive benefits of breastfeeding only. The specialists of the organization advocate that it is possible to feed with both breast and mixtures and combine both methods, the main thing is the safety of the child. The WHO itself also writes about the possibility of combining breastfeeding and formula.
The WHO itself also writes about the possibility of combining breastfeeding and formula.
Rosen-Carol, PhD, a breastfeeding specialist at the University of Rochester, says mothers should be given the freedom to choose how they feed their babies. In her opinion, if the mother is not forced to breastfeed as the only option, she will be more willing to choose this method. Some research supports this idea: the ability to add formula to a baby's diet reduces stress on the mother, which increases breast milk production. Other studies have found no such association.
It is not exclusive breastfeeding that is important for a child's health, but regular and nutritious nutrition. In addition, the mother's health and emotional state must be taken into account: if a woman does not want or cannot breastfeed, she can choose other options.
Listen in Cuprum:
How do you rate the article?
Understandable
Unclear
Topics
Polyclinic
Editor's Choice
Analysis
→
Why do you need dolls in a wheelchair
176 views
Children's health
November 2, 2022
→
How to build trust relations with a child
431 431 431 431 Children's health 9000 Parsing
→
A child was diagnosed with rickets: what to do
205 views
0004
→
How children learn language and what is bilingualism
634 views
Child health
September 30, 2022
Baby friendly hospital - what does it mean?
Brief background.
The aggressive promotion of formula milk manufacturers by the second half of the 20th century led to a significant decrease in the prevalence of breastfeeding. The negative effect of this phenomenon was very clearly visible in the developing countries of Asia and Africa (where breast milk substitutes were supplied for charity purposes): children died from diarrhea / dehydration and other infections.
In the 1970s, information was brought to the attention of the general public; details can be found, for example, in the Wikipedia article Boycott Nestle. And in 1981, at the 34th World Health Assembly, International Code of Marketing of Breast-milk Substitutes (in another translation, the International Code of Marketing of Breast-milk Substitutes) was adopted. The full text of the Code can be found at WHO website.
The work to support breastfeeding did not stop there. At 1989 WHO and UNICEF published "Ten Steps to Successful Breastfeeding" - recommendations to be followed by health facilities serving mothers and newborns. And then, in 1991, to motivate hospitals more, they introduced the Breastfeeding Friendly Hospital Initiative: those institutions that can document full compliance with the Ten Steps can be assigned status Baby Friendly Hospital . To obtain the title, it is necessary to pass an examination and certification by external experts.
And then, in 1991, to motivate hospitals more, they introduced the Breastfeeding Friendly Hospital Initiative: those institutions that can document full compliance with the Ten Steps can be assigned status Baby Friendly Hospital . To obtain the title, it is necessary to pass an examination and certification by external experts.
Almost 30 years have passed and not so long ago, in 2018, the revised "Baby Friendly Hospital Initiative" was introduced. The full document can be downloaded from the WHO website (or in English: Baby-friendly hospital initiative (BFHI)).
In the revised version, some of the "steps" have been simplified in terms of their use in order to ensure their practicality and suitability for all healthcare facilities. The document itself contains more than 60 pages of rationale for each step, recommendations for implementation and standards that must be implemented in a medical institution to receive the title, as well as recommendations for implementing the initiative at the national level. Below are the steps themselves with some comments.
Below are the steps themselves with some comments.
Ten Steps to Successful Breastfeeding (2018 Version)
- Hospital Policies
a. Comply fully with the International Code of Marketing of Breast-milk Substitutes and relevant World Health Assembly resolutions.
In popular terms: Do not advertise or promote the sale of infant formula, feeding bottles or nipples
b. Have a written policy regarding infant feeding and communicate it regularly to medical staff and parents.
c. Establish permanent monitoring and data management systems.
- Professional competence of personnel
Ensure staff have sufficient knowledge, competencies and skills to support breastfeeding appropriately.
- Antenatal care
Discuss with pregnant women and their families the importance and technique of breastfeeding.
In popular terms: To teach women how to feed their baby.
 Most women are able to breastfeed if they have the right help.
Most women are able to breastfeed if they have the right help. - Immediate postpartum care
Early and uninterrupted skin-to-skin contact between mother and child after birth should be encouraged and mothers should be encouraged to initiate breastfeeding as soon as possible after birth.
- Practical support for mothers in breastfeeding
Mothers should be given practical support to start and continue breastfeeding and to learn how to overcome the usual practical difficulties associated with breastfeeding.
In a popular setting: Check if the position for breastfeeding is chosen correctly, if the baby is correctly attached to the breast and if he sucks at the breast. Breastfeeding is a natural process, but most mothers will need help with this in the beginning.
- Power supply
Do not give breastfed newborns any food or drink other than breastmilk, unless medically indicated.
In the popular presentation: Feeding infant formula in a health facility makes it difficult to start breastfeeding.

If it is necessary to introduce additional nutrition, preference should be given to donor breast milk.
Mothers who want to feed their baby formula should be helped to do so in safe ways. - Joint stay in the same room of mother and newborn
Allow mothers to stay with their babies and stay together in the same room day and night.
Ensure that mothers of sick babies can be near them. Mothers should be close to their babies to notice and respond to their baby's signals and reactions regarding feeding needs.
- Feeding according to the child's response
Mothers should be supported and trained to recognize and respond to their baby's signals and reactions regarding feeding needs.
Do not limit the duration of breastfeeding.
Breastfeeding babies on demand is good for everyone. - Feeding bottles, teats and pacifiers
Counsel mothers about the use of feeding bottles, nipples, pacifiers, and the associated risks.

In the popular phrasing: Everything that enters the baby's mouth must be clean.
- Discharge assistance
Ensure that discharges are coordinated so that parents and their children have timely access to ongoing support and appropriate care.
Popularly put: Refer mothers to community resources for support with breastfeeding. Collaborate with local communities to improve breastfeeding support services.
Baby-friendly hospitals in Russia for 2019
In the Russian Federation, the Initiative began to be implemented in 1996. Based on the results of certification, the institution is awarded the WHO/UNICEF International Diploma and the National Diploma of the Scientific and Practical Center for the Promotion, Support and Encouragement of Breastfeeding "Baby Friendly Hospital". The first certified maternity hospital, according to the Russian Association of Physicians in Support of Breastfeeding, was the maternity hospital in Elektrostal, Moscow Region. In the same place, on the website of the Association, you can find a list of maternity hospitals with BDR status, but only until 2013. Meanwhile, according to the Initiative, external evaluations should be carried out regularly - no less than once every five years , preferably more often. Below is a list of recent certifications of Russian maternity hospitals.
In the same place, on the website of the Association, you can find a list of maternity hospitals with BDR status, but only until 2013. Meanwhile, according to the Initiative, external evaluations should be carried out regularly - no less than once every five years , preferably more often. Below is a list of recent certifications of Russian maternity hospitals.
→
About childbirth and maternity hospitals
Pregnancy and health
Nutrition during pregnancy
Breastfeeding
About children
Legal issues during pregnancy and childbirth 9020
#EP after cesarean #childbirth with husband for free #PKS #childbirth with fibroids #childbirth with a scar on the uterus #third caesareanNote
What to bring to the hospital?
Doctors of Moscow and Moscow Region
Which maternity hospital in Moscow is better? Statistics!
Washing schedule in Moscow
Washing schedule in St.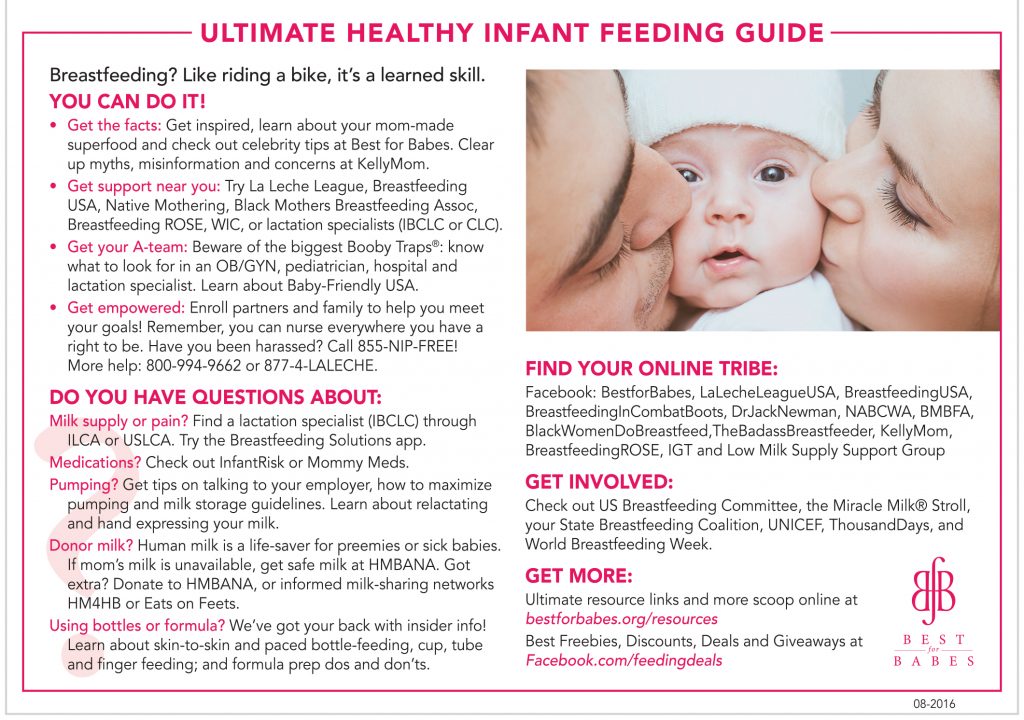 Petersburg
Petersburg
₽Prices for childbirth in maternity hospitals in Moscow
Useful reviews of the month
Maternity Hospital City Clinical Hospital No. 15 named after O.M.Filatov (Moscow)
90☆☆ ★ rating: 3Ivolgina Olga → Oh, no, I gave birth there, and if I had another pregnancy, I definitely wouldn't go there. And I would not advise others to give birth there under the CHI policy. This was my second birth. I arrived there without a referral, but with stomach pains. The deadline was the 41st week, the DA had already passed. In the evening, at six o'clock, very busy...
[full review]
Maternity hospital in Kommunarka (Moscow)
☆☆☆☆★ rating: 1
Ekaterina → I went to Kommunarka in an ambulance for a period of 39.2 with contractions with a frequency of 10 minutes. Third birth. They did an ultrasound, CTG, examination on a chair and turned back home, because.