Formula feeding baby guide
Choosing an Infant Formula | Nutrition
alert icon
Information about finding infant formula can be found
here.external iconAdditional information to help families during the infant formula shortage can be found
here.alert iconCDC’s investigation of Cronobacter infections in infants who consumed powdered infant formula from the Abbott Nutrition facility in Sturgis, MI, is now closed. No new cases have been identified. Get updates about FDA’s investigationexternal icon.
No brand of infant formula is best for all babies. You should pick an infant formula that is made especially for babies. The US Food and Drug Administration (FDA) regulates commercial infant formulas to make sure they meet minimum nutritional and safety requirements. Iron-fortifiedalert icon infant formulas are recommended, and most commercial infant formulas sold in the United States contain iron. Commercial infant formulas come in liquid and powdered forms.
When choosing an infant formula:
- Make sure it is not expired.
- Make sure the container is sealed and in good condition. If there are any leaks, puffy ends, or rust spots, do not feed it to your baby.
- Make sure it is not labeled for toddlers.
Talk with your child’s doctor or nurse if you have questions about choosing an infant formula for your baby or if you are thinking of switching infant formula brand or type.
Homemade Infant Formula
FDAexternal icon and the American Academy of Pediatricsexternal icon warn against using recipes to make homemade infant formula. Using homemade infant formula can lead to serious health problems for your baby. Your baby’s nutritional needs are very specific, especially in the first year of life. Homemade infant formulas may contain too little or too much of certain components, such as vitamins and minerals (like iron).
Homemade infant formula may also have an increased risk of contamination, which could lead to your baby getting sick or developing an infection. Commercial powdered formulas are also not guaranteed to be sterile. However, FDA regularly inspects these products and the manufacturing facilities where they are made to help make sure these products are safe.
Commercial powdered formulas are also not guaranteed to be sterile. However, FDA regularly inspects these products and the manufacturing facilities where they are made to help make sure these products are safe.
Imported Infant Formulas
There are some public claims that infant formulas sold in other countries and promoted as “natural” or “organic” are better for babies. However, there is no scientific evidence that these infant formulas are better for babies than commercial infant formulas sold in the United States. All infant formulas legally sold in the United States—whether made in the United States or imported from other countries—must be reviewed by FDA. The American Academy of Pediatrics warns against using illegally imported formulas, such as products ordered online from third-party distributors. FDA may not have not reviewed these products. Illegally imported formulas also may not have been shipped and stored properly.
FDA reviews all infant formulas sold legally in the United States to make sure they meet minimum nutritional and safety requirements.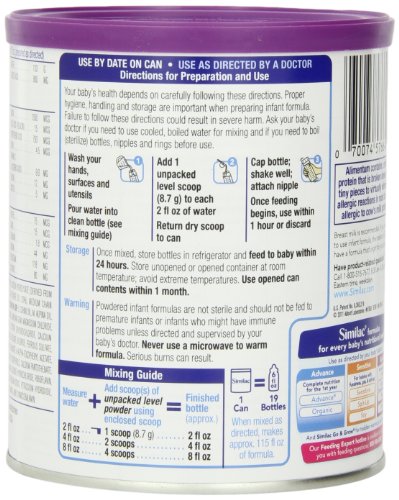 FDA also makes sure that the water used to make formulas meets safety standards set by the US Environmental Protection Agency.
FDA also makes sure that the water used to make formulas meets safety standards set by the US Environmental Protection Agency.
Toddler Milks, Drinks, or Formulas
Toddler milks, drinks, or formulas are not needed to meet the nutritional needs of young children. They typically have added sugars. At age 12 months, your child can be introduced to plain whole cow’s milk or fortified unsweetened soy beverage.
Babies younger than age 12 months should be fed infant formulas specifically designed to meet their nutritional needs. They should not be fed toddler milks, drinks, or formulas labeled for toddlers.
Top of Page
Feeding Guide for the First Year
Feeding Guide for the First Year | Johns Hopkins MedicineReviewed By:
Tiffani Hays, M.S., R.D., L.N., Director of the Pediatric Clinical Nutrition Education & Practice
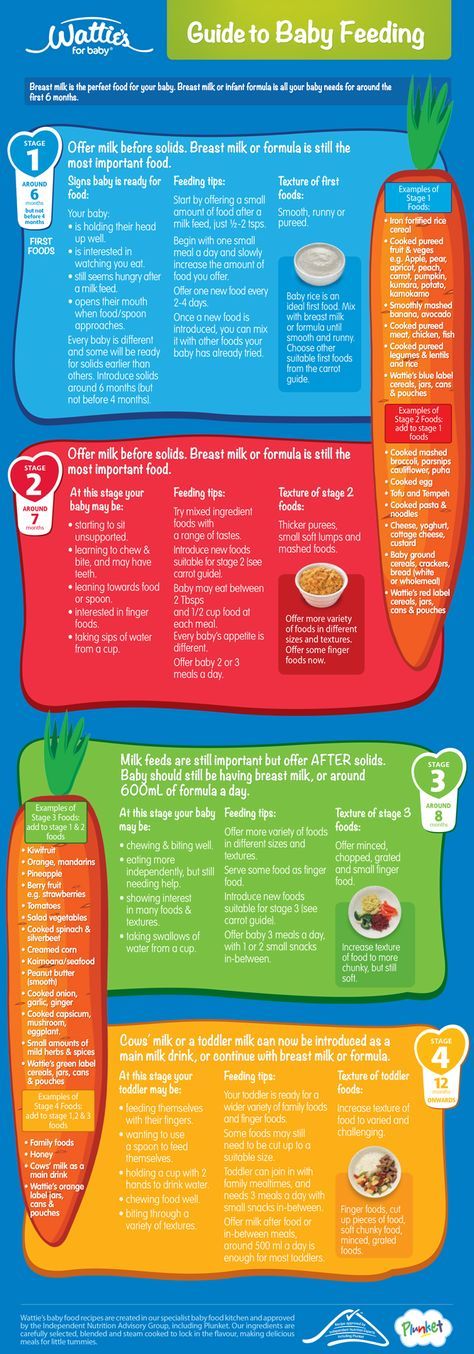
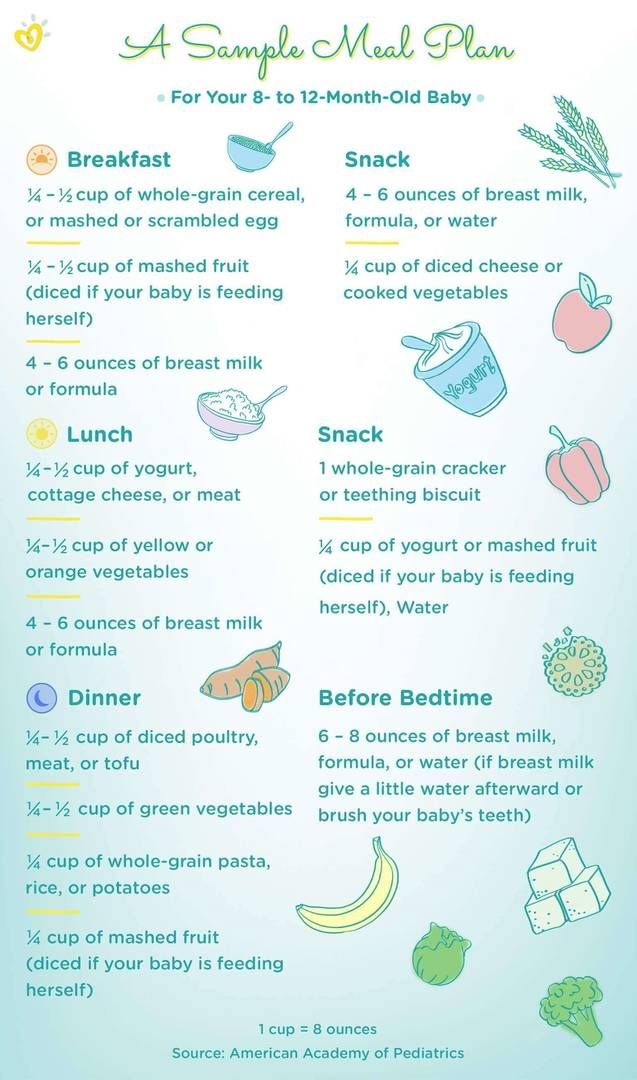
Making appropriate food choices for your baby during the first year of life is very important. More growth occurs during the first year than at any other time. It’s important to feed your baby a variety of healthy foods at the proper time. Starting good eating habits at this early stage will help set healthy eating patterns for life.
More growth occurs during the first year than at any other time. It’s important to feed your baby a variety of healthy foods at the proper time. Starting good eating habits at this early stage will help set healthy eating patterns for life.
Recommended Feeding Guide for the First Year
Breast milk and formula are designed to be the primary sources of nutrition throughout an infant’s first year of life. You should talk with your baby’s health care provider before starting solid foods. Solid foods should not begin before age 4 months because:
- Breast milk or formula provide your baby with all the nutrients that are needed.
- Your baby isn’t physically developed enough to eat solid food from a spoon.
- Feeding your baby solid food too early may result in poor feeding experiences and increased weight gain in both infancy and early childhood.
The American Academy of Pediatrics (AAP) recommends that all infants, children and adolescents take in enough vitamin D through supplements, formula or cow’s milk to prevent complications from deficiency of this vitamin. In November 2008, the AAP updated its recommendations for daily intake of vitamin D for infants, children, and adolescents who are healthy. It is now recommended that the minimum intake of vitamin D for these groups should be 400 IU per day, beginning soon after birth. Your baby’s health care provider can recommend the proper type and amount of vitamin D supplement.
In November 2008, the AAP updated its recommendations for daily intake of vitamin D for infants, children, and adolescents who are healthy. It is now recommended that the minimum intake of vitamin D for these groups should be 400 IU per day, beginning soon after birth. Your baby’s health care provider can recommend the proper type and amount of vitamin D supplement.
Guide for Breast-feeding (Zero to 12 Months)
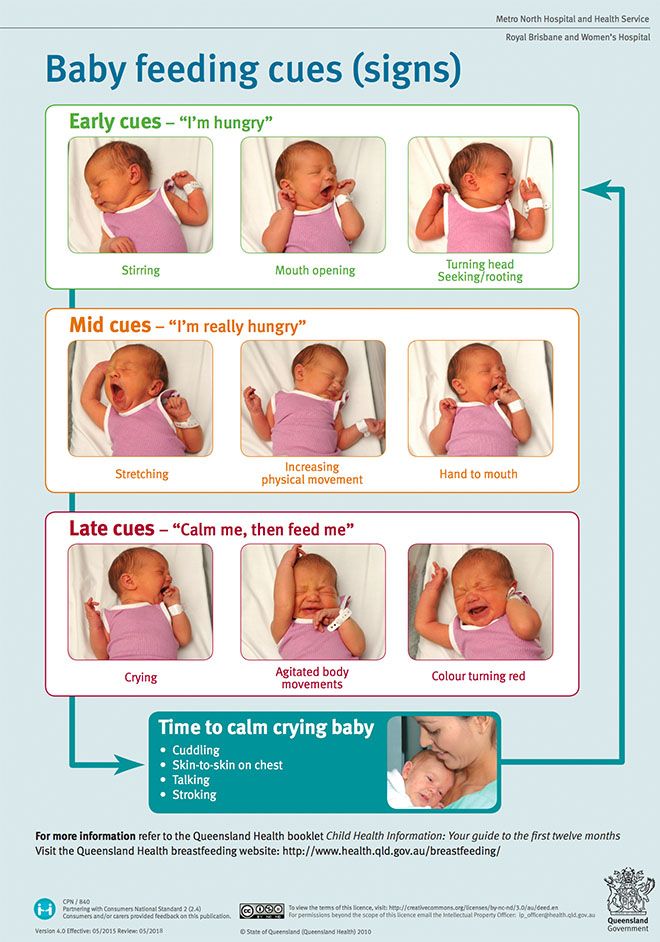
- In the early days after a baby’s birth, the mother should plan to breast-feed every two to three hours, including overnight. The mother should respond to the infant’s cues of hunger in a prompt and relaxed manner, providing a quiet and comfortable environment for both herself and the baby. Frustrated or distracted infants may have difficulties latching on.
- It is normal for infants to wake up overnight to feed for the first several months. If you have any concerns about overnight feeding, please discuss them with your health care provider.

- Alternate breasts to feed on, and allow the infant to completely empty the breast before switching to the other. This practice ensures the infant receives hindmilk, which is richer in nutrients.
- Follow your child’s feeding cues and resist forcing a schedule. Instead, rely on keeping track of wet diapers and your child’s growth to judge whether he or she is receiving enough breast milk. A mother’s milk changes as the infant grows, and feeding habits change as well in order to best meet a child’s needs. If you have any questions about whether your child is receiving enough breast milk, ask your health care provider.
- When not able to breast-feed, use a breast pump to extract milk and maintain milk supply. Pumped breast milk should be stored safely, using appropriate temperature guidelines. Pumped breast milk may be offered to infants in bottles, while responding to the same feeding cues to determine how much they take.
 Forcing bottles to be emptied may result in overfeeding and excess weight gain, even when feeding breast milk.
Forcing bottles to be emptied may result in overfeeding and excess weight gain, even when feeding breast milk. - With the proper support, a mother can meet the needs of most infants, even twins, so seek out help from your health care provider or lactation consultant for success.
Guide for Formula Feeding (Zero to 12 Months)
- When breast milk is not available, standard infant formula is an appropriate alternative for most healthy full term infants, but there are some differences between brands. Do not hesitate to ask your health care provider for a recommendation if you are unsure which formula to use.
- Bottle-feeding should be interactive, with the caregiver holding both the bottle and the infant. Propping a bottle has been linked to an increased risk of ear infections and tooth decay.
- Formula feeding should be in response to the infant’s needs and not based on a predetermined schedule.
 Look for cues of hunger and fullness to determine both when to feed and how much. The number of wet diapers per day and your child’s growth will reflect if he or she is getting enough formula. The chart below demonstrates common intakes for infants at various stages. However, ask your health care provider if you have any questions about how much formula your infant is taking.
Look for cues of hunger and fullness to determine both when to feed and how much. The number of wet diapers per day and your child’s growth will reflect if he or she is getting enough formula. The chart below demonstrates common intakes for infants at various stages. However, ask your health care provider if you have any questions about how much formula your infant is taking. - The amount of formula an infant takes will decrease as the baby increases intake of solid foods, but formula remains a significant source of calories, protein, calcium and vitamin D for the first year of life.
- Ask your health care provider before switching an infant less than 1 year of age from formula to cow’s milk or a cow’s milk alternative.
| Age | Amount of formula per feeding | Number of feedings per 24 hours |
|---|---|---|
| 1 month | 2 to 4 ounces | six to eight |
| 2 months | 5 to 6 ounces | five to six |
| 3 to 5 months | 6 to 7 ounces | five to six |
Complementary Feedings (After 6 Months of Age)
Beverages
- Offer only breast milk or formula in bottles until 1 year of age unless specifically advised by your health care provider.
- Begin offering breast milk and/or formula in a cup starting at 6 months of age. Infants should drink breast milk and/or formula for the first year of life.
- Fruit juice is not recommended under 1 year of age.
- When introducing juice, offer 100% pasteurized juice and limit it to 4–6 ounces per day. Do NOT place juice in a bottle.
- Avoid giving any sugar-sweetened beverages to infants.
Solid Foods
- Introduce solid foods when your infant is ready, at around 6 months of age depending on the infant’s development. Infants are ready to start eating solid foods when they can:
- sit up on their own or with a little support
- reach for and put things in their mouth
- open their mouth when seeing something coming
- keep food in their mouth rather than pushing it out onto the chin
- move food to the back of their mouth with their tongue
- turn their head away when they do not want something
- Prepare to introduce solid foods in a calm feeding environment where the infant is sitting upright and is appropriately supported and moderately hungry.
- Start with small amounts of solid food, feeding with a spoon or allowing finger feeding, then gradually increase the amount as the infant eats more and develops. Avoid offering breast milk or formula until after the solid-food experience has wound down.
- Expose infants to a wide variety of flavors and textures of healthy food. Don’t limit your baby’s food choices to the ones you like. Offering a range of foods early will pave the way for healthy eating habits.
- Maintain the division of responsibility when feeding.
- The caregiver is responsible for what to eat (offering appropriate variety and textures).
- The child is responsible for deciding whether to eat and how much.
- Avoid adding salt or sugar to make baby foods more appealing. Many babies and toddlers need to experience a new food multiple times before accepting it, and increased intakes of salt and sugar among children are associated with obesity in adults.

- Observe infants for any signs of intolerance when introducing a new food or texture, and discuss all concerns with your health care provider.
- Although convenient and safe, commercial baby foods are not required. Young children are more likely to eat foods they see others eating, so as long as they are observed to see how they handle new food in their mouths, baby-led weaning using table foods is an appropriate way to introduce solids.
- Avoid honey in any form during your child’s first year, as it can cause infant botulism. Address any concerns about developing food allergies with your health care provider.
- Don’t restrict fat and cholesterol in the diets of very young children, unless advised by your child’s health care provider. Children need calories, fat and cholesterol for the development of their brains and nervous systems, and for general growth.
Updated on July 26, 2019.
Related
-
Nutrition
Toddler Nutrition
-
Breastfeeding Your Baby
Breastfeeding 101: Q&A with Lactation Expert Nadine Rosenblum
-
Developmental Milestones: Babies and Toddlers
Well-Care Visits
Related Topics
Breastfeeding for beginners | Philips Avent
search support iconSearch Keywords
because it will take a long time during the first few months of a child's life. In this article, we will discuss all of its main aspects, from the basic principles of breastfeeding to the best tips for effective newborn feeding.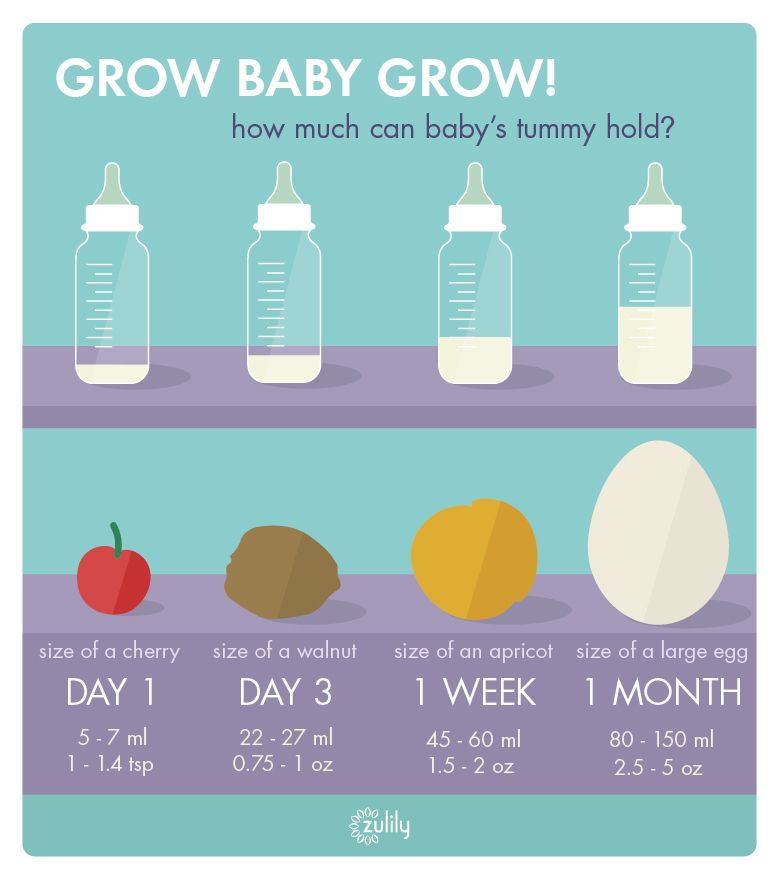
As always, if you have any questions or concerns, seek the opinion of another specialist.
Basic principles of breastfeeding
Although every baby is different, newborns usually eat every two to three hours, for a total of 8 to 12 times a day. In the first one or two days after birth, babies usually drink 25-50 ml of milk per feeding. This volume will gradually increase to 50-75 ml when the baby is about two weeks old.
More information on how much a newborn should eat can be found here.
How long does one feeding last?
Again, every baby is different, so there is no set time frame for every newborn. But in general, breastfeeding a newborn takes five minutes to one hour. This time depends on the size, age of the baby and the frequency and duration of feeding the newborn.
How to start breastfeeding?
In the very first minutes of a child's life, his mother should put the baby on her chest and ensure body contact. This time is called the "golden hour": it is at this hour that a connection is established between mother and child and the newborn's natural instinct to seek the breast manifests itself. As soon as the child begins to show signs of hunger, you need to give him a breast.
This time is called the "golden hour": it is at this hour that a connection is established between mother and child and the newborn's natural instinct to seek the breast manifests itself. As soon as the child begins to show signs of hunger, you need to give him a breast.
Mothers who are just learning to breastfeed their newborns should remember that comfort is key. There is no better way to ensure breastfeeding success than by creating a comfortable and relaxing environment for the mother. For starters, mom can sit comfortably on the couch, on the bed, or in a chair with pillows to support her back while feeding. Breastfeeding moms can get creative with breastfeeding and choose specific lighting, soothing music, or anything else that helps them relax.
Bring your baby to your breast, not the other way around. If you want to make breastfeeding a newborn easier, then do not lean towards the baby, but bring it to your chest. The baby's mouth should be opposite the nipple, the neck should be straight, and the shoulders and hips should be in line.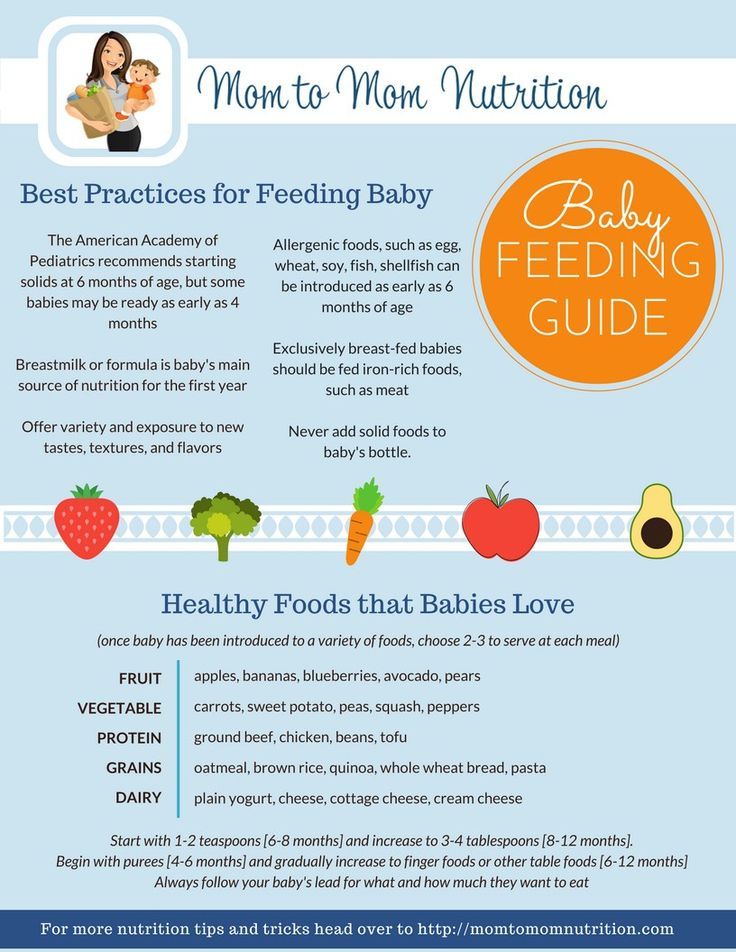 Mom can also lightly touch her nipple to her baby's nose and mouth to encourage him to latch on.
Mom can also lightly touch her nipple to her baby's nose and mouth to encourage him to latch on.
Support your chest. Holding the newborn with one hand, the mother can place the other hand directly under the breast to support it. When learning to breastfeed, some mothers prefer to leave one hand free; in this case, a rolled towel can be used.
Breastfeeding can be done in different positions; experiment with them to find the one that works best for you and your baby. We list the most common breastfeeding techniques below:
- Cradle. In this position, the baby lies on the mother's hand from the side of the breast, which he sucks. The baby's head lies on the mother's elbow during feeding.
- Cross cradle. With a cross cradle, the mother holds the baby with the hand opposite to the mammary gland that the baby sucks. With the other hand, mom can support her breasts.
- Underhand or Football. In this position, the mother holds the child next to her, putting her back on her arm.
 With the other hand, she supports the baby's head, facing the mammary gland, with which she feeds the baby.
With the other hand, she supports the baby's head, facing the mammary gland, with which she feeds the baby.
- Lying on your side. In this position, the mother lies on her side, and the child lies next to her, facing her chest. Mom can support the child under the back with the hand that is on top, or put a folded towel under the back of the child.
Newborn Breastfeeding Tips
After looking at breastfeeding techniques, here are some tips for new mothers:
A good grip is important for both mother and baby. With a good grip, the baby will suck out milk correctly, and the mother's nipples will not hurt. To achieve a good latch, the mother needs to find a position that makes it easier for the newborn to latch onto the breast, and to do this, she should experiment with different positions. If a mother is having difficulty feeding, she should contact a lactation consultant.
2. Maintain milk supply. Sometimes a nursing mother cannot be constantly with her child during feedings. In such cases, it is very important to maintain milk production. An excellent solution for maintaining milk production when mother and baby are not together is pumping milk.
In such cases, it is very important to maintain milk production. An excellent solution for maintaining milk production when mother and baby are not together is pumping milk.
Take a look at this double breast pump: it reduces pumping time and features a massage petal attachment to gently stimulate milk flow.
3. Breastfeeding everywhere. One of the many benefits of breast milk is that mom always has it with her. But some moms feel awkward at first when they have to breastfeed their baby in public. For such mothers, we recommend that you first practice breastfeeding your newborn in front of a mirror and choose clothes that allow you to cover your breasts during feeding. A shawl or scarf can help with this - with them, the mother will feel more comfortable when feeding the baby outside the home.
And to keep clothes dry and clean while breastfeeding, we recommend that mums use these disposable bra pads with a porous and breathable structure: they do not leak and let air through.
Be prepared for difficulties. It is important for moms not to panic or get upset when faced with a common breastfeeding problem, such as insufficient milk production, breast engorgement, clogged milk ducts, mastitis, or sore nipples. To feel calm and confident during all stages of breastfeeding a baby, mothers need a circle of support: family members, friends, and healthcare professionals. The main thing is to stay calm, but if a mother is concerned about any aspect of breast health, she should definitely see a doctor. Learn more about breastfeeding difficulties and how to overcome them.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.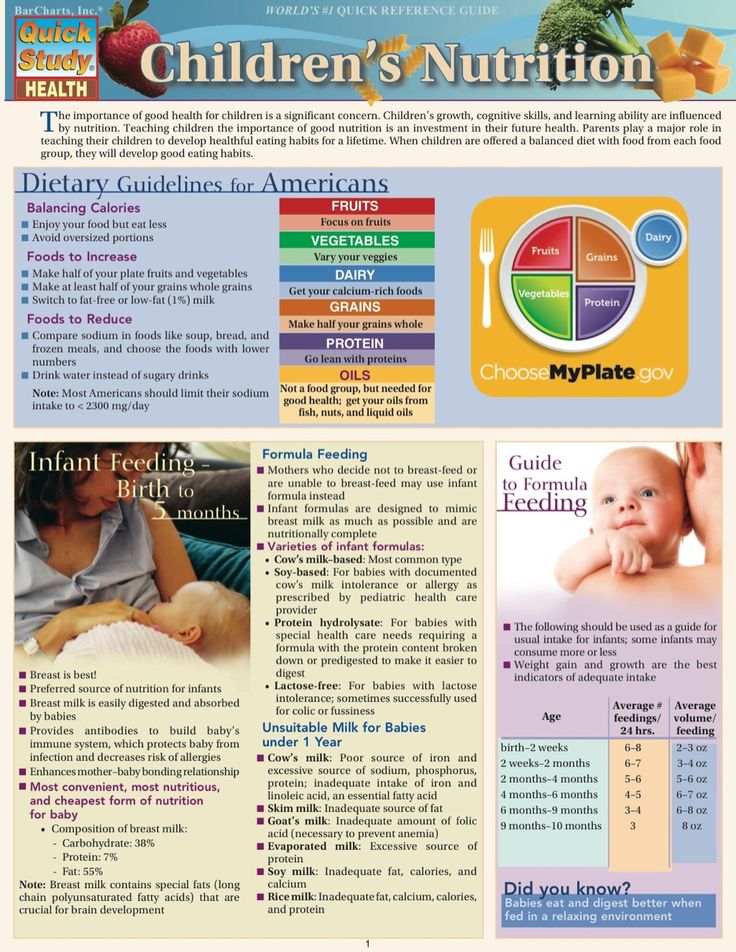
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Breastfeeding Guide.
Home » Information for patients
The benefits of breastfeeding for the baby.
Most parents are well aware of the benefits of breastfeeding for term babies. Just as important, if not more so, is breast milk for premature babies. To date, it is known that the milk of mothers who have given birth prematurely has a special composition and differs from the milk of women who have carried the pregnancy to term, as it contains in large quantities substances called enzymes that contribute to the development of the immature stomach and intestines of the child. In addition, these enzymes break down the nutrients in milk and reduce the chance that a child will develop a food intolerance.
In addition, these enzymes break down the nutrients in milk and reduce the chance that a child will develop a food intolerance.
An important benefit of mother's milk is that it provides protection against infections.
This is important because children have limited ability to fight off bacteria and viruses on their own.
Mother's milk contains many specialized protective factors, including antibodies, that protect babies from infection.
Some substances found in breast milk form a protective layer on the surface of the intestine and prevent bacteria and viruses from entering the bloodstream.
Other compounds kill microorganisms directly or prevent their growth. Some of the nutrients found in milk can perform both of these tasks at the same time.
These substances may continue to protect the baby from infection even when the baby is no longer receiving breast milk.
Breast milk contains anti-inflammatory agents that help protect the baby's delicate intestinal tissues from swelling and irritation.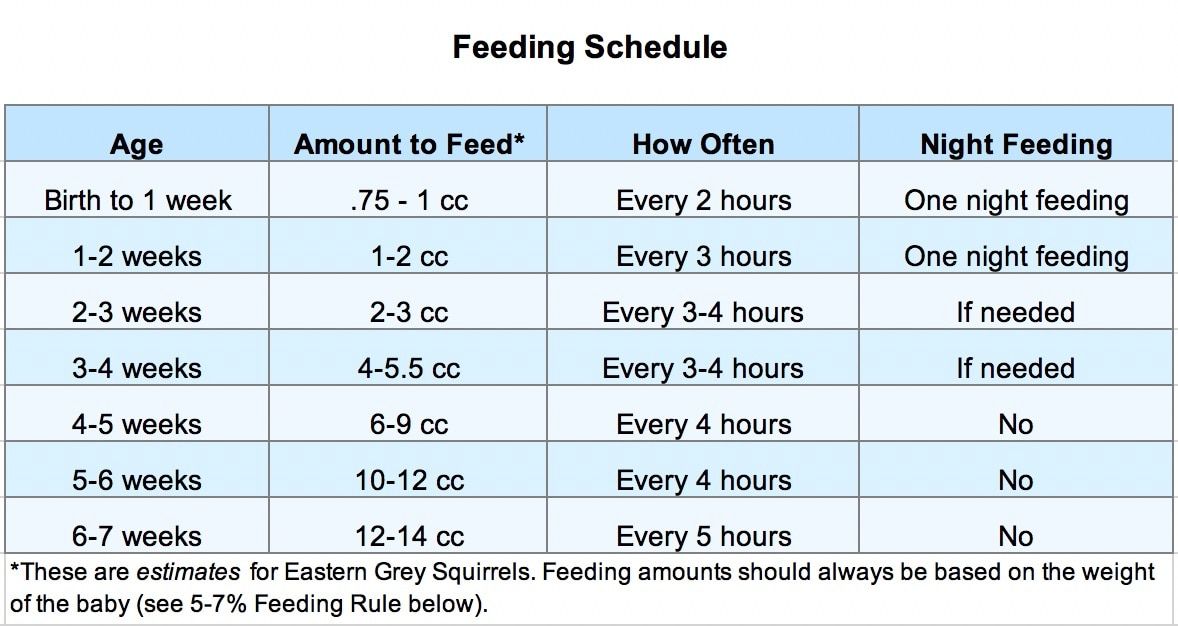 These compounds are believed to prevent the development of serious intestinal pathology in children.
These compounds are believed to prevent the development of serious intestinal pathology in children.
Breast milk is the main source of nutrition for children. The milk of a mother who gave birth prematurely contains much more protein, the need for which in a premature baby is much higher than in a full-term baby. Of particular importance is the type of fat contained in breast milk.
During the first or second day there is very little milk, only a few drops of a yellowish color. This "early" milk is called colostrum. Even a small dose of it contains a large amount of substances that help protect the child from infection. Therefore, for feeding, you should collect any, even
very small quantities of milk. Over the next few days, the milk will gradually start to increase in volume, and its color and consistency will change.
Because even small amounts of mother's milk can have a significant impact on a baby's health, it is important to start breastfeeding as soon as possible after delivery.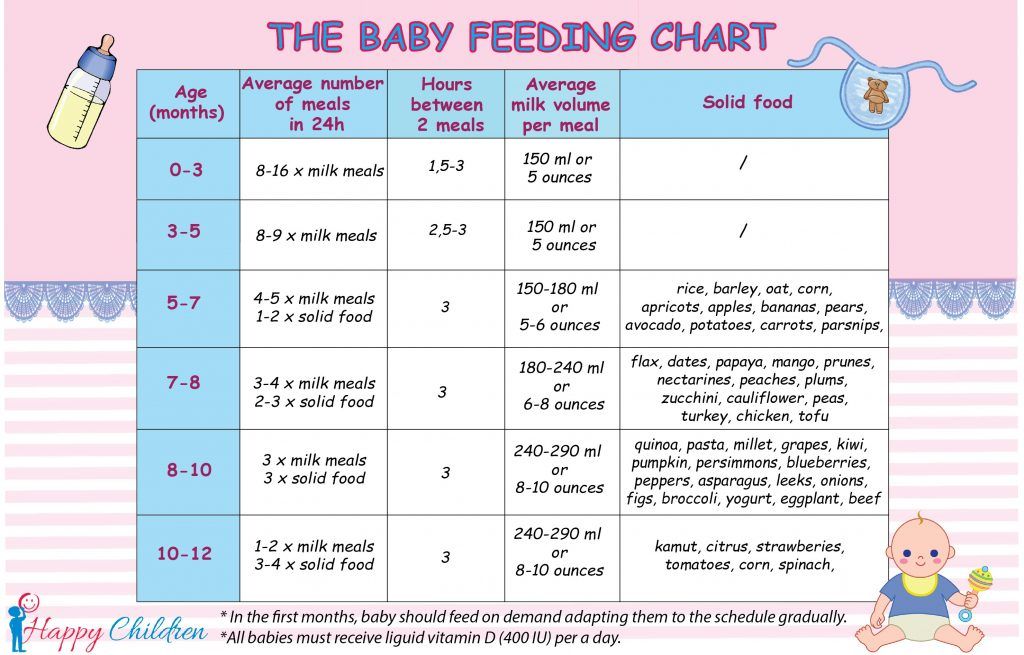
Maternal nutrition and well-being
Almost all mothers are concerned about whether they are eating properly in order to provide their baby with good milk. However, it should be emphasized that the milk that is produced in the mother's body will be nutritious, even if her diet is not ideal.
But in the process of milk production in the body, the reserves of some nutrients can be depleted, and in order to fill the needs of the mother's body, it is necessary to continue taking vitamins specially designed for lactating women.
Diet does not affect the quality of milk, but it may cause a decrease in its quantity, especially if the lack of appetite is mainly due to stress and anxiety.
Mom should not forget about her diet by filling out a diary every day, where the volume of milk is noted.
Mothers should consult their doctor before taking any medications or supplements. The neonatologist will recommend drugs that are compatible with breastfeeding and, if necessary, will consult with other specialists on this issue.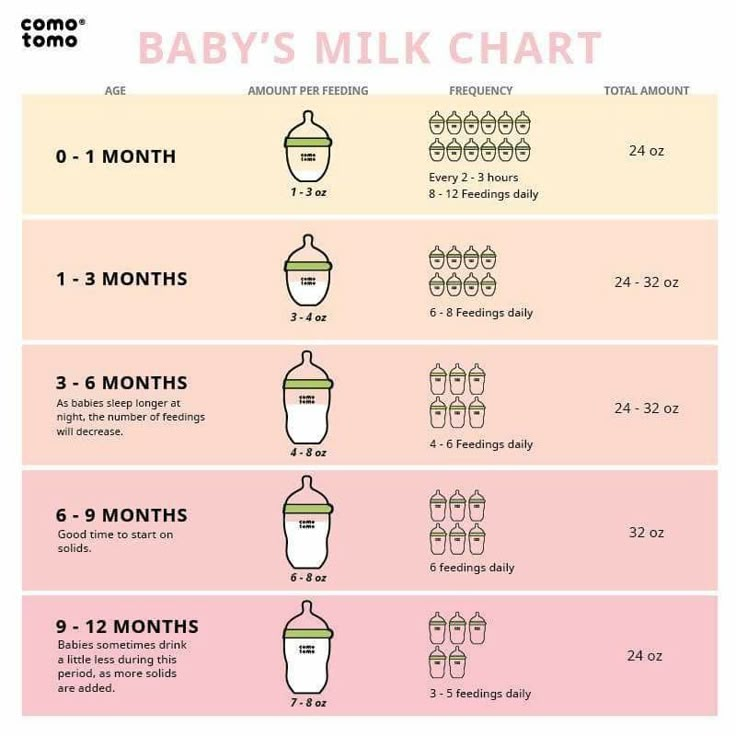
First breastfeeding and breastfeeding
The baby's general health will determine when breastfeeding can begin. There are no specific parameters for the weight or age of the child, which will allow you to say when the baby can be attached to the breast. The ability to start breastfeeding is determined by the newborn's ability to suck and swallow.
Breastfeeding positions, baby clothes
Keep the baby's head, shoulders and torso in a straight line and use the hand that holds the head to bring it closer to the breast. The child's arms should be separated and placed around the mother's chest, and his nose should
touch the surface of the breast. The other hand must hold the chest.
Two postures are particularly comfortable: the soccer ball hold and the lateral support. Both of them allow the mother to grasp the baby's head with one hand and support the breast with the other. A pillow under her forearm will help her relax her shoulders and back, and possibly allow her milk to flow more freely.
The first method allows you to better control the position of the baby's head and check whether he takes the breast correctly. It is worth trying this position if the mother is worried that the baby is very small and the breasts are large, and also if the mother is experiencing abdominal pain after a caesarean section.
Football Hold
* Place a pillow to your side to support your elbow and baby's lower body. Place the baby's head in the palm of your hand.
* Raise the baby's head to chest level.
* Support the base of the baby's head with your thumb and forefinger.
* If the baby does not seem to like it, put a soft blanket between your arm and the baby's head as a pad.
Lateral Holding Position
Lateral Holding Position is another comfortable feeding position for the baby, while the mother controls the position of the baby's head and can better see how he takes the breast.
* Hold the baby's head on your forearm perpendicular to your body, opposite the breast from which he will suckle.
* The baby will be in the same position as normal motion sickness, but you can use your other hand to hold him.
* The baby should be at chest level with the whole body pressed against the mother.
The baby does not need to be swaddled tightly - just a diaper and cap is sufficient. An undershirt is not needed because the skin of the mother's breasts is warm, the mother's skin temperature can be around 37 ° C, as heat is generated during milk production. To protect the child from heat loss, you can cover him with a blanket from above.
How to know if your baby is getting enough breast milk
Milk intake can be determined using a procedure called weighing. The baby is weighed on a very accurate scale just before and after breastfeeding. The difference between a baby's weight before and after a feed (measured in grams) is the amount of milk (measured in cubic centimeters, or milliliters) that the baby gets during a feed. For example, if the difference between the weight of the child before and after feeding is 30 grams, this indicates that he sucked 30 ml of milk from the breast.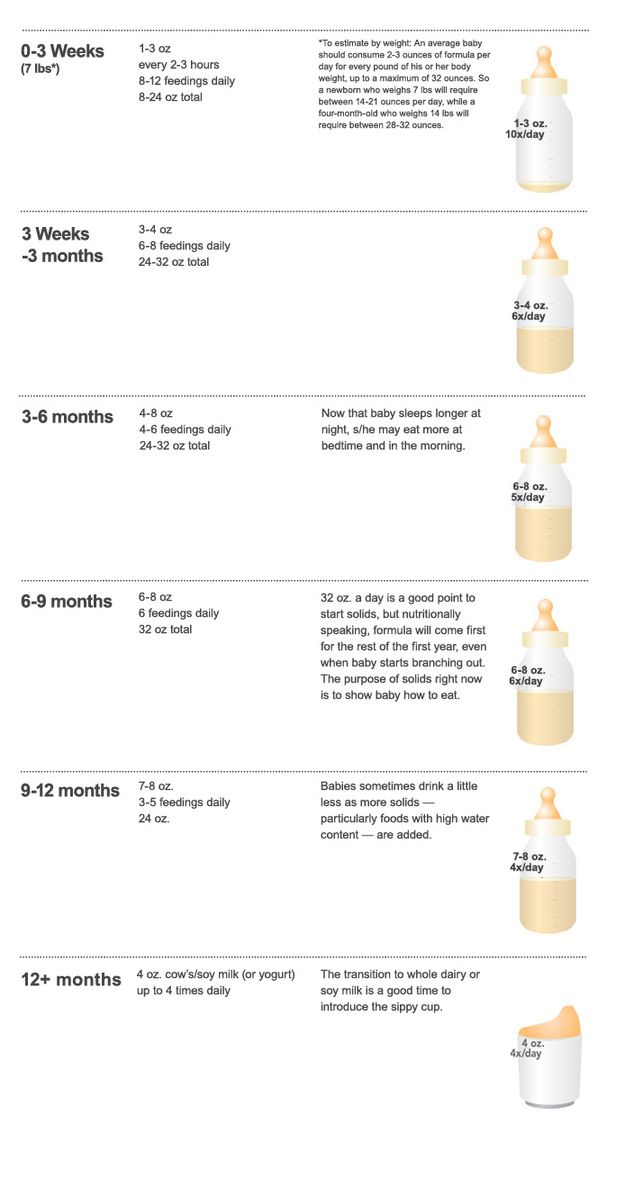 However, it should be remembered that when weighing before and after breastfeeding, the baby must be in the same clothes, which will accurately measure the amount of milk consumed. Changing the diaper between two weighings will result in inaccurate measurements.
However, it should be remembered that when weighing before and after breastfeeding, the baby must be in the same clothes, which will accurately measure the amount of milk consumed. Changing the diaper between two weighings will result in inaccurate measurements.
How to make sure your baby is breastfeeding correctly
The way your baby latch is one of the most important factors in determining the success of breastfeeding. For proper latch-on, the baby's mouth should be positioned over the milk sinuses, which are about 2.5 to 4 cm deeper than the nipple. With this arrangement, the baby will receive more milk, this will help to avoid pain in the mother during feeding and prevent the formation of nipple cracks.
Gently lift and support the chest so that the thumb is on top of the chest and the other fingers are below, well below the areola. This position is called "C-capture".
Lightly tap the baby's bottom lip with the nipple down a few times.