How much pumped breastmilk should i feed my baby
Feeding expressed milk | introducing bottle
When can you start feeding your baby expressed breast milk? What’s the best way to do it? And should you be concerned about ‘nipple confusion’? We answer your questions about expressed milk feeding
Share this content
When should I start giving my baby expressed milk?
If your baby is healthy and breastfeeding is going well, there’s no need to rush into giving her expressed milk. For the first four weeks, you’re working together to initiate and build your breast milk supply while she learns to breastfeed efficiently. While there is limited data,1 it is thought that unnecessarily introducing bottles during this crucial first month could interfere with these processes.
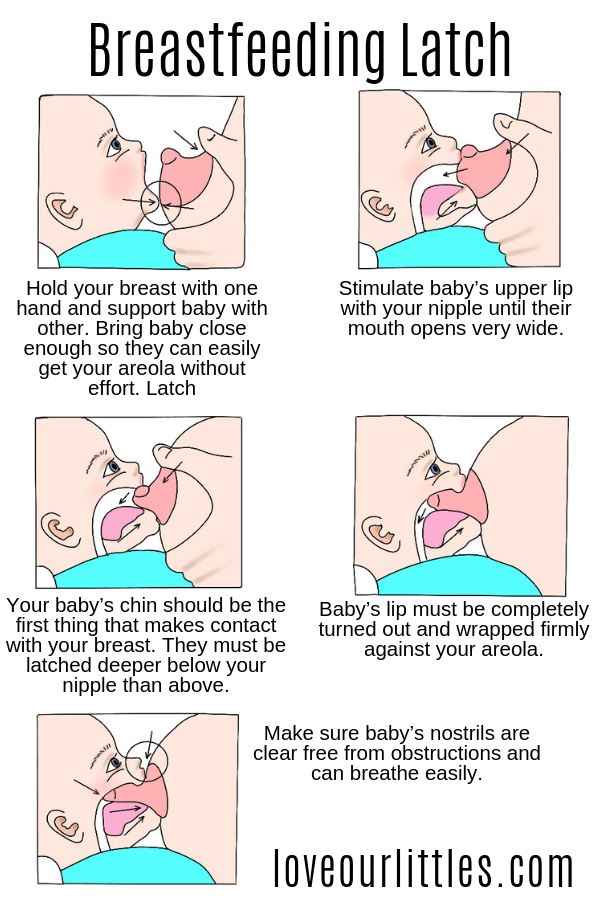
But if your newborn struggles to latch or suck for any reason, then start expressing milk as soon as possible after the birth. Read our articles on overcoming problems in the first week and feeding breast milk to your premature baby or infant with special needs for more advice, as well as getting support from your healthcare professionals.
How can I feed expressed milk to my baby?
There is a range of expertly designed feeding solutions that can help you give expressed milk to your baby, depending on your and her needs.
For example, Medela’s innovative Calma teat will only allow milk to flow when babies create a vacuum by sucking. This means they can feed from a bottle using the same technique, tongue motion and jaw movement they would at the breast.2,3 Developed with breastfeeding experts from the University of Western Australia, Calma allows your baby to suck, swallow, pause and breathe just as she does when breastfeeding.4 By maintaining babies’ natural sucking behaviour, Calma is designed to make it easy to switch from breast to bottle-feeding and back again.
Medela also makes conventional bottle teats in two flow versions. And all our teats can be attached directly to the bottles you express milk into, minimising the risk of spillages.
If your newborn needs expressed milk, but you don’t want to offer her a bottle until she’s become used to breastfeeding, you could use a baby cup designed for short-term feeding. This allows your baby to sip or lap your expressed milk – be careful to avoid spills! It’s advisable to have a healthcare professional on hand the first time you use the baby cup, to make sure you’re both getting the hang of it.
This allows your baby to sip or lap your expressed milk – be careful to avoid spills! It’s advisable to have a healthcare professional on hand the first time you use the baby cup, to make sure you’re both getting the hang of it.
For babies who need expressed milk supplements in addition to regular breastfeeding, a supplemental nursing system (SNS) can be helpful. This has a thin, flexible feeding tube that can be fixed alongside your nipple to give your baby expressed milk while you’re breastfeeding her. This allows your baby to stay at your breast longer, which further stimulates your breasts to help maintain your milk supply, and also helps improve her breastfeeding skills. It can be useful for mums with low milk supply or with adopted or surrogate babies.
If your baby can’t create the suction needed to breastfeed – perhaps because of a disability, congenital condition or weakness – you could try a feeder designed for babies with special needs. These allow infants who can’t suck to feed using gentle compression instead.
What’s the best way to introduce a bottle?
If breastfeeding is going well and you’ve decided it’s the right time to give your baby a bottle of expressed milk, follow these tips:
Take your time
Don’t wait until your big night out or first day back at work to introduce your baby to the bottle. Start trying with a small amount of expressed milk, in a relaxed and unhurried way, a couple of weeks beforehand. Gradually build up to giving a full feed of expressed breast milk from a bottle.
Pick your moment
Ideally your breastfed baby should be alert, but not too hungry, the first time she has a bottle of expressed milk, so that she is as relaxed as possible.
Delegate feeding duties
Your baby may be confused or frustrated when you offer a bottle, as she’s used to your breast. It might be easier if someone else gives the first bottle, and you stay out of the room so your baby can’t see or smell you.
Not too hot, not too cold
Your baby may be more likely to take the expressed milk if it’s around body temperature, 37 °C (98.6 °F).
Dip and sip
Try dipping the bottle teat into some expressed milk before offering it, so it tastes and smells of your breast milk. Then gently stimulate your baby’s top lip with the teat to encourage her to open her mouth.
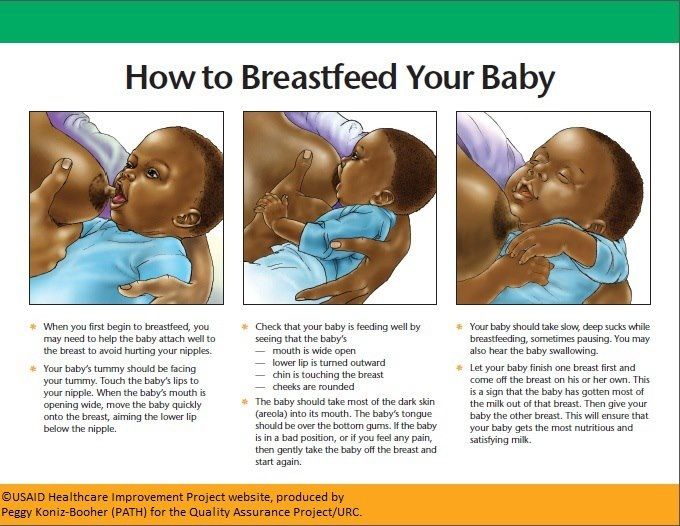
Positioning for bottle-feeding
Feed your baby on demand and cuddle her in a semi-upright position. Never bottle-feed her while she’s lying flat or prop her up with the bottle, in case of choking. Go at her pace, with as many pauses as she needs – you can even try switching sides during the feed.
Be patient
Don’t worry if she doesn’t take to the bottle straight away – it may take several tries. If she pushes the bottle away or becomes upset, comfort her and wait a few minutes before trying again. If she still won’t drink from the bottle, wait a few more minutes and then breastfeed her as normal. Try again with the bottle at a different time of day.
Try again with the bottle at a different time of day.
How much expressed milk should I give my baby?
Every baby is different. Research shows that in babies aged one to six months, one baby may take as little as 50 ml during a feed while another may take as much as 230 ml. Start by preparing a bottle with around 60 ml, and see if your baby needs more or less. You'll soon learn how much she typically takes – but don’t ever pressure her to finish the bottle.
How can I ensure bottle-feeding is safe for my baby?
Always clean and sanitise your breast pump set and bottles according to the instructions, and wash your hands before pumping, handling milk or feeding your baby. Follow our guidelines for storing and thawing your expressed milk safely.
If warming your breast milk, place the milk bottle or bag into a bowl of warm water or a warmer, or run it under a warm tap (max 37 °C or 98.6 °F). Never warm breast milk in the microwave or on the stove top.
Will my baby cope with switching from breast to bottle?
Mums sometimes worry that if they introduce a bottle too soon, their baby will get accustomed to the artificial teat and struggle to return to breastfeeding.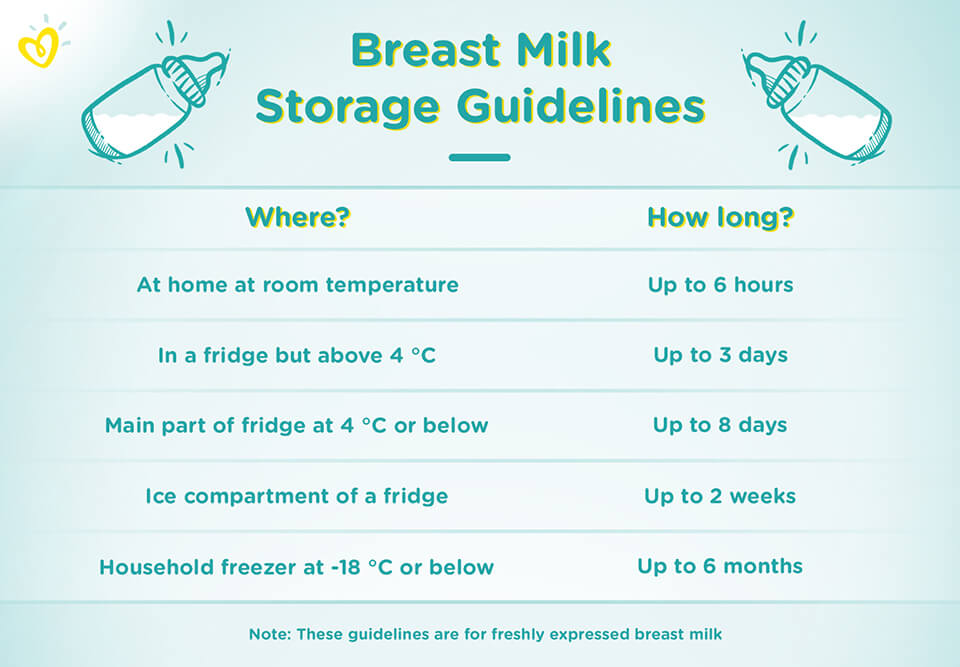 Others are concerned about the opposite problem – if they don’t get their baby used to a bottle early she may never accept one later. Both of these problems are commonly referred to as ‘nipple confusion’.
Others are concerned about the opposite problem – if they don’t get their baby used to a bottle early she may never accept one later. Both of these problems are commonly referred to as ‘nipple confusion’.
Experts disagree on whether nipple confusion is really an issue.1 Certainly sucking from a conventional bottle teat that doesn’t require a vacuum to be created is less effort for a baby than sucking from mum’s nipple, as the milk flows more freely and gravity lends a hand. And some babies do seem to have a preference for breast or bottle, and never take to the other. But many babies switch happily between the two.
If you’re still struggling to feed your baby expressed breast milk, speak to a lactation consultant or breastfeeding specialist.
References
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J Perinatol. 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only.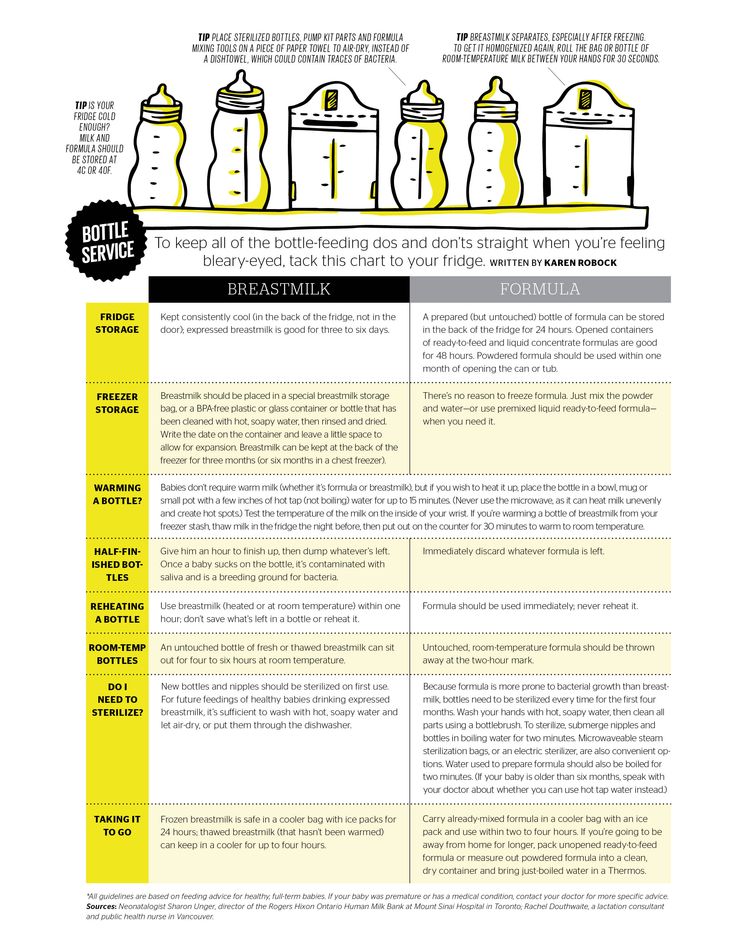 Early Hum Dev. 2012;88(6):443-449.
Early Hum Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J Perinatol. 2013;33(4):319-323.
4 Sakalidis VS et al. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. Int J Pediatr. 2012;2012:130769.
How Much Breast Milk Should a Newborn Eat?
In the early days at home with your newborn, getting into a regular feeding routine may be challenging - but learning how your baby's stomach grows over their first weeks outside the womb can help you both establish consistent nursing and feeding sessions.
Share this content
Learn How Your Baby's Stomach Grows Over Their First Days and Weeks
During the initial postpartum days with an at-term infant, getting into a regular feeding routine with your newborn may be challenging – it’s simply too early, and your baby will eat when he or she is hungry. Because their stomachs are so small, expect your little one to feed often but only drink a small volume of breast milk during these early nursing sessions. Each day, their stomach grows and the volume of breast milk it holds will quickly increase – this means that your baby will want and be able to drink larger volumes of milk as the days turn to weeks. This is a time of rapid growth for your newborn, so right now it’s usually best to follow their lead: Learn his or her cues and feed them as often as they indicate (at least 8 – 10 times per day through the first week), for as long as they want. Of course, this applies to babies who were born at term – late-term or early-term preemies may demonstrate different feeding cues and have special feeding situations.
Because their stomachs are so small, expect your little one to feed often but only drink a small volume of breast milk during these early nursing sessions. Each day, their stomach grows and the volume of breast milk it holds will quickly increase – this means that your baby will want and be able to drink larger volumes of milk as the days turn to weeks. This is a time of rapid growth for your newborn, so right now it’s usually best to follow their lead: Learn his or her cues and feed them as often as they indicate (at least 8 – 10 times per day through the first week), for as long as they want. Of course, this applies to babies who were born at term – late-term or early-term preemies may demonstrate different feeding cues and have special feeding situations.
Use our helpful guide to learn what the range of normal is when breastfeeding and consider the following to better understand your baby’s growing stomach size in the early days after birth:
How Many Ounces of Breast Milk Should a Newborn Drink?
- Day One ---> Your baby’s stomach is about the size of a cherry! This means that it holds just 1 – 1 ½ teaspoons of milk at a time.
- Day Three ---> Your baby’s stomach is about the size of a walnut! This means that it holds just ¾ - 1 ounce of milk at a time.
- One Week ---> Your baby’s stomach is about the size of an apricot! This means that it holds about 1 ½ - 2 ounces of milk at a time.
- Two Weeks ---> Your baby’s stomach is about the size of a large egg! This means that it holds about 2 ½ - 5 ounces of milk at a time.
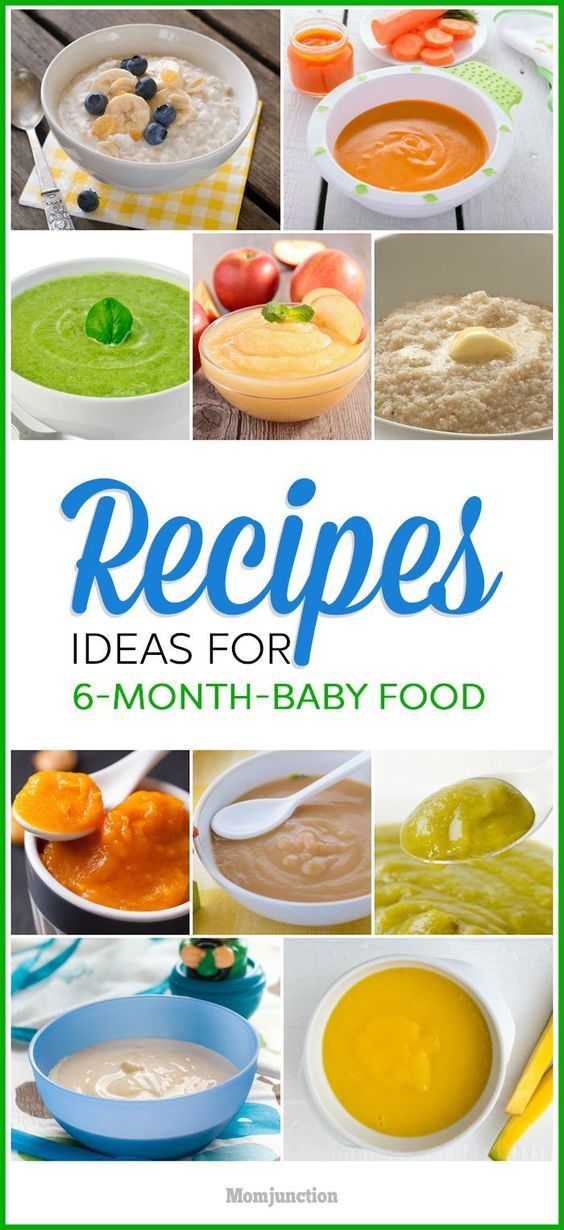
Between one month old and six months old, your baby will begin to eat more efficiently in fewer sessions throughout the day, but the total amount of milk that he or she drinks per day will not change significantly. Every baby is different and many will certainly have days when they are hungrier than others, but the amount of breast milk that your little one will take in during this time typically averages out to anywhere from 19 – 30 ounces per day. However, this can change if you begin supplementing or, later on, as you’re introducing solid foods.
Though it’s totally normal for newborns to lose some weight after birth, most babies are back to their original birth weights by about two weeks old and should have at least 6 wet diapers and 3 or more diapers with a bowel movement in a 24-hour period. If you have concerns about your baby and whether they are getting enough breast milk, talk to your healthcare provider and pediatrician right away. As long as you and your little one are doing well, and he or she is meeting the recommended weight, digestive, and health measures, you can rest assured that you’re doing just fine.
If you need a little help tracking how much milk your baby is drinking each day, download our Medela Family app to easily log your pumping, nursing, and feeding sessions and your little one’s diapers. You can also download our printable feeding and pumping log - available in English and Spanish - to stay as organized as possible during those early weeks at home with your baby.
Your breast milk provides so many benefits to your newborn, mama. The vitamins, minerals, healthy fats, and other great nutrients are exactly what they need right now. Remember, you and your baby will establish a regular daily feeding pattern soon enough, so be patient with yourself during this early postpartum period and know that you are rocking this new mom life – You’re doing a great job!
The vitamins, minerals, healthy fats, and other great nutrients are exactly what they need right now. Remember, you and your baby will establish a regular daily feeding pattern soon enough, so be patient with yourself during this early postpartum period and know that you are rocking this new mom life – You’re doing a great job!
Feeding with expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast. There is not enough scientific data on this yet, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding.
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after delivery. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How can I feed my baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs.
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2.3 Calma was developed with the help of breastfeeding experts from the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding.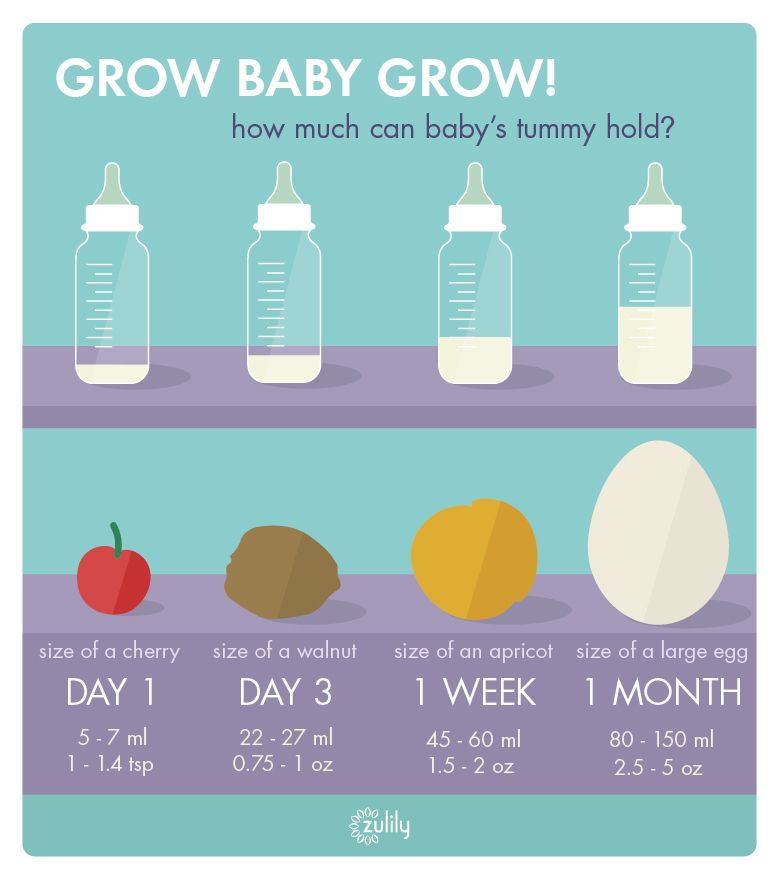 4 Preserving natural sucking habits allows baby to transition easily from breast to bottle and back.
4 Preserving natural sucking habits allows baby to transition easily from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible.
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature.
Dip the nipple in milk
Try dipping the nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much pumped milk should I give my baby?
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.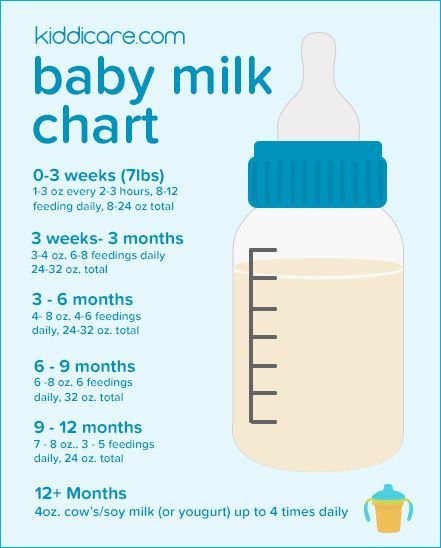
How can I keep my baby safe when bottle feeding?
Always clean and sterilize your pump and bottles according to the manufacturer's instructions. Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, the baby will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it. In general, in these cases, they say that the child confuses the nipple with the breast.
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist.
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." Zh Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Hum Dev . 2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J. Perinatol. 2013;33(4):319-323. - Segami, I. et al., "Perioral movements and sucking during bottle feeding with a new experimental nipple are very similar to sucking from the breast." Zh Perinatol (Journal of Perinatology). 2013;33(4):319-323.
4 Sakalidis VS et al. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. Int J Pediatr. 2012;2012:130769. - Sakalidis V.S. et al., "Oxygenation and Coordination of Sucking, Swallowing, and Breathing in the Term Infant During Breastfeeding and Feeding from a Purely Vacuum Teat".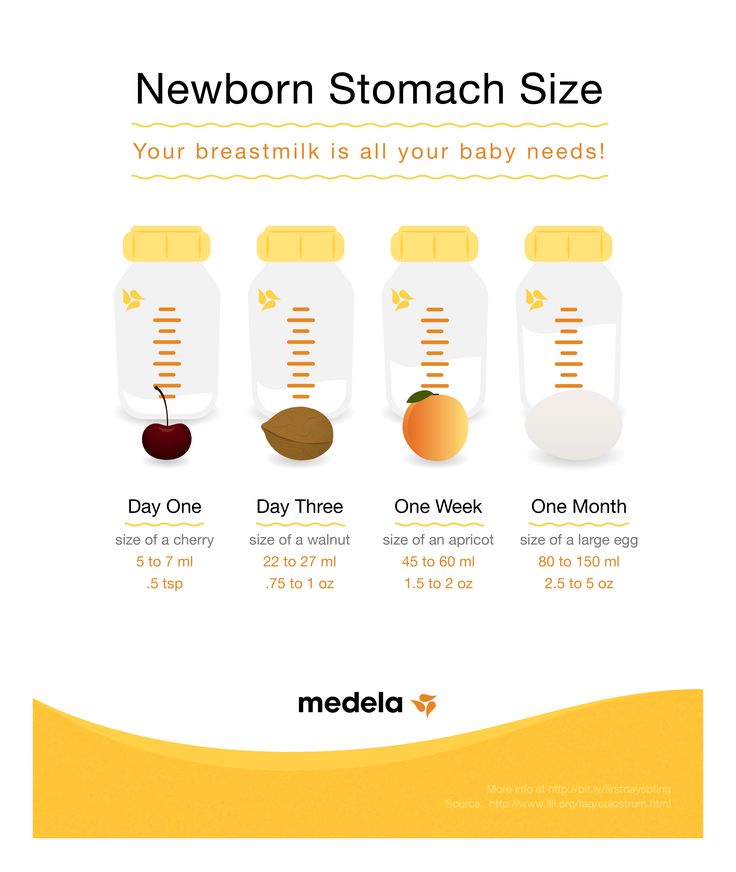 Int J Pediatrician 2012;2012:130769.
Int J Pediatrician 2012;2012:130769.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № ФСЗ 2010/07353 dated 07/19/2010
Expression of breast milk | Medela
Eglash, A. ABM clinical protocol #8: Human milk storage information for home use for full-term infants (original protocol March 2004; revision #1 March 2010). Breastfeed Med 5, 127–130 (2010). - Eglash A., Simon L., AVM Clinical Protocol #8: Home Storage of Milk for Term Infants (original protocol March 2004, first revised March 2010) Brestfeed Med ( breastfeeding medicine) 5 , 127-130 (2010)
Eteng, M.U., Ebong, P.E., Eyong, E.U. et al. Storage beyond three hours at ambient temperature alters the biochemical and nutritional qualities of breastmilk. Afr J Reprod Health 2001;5:130–134. - Eteng M.W., Ebong P.I., Eyong I.W. et al., "Storage at room temperature for more than three hours affects the biochemical and nutritional properties of breast milk." Afr J Reprod Health 2001;5:130–134.
- Eteng M.W., Ebong P.I., Eyong I.W. et al., "Storage at room temperature for more than three hours affects the biochemical and nutritional properties of breast milk." Afr J Reprod Health 2001;5:130–134.
Hill, P.D., Aldag, J.C., Chatterton, R.T. Initiation and frequency of pumping and milk production in mothers of non-nursing preterm infants. J Hum Lact . 2001;17(1):9–13 - Hill P.D., Aldag J.S. and Chatterton, R.T., "Onset and frequency of expression and milk production in mothers who have given birth to premature babies and have not breastfed them." J Hum Lakt (Journal of the International Association of Lactation Consultants) 2001;17(1):9-13.
Hill, P.D., Aldag, J.C., Chatterton, R.T., Zinaman, M. Comparison of Milk Output Between Mothers of Preterm and Term Infants: The First 6 Weeks After Birth. J Hum Lact . 2005 February 1, 2005; 21(1):22–30. - Hill P.D., Aldag J.S., Chatterton R.T., Zinaman M., "Comparison of the amount of milk in mothers of full-term and premature babies in the first 6 weeks after birth." J Hum Lakt (Journal of the International Lactation Consultants Association) February 1, 2005, 21(1): 22-30.
- Hill P.D., Aldag J.S., Chatterton R.T., Zinaman M., "Comparison of the amount of milk in mothers of full-term and premature babies in the first 6 weeks after birth." J Hum Lakt (Journal of the International Lactation Consultants Association) February 1, 2005, 21(1): 22-30.
Human Milk Banking Association of North America 2011 Best practice for expressing , storing and handling human milk in hospitals , homes , and child care settings ( HMBANA , Fort Worth , (2011). - North American Association of Breast Milk Banks. Fort Worth: SABGM; 2011.)
Kent, J.C. et al. Importance of vacuum for breastmilk expression. Breastfeed Med 3, 11-19 (2008). - Kent J.S. et al., "The Importance of Vacuum in Expression of Breast Milk". Brestfeed Med 3 (Breastfeeding Medicine). 3.11-19 (2008).
Meier, P.P., Engstrom, J.L., Janes, J.E., Jegier, B.J. & Loera, F. Breast pump suction patterns that mimic the human infant during breastfeeding: Greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol 32, 103-110 (2012). - Meyer P.P., Engstrom J.L., Jaynes J.I., Jaegier B.J., Loera F. "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constant pumping mothers of premature babies". Zh Perinatol (Journal of Perinatology) 32, 103-110 (2012).
Morton, J.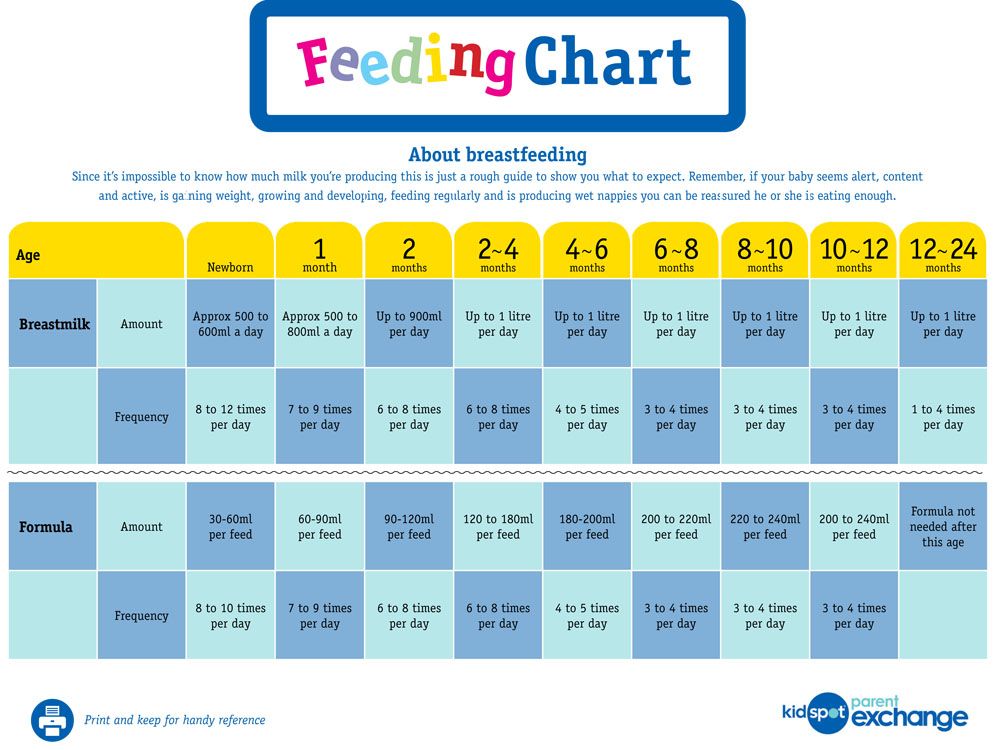 , Hall, J.Y., Wong, R.J., Benitz, W.E. & Rhine, W.D. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J Perinatol 29, 757–764 (2009). — Morton J., Hall J.I., Wong R.J., Benitz W.I. and Rhine, W.D., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants." J Perinatol (Journal of Perinatology) 29, 757-764 (2009)
, Hall, J.Y., Wong, R.J., Benitz, W.E. & Rhine, W.D. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J Perinatol 29, 757–764 (2009). — Morton J., Hall J.I., Wong R.J., Benitz W.I. and Rhine, W.D., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants." J Perinatol (Journal of Perinatology) 29, 757-764 (2009)
Parker, L.A., Sullivan, S., Krueger, C. & Mueller, M. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med (2015). - Parker L.A., Sullivan S., Kruger S., Kelechi T. and Muller M., "Association of the time of onset of expression with the amount of milk and the timing of the second stage of lactogenesis in mothers of children who had extremely low birth weight" .