How to feed baby mother milk
Hints to Help You Get Off to a Good Start
Breastfeeding has many benefits for your baby. Breast milk is rich in nutrients. It has antibodies, which help protect your baby against infections. It also can help prevent sudden infant death syndrome (SIDS). Babies who are breastfed are less likely to have allergies, asthma, and diabetes. They also are less likely to become overweight.
Breastfeeding has benefits for you as well. It’s cheaper than using formula. You don’t have to wash bottles or mix formula. It helps your uterus go back to normal size after stretching out during pregnancy. This can help you lose weight faster. It can delay the return of your periods. However, you shouldn’t count on it to prevent pregnancy. Breastfeeding helps make time for you to be close to your baby. Women who breastfeed have lower risks of type 2 diabetes, breast cancer, ovarian cancer, high blood pressure, and heart disease.
Path to improved health
Breastfeeding promotes wellbeing for you and your baby. Although it is a natural part of the birthing process, it’s not always easy. Many women need help learning how to breastfeed. The American Academy of Family Physicians (AAFP) recommends that all doctors provide assistance to women during pregnancy and after birth to support breastfeeding. Your doctor may recommend breastfeeding for at least the first 6 months of your baby’s life.
Below are helpful tips to help you get off to a good start.
Before you give birthDuring pregnancy, the following things can prepare you for breastfeeding.
- Prenatal care. It’s important to take good care of yourself and your baby. Babies who are born early (premature) have a harder time breastfeeding.
- Talk to your doctor. Make sure your doctor knows your plan to breastfeed. They can give you some resources. Ask questions about what type of care the hospital provides after birth. Some offer lactation consultants, who are breastfeeding specialists.

- Breastfeeding class. Some women find that taking a class can help them practice for the real thing.
- Breastfeeding items. Plan ahead by purchasing the items you need. These can include a nursing pillow, nursing bra, and covers. Some hospitals and insurance plans provide free breast pumps.
Once your baby is born, your breasts will start to fill up. At first, your body will produce a “pre-milk,” called colostrum. This can be thin and watery or thick and more yellow-colored. The pre-milk has a slower flow to help your baby learn to nurse. A newborn’s stomach is only about the size of a large grape. After 3 to 4 days of nursing, your real breast milk will come in.
Most babies are ready to eat 1 to 2 hours after birth. Below is a step-by-step guide on how to breastfeed.
- Wash your hands before each feeding.
- Place your baby in one of the breastfeeding positions (outline below).

- Put the thumb of your free hand on top of your breast and your other fingers below.
- Touch your baby’s lips to your nipple until your baby opens their mouth wide.
- Put your nipple all the way in your baby’s mouth and pull your baby close to you. This lets your baby’s jaw squeeze the milk ducts under your areola (nipple).
How do I know if my baby is latched on?
When your baby is “latched on” the right way, both lips should cover nearly all of your areola. Your baby’s jaw should begin to move back and forth. Your baby may make low-pitched swallowing noises instead of smacking noises. If you feel pain while your baby is nursing, they may not be latched on.
Your baby’s nose may touch your breast during nursing. Babies’ noses are designed to allow air to get in and out. If you’re concerned your baby can’t breathe easily, gently press down on your breast near your baby’s nose to give them more room to breathe. Your baby shouldn’t have to turn their head or strain their neck to nurse.
You can hold your baby in a number of ways. Some of the most common positions are:
- Put your baby’s head in the crook of your arm. Support your baby’s back and bottom with your forearm. Your baby should be lying facing you. Your breast should be right in front of your baby’s face.
- Side-lying. While lying down, place your baby alongside you. Your baby should be facing you. Pull your baby close to you so they can latch on. You can use a pillow to prop up, if needed. This position is helpful if you had a cesarean section (C-section). You don’t want to fall asleep while nursing in this (or any other) position. Co-sleeping can be dangerous for your baby. It increases the risk of sudden infant death syndrome (SIDS).
- Tuck your baby under your arm, along your side. Their head should be resting in your hand. Support your baby’s body with your forearm. Your baby should be facing you.
 This position is helpful if you had a C-section. It also can help if your breasts are large, your baby is small, or you have multiple babies.
This position is helpful if you had a C-section. It also can help if your breasts are large, your baby is small, or you have multiple babies. - Cross-cradle. Hold your baby with the opposite arm of the breast you’re using. Support your baby’s head and bottom with the palm of your hand and forearm. Your baby should still be lying facing you. This position can help premature babies or babies who have a weak suck. It provides added head support.
The let-down reflex means your milk is ready to flow. It makes breastfeeding easier for you and your baby. You may feel a tingle in your breast(s) as you start to breastfeed. Milk may drip from the breast not being used. These are signs that your milk has “let-down.” The let-down reflex also may occur if a feeding is overdue, if you hear a baby cry, or if you think about your baby.
The reflex can be forceful enough to cause your baby to cough. If this is a problem, try to discharge some of your milk by hand before a feeding.
Feed your baby as often as they want to be fed. Learn how to tell when your baby is hungry. Crying can be a sign of hunger, but it may be too late. Babies who are crying or are upset have a harder time latching on. Watch out for early signs of hunger. Your baby may:
- Make sucking motions
- Turn toward the breast if they are being held
- Put their hands in their mouth
- Become excited or alert
After birth, your baby may be hungry 8 to 12 times a day or more. This number may decrease over time or increase during a growth spurt. Growth spurts occur at about 2 weeks and 6 weeks of age and again at about 3 months and 6 months of age.
Let your baby eat until they are satisfied. This may be for about 15 to 20 minutes at each breast. Try to have your baby nurse from both breasts at each feeding. Make sure your baby finishes one breast before starting the other. Your baby should let go on their own once they are done.
Don’t limit the time you let your baby nurse. It may keep your milk ducts from completely emptying. This can decrease your milk flow and make it harder for your baby to latch it on. It also can cause swelling and pain. Applying a cold compress before nursing can ease discomfort.
How do I know if my baby is getting enough milk?Your baby is getting enough milk if they:
- Act satisfied after each feeding
- Gain weight consistently after the first 3 to 7 days after birth. (Your baby may lose a little weight during the first week after being born.)
- Have about 6 to 8 wet diapers a day
- Have about 2 to 5 or more stools a day at first. This number may decrease to about 2 stools or less a day
Sometimes babies fall asleep while nursing. You can squeeze your breast to make more milk flow. This may awaken your baby. If you are not sure they got enough milk, offer your other breast to see if your baby latches on again.
If you think your baby needs more milk, increase the number of feedings a day. It’s important for you to get plenty of rest and eat right. Give your body time to catch up to your baby’s demands.
Don’t replace breast milk with baby formula or cereal. This can make babies lose interest in breast milk. It also will decrease your milk supply. You shouldn’t give your baby solid foods until about 6 months of age.
What if I work?There is no reason you have to stop breastfeeding when you return to work. Make a plan for pumping your breast milk at work. The federal Break Time for Nursing Mothers law requires your employer to provide basic accommodations for breastfeeding mothers at work, according to the U.S. Department of Health and Human Services (HHS). “These accommodations include time for women to express milk and a private space that is not a bathroom each time they need to pump,” reports the HHS.
Breastfeed your baby before you leave for work, and every 3-4 hours at work (or however often you would normally feed your baby). Keep the milk refrigerated and your baby can have it the next day while you are at work. It keeps for up to 4 days in the refrigerator. If you aren’t going to use the milk within 4 days, freeze it. Breastmilk will last up to 6-12 month in the freezer. After work, breastfeed your baby as you normally would.
Things to consider
What food should I eat while breastfeeding?The best diet is well balanced and has plenty of calcium. A balanced diet includes eating from all 5 food groups. You should get 5 servings of milk or dairy products each day. It is okay to eat foods that were restricted while you were pregnant. These will not make your baby sick.
If you don’t eat meat or dairy, you can get calcium from foods such as broccoli, sesame seeds, tofu, and kale. Talk to your doctor about taking a calcium supplement if you don’t get enough from your diet.
You should eat about 500 extra calories per day. Make sure you drink extra fluids as well. Continue to take a prenatal vitamin so your body gets enough nutrients.
What should I avoid while breastfeeding?Certain foods can bother your baby. They may make him or her fussy or gassy. Pay attention to what you eat and how your baby acts after feedings. Stop eating foods that affect them. These may include spicy foods, broccoli, or milk.
Some babies react to cow’s milk in your diet. Symptoms can include gas, vomiting, diarrhea, rash, or colic. Your baby also can have an allergic reaction to something you eat. Common foods are eggs and peanuts. They may get a rash or have trouble breathing. Contact your doctor right away if your baby has any of these signs.
Limit your intake of caffeine and alcohol. These can get into your milk. Don’t have more than a couple cups of coffee, tea, soda, or other caffeine each day. Don’t have more than one alcoholic drink each day. Avoid drinking caffeine and alcohol less than 2 hours before a feeding.
Avoid drinking caffeine and alcohol less than 2 hours before a feeding.
Some medicines can get into your milk. This includes over-the-counter drugs and prescriptions, such as antidepressants and birth control medicines. Don’t take anything without talking to your doctor first. Smoking also is bad for breastfeeding. The chemicals and smoke can get in your milk. Smoking can cause you to make less milk. If you smoke, try to quit.
If possible, avoid using bottles or pacifiers after birth. This can confuse your baby and make breastfeeding harder.
What can I do if my nipples get sore?It’s easier to prevent sore nipples than it is to treat them. The main cause of sore nipples is when your baby doesn’t latch on the right way. You need to start over to correct this. To take your baby off your breast, release the suction by putting your finger in the corner of your baby’s mouth between the gums. Switch breasts and try to breastfeed again.
Other ways to prevent and heal sore nipples are:
- Make sure your baby is sucking the right way.
 If the sucking hurts, your baby’s mouth may not be in the right position.
If the sucking hurts, your baby’s mouth may not be in the right position. - Offer your baby the less sore of your two nipples first. Your baby’s sucking may be less forceful after the first few minutes.
- If possible, position cracked or tender parts of your breast at the corner of your baby’s mouth. This way the spots get less pressure during feeding.
- Change positions.
- Let your nipples air dry between feedings. Let the milk dry on your nipples instead of wiping it off.
- Wash your nipples daily with warm water. Don’t use soap or lotion that may contain alcohol. This can dry out your skin.
- Rub lanolin on your nipples to help soothe them.
- Avoid bra pads lined with plastic. Change bra pads between feedings to keep your nipples dry.
- Discharge milk with your hand until the let-down reflex occurs. This can help make your milk flow easier so your baby sucks less hard.
When to see your doctor
Call your doctor if you have:
- A red, sore, or painful spot on your breast
- Painful engorgement (overfull breasts)
- A fever or if you feel achy (these may be signs of an infection)
You also should call your doctor if your baby is losing weight for no apparent reason.
Questions to ask your doctor
- Where can I take a breastfeeding class?
- What type of breastfeeding care and information will the hospital provide after birth?
- What should I do if my baby won’t latch on?
- What can I do if my body is not producing enough milk?
- Is it okay to give my baby bottles or pacifiers?
Resources
National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development: Breastfeeding and Breast Milk
National Institutes of Health, MedlinePlus: Breastfeeding
U.S. Department of Health & Human Services, Office on Women’s Health: Learning to Breastfeed
Frequently Asked Questions (FAQs) | Breastfeeding
What are the benefits of breastfeeding?
Breastfeeding is good for both infants and mothers. Breast milk is the best source of nutrition for most infants. As an infant grows, breast milk changes to meet the infant’s nutritional needs. Breastfeeding can also help protect the infant and mother against certain illnesses and diseases:
Breastfeeding can also help protect the infant and mother against certain illnesses and diseases:
Benefits to Infants
Infants who are breastfed have a lower risk of:
- Asthma.
- Obesity.
- Type 1 diabetes.
- Severe lower respiratory disease.
- Acute otitis media (ear infections).
- Sudden infant death syndrome (SIDS).
- Gastrointestinal infections (diarrhea/vomiting).
- Necrotizing enterocolitis (NEC) for preterm infants.
Benefit to Mothers
Mothers who breastfeed their infants have a lower risk of:
- Breast cancer.
- Ovarian cancer.
- Type 2 diabetes.
- High blood pressure.
Families can visit CDC’s Infant and Toddler Nutrition website to learn more about what to expect while breastfeeding.
When should a mother avoid breastfeeding (contraindications)?
Breast milk provides the best nutrition for most infants, including premature and sick newborns. However, there are rare exceptions when breast milk or breastfeeding is not recommended. Learn more about contraindications to breastfeeding.
However, there are rare exceptions when breast milk or breastfeeding is not recommended. Learn more about contraindications to breastfeeding.
Only a few medications are contraindicated (not recommended) while breastfeeding. Although many medications do pass into breast milk, most have little or no effect on milk supply or on an infant’s well-being. However, health care providers should always weigh the risks and benefits when prescribing medications to breastfeeding mothers.
Learn more about safe prescription medication use while breastfeeding.
Top of Page
How is growth assessed for breastfed infants?
In the United States, the World Health Organization (WHO) Growth Standard Charts are recommended for use with both breastfed and formula-fed infants and children, from birth to 2 years of age, to monitor growth. The WHO growth charts reflect growth patterns among children who were predominantly breastfed for at least 4 months and were still breastfeeding at 12 months. The WHO growth charts establish the growth of the breastfed infant as the norm for growth and are the standards for how children should grow when provided optimal conditions. Clinicians should be aware that healthy breastfed infants typically gain weight faster than formula-fed infants in the first few months of life but then gain weight more slowly for the remainder of infancy, even after complementary foods are introduced.
The WHO growth charts establish the growth of the breastfed infant as the norm for growth and are the standards for how children should grow when provided optimal conditions. Clinicians should be aware that healthy breastfed infants typically gain weight faster than formula-fed infants in the first few months of life but then gain weight more slowly for the remainder of infancy, even after complementary foods are introduced.
For children older than 2 years (2 to 19 years of age) CDC and the American Academy of Pediatrics recommend that health care providers use the CDC Growth Reference Charts.
Visit the Growth Chart Training website for a set of self-directed, interactive training courses.
Source: Grummer-Strawn LM, Reinold C, Krebs NF. Use of the World Health Organization and CDC growth charts for children aged 0 to 59 months in the United States. MMWR Recomm Rep. 2010;59(RR-9):1–15.
Top of Page
How long should a mother breastfeed?
The U. S. Dietary Guidelines for Americans [PDF-30.6MB] recommend that infants be exclusively breastfed for about the first 6 months, and then continuing breastfeeding while introducing appropriate complementary foods until your child is 12 months old or older. The American Academy of Pediatrics and the World Health Organization also recommend exclusive breastfeeding for about the first 6 months, with continued breastfeeding along with introducing appropriate complementary foods for up to 2 years of age or longer.
S. Dietary Guidelines for Americans [PDF-30.6MB] recommend that infants be exclusively breastfed for about the first 6 months, and then continuing breastfeeding while introducing appropriate complementary foods until your child is 12 months old or older. The American Academy of Pediatrics and the World Health Organization also recommend exclusive breastfeeding for about the first 6 months, with continued breastfeeding along with introducing appropriate complementary foods for up to 2 years of age or longer.
Mothers should be encouraged to breastfeed their children for at least 1 year. The longer an infant is breastfed, the greater the protection from certain illnesses and long-term diseases. The more months or years a woman breastfeeds (combined breastfeeding of all her children), the greater the benefits to her health as well.
The American Academy of Pediatrics recommends that children be introduced to foods other than breast milk or infant formula when they are about 6 months old. To learn more about infant and toddler feeding, visit CDC’s Infant and Toddler Nutrition website.
To learn more about infant and toddler feeding, visit CDC’s Infant and Toddler Nutrition website.
Top of Page
What can happen if someone else’s breast milk is given to another child?
Very few illnesses are transmitted via breast milk. Learn more about what to do if an infant or child is mistakenly fed another woman’s expressed breast milk.
Top of Page
Are special precautions needed for handling breast milk?
CDC does not list human breast milk as a body fluid to which universal precautions apply. Occupational exposure to human breast milk has not been shown to lead to transmission of HIV or Hepatitis B infection. However, because human breast milk has been implicated in transmitting HIV from mother to infant, gloves may be worn as a precaution by health care workers who are frequently exposed to breast milk (e.g., people working in human milk banks (defined below). For additional information regarding universal precautions as they apply to breast milk in the transmission of HIV and Hepatitis B infections, visit the following resources:
Centers for Disease Control and Prevention. Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988;37(24):377–388.
Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988;37(24):377–388.
Top of Page
Where can mothers find more information about preparation and storage of breast milk?
CDC has guidelines for proper storage and preparation of breast milk to maintain the safety and quality of expressed breast milk for the health of the baby.
For more information about specific storage and preparation of breast milk questions, such as where to store breast milk at work, and what to do when the power goes out, visit CDC’s Storage and Preparation of Breast Milk Frequently Asked Questions.
Top of Page
What are human milk banks?
Human milk banks are a service established for the purpose of collecting milk from donors and processing, screening, storing, and distributing donated milk to meet the specific needs of individuals for whom human milk is prescribed by licensed health care providers. When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
Milk banks accept donations directly at their deposit sites or they can arrange for safe, overnight transportation of human milk at no cost to the donor. Learn more about donating to a milk bank by visiting the Human Milk Banking Association of North America (HMBANA).
Top of Page
Is it safe for families to buy breast milk on the internet?
The American Academy of Pediatrics and the Food and Drug Administration recommend avoiding Internet-based milk sharing sites and instead recommend contacting milk banks. Research has demonstrated that some milk samples sold online have been contaminated with a range of bacteria.1
Nonprofit donor human milk banks, where processed human milk comes from screened donors, have a long safety record in North America. All member banks of the Human Milk Banking Association of North America (HMBANA) must operate under specific evidence-based guidelines that require extensive testing and processing procedures as well as self-reported health information and a health statement from both the donor’s health care provider and the infant’s health care provider. Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA.
Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA.
1Keim, SA, Hogan, JS, McNamara, KA, et al. Microbial contamination of human milk purchased via the internet. Pediatrics. 2013;132(5).
Top of Page
What legal rights do breastfeeding mothers have?
Breastfeeding Laws
- All 50 states, the District of Columbia, Puerto Rico and the Virgin Islands have laws that specifically allow women to breastfeed in any public or private location. Visit the National Conference of State Legislatures to learn more about federal and state laws that protect and support breastfeeding.
Workplace Laws
- The “Break Time for Nursing Mothers Provision” of the Patient Protection and Affordable Care Act (ACA) requires employers to support breastfeeding mothers to express breast milk for 1 year after each child’s birth by providing mothers with reasonable break time and a private, non-bathroom space to express their breast milk.
 Visit the United States Department of Labor to learn more.
Visit the United States Department of Labor to learn more.
Travel Laws
- Air travelers are permitted by the Transportation Security Administration (TSA) to bring breast milk, formula, and juice in excess of 3.4 ounces in their carry-on baggage and it does not need to fit within a quart size bag. Ice packs, freezer packs, and other accessories needed to keep the liquid cool are also allowed in carry-on bags. All liquids and partially frozen accessories are subject to being screened by X-ray. TSA is required by the Bottles and Breastfeeding Equipment Screening Act (BABES act) to provide ongoing training to ensure TSA staff receive consistent training related to traveling with breast milk, formula, and infant feeding equipment. Visit the TSA to learn more about traveling with breast milk, formula, and juice. For tips on travel and breastfeeding, visit Travel Recommendations for the Nursing Mother.
Visit the Federal Policies, Programs, & Initiatives website to learn more about laws related to breastfeeding protections.
Top of Page
How can a mother continue to provide breast milk to her infant after returning to work or school?
Being prepared for returning to work or school can help a mother ease the transition and continue to breastfeed after her maternity leave is over. The Office on Women’s Health has information for making this transition easier.
When a mother is away from her infant, she can pump or hand express her breast milk so that her infant can drink breast milk from a bottle. Mothers can visit CDC’s Infant and Toddler Nutrition website to learn more about pumping breast milk.
Mothers who are expressing their breast milk should visit the CDC’s Proper Storage and Preparation of Breast Milk website to learn how to prepare and store breast milk safely for her infant.
The Patient Protection and Affordable Care Act (ACA) requires employers to support breastfeeding mothers to express breast milk for 1 year after each child’s birth by providing mothers with reasonable break time and a private, non-bathroom space to express their breast milk.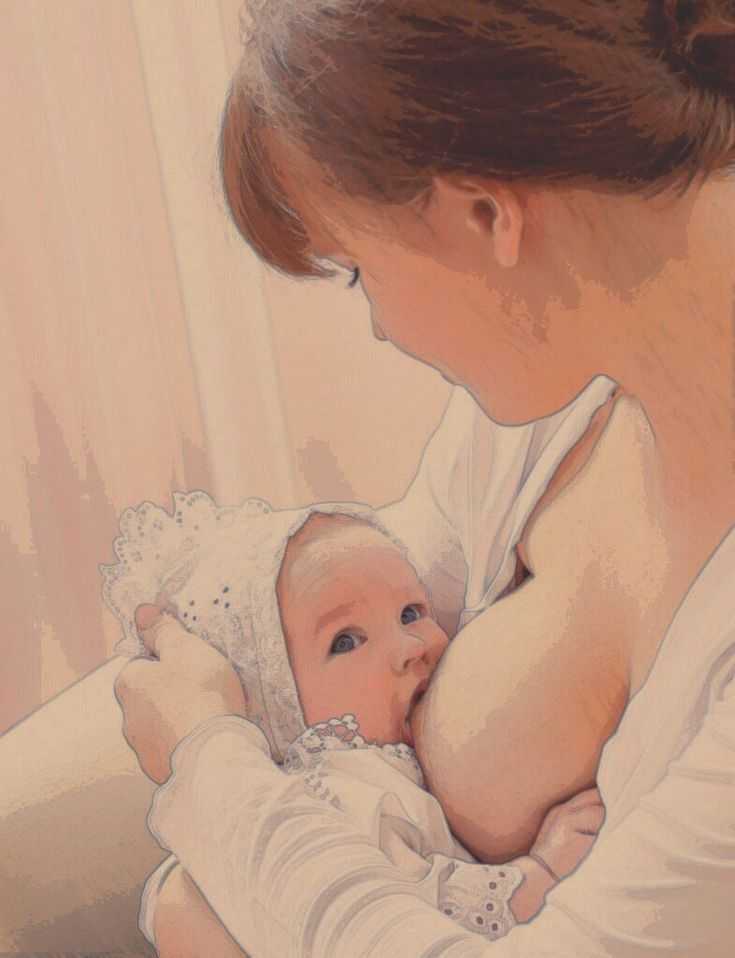 For more information about the types of employees and employers to which the requirements apply, refer to the United States Department of Labor’s Frequently Asked Questions.
For more information about the types of employees and employers to which the requirements apply, refer to the United States Department of Labor’s Frequently Asked Questions.
Top of Page
Where can mothers find breastfeeding support and additional Information about breastfeeding?
Help mothers find lactation support through the following resources:
- International Lactation Consultant Association (IBCLCs)
- United States Lactation Consultant Association (IBCLCs)
- Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics
- La Leche League
Help mothers find resources about breastfeeding by directing them to the following websites:
- CDC— Infant and Toddler Nutrition
- Office on Women’s Health—Breastfeeding
- American Academy of Pediatrics—Healthy Children
- United States Breastfeeding Committee—State Coalitions Directory
- US Department of Agriculture—WIC Breastfeeding Support
Top of Page
Does breastfeeding during a child’s vaccine injections help with pain management?
Parents who are breastfeeding should be encouraged to breastfeed children age 2 years or younger before, during, and after their child’s vaccination. Several aspects of breastfeeding are thought to decrease pain by multiple mechanisms: being held by the parent, feeling skin-to-skin contact, suckling, being distracted, and ingesting breast milk. Potential adverse events such as gagging or spitting up have not been reported. Alternatives to breastfeeding include bottle-feeding with expressed breast milk or formula throughout the child’s procedure, which simulates aspects of breastfeeding.
Several aspects of breastfeeding are thought to decrease pain by multiple mechanisms: being held by the parent, feeling skin-to-skin contact, suckling, being distracted, and ingesting breast milk. Potential adverse events such as gagging or spitting up have not been reported. Alternatives to breastfeeding include bottle-feeding with expressed breast milk or formula throughout the child’s procedure, which simulates aspects of breastfeeding.
Top of Page
Does breastfeeding after a child’s rotavirus vaccine impact the vaccine’s efficacy?
There is not sufficient evidence to suggest that breastfeeding can have a negative effect on rotavirus vaccine efficacy. A previous study found that human milk from women who live in areas with endemic rotavirus contains antibodies that can neutralize live rotavirus vaccine virus. However, in licensing trials, the effectiveness of rotavirus vaccine in breastfed infants was comparable to that in non-breastfed infants.
CDC does not recommend restricting or discontinuing breastfeeding before or after a child receives the rotavirus vaccine. Breastfed infants should be vaccinated according to the same schedule as non-breastfed infants.
Breastfed infants should be vaccinated according to the same schedule as non-breastfed infants.
Learn More about prevention of Rotavirus Gastroenteritis among infants and children.
Top of Page
Breastfeeding your baby with special needs
If your baby has special needs and has difficulty latch-on, there are many other ways to breastfeed
Share this information
Breastfeeding is a serious stress for a baby. This process involves 40 muscles in the lips, tongue, jaw and cheeks, as well as six cranial nerves 1 for coordinating sucking, swallowing and breathing.
If a baby has a congenital disorder or disease that affects these muscles or nerves, the baby may not be physically fit to breastfeed or may not be able to get enough milk while nursing. But this does not mean that your baby should be deprived of extremely healthy breast milk. Moreover, the protective properties of milk and useful substances in its composition are even more necessary for children with special needs.
“Breast milk contains many living cells and growth factors that help boost immunity and prevent inflammation,” explains Dr. Katsumi Mitsuno, Professor of Internal Medicine in Pediatrics, Koto Toyosu Hospital at Showa University, “It is important for infants with special needs to give breast milk to prevent infectious diseases and ensure optimal nutrition.”
“Children with congenital and neurological pathologies are more susceptible to respiratory 2.3 and ear 4 infections and diseases of the gastrointestinal tract 5 , and are also more likely to require surgical intervention. Breast milk helps to protect the baby's body from infections and promotes recovery 6 ,” adds Dr. Mitsuno.
Reasons your baby may have difficulty breastfeeding
Cleft lip and/or palate
breastfeeding or supervising physician can show several helpful tricks. Newborns with cleft palate are often unable to breastfeed with sufficient force. 7
7
Prematurity
If the baby was born prematurely, he may be too weak and not have enough coordination to suckle effectively. Read more about this in the article on breastfeeding premature babies.
Down's syndrome and other chromosomal disorders
Babies with Down's syndrome typically have problems with muscle tone and mouth-tongue coordination that prevents effective breastfeeding. 8 Other chromosomal disorders, such as Edwards syndrome or Patau syndrome, also make breastfeeding difficult.
Neurological disorders
Neurological disorders (disorders of the brain, spine or nerves) often cause hypotonia, the medical term for low muscle tone. Cerebral palsy, 9 hydrocephalus, birth asphyxia, spina bifida, cerebral hemorrhage during childbirth, cerebral malformations and hypoxic-ischemic encephalopathy can cause difficulties in breastfeeding.
Pierre Robin's syndrome
With Pierre Robin's syndrome, the baby's lower jaw is much smaller than normal. Often this is combined with a cleft palate and tongue retraction, making breastfeeding almost impossible. 10
Often this is combined with a cleft palate and tongue retraction, making breastfeeding almost impossible. 10
Maxillofacial surgery
If your baby has had oral, tongue or jaw surgery, it may be painful or uncomfortable to suckle for a while.
Expressing milk for children with special needs
Regardless of whether the baby can breastfeed, the first step is to start milk production in order to get enough milk. If the baby is unable to feed directly from the breast, it is important to ensure frequent pumping to collect as much milk as possible. It is necessary to start and stimulate the production of milk as early as possible so that the baby has enough of it now and in the future.
Double pumping is recommended about eight times a day as this is the best way to stimulate a steady supply of milk. 11 Ask your healthcare provider or lactation consultant for help.
“For the first few months my life revolved around pumping. I set an alarm and woke up every three hours at night to express milk,” recalls Katherine, a mother of two from New Zealand, “Michael had a cleft palate, so he couldn’t suckle, and we had to use a special squeeze bottle. When he ate, I did not take my eyes off him - as soon as I turned away, he could choke, or I did not notice how milk began to flow from his nose, which he did not like very much.
I set an alarm and woke up every three hours at night to express milk,” recalls Katherine, a mother of two from New Zealand, “Michael had a cleft palate, so he couldn’t suckle, and we had to use a special squeeze bottle. When he ate, I did not take my eyes off him - as soon as I turned away, he could choke, or I did not notice how milk began to flow from his nose, which he did not like very much.
Participating in online support groups for mothers who only feed their babies with expressed milk has helped me a lot. I was able to express milk for my son for seven whole months - it was a real work in the name of love!”
Ways to breastfeed your baby
In some cases, your baby needs to be fed in a special way before he can breastfeed or bottle feed. For example, a feeding tube can be used to deliver milk directly into the baby's stomach. The tube is inserted by the attending physician, usually through the nose or mouth. As soon as the baby can eat in the usual way, the tube will be removed.
If the baby can swallow but is unable to breastfeed, alternative ways of feeding may be recommended. “For infants suffering from neurological disorders, you can use a drinking tube with a feeding tube or a special silicone nozzle on the finger, which an adult presses a finger against the palate. Some babies find it more convenient to eat with a special cup*, says Dr. Mitsuno. It all depends on the characteristics of the baby. Some people prefer drinking cups.”
“Cup cup feeding* is one of the most popular and safest ways to feed a baby who cannot breastfeed,” Dr. Mitsuno continues. you will be able to breastfeed your baby longer. Cup feeding usually spills quite a lot of milk, 12 and the amount spilled must be measured and accounted for if a specific amount of milk is recommended for an infant.”
Sarah, a UK mother of three, recalls: “Our eldest daughter is a child with special needs. In particular, she has cerebral palsy. At first she suckled well at the breast, but on the third day her condition worsened, and until the age of two months she was fed expressed breast milk through a nasogastric tube. While she was in the hospital, I pumped milk every three hours.”
While she was in the hospital, I pumped milk every three hours.”
Sarah's story ended well: “At about eight weeks, my daughter's condition stabilized, and with the help of a specialist, we resumed breastfeeding. She switched to breastfeeding very easily. By the time she was 12 weeks old and we took her home, she was exclusively breastfed.
Although many people cared for our baby, pumping made me feel important, my special role. It helped me get through that incredibly difficult period.”
If your baby can latch on
If your baby has special needs but is physiologically able to latch on, offer the breast regularly along with other feeding methods. Even if he can't suckle milk from his breast, this "soothing" suckling will help him feel safe, warm, and cared for. It will also help your baby practice suckling skills, making it easier for him to transition to breastfeeding later on.
If your baby can breastfeed but is not getting enough milk, talk to your doctor about how much pumped milk you need to supplement and how best to give it. You can give your baby expressed milk while breastfeeding with a supplemental feeding system* or use one of the devices mentioned above.
You can give your baby expressed milk while breastfeeding with a supplemental feeding system* or use one of the devices mentioned above.
If your baby is recovering from maxillofacial surgery (eg for a cleft lip or palate), breastfeeding may be uncomfortable. However, offer your baby the breast along with other ways of feeding, according to some studies, sedative sucking can relieve pain. 13
“Everyone told me that because of the cleft lip, my son would not be able to breastfeed. But in fact, he was good at it, even though he injured my nipples while doing it,” recalls Nicola, a mother of three children from the UK, “After the operation, he was in pain at first, but soon everything returned to normal. He began to latch on very differently so it took us both some time to adjust, but pretty soon he was able to breastfeed normally and I breastfed him for up to a year.”
Literature
1 Walker M. Breastfeeding management for the clinician. 4th edition. Burlington, MA, USA: Jones & Bartlett Publishers; 2016. 738 p. — Walker, M., Breastfeeding Considerations for Practitioners, 4th edition. Burlington, Massachusetts, USA: Jones & Bartlett Publishers; 2016. Pp. 738.
4th edition. Burlington, MA, USA: Jones & Bartlett Publishers; 2016. 738 p. — Walker, M., Breastfeeding Considerations for Practitioners, 4th edition. Burlington, Massachusetts, USA: Jones & Bartlett Publishers; 2016. Pp. 738.
2 Seddon PC, Khan Y. Respiratory problems in children with neurological impairment. Arch DisChild. 2003;88(1):75-78. - Seddon PS, Khan Y, "Respiratory problems in children with neurological deficits." Arch Dis Child. 2003;88(1):75-78.
3 Proesmans M. Respiratory illness in children with disability: a serious problem?. Breathe. 2016;12(4): e 97. - Proesmans M., "Respiratory diseases in children with disabilities: a serious problem?" Breeze (Breath). 2016;12(4):e97.
4 Zeisel SA, Roberts JE. Otitis media in young children with disabilities. Infants Young Child. 2003;16(2):106-119. - Zeisel SA, Roberts JI, "Otitis media in young disabled children". Infants Young Children. 2003;16(2):106-119.
2003;16(2):106-119. - Zeisel SA, Roberts JI, "Otitis media in young disabled children". Infants Young Children. 2003;16(2):106-119.
5 González DJ et al. Gastrointestinal disorders in children with cerebral palsy and neurodevelopmental disabilities. An Pediatr (Barc). 2010;73(6):361. - Gonzalez D.J. et al., Gastrointestinal Disorders in Children with Cerebral Palsy and Neurological Diseases. An Pediatrician (Bark). 2010;73(6):361.
6 Salvatori G et al. Human milk and breastfeeding in surgical infants. Breastfeed Med . 2014;9(10):491-493. - Salvatori J. et al., Breast milk and breastfeeding in children undergoing surgery. Brestfeed Med (Breastfeeding Medicine). 2014;9(10):491-493.
7 Reilly S et al. ABM Clinical Protocol# 17: Guidelines for breastfeeding infants with cleft lip, cleft palate, or cleft lip and palate, Revised 2013. Breastfeed Med . 2013;8(4):349-353. - Reilly S. et al., AVM Clinical Protocol #17: Guidelines for breastfeeding children with cleft lip, cleft palate, or cleft lip and palate, 2013 edition. Brestfeed Med (Breastfeeding Medicine). 2013;8(4):349-353. Thomas J et al . ABM Clinical Protocol #16: Breastfeeding the Hypotonic Infant, Revision 2016. Breastfeed Med 2016;11(6). - Thomas J. et al., "AVM Clinical Protocol #16: Breastfeeding a Baby with Reduced Muscle Tone, Revision 2016." Brestfeed Med (Breastfeeding Medicine). 2016;11(6).
Breastfeed Med . 2013;8(4):349-353. - Reilly S. et al., AVM Clinical Protocol #17: Guidelines for breastfeeding children with cleft lip, cleft palate, or cleft lip and palate, 2013 edition. Brestfeed Med (Breastfeeding Medicine). 2013;8(4):349-353. Thomas J et al . ABM Clinical Protocol #16: Breastfeeding the Hypotonic Infant, Revision 2016. Breastfeed Med 2016;11(6). - Thomas J. et al., "AVM Clinical Protocol #16: Breastfeeding a Baby with Reduced Muscle Tone, Revision 2016." Brestfeed Med (Breastfeeding Medicine). 2016;11(6).
9 Wilson EM, Hustad KC. Early feeding abilities in children with cerebral palsy: a parental report study. J Med Speech Lang Pathol. 2009: nihpa 57357. - Wilson I.M., Khustad K.S., "Early independent feeding ability in children with cerebral palsy: a study of parent reports". J Med Speech Lang Patol. 2009: nihpa 9 E et a. Feeding-facilitating techniques for the nursing infant with Robin sequence. Cleft Palate Craniofac 2006;43(1):55-60. — Nassar, I. et al., Feeding Ease Techniques for Babies with Robin Syndrome. Kleft Palet Kraniofak J. 2006;43(1):55-60.
J Med Speech Lang Patol. 2009: nihpa 9 E et a. Feeding-facilitating techniques for the nursing infant with Robin sequence. Cleft Palate Craniofac 2006;43(1):55-60. — Nassar, I. et al., Feeding Ease Techniques for Babies with Robin Syndrome. Kleft Palet Kraniofak J. 2006;43(1):55-60.
11 Kent JC Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
12 Dowling DA et al. Cup-feeding for preterm infants: mechanics and safety. J Hum Lact 2002;18(1):13-20. - Dowling D.A. et al., "Cup feeding preterm infants: technique and safety issues". F Hum Lakt. 2002;18(1):13-20.
J Hum Lact 2002;18(1):13-20. - Dowling D.A. et al., "Cup feeding preterm infants: technique and safety issues". F Hum Lakt. 2002;18(1):13-20.
13 Harrison D et al. Breastfeeding for procedural pain in infants beyond the neonatal period. Cochrane Database of 2014;10: CD 11248 - Harrison D. et al., "Breastfeeding for Pain Relief from Medical Intervention in the Neonatal Period." Cochrane Database of System Rev. 2014;10: CD 11248
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. FZZ 2010/07353 of 07/19/2010
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 No wonder this time is called the "magic hour"!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What should I do if the birth did not go according to plan?
If you had a caesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
“While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum you can feed your baby. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk, and therefore grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns its head if it feels a touch on its cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black.
- Texture: sticky like tar.
Second day
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. 11
In addition, during the first few days, the weight of wet diapers increases. 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that your baby is not getting enough milk. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.