How to feed newborn baby after c section
Breastfeeding After C-section: What You Should Know
Many expecting parents who consider a possible cesarean delivery — also known as a C-section — have concerns about how it might affect their ability to breastfeed. This is totally understandable.
Will my milk come in? Will I be able to find a comfortable position? How will the pain meds affect me and my baby? What if I’m separated from my baby? Will I have the energy to breastfeed? These are just some of the many questions you may have about breastfeeding after a C-section.
Despite what you may have heard, though, breastfeeding after a C-section is absolutely possible. While you may face challenges, most who wish to breastfeed can successfully do so after their C-section.
In most cases, you’ll be able to breastfeed soon after your C-section. Sometimes this can even happen while you’re still in the operating room.
You may have heard that breastfeeding in the first hour after birth is recommended to ensure your chances of successful breastfeeding. Since a C-section is major surgery, it makes sense that you might be concerned about your ability to breastfeed within that first hour or so.
But even if you aren’t able to initiate breastfeeding right away — for example, if you or your baby have a medical issue that requires you two to be separated — you can still protect your milk supply and establish a strong breastfeeding relationship with your baby.
Although many new parents sail through their C-section and breastfeeding experiences without issues, some encounter challenges related to their C-section. Still, there are many ways to address these challenges successfully. You can do this!
Here are some potential complications, as well as tips on how how to manage them:
Post-delivery medical needs
If your baby has a medical need and must spend some time in the neonatal intensive care unit (NICU), you can still breastfeed successfully. The same is true if you have a post-birth complication and need to be separated from your baby.
If at all possible, pump your breast milk as soon as possible after birth. This will get your milk supply started and ensure a robust supply for your baby. Once you’re reunited with your baby, you can work on latching and initiating breastfeeding.
Medications
As you recover from your C-section, you’ll be given medications to manage the pain. Most pain medications are compatible with breastfeeding, as only small amounts of them pass into your milk.
You can consult your OB-GYN about the medication you’re taking and its compatibility with breastfeeding. If they say it’s not compatible, there are usually alternative pain medications.
Anesthesia
The type of anesthesia used, as well as how much you were given, may affect breastfeeding.
Anesthesia can make your baby more drowsy at first, which can affect their ability to breastfeed. Yet, all babies respond differently to anesthesia, and its potential effects depend on the type of anesthesia you were given, along with the duration of its administration.
For example, a regional anesthetic, which allows you to be awake for the surgery, will likely have less of an effect on your baby than general anesthesia.
Delayed milk production
Studies have shown that C-sections may delay the start of mature milk production, which is when your milk comes in.
During the first few days after birth, your body produces colostrum — your baby’s first milk. Colostrum is low in volume but full of antibodies and other protection for your baby. About 2 to 5 days after birth, your milk becomes more abundant.
When exactly your milk comes in may be delayed by a few days if you’ve had a C-section, but it will come in eventually. You can help quicken this process by breastfeeding or pumping regularly, breastfeeding on demand, and having lots of skin-to-skin time with your baby.
Pain
You’re recovering from major abdominal surgery. As such, you’ll experience some pain or discomfort. Plus, no matter how delivery happens, you’ll experience uterine contractions after birth as your uterus shrinks back to pre-pregnancy size.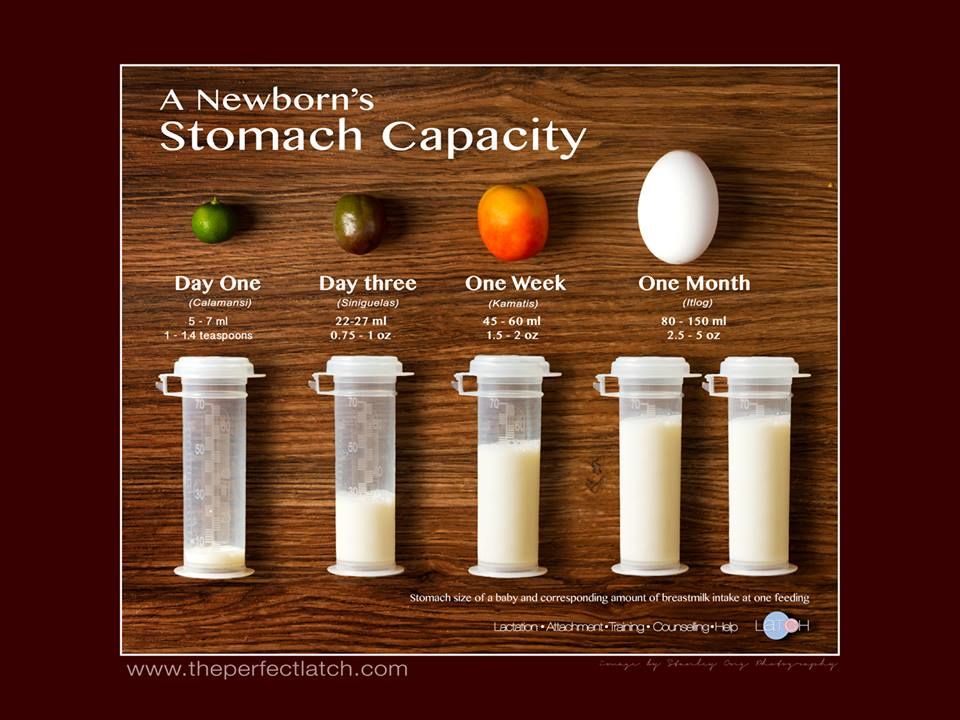
Don’t hesitate to use medication to soothe your pain or discomfort. Pain will definitely interfere with your ability to comfortably breastfeed, so it’s important to do what you need to do to take the edge off.
Again, most medications don’t pass into breast milk at high enough levels to affect the baby, but you can talk to your doctor or lactation consultant about options.
Emotions
Giving birth is an experience that generates intense emotions.
It’s not uncommon to feel overwhelmed or sad in the post-birth days. Known as the baby blues, this emotional rollercoaster is due to shifting hormone levels, as well as the shift in identity that you experience as you become a parent or expand your family.
If you experienced a traumatic birth or complications after your C-section, your baby blues may be even more intense. You may feel guilt or anxiety, and if breastfeeding is challenging, things just might feel really hard.
Share how you’re feeling with others. Don’t hesitate to reach out to your doctor or midwife if your feelings are too hard to manage alone.
Don’t hesitate to reach out to your doctor or midwife if your feelings are too hard to manage alone.
Ensuring that you’re able to initiate breastfeeding as soon as possible after your baby’s birth might take some planning. If you know you’re going to have a C-section, you can do a few things before the birth to make sure you can initiate breastfeeding as soon as possible after your baby is born.
Choose a baby-friendly hospitalHospitals that have earned the Baby-Friendly designation from the Baby-Friendly Hospital Initiative (BFHI) are more likely to have policies that promote early breastfeeding, such as skin-to-skin time and rooming-in, which is the practice of keeping a newborn’s crib at the side of their mother’s bed.
Even if your hospital isn’t a designated Baby-Friendly hospital, you can ask about what policies it has that will allow you early access to your baby for breastfeeding.
Make sure you understand hospital policies
Familiarizing yourself with your hospital’s policies beforehand can be very helpful. For example, does your hospital allow you to breastfeed in the operating room, assuming mom and baby are healthy? Will the hospital provide you a pump if your baby can’t be brought to your breast right away?
For example, does your hospital allow you to breastfeed in the operating room, assuming mom and baby are healthy? Will the hospital provide you a pump if your baby can’t be brought to your breast right away?
Find out whether a lactation consultant can be brought into the delivery room
Having a breastfeeding helper nearby can be very helpful during that first hour or two after your C-section.
As you’re recovering, you may need help bringing your baby to your breast and positioning them. A lactation consultant can also be an advocate for you in prioritizing early breastfeeding.
Advocate for yourself
Make sure your OB-GYN knows about your desire to breastfeed as soon as possible after birth. Ask them how that can be accomplished. Can someone — your partner, nurse, or lactation consultant — bring you the baby after surgery and help you initiate breastfeeding?
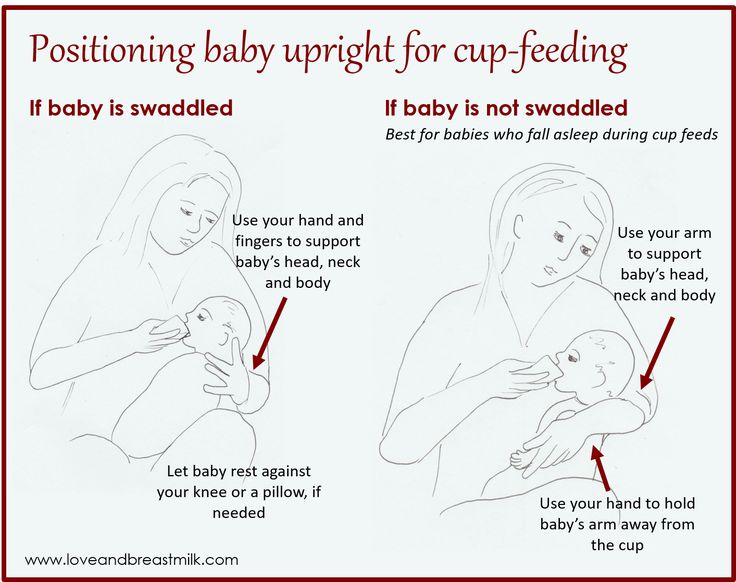
As you recover from your C-section, certain breastfeeding positions will be more comfortable than others.
You’ll want to be sure that you use positions that keep your baby’s weight off your healing incision, so more traditional breastfeeding positions like the cradle or cross-cradle hold might not be comfortable in the early weeks.
Two positions that are usually best for post-C-section breastfeeding are the side lying position and football hold. In these positions, your baby doesn’t make contact with your incision. Here’s how to do them:
Side lying
Lie in bed on your side, belly to belly with your baby. Place your baby a few inches below the breast that’s making contact with the bed.
Next, position your baby’s nose to your nipple, and then latch them on. You might need to experiment with pillows for your own comfort. You can ask a helper to bring you the baby when you’re in bed and help you position them.
Football hold
Sitting up in a chair or recliner, wrap your baby around the side of your body (under your arm), with their belly facing your body. Keeping them snug and close, have them latch onto your breast. Pillows can help prop your baby up against your body.
Keeping them snug and close, have them latch onto your breast. Pillows can help prop your baby up against your body.
Your top goals should be to breastfeed frequently, keep your milk flowing, and reach out for help if needed. Here’s what to keep in mind:
- Practice skin-to-skin contact. This is a great way to keep your milk supply up, establish breastfeeding, and bond with your baby.
- Pump often. If your baby is separated from you, sleepy at the breast, or your milk is slow to come in, pump every 2 to 3 hours. Expressing by hand can be helpful in the early days before your milk is in.
- Breastfeed on demand. Respond to baby’s cues and initiate feedings whenever they’re requested, or at least every 2 to 3 hours. The more frequently you bring your baby to the breast, the more robust your milk supply will be.
- Get help! You’re recovering from surgery, caring for a baby, and learning to breastfeed.
 That’s a lot and you can’t possibly do it alone. Accept offers of help, don’t expect to entertain visitors right now, and make sure you get lots of rest as you recover and snuggle that baby close.
That’s a lot and you can’t possibly do it alone. Accept offers of help, don’t expect to entertain visitors right now, and make sure you get lots of rest as you recover and snuggle that baby close. - Contact a breastfeeding consultant. If you can’t solve a breastfeeding problem on your own, it may be time to get an expert involved. Usually, the sooner you address a breastfeeding concern, the easier it will be to solve.
Breastfeeding after a C-section is possible, but that doesn’t mean it’s easy.
If you’re struggling, you might be overwhelmed by difficult feelings. One of the best things you can do is share how you’re feeling with others. Your feelings are normal and OK.
If you’re having trouble managing your emotions or functioning, reach out to your healthcare provider. They can evaluate whether you have a postpartum mood disorder and get you the help you need.
Most of all, remember that you’re an amazing parent. You can do this, and before you know it, breastfeeding your baby will be second nature.
Breastfeeding After C-section: What You Should Know
Many expecting parents who consider a possible cesarean delivery — also known as a C-section — have concerns about how it might affect their ability to breastfeed. This is totally understandable.
Will my milk come in? Will I be able to find a comfortable position? How will the pain meds affect me and my baby? What if I’m separated from my baby? Will I have the energy to breastfeed? These are just some of the many questions you may have about breastfeeding after a C-section.
Despite what you may have heard, though, breastfeeding after a C-section is absolutely possible. While you may face challenges, most who wish to breastfeed can successfully do so after their C-section.
In most cases, you’ll be able to breastfeed soon after your C-section. Sometimes this can even happen while you’re still in the operating room.
You may have heard that breastfeeding in the first hour after birth is recommended to ensure your chances of successful breastfeeding. Since a C-section is major surgery, it makes sense that you might be concerned about your ability to breastfeed within that first hour or so.
Since a C-section is major surgery, it makes sense that you might be concerned about your ability to breastfeed within that first hour or so.
But even if you aren’t able to initiate breastfeeding right away — for example, if you or your baby have a medical issue that requires you two to be separated — you can still protect your milk supply and establish a strong breastfeeding relationship with your baby.
Although many new parents sail through their C-section and breastfeeding experiences without issues, some encounter challenges related to their C-section. Still, there are many ways to address these challenges successfully. You can do this!
Here are some potential complications, as well as tips on how how to manage them:
Post-delivery medical needs
If your baby has a medical need and must spend some time in the neonatal intensive care unit (NICU), you can still breastfeed successfully. The same is true if you have a post-birth complication and need to be separated from your baby.
If at all possible, pump your breast milk as soon as possible after birth. This will get your milk supply started and ensure a robust supply for your baby. Once you’re reunited with your baby, you can work on latching and initiating breastfeeding.
Medications
As you recover from your C-section, you’ll be given medications to manage the pain. Most pain medications are compatible with breastfeeding, as only small amounts of them pass into your milk.
You can consult your OB-GYN about the medication you’re taking and its compatibility with breastfeeding. If they say it’s not compatible, there are usually alternative pain medications.
Anesthesia
The type of anesthesia used, as well as how much you were given, may affect breastfeeding.
Anesthesia can make your baby more drowsy at first, which can affect their ability to breastfeed. Yet, all babies respond differently to anesthesia, and its potential effects depend on the type of anesthesia you were given, along with the duration of its administration.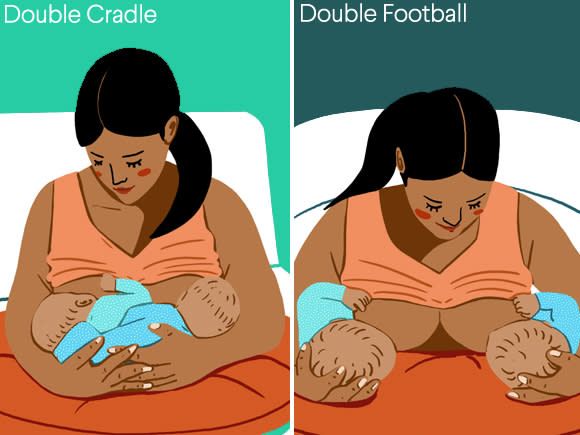
For example, a regional anesthetic, which allows you to be awake for the surgery, will likely have less of an effect on your baby than general anesthesia.
Delayed milk production
Studies have shown that C-sections may delay the start of mature milk production, which is when your milk comes in.
During the first few days after birth, your body produces colostrum — your baby’s first milk. Colostrum is low in volume but full of antibodies and other protection for your baby. About 2 to 5 days after birth, your milk becomes more abundant.
When exactly your milk comes in may be delayed by a few days if you’ve had a C-section, but it will come in eventually. You can help quicken this process by breastfeeding or pumping regularly, breastfeeding on demand, and having lots of skin-to-skin time with your baby.
Pain
You’re recovering from major abdominal surgery. As such, you’ll experience some pain or discomfort. Plus, no matter how delivery happens, you’ll experience uterine contractions after birth as your uterus shrinks back to pre-pregnancy size.
Don’t hesitate to use medication to soothe your pain or discomfort. Pain will definitely interfere with your ability to comfortably breastfeed, so it’s important to do what you need to do to take the edge off.
Again, most medications don’t pass into breast milk at high enough levels to affect the baby, but you can talk to your doctor or lactation consultant about options.
Emotions
Giving birth is an experience that generates intense emotions.
It’s not uncommon to feel overwhelmed or sad in the post-birth days. Known as the baby blues, this emotional rollercoaster is due to shifting hormone levels, as well as the shift in identity that you experience as you become a parent or expand your family.
If you experienced a traumatic birth or complications after your C-section, your baby blues may be even more intense. You may feel guilt or anxiety, and if breastfeeding is challenging, things just might feel really hard.
Share how you’re feeling with others. Don’t hesitate to reach out to your doctor or midwife if your feelings are too hard to manage alone.
Don’t hesitate to reach out to your doctor or midwife if your feelings are too hard to manage alone.
Ensuring that you’re able to initiate breastfeeding as soon as possible after your baby’s birth might take some planning. If you know you’re going to have a C-section, you can do a few things before the birth to make sure you can initiate breastfeeding as soon as possible after your baby is born.
Choose a baby-friendly hospitalHospitals that have earned the Baby-Friendly designation from the Baby-Friendly Hospital Initiative (BFHI) are more likely to have policies that promote early breastfeeding, such as skin-to-skin time and rooming-in, which is the practice of keeping a newborn’s crib at the side of their mother’s bed.
Even if your hospital isn’t a designated Baby-Friendly hospital, you can ask about what policies it has that will allow you early access to your baby for breastfeeding.
Make sure you understand hospital policies
Familiarizing yourself with your hospital’s policies beforehand can be very helpful. For example, does your hospital allow you to breastfeed in the operating room, assuming mom and baby are healthy? Will the hospital provide you a pump if your baby can’t be brought to your breast right away?
For example, does your hospital allow you to breastfeed in the operating room, assuming mom and baby are healthy? Will the hospital provide you a pump if your baby can’t be brought to your breast right away?
Find out whether a lactation consultant can be brought into the delivery room
Having a breastfeeding helper nearby can be very helpful during that first hour or two after your C-section.
As you’re recovering, you may need help bringing your baby to your breast and positioning them. A lactation consultant can also be an advocate for you in prioritizing early breastfeeding.
Advocate for yourself
Make sure your OB-GYN knows about your desire to breastfeed as soon as possible after birth. Ask them how that can be accomplished. Can someone — your partner, nurse, or lactation consultant — bring you the baby after surgery and help you initiate breastfeeding?
As you recover from your C-section, certain breastfeeding positions will be more comfortable than others.
You’ll want to be sure that you use positions that keep your baby’s weight off your healing incision, so more traditional breastfeeding positions like the cradle or cross-cradle hold might not be comfortable in the early weeks.
Two positions that are usually best for post-C-section breastfeeding are the side lying position and football hold. In these positions, your baby doesn’t make contact with your incision. Here’s how to do them:
Side lying
Lie in bed on your side, belly to belly with your baby. Place your baby a few inches below the breast that’s making contact with the bed.
Next, position your baby’s nose to your nipple, and then latch them on. You might need to experiment with pillows for your own comfort. You can ask a helper to bring you the baby when you’re in bed and help you position them.
Football hold
Sitting up in a chair or recliner, wrap your baby around the side of your body (under your arm), with their belly facing your body.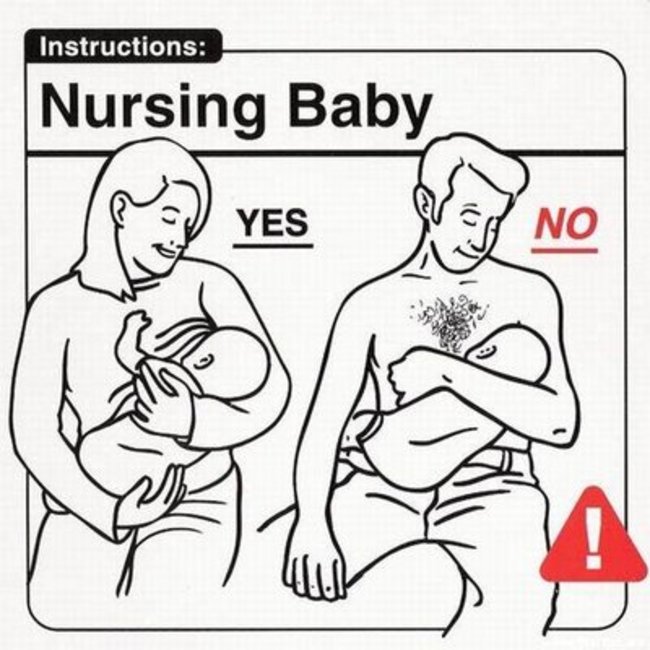 Keeping them snug and close, have them latch onto your breast. Pillows can help prop your baby up against your body.
Keeping them snug and close, have them latch onto your breast. Pillows can help prop your baby up against your body.
Your top goals should be to breastfeed frequently, keep your milk flowing, and reach out for help if needed. Here’s what to keep in mind:
- Practice skin-to-skin contact. This is a great way to keep your milk supply up, establish breastfeeding, and bond with your baby.
- Pump often. If your baby is separated from you, sleepy at the breast, or your milk is slow to come in, pump every 2 to 3 hours. Expressing by hand can be helpful in the early days before your milk is in.
- Breastfeed on demand. Respond to baby’s cues and initiate feedings whenever they’re requested, or at least every 2 to 3 hours. The more frequently you bring your baby to the breast, the more robust your milk supply will be.
- Get help! You’re recovering from surgery, caring for a baby, and learning to breastfeed.
 That’s a lot and you can’t possibly do it alone. Accept offers of help, don’t expect to entertain visitors right now, and make sure you get lots of rest as you recover and snuggle that baby close.
That’s a lot and you can’t possibly do it alone. Accept offers of help, don’t expect to entertain visitors right now, and make sure you get lots of rest as you recover and snuggle that baby close. - Contact a breastfeeding consultant. If you can’t solve a breastfeeding problem on your own, it may be time to get an expert involved. Usually, the sooner you address a breastfeeding concern, the easier it will be to solve.
Breastfeeding after a C-section is possible, but that doesn’t mean it’s easy.
If you’re struggling, you might be overwhelmed by difficult feelings. One of the best things you can do is share how you’re feeling with others. Your feelings are normal and OK.
If you’re having trouble managing your emotions or functioning, reach out to your healthcare provider. They can evaluate whether you have a postpartum mood disorder and get you the help you need.
Most of all, remember that you’re an amazing parent. You can do this, and before you know it, breastfeeding your baby will be second nature.
How to improve lactation after caesarean section
Kushalieva Xenia
Published: 01/15/2023
Reading time: 5 min
1577
Less than half of babies in Russia up to six months of age are breastfed. Only a third of children receive it per year. These are the data of the Federal State Statistics Service.
Meanwhile, a full-fledged replacement for breast milk has not yet been invented, and it is almost always possible to establish lactation if the mother and the newborn do not have serious illnesses.
This is important!
Even after a caesarean section, which in practice in 70% of cases leads to the introduction of formula supplementation already in the hospital, breastfeeding can be successfully started and continued for as long as the young mother and her baby need.
Why does caesarean section negatively affect lactation?
Caesarean section is not a reason to stop breastfeeding, but it is objectively more difficult for mothers to establish lactation after this operation than for women who gave birth naturally.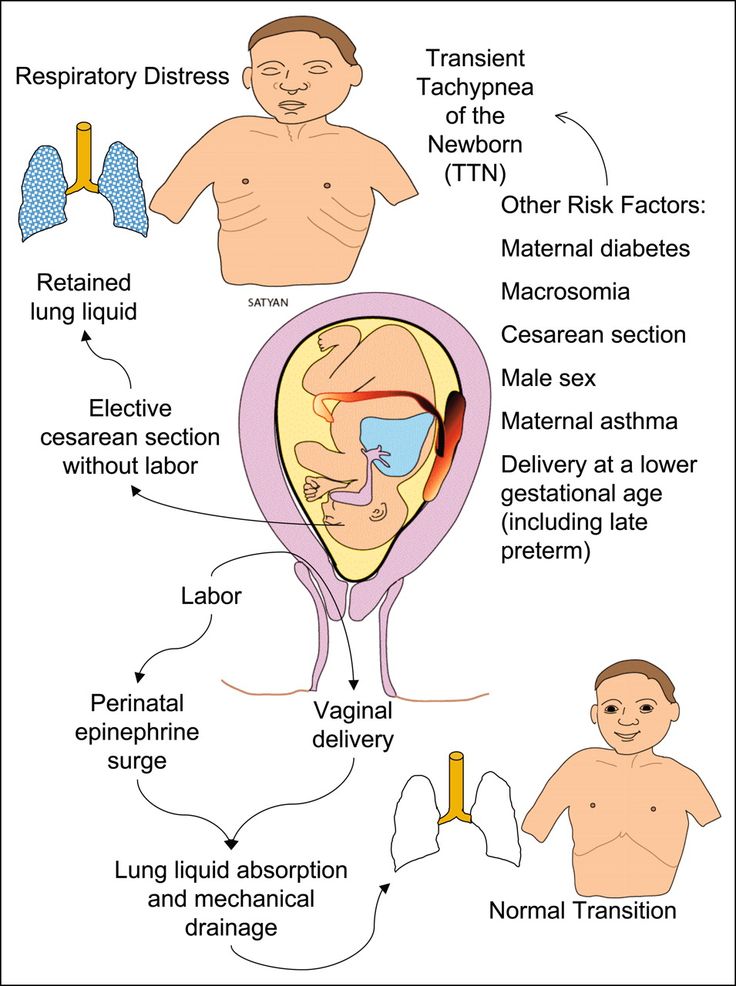
- The body of the expectant mother prepares for feeding the baby from the first days of pregnancy: the structure and size of the breast changes, colostrum production begins in the second trimester. Childbirth is the logical conclusion of this preparation. When a baby is born by caesarean section, the mechanism of lactation starts late, as its natural hormonal setting gets off.
- In a newborn after a caesarean section, the sucking reflex may be weak at first, because the child did not pass through the birth canal and did not have time to adapt to the new conditions that suddenly appeared.
- The first application to the breast is possible in the first minutes after the caesarean section, only if the operation was planned and performed under epidural anesthesia. If a woman in labor needs an emergency CS, then it can be under general anesthesia. In this case, the first feeding can take place only a day after the operation. During this time, the child will already be fed with a mixture and it will be much more difficult to successfully establish lactation.
- After a caesarean section, a woman may be given antibiotics. Doctors usually prescribe medications that are compatible with breastfeeding, but complications sometimes require stronger medications. Then the mother will have to express milk regularly to maintain lactation until the end of the course of treatment. However, it is not a fact that the baby will prefer the breast to the familiar bottle with the mixture.
- After the operation, a young mother may have difficulty recovering from anesthesia, feel weak if there was a large blood loss. A painful stitch will make it difficult to find a comfortable feeding position. In this state, it takes a lot of determination to feed on demand, against all odds.
Despite the fact that caesarean section creates additional difficulties in organizing breastfeeding, the mother can and should try to cope with them. This will help her save her own health and protect her baby.
Tips on breastfeeding after a caesarean section
- If you have an elective caesarean section, talk to your doctor ahead of time and let them know that you would like to breastfeed.
Discuss any points that make you anxious. Your mental attitude is just as important as your physical condition, so work on it and get support.
- Before the operation, ask that the baby be placed on your breast immediately, if possible, while still on the operating table.
- Insist on sharing the ward with your newborn, even if you are offered to rest alone and bring the baby to feeds. The baby will feel protected next to you, and you can feed him on demand - then the milk will come faster and there will be more of it.
- Ask your puerperal midwife or nurse to show you how to properly latch on to your baby. The baby's mouth should be wide open, the lower lip turned inside out, the areola can be visible only above the upper lip, and completely hidden from below in the baby's mouth. If the baby does not take the breast correctly, he may remain hungry, and it will be painful for you to feed, cracked nipples may appear.
- Learn how to express manually and, if necessary, with a breast pump.
It will help to maintain lactation if, while taking medication, you will not be able to breastfeed for the first time.
- Do not give your baby a pacifier or a bottle with a nipple for at least the first month after birth, until lactation is fully established. Drink the mixture or medicine, if necessary, from a spoon or syringe.
So, a caesarean section is not a hindrance to breastfeeding, although it will be a little more difficult to establish lactation. Considering how beneficial breastfeeding is for the mother, and breast milk for the baby, you need to tune in to overcome difficulties. Successful breastfeeding after cesarean will be helped by the joint stay of mother and baby in the postpartum ward, on-demand feeding, the correct application technique and psychological support from both medical staff and loved ones.
Author of article
Kushalieva Xenia
Pediatrician, lactation specialist
About the author
Share on Vkontakte Share on Odnoklassniki
Contents of the article
- Why does caesarean section negatively affect lactation?
- Advice on how to establish breastfeeding after caesarean section
Products from article
Baby formula Nutrilak Premium Caesarea BIFI
From birth
Might be interesting
- 10 recipes for nursing mothers
- Choosing a maternity hospital
- Cesarean
- Long-term breastfeeding
Breastfeeding after caesarean section
You must have heard the opinion that it is difficult to breastfeed after a caesarean section because there is no milk in the breast. This statement is not true. The signal that causes the body to produce milk is the delivery of the placenta, and this happens both in a vaginal birth and in a caesarean section, just a little differently.
Lactation is not the same for every woman. Some have a lot of milk and it appears quite quickly, while others produce it later and in smaller quantities. Your correct attitude towards breastfeeding is very important, and you should not give in to the suggestions of grandmothers or aunts that your milk is not valuable enough or there is not enough of it. Colostrum appears first. It is quite enough to feed a newborn. Therefore, you should not supplement the baby with a formula for newborns, but apply it to the breast as often as possible. This stimulates lactation. Your breasts produce more milk to meet the needs of a growing little person.
Birth can be difficult for both caesarean section and vaginal delivery.
Don't despair, keep trying until you succeed. While in the hospital, you can always ask the midwife to help you show you how to attach the baby so that he suckles properly.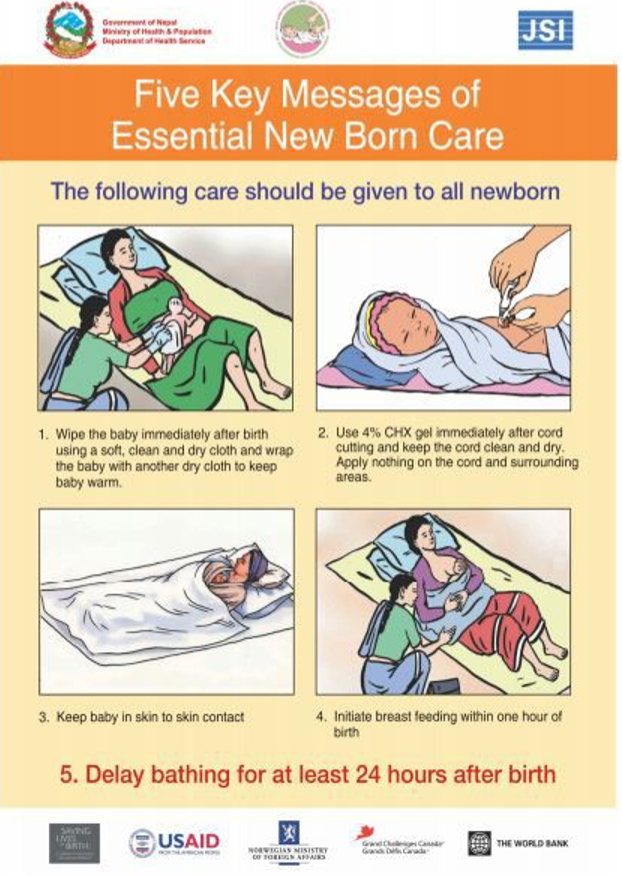
If, despite everything, you still have problems with lactation, don't worry. This can be caused by stress and emotions that have not subsided yet. At home, when you are alone with your child, it will be easier for you to calm down and focus. You will be able to carefully study your baby's daily routine, find the most appropriate position for feeding, and your baby will eventually begin to suckle, and there is a lot of evidence for this. Lactation does not stop overnight. It can be stimulated even after a few days.
You can always ask for help from a lactation specialist. It is worth looking for a good specialist even before the birth of the child.
Remember! The sooner you attach the baby, the better. Each application stimulates the lactation process.
A breastfed newborn needs frequent latching, but not because the mother's milk is not complete. Feeding satisfies not only hunger, but also the need for security.
If you have had a local or spinal anesthetic and you and your baby are well, you can apply it right away. But you should know that after the operation, you must lie in a horizontal position without lifting your head for 12 hours. Sometimes this period may be shorter, but the anesthesiologist must make the decision, and he will definitely instruct the midwives who will care for you.
But you should know that after the operation, you must lie in a horizontal position without lifting your head for 12 hours. Sometimes this period may be shorter, but the anesthesiologist must make the decision, and he will definitely instruct the midwives who will care for you.
If you had an operation under general anesthesia, which is now very rarely used, then with the first feeding you need to wait until you regain consciousness and gain strength. In addition, your body must remove the anesthetic, as it can pass through your milk and into the body of the newborn.
In most hospitals, after a caesarean section, the newborn is brought to the mother for the first feeding within the first day after birth. If you feel well, you can always ask the staff to bring the baby in for feeding earlier than recommended. In some hospitals, the baby is released to the mother immediately after the caesarean section. Ask in advance what the procedure is at the hospital where you are going to give birth.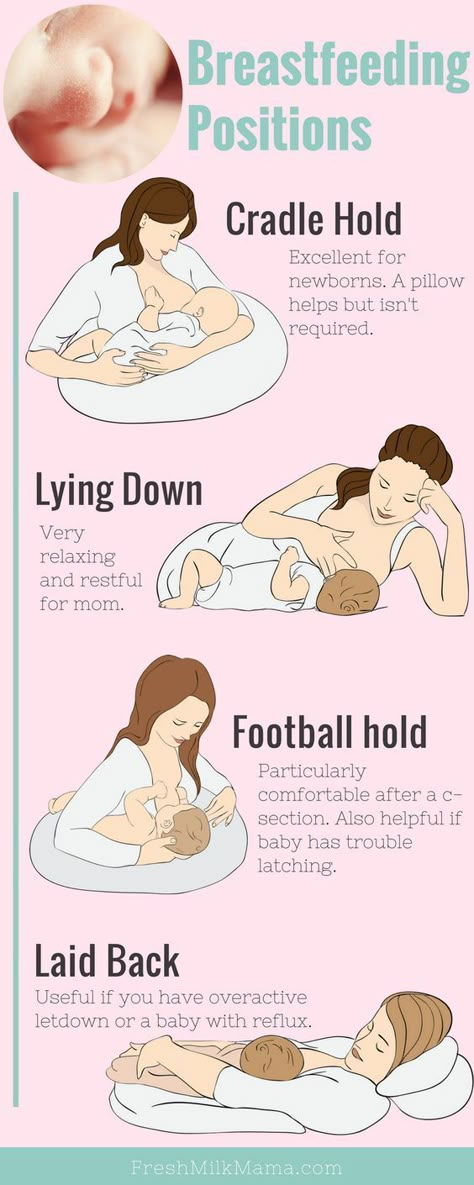
Feeding positions after caesarean section:
In fact, every position is good. The most important thing is that you and your baby are comfortable.
Lying on the back - in this position, the baby sucks milk slowly. This is a safe position, as the child does not swallow a large amount of air, and lying on you does not put pressure on the wound on the stomach. This is especially recommended after a cesarean section, when the first couple of hours you need to lie strictly horizontally. The baby's head should be at the same level as your chest. When the baby lies on you, support him with your hand on one side.
>"Side feeding" - you lie on one side, put your hand on the bed, and your head a little higher on the pillow. You put the baby in front of you, tummy to tummy. Rest his head against your hand or lay him directly on the bed. You can place a rolled up blanket or a few pillows behind your back or between your legs. This position is recommended after caesarean section and for night feedings. "
"
Linked position - in this position, the baby's legs are under your armpit, you hold his head and neck with your hand, and your back with your forearm so that he does not touch the wound. His tummy is pressed against to your side.This position is best for breastfeeding on a couch or in a chair.Put a pillow under your back to make it more comfortable.You can place a rolled blanket over your knees and on your side to support your hand during feeding, which can take some time.
What if the baby is premature?
If your baby was born by caesarean section and for some reason has to spend some time in an incubator, this does not mean that he cannot drink your milk. You can express milk with a breast pump until your baby is strong enough to suckle on his own.
The most important thing is to maintain lactation. It may be just a few drops at first, but over time it will definitely become more abundant. When the baby becomes more independent, apply it to the chest.