How to make baby feed more
Feeding Your 1- to 3-Month-Old (for Parents)
During your baby's first 3 months, breast milk or formula will provide all the nutrition needed. Doctors recommend waiting until your baby is about 6 months old to start solid foods. Some babies may be ready for solids sooner than 6 months, but wait until your baby is at least 4 months old.
What Changes Should I Expect?
As your infant grows, feeding will change. Babies will start drinking more milk during each feeding, so they won't need to feed as often and will sleep longer at night.
Your baby's appetite will increase during growth spurts. Continue to feed on demand and increase the number of feedings as needed.
Your infant also will become more alert as the weeks go by, cooing and smiling. So there will be more interaction between you and your baby during feedings.
The following are general guidelines, and your baby may be hungrier more or less often than this. That's why it's important to pay attention to your baby's signals of being hungry or full. A baby who is getting enough might slow down, stop, or turn away from the breast or bottle.
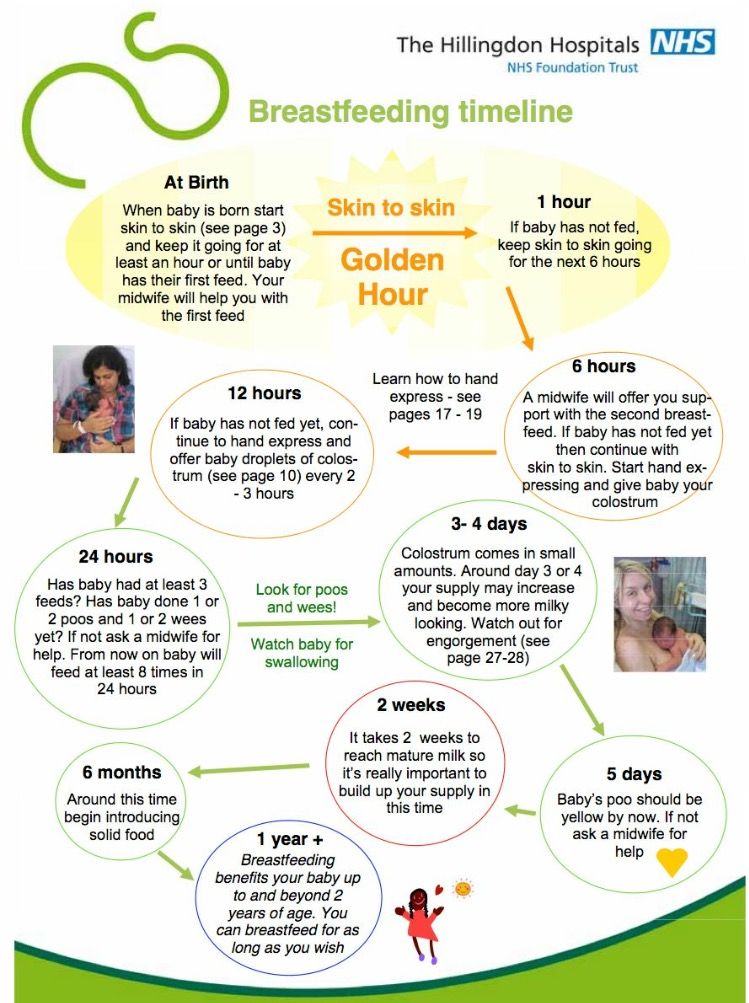
Breastfeeding: How Much and How Often?
As babies get older, they will start to breastfeed less often and sleep for longer periods at night. Your infant probably is eating enough if he or she:
- seems alert, content, and active
- is steadily gaining weight and growing
- feeds six to eight times per day
- is wetting and soiling diapers on a regular basis
Babies might not be eating enough if they:
- don't appear satisfied
- cry constantly
- are irritable, even after feeding
- are not making wet diapers
Call your doctor if you're concerned your baby isn't eating enough.
A few weeks after birth, breastfed babies tend to have fewer bowel movements (BMs, or poop) than they did before. At around 2 months of age, your baby may not poop after each feeding, or even every day. During growth spurts, you may notice that your little one wants to feed more often.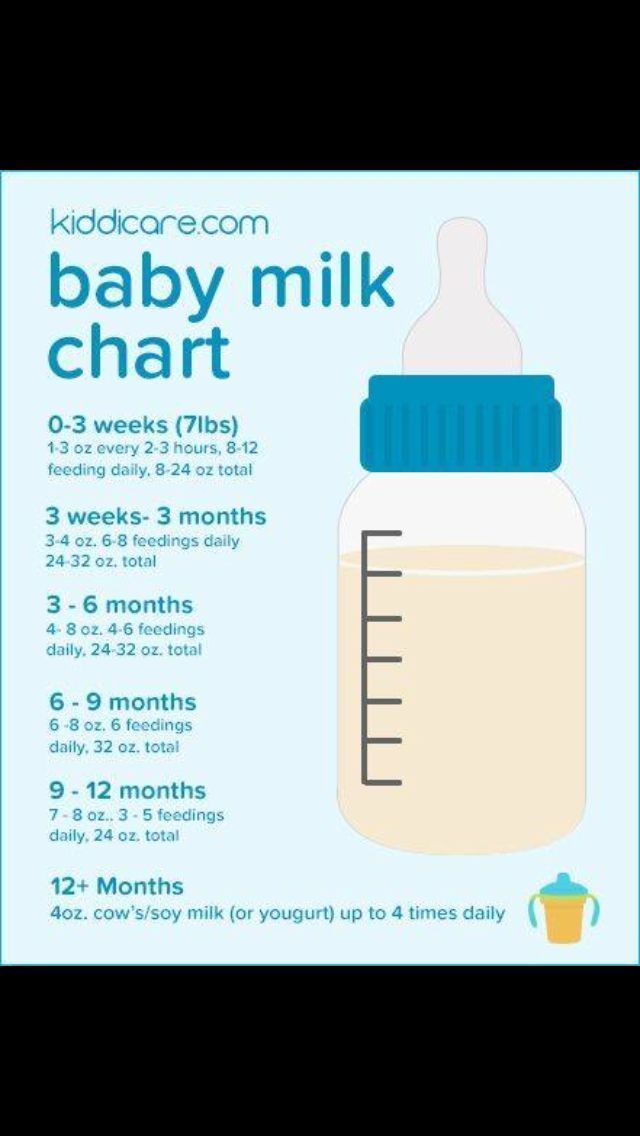 This frequent nursing sends a signal to make more milk. Within a couple of days, supply and demand will get into balance.
This frequent nursing sends a signal to make more milk. Within a couple of days, supply and demand will get into balance.
Babies who get breast milk only should get vitamin D supplements within the first few days of life. Other supplements, water, juice, and solid foods aren't usually needed.
Formula Feeding: How Much and How Often?
Babies digest formula more slowly than breast milk, so if you're bottle-feeding, your baby may have fewer feedings than a breastfed infant.
As babies grow, they can eat more at each feeding and may go for longer stretches between feedings. You'll also notice that your baby is starting to sleep longer at night.
During the second month, infants may take about 4 or 5 ounces at each feeding. By the end of 3 months, your baby may need an additional ounce at each feeding.
It's easy to overfeed a baby when using a bottle because it easier to drink from a bottle than from a breast. Make sure that the hole on the bottle's nipple is the right size.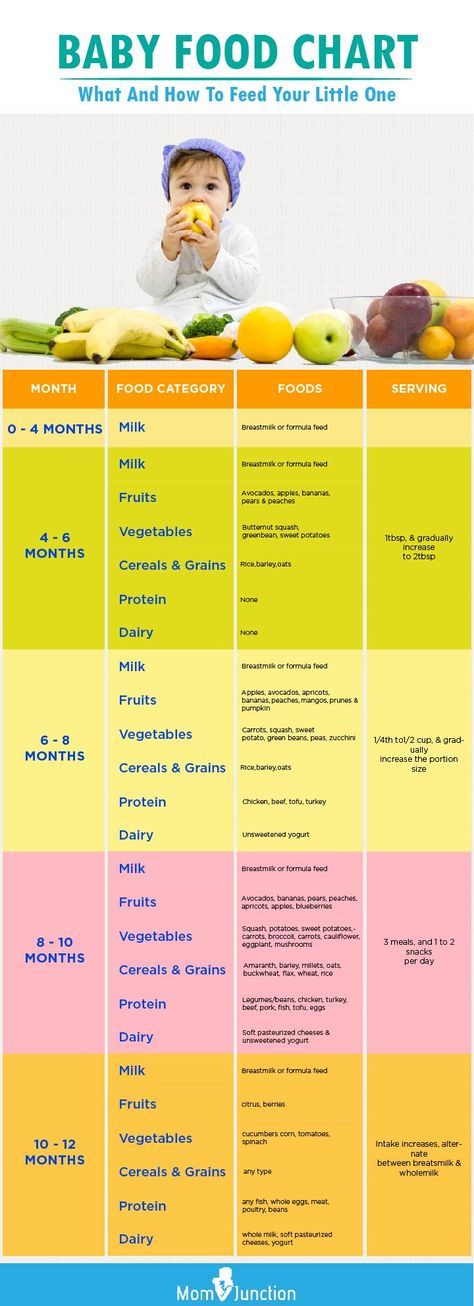 The liquid should drip slowly from the hole and not pour out. Also, resist the urge to finish the bottle when your baby shows signs of being full.
The liquid should drip slowly from the hole and not pour out. Also, resist the urge to finish the bottle when your baby shows signs of being full.
Never prop a bottle. Propping a bottle might cause choking and it increases the chances of getting ear infections and tooth decay.
Should I Worry About Spitting Up?
It's normal for infants to "spit up" after eating or during burping. Spitting up a small amount — usually less than 1 ounce (30 ml) — shouldn't be a concern as long as it happens within an hour of feeding and doesn't bother your baby.
You can reduce spitting up in these early months by:
- feeding before your baby gets very hungry
- keeping your baby in a semi-upright position during the feeding and for an hour after
- burping your baby regularly
- avoiding overfeeding
- not jostling or playing vigorously with your baby right after a feeding
If your baby seems to be spitting up large amounts, is spitting up forcefully, is irritable during or after feedings, or seems to be losing weight or is not gaining weight as expected, call your doctor. And if your child has a fever or shows any signs of dehydration (such as not wetting diapers), call the doctor right away.
And if your child has a fever or shows any signs of dehydration (such as not wetting diapers), call the doctor right away.
Call your doctor if you have any questions or concerns about feeding your infant.
Reviewed by: Mary L. Gavin, MD
Date reviewed: November 2021
Learning, Play, and Your 1- to 3-Month-Old (for Parents)
Reviewed by: Mary L. Gavin, MD
en español Aprendizaje, juego y su hijo de 1 a 3 meses
After learning to recognize your voice, your face, and your touch, and to associate them with comfort, your baby will start responding even more to you during these months — and will even give you a smile!
Babies this age spend more time awake and become more curious about their surroundings. They are getting stronger and starting to coordinate movements. Encourage the learning process by talking to your little one, responding to any vocal expressions, and providing colorful age-appropriate toys.
What Is My Baby Learning?In the first month or two of life, newborns depend on others to lead interaction.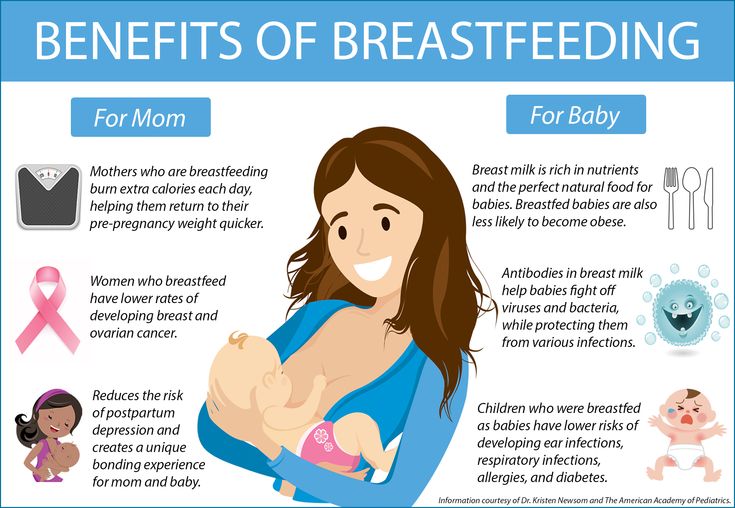 But by the end of the third month, your baby will engage you with facial expressions and vocalizations. You'll begin to see your baby's personality emerge!
But by the end of the third month, your baby will engage you with facial expressions and vocalizations. You'll begin to see your baby's personality emerge!
Your baby will carefully watch your facial expressions and listen to your voice, responding to you with sounds and gurgles. At around 2 months, babies seem happy to see caregivers and smile when they talk or smile at them.
Babies also start to open and shut their fists. This means they may be able to hold a rattle placed in their hands. They'll soon discover that they're the ones that make the rattle make noise!
How Can I Help My Baby Learn?Respond to coos and gurgling with sounds of your own. Encourage your baby to keep “talking.” In this way, your little one learns about language and back-and-forth conversation.
Provide colorful toys of different textures, shapes, and sizes for your baby to hold and explore. This is a good age to introduce an infant gym with interesting objects that dangle for your baby to swat at.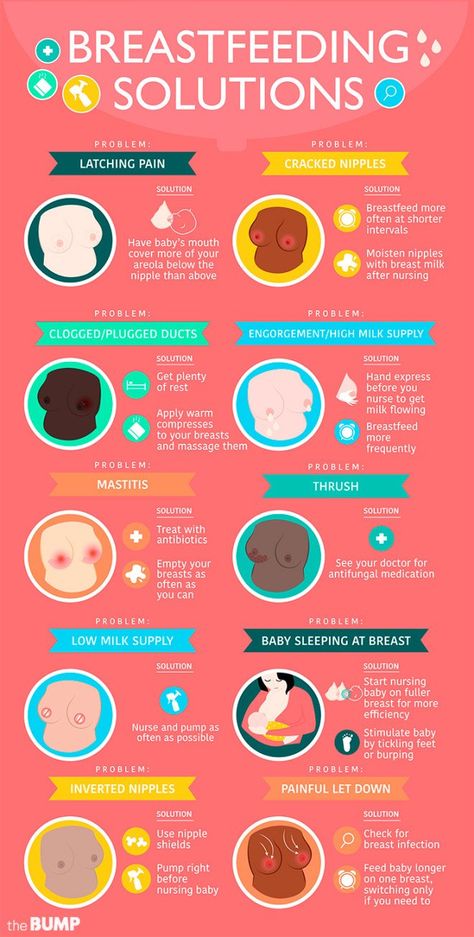 Or hold a toy just out of reach for your baby to reach for, swat, and try to grab hold of. But don't string up toys on cribs or other baby equipment — your baby could get tangled in them.
Or hold a toy just out of reach for your baby to reach for, swat, and try to grab hold of. But don't string up toys on cribs or other baby equipment — your baby could get tangled in them.
Watch for signs — fussing, squirming, or crying — that your little one might be ready for a break.
How Can I Help My Baby Play?Other ideas for encouraging your baby to learn and play:
- Gently clap your baby's hands together or stretch arms (crossed, out wide, or overhead).
- Gently move your baby's legs as if pedaling a bicycle.
- Use a favorite toy for your baby to focus on and follow, or shake a rattle for your infant to find.
- Make different facial expressions for your baby to imitate.
- Talk to your baby and let your baby respond.
- Read to your baby.
- While awake, let your baby spend some time lying on the tummy to help strengthen the neck and shoulders. Always supervise your infant during "tummy time" and be ready to help if they get tired or frustrated in this position.
 Never put a baby to sleep on their stomach. Infants should sleep on their backs to reduce the risk of sudden infant death syndrome (SIDS).
Never put a baby to sleep on their stomach. Infants should sleep on their backs to reduce the risk of sudden infant death syndrome (SIDS).
There is a wide range of normal development, so some children may gain skills earlier or later than others.
Talk to your doctor if you have any concerns about how your baby sees and hears, or if you have any questions or concerns about your baby's development.
Reviewed by: Mary L. Gavin, MD
Date reviewed: May 2022
Breastfeeding with pierced, flat or inverted nipples
The shape and size of nipples can vary greatly from woman to woman. Our practical tips will help you make breastfeeding easier, no matter what your nipples are.
Share this information
Most women's nipples protrude, enlarge and swell when touched, but some have flat or even inward nipples. In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
“Don't panic if you have flat or inverted nipples. As a rule, this does not interfere with breastfeeding in any way,” says Shawnad Hilton, a lactation consultant, health visitor and newborn care specialist who has worked with Medela in the UK for more than a decade. “Remember that your baby takes into his mouth not only the nipple, but also part of the breast.”
However, in the early days, when the baby's mouth is still very small and suckling skills have not developed, inverted or flat nipples can make feeding difficult, especially if the baby is unwell or born prematurely.
“Flat or inverted nipples may not reach the baby's palate and therefore not trigger the sucking reflex,” Schoned explains. “That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk.”
How to tell if you have flat or inverted nipples
Flat nipples 1 do not protrude much from the areola (the darker
area surrounding the nipple) even when stimulated.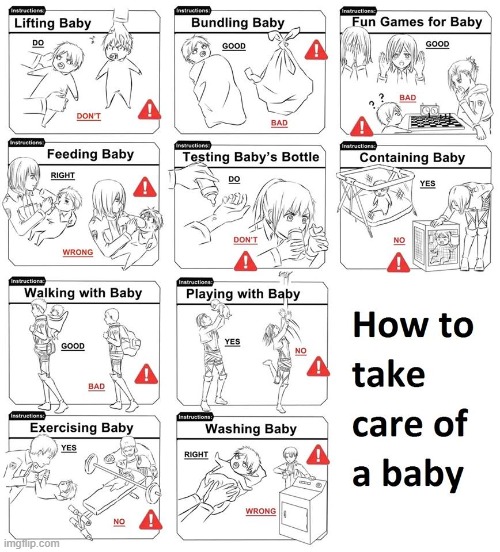
Inverted nipples seem to be recessed in the center. They may look like this all the time or only if they are stimulated. Sometimes inverted nipples are on the same level with the areola, and sometimes even sink deep into the breast tissue.
This feature may occur on one or both nipples. It is estimated that approximately 10% of nulliparous women have at least one retracted nipple. 2 If you're not sure what type of nipples you have, try a simple pinch test: Gently squeeze your breast with your thumb and forefinger on both sides of the areola. The nipple should come forward. If your nipple hides inside, creating a depression, then it is retracted.
Preparing inverted and flat nipples during pregnancy
You may have noticed that during pregnancy your breasts have changed and your nipples have become more protruding. If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
“In a normal pregnancy, nipple formers can be worn from 32 weeks,” advises Schoned. - Start wearing them for an hour a day, gradually increasing the time to eight hours. If you have an incompetent (weakened) cervix or are at risk of preterm labor, check with your healthcare provider about when you can start using shapers, as nipple stimulation can trigger contractions.”
“Nipple formers can continue to be worn after childbirth,” adds Schoned. “Try to put them in a bra 30 to 60 minutes before feeding.”
“I have inverted nipples, and after two or three weeks of constantly trying to latch on, I almost switched to formula,” recalls Nina, a mother from Germany. “I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old. ”
”
How to help your baby latch on to flat or inverted nipples
If your baby enjoys sucking on your thumb but isn't as interested in your breast, chances are your nipple isn't reaching the palate. The baby may become nervous, push off the breast and cry or even fall asleep on your chest. If this happens, ask a lactation consultant or healthcare professional to check the grip.
There are several tricks you can use before every feed to make your nipples more comfortable to latch on to. Schoned recommends the following:
- twist the nipple between thumb and forefinger so that it protrudes better;
- place fingers in a "V" or "C" shape and squeeze the breast just behind the areola to push out the nipple;
- apply a cold compress or ice cube to the nipple to push it forward;
- Express milk manually or with a breast pump for a couple of minutes before feeding so that the nipple comes out more.
“I had a flat nipple, but I only found out about it when I noticed Austin was having trouble suckling on that side,” says Jennifer, mother of two in the UK.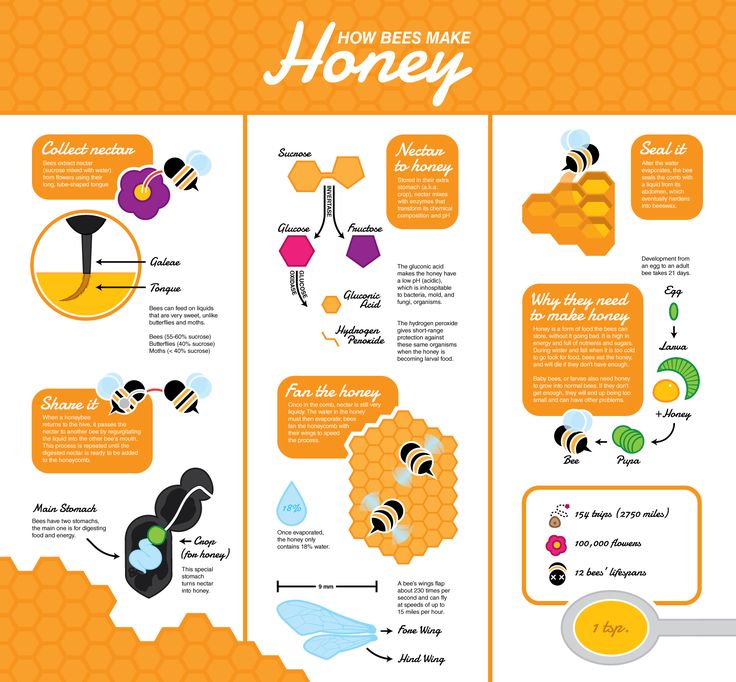 “From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.”
“From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.”
Using nursing pads
If none of the above work and your baby still has difficulty latch-on, your lactation consultant or healthcare professional may recommend that you breastfeed with a nursing pad*. They are thin and flexible nipple-shaped silicone funnels with holes at the tip through which milk will flow.
It is easier for the baby to put the feeding pad in his mouth, as it is larger and more rigid. In addition, such an overlay will reach him to the sky, causing a sucking reflex. Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
Over time, as your baby learns to suckle properly and your nipples get used to feeding, you will be able to breastfeed without the pads.
“My nipples are rather flat. The doctor advised me breastfeeding pads, and I was successfully able to feed my two babies,” says Ann-Sophie, mother of two from Sweden. “My secret is to make them adhere better to the skin, I lightly wet the edges before use.”
Breastfeeding with pierced nipples
Many women with pierced nipples find it does not affect their ability to breastfeed. However, jewelry must be removed before feeding, as the child may choke on them or injure their tongue, gums or palate.
“I had a nipple piercing, but I got it off a year later when I got pregnant because my breasts were very sensitive,” says Kelly, mother of three from the UK. “I breastfed my daughter exclusively, and then her two younger brothers, and never had any problems. And the pierced nipple was my favorite!”
And the pierced nipple was my favorite!”
Some women report that milk can leak from piercings, while others believe that piercing scars reduce milk production 4 - but this has not been well researched.
“You can't predict how a piercing will affect breastfeeding until milk production begins,” Schoned explains. - If you are concerned, talk to a lactation consultant or healthcare professional. And remember that one breast may be enough for babies to get the nutrition they need if there are problems with the second. ”
What to do if you can't breastfeed with flat or inverted nipples
If you've tried all the options and still can't breastfeed, you still shouldn't deprive your baby of breastmilk.
“Mom and baby's health is the most important thing,” says Schoned. “Maybe you should switch to full pumping and feed your baby only expressed milk. You can also try the supplementary feeding system** where the baby continues to feed at the breast while receiving additional expressed milk through a tube. That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more.
That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more.
“I have inverted nipples. After the disastrous experience of breastfeeding my first son with my second, I decided to get my way after all,” says Babettli, mother-of-two from Italy. - On the advice of experts, I tried nipple formers and nursing pads, but everything was unsuccessful. In the end, pumping with the Medela Symphony*** Double Electronic Clinical Breast Pump proved to be the best solution for us. I fed exclusively on expressed milk for up to four months.”
Care for different types of nipples
Flat or inverted nipples may require extra care as the baby may squeeze them harder and they may become inflamed at first. Tips on how to care for sore nipples can be found in Nursing Nipple Care.
If your nipples become inverted after a feed, any moisture can lead to inflammation and increase the risk of infections, including thrush. Blot your nipples dry after each feed before they have time to hide inside.
Blot your nipples dry after each feed before they have time to hide inside.
With swelling of the mammary glands, when even protruding nipples can become flat, flat or inverted nipples can be difficult. Read the helpful tips in the article on breast swelling.
The good news is that continuous breastfeeding or pumping can change the shape of your nipples and breastfeeding will become easier over time. With the arrival of the next child, you may not have to face this problem at all, as happened with Leanne, a mother of two from the UK.
“The second feeding was like a fairy tale,” she says. “After almost four months of pumping for my first son, my flat nipples were so extended that with my second son I no longer had to use breast pads - he was able to suck directly from the breast. The youngest is now nine months old and I still breastfeed him.”
Literature
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing ; 2015.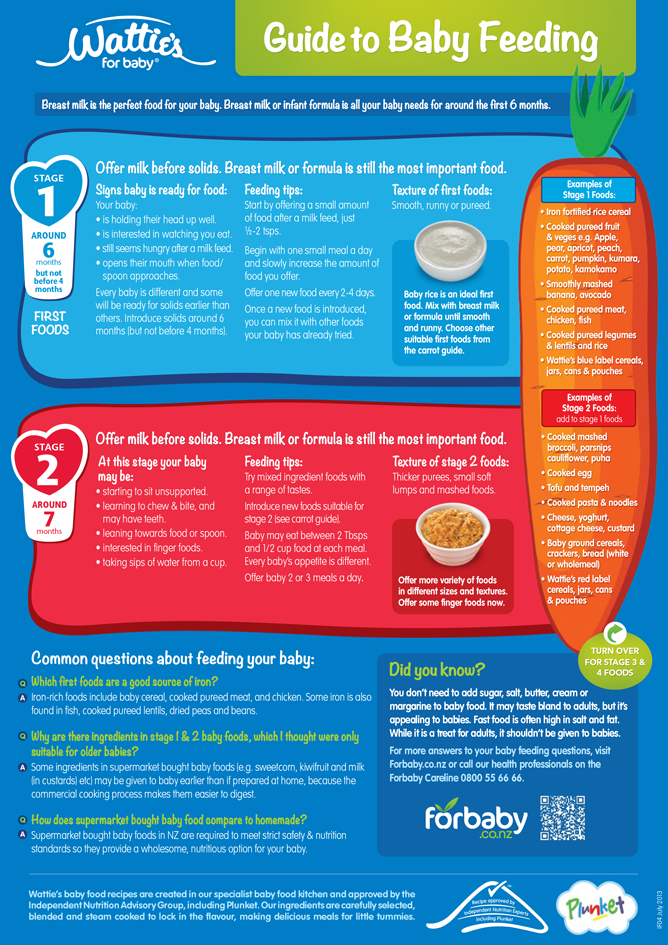 - Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
- Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast . 1997;6(2):72-78. — Alexander JM, Campbell MJ, "Prevalence of inverted and intractable nipples in pregnant women who intend to breastfeed." Ze Brest (Chest). 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature.Breastfeeding Medicine. 2010;5(6):309-314. — McKechnie A.S., Eglash A., "Nipple Covers: A Review of the Literature". Brestfeeding Medicine (Breastfeeding Medicine). 2010;5(6):309-314.
4 Garbin CP0106 , Rowan MK , Hartmann PE , Geddes DT . Association of nipple piercing with abnormal milk production and breastfeeding. JAMA, Journal of the American Medical Association. 2009;301(24):2550-2551. - Garbin S.P., Deacon J.P., Rowan M.C., Hartmann P.I., Geddes D.T., "Nipple piercing and its impact on abnormal milk production and breastfeeding", JAMA (Journal of the American medical association). 2009;301(24):2550-2551.
Association of nipple piercing with abnormal milk production and breastfeeding. JAMA, Journal of the American Medical Association. 2009;301(24):2550-2551. - Garbin S.P., Deacon J.P., Rowan M.C., Hartmann P.I., Geddes D.T., "Nipple piercing and its impact on abnormal milk production and breastfeeding", JAMA (Journal of the American medical association). 2009;301(24):2550-2551.
Read instructions before use. Consult a specialist about possible contraindications.
* RC No. FSZ 2010/07352 dated 07/19/10
** RC No. FSZ 2010/07353 dated 07/19/10
*** RC No. FSZ 2010/06525 dated 03/17/2021 9003 How to get help with breastfeeding | help with breastfeeding
Many mothers need help with breastfeeding, especially in the first days after giving birth. Where can you get it?
Share this information
Some mothers breastfeed easily, but many need help. There are many ways to avoid problems and start breastfeeding successfully.
Before the birth of a child
Every expectant mother would do well to take courses for pregnant women. In these courses, you will learn the importance of skin-to-skin contact in triggering milk production and receive other helpful breastfeeding tips. The course leader can provide you with a list of local lactation consultants and breastfeeding support groups. If the manager does not have this information, find out about local specialists, hotlines and support services yourself.
Be sure to include breastfeeding and early skin-to-skin contact with your baby in your birth plan. It is important that the medical staff is aware of your wishes.
Who can provide breastfeeding support?
Seek help immediately after giving birth if you need it. Small problems can quickly turn into big ones, but most of them are easy to fix if you take action right away.
Medical professionals such as obstetricians, nurses and physicians often have basic breastfeeding training. If you have more complex problems, you should contact professionals with a narrow specialization. These are lactation consultants (including self-help and breastfeeding support professionals).
If you have more complex problems, you should contact professionals with a narrow specialization. These are lactation consultants (including self-help and breastfeeding support professionals).
Self-help members
These are mothers who have experienced breastfeeding and have been trained to help with common problems. They can assess whether the baby is latching on well and getting enough milk. If the grip is wrong, they can suggest a more comfortable position for feeding. For more serious problems, they can recommend a qualified technician.
Breastfeeding Support Specialists
Breastfeeding support professionals (eg, La Leche Liga, AKEV) have more knowledge and can help with more serious problems, such as if the baby is not gaining enough weight or does not want to latch on.
Lactation Counselors
The Lactation Counselor helps with more complex problems. It can diagnose insufficient milk production and assist with breastfeeding premature babies.
What problems can experts help with?
Here are some of the most common breastfeeding problems and links to detailed articles on them.
Latching problems
Ideally, a newborn baby will be able to latch on by himself in the first few hours of life. If this does not happen, or if the latch makes you uncomfortable, the obstetrician or self-help member can check that you are properly latching on to your baby. If the maternity hospital has already performed such a check, but the problem has not been solved, do not hesitate to ask for it again. If the baby does not take the breast after a day, and you have already been discharged from the hospital, contact a consultant for further support. Read more in the article on the correct grip on the chest.
Sore nipples
This problem is almost always due to the fact that the baby does not latch on properly. A member of the self-help movement or a breastfeeding support specialist will suggest a better position for the baby. If you experience severe pain or inflammation that does not go away even after changing position, seek the help of a consultant to find out the cause. Read more in the article about sore nipples.
If you experience severe pain or inflammation that does not go away even after changing position, seek the help of a consultant to find out the cause. Read more in the article about sore nipples.
Breast swelling
The best way to avoid breast swelling (a condition that occurs on the second or fourth day after delivery, when the breasts fill up and harden with incoming milk) is to feed your baby often. Your lactation consultant will teach you how to massage your breasts and how to express milk manually or with a breast pump to help relieve discomfort. If you are unable to breastfeed your baby due to swelling of the mammary glands, you should consult an obstetrician. Read more in the article about swelling of the mammary glands.
Problems with milk production
Many mothers in the first days after giving birth worry that they are not producing enough milk. A self-help member, obstetrician or nurse will help you calm down and explain that during this period it is perfectly normal for a child to ask for a breast every one to two hours.