Is it normal for my baby to vomit after feeding
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
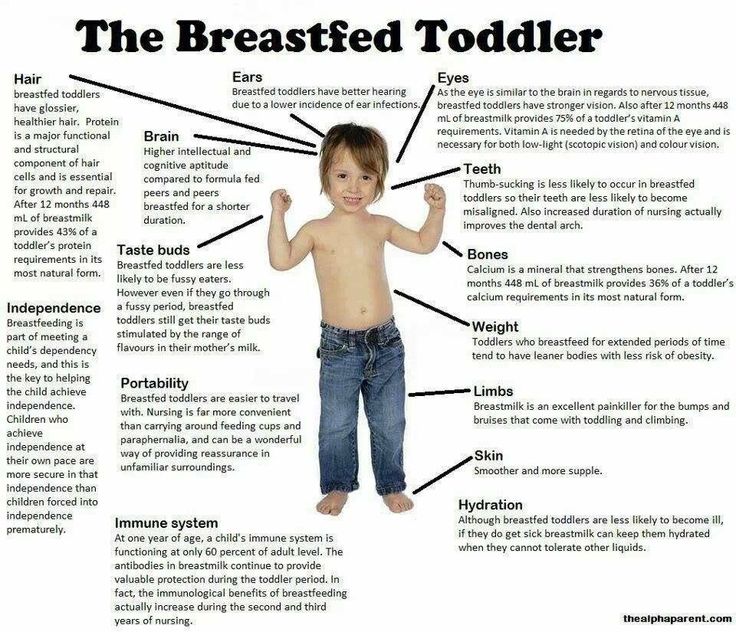
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
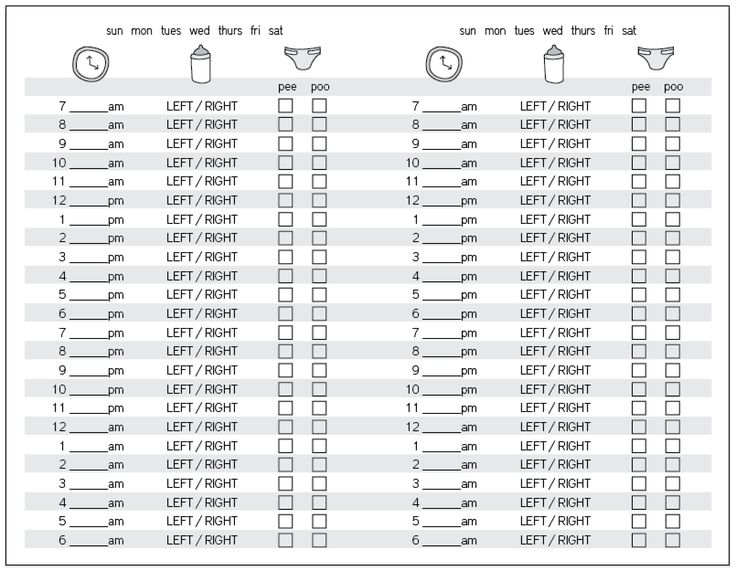
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug. Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant. Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting. Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Vomiting in babies | Pregnancy Birth and Baby
beginning of content5-minute read
Listen
From birth to 12 months, babies are known to vomit — it’s just one of their design features. However, as normal as vomiting is, it can also be worrying for parents. Occasionally, vomiting can be a sign of illness or complications, but for most babies, vomiting and reflux occurs simply because their guts are still developing.
However, as normal as vomiting is, it can also be worrying for parents. Occasionally, vomiting can be a sign of illness or complications, but for most babies, vomiting and reflux occurs simply because their guts are still developing.
What are the different types of vomiting
There are a few different types of vomiting and although the result is the same, the reasons are different:
- Possetting is the name for small amounts of milk brought up after a feed.
- Reflux happens when the valve at the top of a baby’s stomach is not tight enough to keep milk in there. A baby’s oesophagus (food pipe) is short, so when the valve opens and there’s only a short distance between it and their mouth, vomiting can occur.
- Projectile vomiting is vomiting with force. Projectile vomiting can be a symptom of a blockage at the outlet of a baby's stomach. If it's happening after most or all feeds, take your baby to a doctor.
What causes babies to vomit?
Generally, mild vomiting occurs because a young baby is still getting used to feeding on, digesting and eliminating milk.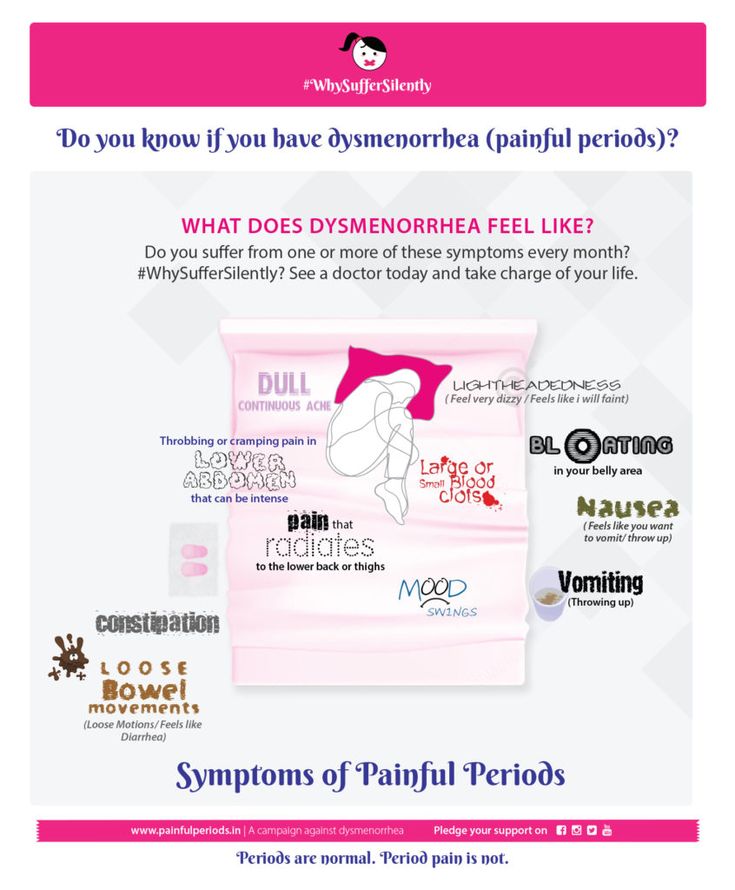 On average, a newborn baby’s stomach can hold around 20 millilitres, so it doesn’t take much milk for them to fill up and vomit the excess.
On average, a newborn baby’s stomach can hold around 20 millilitres, so it doesn’t take much milk for them to fill up and vomit the excess.
How can I tell if my baby is sick?
Vomiting by itself can be reassuring. However, if your baby has a temperature, is not feeding well, has diarrhoea or a rash, or experiences any other symptoms, your baby needs to see a doctor. If your baby seems healthy and well and is bright and alert, you may just want to monitor their vomiting to see when and how often it happens — but note that the amount that a baby vomits can be hard to work out and may seem larger than it really is.
What’s the difference between vomiting and reflux?
Vomiting caused by reflux generally occurs after feeding. It can seem effortless or cause pain. Some babies with reflux constantly 'spill' after and in-between their feeds. It’s important to think about how your baby’s vomiting affects them. If your baby seems happy, is thriving and gaining weight, you could simply try changing the frequency and amount of feeds you give them. If your baby seems to be in pain and/or not thriving, take them to a doctor. Sometimes medication is necessary for reflux.
If your baby seems to be in pain and/or not thriving, take them to a doctor. Sometimes medication is necessary for reflux.
Does breast or formula feeding cause more vomiting?
Breastfed babies can vomit as much as babies who are formula fed. There's no real difference between the two. Generally, the only difference is that feeding on formula makes a baby’s vomit smell and look different to that after feeding on breastmilk.
Can solids cause vomiting?
Some babies take time to adjust to digesting solid foods. They can vomit more when solids are introduced. This can occur because of overfeeding. Their stomachs are simply too small to accommodate extra volume. Start small when introducing solids — around 1-2 teaspoons of solids are ideal.
Is vomiting a sign of allergies?
Some allergies can cause vomiting, especially allergies to cow's milk. Your baby can react to particular foods or ingredients if they’re sensitive to them. Your doctor can help guide you to decide which foods are best for your baby.
How can I treat my vomiting baby?
Most babies recover quickly after vomiting and don't need any specialised care. They can seem hungry again straight away or take a while to want to feed again. However, if they vomit a lot and have other symptoms, a doctor needs to assess them.
Generally, babies are not given medication for vomiting unless they can’t keep any milk or fluids down. Dehydration is generally managed by giving intravenous fluids.
Sometimes changing feeding positions and frequency can reduce the likelihood of vomiting. It's still important to always follow the safe sleeping guidelines when settling your baby, even if they vomit. Back sleeping is protective against choking.
When should you see a doctor?
You should take your baby to see your doctor if:
- you are concerned about your baby's vomiting
- your baby is showing other signs of illness
- your baby seems lethargic, sleepy and not interested in feeding
- your baby is losing weight and not thriving
- there is blood or bile in their vomit
- their vomiting isn’t stopping or getting worse
Sources:
Raising Children (Vomiting), Red Nose Australia (Will baby choke if he/she vomits while sleeping on the back?), Safer Care Victoria (Vomiting in neonates), The Royal Australian College of General Practitioners (The vomiting child)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Vomiting in children
- Reflux
- How to know when your baby is well - video
- Knowing your baby is well - podcast
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein.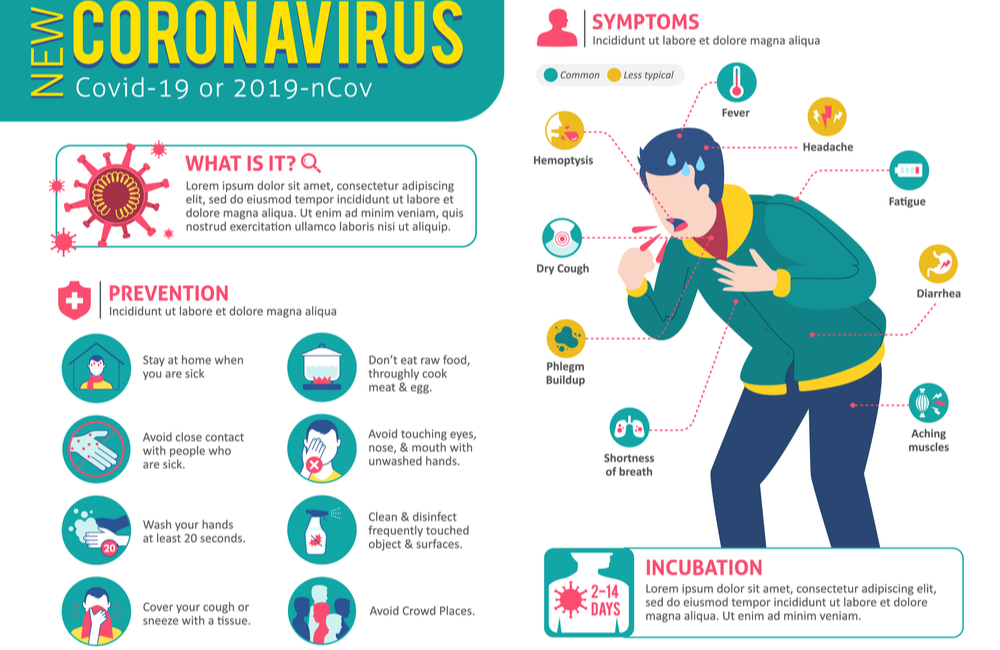 With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause. To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
Why does the baby spit up after feeding?
search support iconSearch Keywords
Regurgitation is a common condition in newborns and infants and is most often a normal variant. However, it is not uncommon for parents to worry if their baby is spitting up frequently, believing that it is due to nutritional or health problems in general. Sometimes these fears are not unfounded, and regurgitation really has a pathological origin. What is its cause and when should you really consult a doctor about this?
Regurgitation — Return of a small amount of food (uncurdled or partially curdled milk) from the stomach up the digestive tract: into the esophagus and further into the oral cavity. According to statistics, at least 1 time during the day can spit up at least 50% of babies from 0 to 3 months, more than 60% of children 3-4 months, and 5% of children spit up until the year 1 .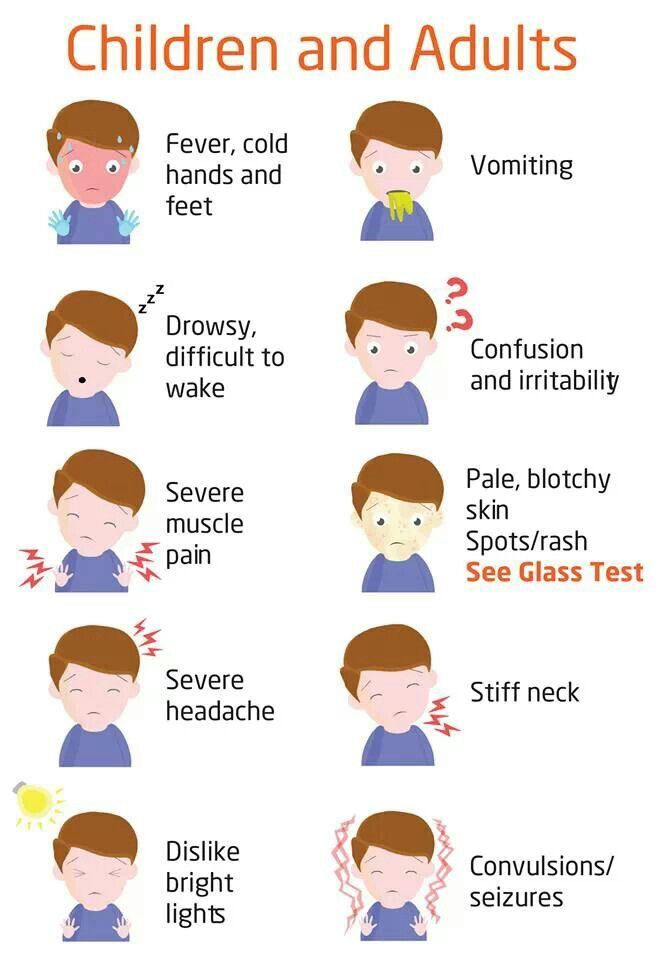
Regurgitation in newborns is considered a physiological process. It is caused by a number of factors, including:
- Features of the structure of the upper digestive tract in babies
- In newborns and infants up to a year of age, the stomach has a spherical shape. It holds a small amount of food, besides, the release from it into the duodenum is slower in comparison with children after the year 2 .
- Weakness of the lower esophageal sphincter that separates the esophagus from the stomach
- Normally, the lower esophageal sphincter should tightly “close” the esophagus, allowing food to pass into the stomach and not allowing it to enter back into the upper digestive tract. However, in young children (up to a year), the muscles of the esophageal sphincter are poorly developed, and it does not do its job very well 2 .
- Slow movement of food through the gastrointestinal tract
- The neuromuscular apparatus of newborns is immature.
 It does not ensure the proper movement of food through the esophagus, causing regurgitation.
It does not ensure the proper movement of food through the esophagus, causing regurgitation.
One of the important risk factors contributing to the appearance of regurgitation in newborns is aerophagia. This is the swallowing of large amounts of air during feedings. This happens when the baby is not properly attached to the breast, the mother has a lack of breast milk, or the bottle is in the wrong position in the child who receives the mixture. The size of the opening in the nipple also matters - if it is too large, the newborn swallows a lot of air 3 .
With aerophagia, the baby becomes capricious, restless immediately after feeding. Noticeable bloating. If the baby spits up immediately after a feed, the milk (or formula) remains practically fresh, uncurdled 3 .
Promotes post-feeding regurgitation and predominantly horizontal position of the baby during the day, combined with relatively high intra-abdominal pressure 4 . Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Regurgitation in many newborns can be triggered by other situations in which pressure in the abdominal cavity increases and stomach contents are thrown into the esophagus, in particular 3 :
- tight swaddling;
- stool disorders, in particular constipation;
- long, forced cry and some others.
Want to avoid common feeding problems?
Start with a baby bottle with an anti-colic system that helps you avoid common feeding problems such as colic, gas and spitting up*
How can you tell the difference between normal spitting up and vomiting?
Sometimes regurgitation is considered a manifestation of disorders in the digestive tract of children. Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
If the mother is worried that her baby is spitting up, keep track of when this happens and count the total number of spit ups per day. Normally, regurgitation usually occurs after eating (the child burps after each feeding), lasts no more than 20 seconds and repeats no more than 20-30 times a day. With pathology, the problem manifests itself at any time of the day, regardless of when the baby was fed. Their number can reach 50 per day, and sometimes more 1 .
The amount of discharge during regurgitation also matters. With normal, physiological regurgitation, it is approximately 5 - 30 ml. If this volume fluctuates between 50 and 100 ml, it is already defined as profuse vomiting. When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
Vomiting in babies is a warning sign. Doctors are especially alarmed by repeated vomiting, a fountain, with an admixture of bile, in combination with constipation. Vomiting can lead to the development of dehydration, acid-base imbalance and other consequences, therefore, if it occurs, you should urgently contact a pediatrician to find out the cause and begin treatment. A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
Physiological regurgitation: symptoms
Regurgitation in newborns, which is considered normal and not of concern to pediatricians 3 :
- usually continues for a certain period of time;
- is characterized by slow, "passive" leakage; if the baby spits up a fountain, it is better to consult a doctor;
- has a sour smell of curdled milk;
- occurs without the participation of muscles - the baby does not strain during regurgitation;
- does not affect the general well-being of the baby.

How to help a newborn who spit up often?
If the baby is healthy, no medication is prescribed for spitting up. To help the child allow simple measures based on lifestyle changes and feeding.
. To improve the situation, it is recommended to feed the baby more often, avoiding oversaturation, best of all - on demand 5 . The AirFree valve prevents air from entering the baby's stomach. To allow air that has entered the digestive tract during meals to escape, it is important to keep the newborn upright for 10-20 minutes after feeding 4 . To reduce the negative impact of the acidic contents of the stomach on the esophagus, it is necessary to put the baby to sleep in the supine position. The side or prone position, which many pediatricians used to recommend, is no longer recommended. It was found to be associated with an increased risk of sudden infant death syndrome 5 . If parents notice alarming symptoms, such as spitting up too often or large volume, etc., it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy. 1 Zakharova I. Nagornaya 2904 V., Limarenko M. P., Logvinenko N. G. Experience with the use of domperidone in suspension in young children with regurgitation syndrome // Child Health, 2013. No. 5 (48). 3 Zakharova IN Regurgitation and vomiting in children: what to do? //Pediatrics. Supplement to Consilium Medicum, 2009. No. 3. S. 58-67. 4 Zakharova I. N., Sugyan N. G., Pykov M. I. Regurgitation syndrome in young children: diagnosis and correction // Effective pharmacotherapy, 2014. No. 3. P. 18-28. 5 Vandenplas Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) //Journal of pediatric gastroenterology and nutrition.
Every feeding, the mother must ensure that the baby does not swallow too much air during suckling. When sucking, there should be no loud, smacking, clicking sounds. You also need to control that the baby captures the nipple along with the areola.
If the newborn is bottle-fed and receiving formula, it is important to choose the right bottle and nipple. The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air New Anti-colic bottle with AirFree valve
References  N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. V. 7. No. 4.
N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. V. 7. No. 4.