Lactose intolerance foods for babies
Lactose Intolerance in Infants & Children: Parent FAQs
By: Anthony Porto, MD, MPH, FAAP
It can be difficult to know whether your infant or child is having symptoms of lactose intolerance or whether he or she may have a milk allergy.
The following frequently asked questions from parents will help you learn more about the common symptoms of lactose intolerance, diagnosis, and treatment options.
Is lactose intolerance the same thing as a milk allergy?
No. Many parents confuse the terms lactose intolerance and milk allergy. While they may share similar symptoms, they are entirely different conditions. Lactose intolerance is a digestive problem, while milk allergy involves the immune system. So, while lactose intolerance can cause a great deal of discomfort, it will not produce a life-threatening reaction such as anaphylaxis.
Milk allergies tend to appear within the first year of life, while an infant's digestive system is still quite immature. Lactose intolerance can start in childhood into adolescence and can become more noticeable into adulthood.
What is lactose?
Lactose is a sugar found in foods that many children love—milk and dairy products, such as frozen yogurt and cheeses. The list of other foods containing lactose is long and includes some breads, cereals, and frozen or canned foods.
Lactose is broken down by the lactase enzyme located in the small intestine—the organ where most food digestion and nutrient absorption takes place. When we eat lactose, lactase breaks lactose down into two simple sugars: glucose and galactose. The body then absorbs these simple sugars into our intestines. When there is a decrease or loss of the lactase enzyme, we cannot break down or absorb lactose. The unabsorbed lactose can lead to symptoms, which is called an intolerance.
In addition to milk, what other food products contain lactose?
Lactose is present in many food products and in some medications. Manufacturers also often add milk and milk products to boxed, canned, frozen, packaged, and prepared foods. People who have digestive symptoms after consuming a small quantity of lactose should be aware of the many food products that may contain even small amounts of lactose.
Manufacturers also often add milk and milk products to boxed, canned, frozen, packaged, and prepared foods. People who have digestive symptoms after consuming a small quantity of lactose should be aware of the many food products that may contain even small amounts of lactose.
You can check the ingredients on food labels and the nutrition facts to find possible sources of lactose in food products. If a food label includes any of the following words, the product contains lactose:
What are some key symptoms of lactose intolerance?
The symptoms of lactose intolerance depend on the amount of lactose that's consumed. The more lactose your child consumes, the more symptoms he or she will experience. Symptoms of lactose intolerance can occur within minutes to hours after drinking milk or eating dairy products and range from mild to severe based on the amount consumed and the amount tolerated. Here are symptoms you should look out for:
Nausea
Abdominal pain, cramping, and bloating
Loose stools and gas
Watery diarrhea with gas
If I think my child might be lactose intolerant.
 How can I tell?
How can I tell?One way to check if your child has trouble digesting lactose is to take all the milk products out of your child's diet for two weeks and to then see if his or her symptoms improve. After two weeks, slowly reintroduce the products in small amounts each day to see if symptoms return. Your pediatrician can also test your child for lactose intolerance with a hydrogen breath test.
I've heard lactose intolerance can sometimes be a temporary side effect when kids are sick. Is that true?
Yes. Lactose intolerance can occur temporarily in children after a viral infection (that is why you may be told to avoid milk with lactose in it during a stomach bug) or it may be seen with conditions that lead to inflammation of the intestines, such as celiac disease.
Can infants be lactose intolerant?
Lactose intolerance is actually not very common in infants and typically only starts showing up after age three in children who were born full-term.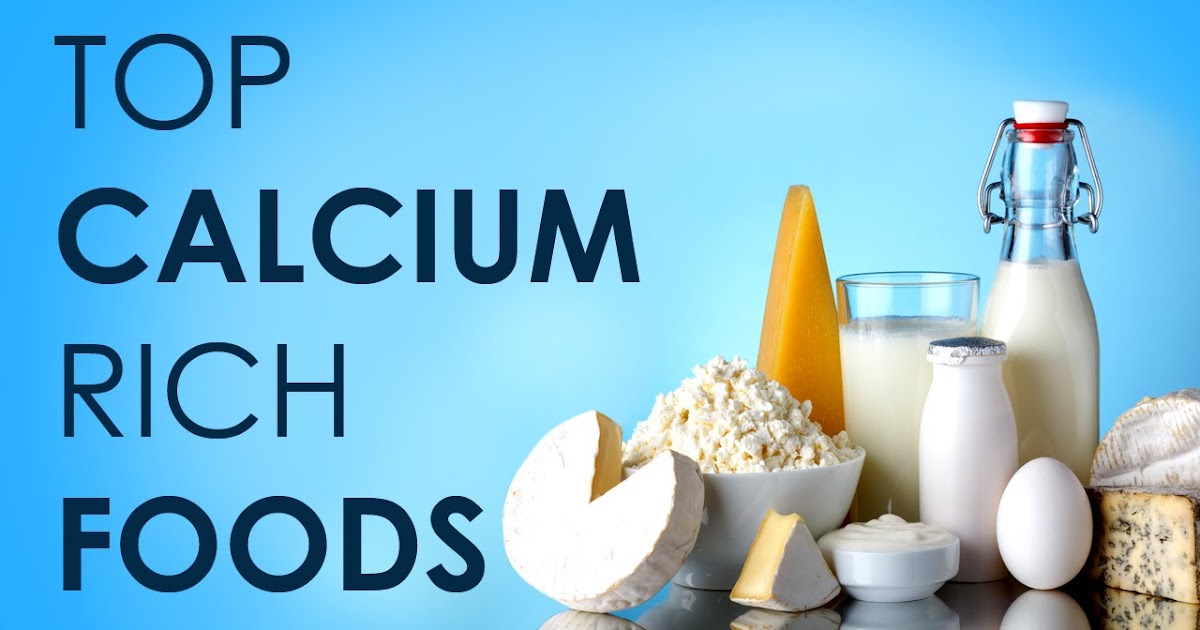 All babies are born with lactase in their intestines. As they grow older, the lactase enzyme decreases.
All babies are born with lactase in their intestines. As they grow older, the lactase enzyme decreases.
Babies who were born premature are more likely to have a type of lactose intolerance called developmental lactase deficiency. This condition usually lasts only for a short time after birth. However, the majority of premature infants will be able to consume lactose-containing formula and breast milk.
Congenital lactase deficiency is a very rare disorder in which babies can't break down the lactose in breast milk or formula. Genes inherited from parents cause this disorder. This type of intolerance results in severe diarrhea, and if not fed a lactose-free infant formula, those babies could develop severe dehydration and weight loss.
If a mother is lactose intolerant, is it safe for her to breastfeed her baby?
It's perfectly safe to breastfeed your child if you're lactose intolerant. Breastfeeding does not put your baby at greater risk of becoming lactose intolerant, and it has important health benefits for your baby.
Breastfeeding does not put your baby at greater risk of becoming lactose intolerant, and it has important health benefits for your baby.
How can my child get enough calcium in her diet if milk or lactose are reduced?
If your child has lactose intolerance, he or she can still eat lactose-free dairy products including lactose-free milk, cheese, and yogurts—all are good sources of calcium. In addition, your child can get calcium from dark green leafy vegetables such as spinach, broccoli and kale, nuts (almonds), beans (white beans), fish (sardines, salmon) and calcium-fortified orange juice. If you feel your child is not getting enough calcium, talk with your pediatrician about starting a calcium supplement.
Are soy or almond milks adequate substitutes for children who are lactose intolerant?
There are many milk substitutes that a child with lactose intolerance can drink, including soy, almond, rice, hemp, and oat milk. Soy milk is a popular milk alternative, because it is a good source of calcium and protein. Almond milk has also become a popular alternative and is safe for children with lactose intolerance or a cow's milk protein allergy. Although almond is a good source of calcium, it is lower in protein and contains fewer calories than cow's milk. Before starting any alternative milks, it is important to talk with your pediatrician about which may be best for your child.
Almond milk has also become a popular alternative and is safe for children with lactose intolerance or a cow's milk protein allergy. Although almond is a good source of calcium, it is lower in protein and contains fewer calories than cow's milk. Before starting any alternative milks, it is important to talk with your pediatrician about which may be best for your child.
How is lactose intolerance diagnosed?
Your pediatrician will take a medical, family, and diet history to help diagnose lactose intolerance in your infant or child. During this discussion, he or she will review your child's symptoms with you.
In some cases, a hydrogen breath test is done to test for lactose intolerance. For the test, your child breathes into a container that measures breath hydrogen level before and after he or she drinks a beverage that contains a known amount of lactose. Normally, only a small amount of hydrogen is detectable in the breath when a person eats or drinks and digests lactose.
 An increase in hydrogen levels is considered a positive test for lactose intolerance.
An increase in hydrogen levels is considered a positive test for lactose intolerance.Pediatricians check acidity in the stools of infants and young children who may be unable to properly do the hydrogen breath test. Acidic stool (low pH) may indicate lactose malabsorption. Another stool test (reducing substances) looks for the presence of glucose in the stool, which signifies undigested lactose.
If your child's symptoms persist, he or she may be referred to a pediatric gastroenterologist (GI) for further evaluation. Depending on the severity of your child's symptoms, the GI may perform an endoscopy to measure lactase levels directly from the intestine. This is done with a biopsy.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age. Here is a breakdown of the Recommended Dietary Allowances (RDA) for calcium and vitamin D.
How is lactose intolerance treated?
How lactose intolerance is treated depends on the extent of your child's symptoms. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
To help alleviate symptoms if/when your child consumes lactose-containing food, your pediatrician may recommend an over-the-counter lactase enzyme supplement.
If your child's symptoms are severe and warrant removing all lactose from his or her diet, your pediatrician may refer your child to a registered dietitian. Since dairy is a good source of calcium and vitamin D—which all kids need—a registered dietitian can suggest other foods to provide those nutrients and may suggest vitamin supplements.
Is lactose intolerance a lifelong condition?
In some cases, lactose intolerance is temporary—if lactose intolerance develops after a viral illness or if it is associated with other conditions, like celiac disease. For example, once celiac disease is treated, lactase levels can become in the normal range and lactose may be tolerated in the diet. More than likely, however, lactose intolerance is long-term and requires many older children and adults to alter their diet to avoid symptoms.
For example, once celiac disease is treated, lactase levels can become in the normal range and lactose may be tolerated in the diet. More than likely, however, lactose intolerance is long-term and requires many older children and adults to alter their diet to avoid symptoms.
Additional Information & Resources:
Vitamin D: On the Double
Milk Allergy
Infant Allergies and Food Sensitivities
Lactose Intolerance in Infants, Children and Adolescents (AAP Clinical Report)
About Dr. Porto:
Anthony Porto, MD, MPH, FAAP is a board certified pediatrician and board certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.
Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Lactose intolerant babies and toddlers
Read time: 8 minutes
What to know about the difference between a cow’s milk protein allergy and lactose intolerance in babies and toddlers:
What is lactose intolerance and how can it be managed in babies and toddlers?
Learn the difference between lactose intolerance and lactose overload in babies
Understand what a cow’s milk protein allergy is and how to help your baby or toddler eat while avoiding dairy.

Some babies can’t tolerate dairy, whether through the mother’s diet in breast milk, in formula, or once they’ve started solids. But how do you know if it’s lactose intolerance, a dairy allergy, or something else entirely?
Read on to learn how to figure out if your little one may be intolerant to lactose, or if their symptoms may indicate a milk protein allergy.
What is a lactose intolerance?Lactose itself is the sugar naturally found in dairy products.1 People with lactose intolerance do not have enough of the enzyme lactase, which helps the body break down and digest this milk sugar. Without lactase, bacteria break down the excess lactose, creating more fluid and gas, which is where the symptoms of lactose intolerance come from.2
Symptoms of lactose intolerance include:
Gas
Bloating, cramping, abdominal pain
Diarrhea
Nausea or even vomiting1,2
Symptoms usually show up between 30 minutes and 2 hours after having dairy. 6
6
A lack of the digestive enzyme lactase is sometimes genetic.2 Other times lactose intolerance may occur as a result of infections in the intestines or other illnesses such as Crohn’s disease, Celiac disease, or Irritable Bowel Syndrome; or as a temporary symptom of a virus your child may have.3,4
One of the most common causes of lactose intolerance, however, is the slow natural decline of lactase that happens over time.5 This may start to occur after the age of 5 years.
Premature babies born before 34 weeks may also experience temporary lactase deficiency.5 Though this normally improves fairly quickly.4
Babies born at full term usually have plenty of lactose since it is a primary component of breastmilk (just like all mammalian milks). 5,7 For this reason, lactose intolerance is generally not common in babies, but may start showing up in toddlers sometime after the age of three years.1
5,7 For this reason, lactose intolerance is generally not common in babies, but may start showing up in toddlers sometime after the age of three years.1
Read more: Is Your Baby Reacting to Something in Your Breastmilk?
Diagnosis of lactose intoleranceIf you suspect your little one has lactose intolerance, call their health care provider. Sometimes just a medical and diet history can help their doctor figure out if your baby is not able to digest lactose well.4 Other times, more tests may be needed.
Tests that may help identify lactose intolerance:
Hydrogen breath test. If your toddler is not able to digest lactose, there will be more hydrogen in their breath than usual.
Stool acidity. Taking a stool sample may help the doctor see if your little one is not digesting lactose.
 The stool will be more acidic.4
The stool will be more acidic.4
If your baby or toddler is diagnosed with lactose intolerance, the best treatment is avoiding or limiting dairy products and choosing lactose free products when they are available.2
While lactose intolerance is very rare in babies, should you feel your little one has a problem with lactose there is no need to stop breastfeeding. Simply minimize dairy in your diet and continue to breastfeed. However, keep in mind that your baby’s symptoms might actually be ‘lactose overload’ or cow’s milk protein intolerance. Keep reading to learn more about these alternate diagnoses.
For a baby on formula, you may consider a low lactose (‘sensitive’) formula to see if that is helpful. The pediatrician can help guide this decision.
The good news is that most people who are lactose intolerant can in fact continue to drink or eat a certain amount of dairy without it causing symptoms.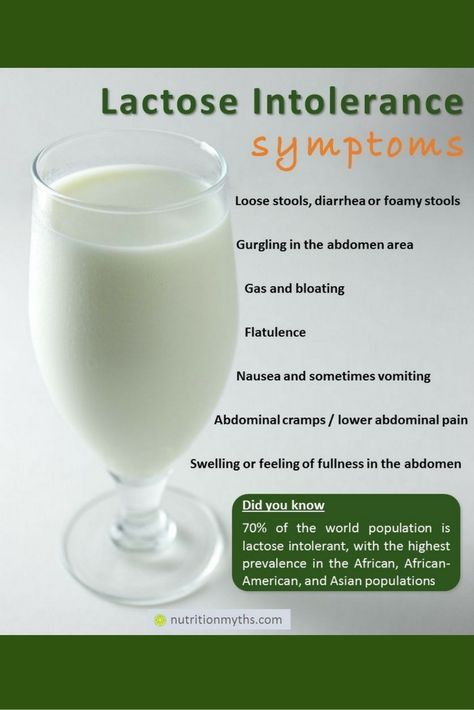 2 Some people may be able to have one serving of dairy, while others may tolerate a little more or less. Try different amounts to see if your toddler can still have a bit of dairy in their diet.
2 Some people may be able to have one serving of dairy, while others may tolerate a little more or less. Try different amounts to see if your toddler can still have a bit of dairy in their diet.
There are also dairy products that naturally have less lactose in them or are manufactured to be lactose-free which your toddler may be able to tolerate, including yogurt, cow’s milk, as well as hard cheeses such as cheddar or swiss. And of course, always be sure to provide your baby or toddler with foods in a texture they are developmentally ready to eat!
Read about: What Type of Milk Should my Toddler Drink?
What is lactose overload?Some women overproduce breastmilk, causing their little ones to take in a high volume of milk before they’re able to get a decent amount of the fat from the feed.8 This may cause something called ‘lactose overload’, or too much lactose for baby’s little tummy to digest at one time. 8
8
Many times, lactose overload is mistaken for lactose intolerance, but with some changes in breastfeeding this issue can be managed and resolved.8,9
Symptoms of lactose overload include frothy or explosive stools that are a bit smelly and more than 10 urine diapers per day.8,9 A baby with lactose overload may have good or even higher-than-average weight gain.9
Interestingly, a baby who is suffering from lactose overload may always seem hungry, even though they are gaining enough weight.9 This is because when baby is not getting enough fat, they are not registering the fullness and satisfaction that fat triggers in the brain.8
Management of lactose overloadThe most important thing is to first figure out if oversupply is the main culprit. The help of a lactation consultant will be important to get to the bottom of lactose overload.
The help of a lactation consultant will be important to get to the bottom of lactose overload.
If oversupply is the issue, the lactation consultant may recommend block feeding for a few days.8,9 This will help baby more fully empty a breast and get higher-fat feeds. Once symptoms are relieved, it’s time to go back to regular breastfeeding.9
For some mothers, the issue is not oversupply but rather feeding on a schedule or not feeding often enough.8,9 All of these may allow the breasts to fill up too much and provide baby with too much lactose and not enough fat.
Be sure to feed your little one on demand, or when baby asks to feed.11 This is normally anywhere between 8 and 12 times per 24 hours depending on baby’s age.10
Read more:
What is Breastmilk Oversupply and How to Manage it
Should I Breastfeeding On Demand or on a Schedule
What is a cow’s milk protein allergy?While lactose intolerance is rare in babies, some little ones believed to have lactose intolerance may actually have an allergy or intolerance to the cow’s milk proteins whey and casein.
A cow’s milk protein allergy (CMPA or CMA) or intolerance (CMPI) happens when the body has an overreactive immune response to the protein, triggering an allergic reaction.12 CMA is one of the most common allergies in young children, affecting about 1 to 3% of babies and toddlers.13,14
Fortunately, most children will eventually outgrow this as they get older and their digestive and immune systems mature.16
Symptoms of a cow’s milk protein allergyReactions usually happen within 1 to 2 hours after being exposed to cow’s milk protein, whether from breastmilk, formula, or from eating it in a meal.13 Reactions may range from mild to life-threatening.
In babies, symptoms of a milk protein allergy may include:
Colic, crying
Gassiness, bloating, discomfort
Eczema
Blood or mucous in the stool
Frequent stools
Vomiting16
In toddlers, symptoms of a milk protein allergy may include:
Red, itchy hives on the skin
Coughing and wheezing
Swelling of the lips, tongue, or throat
Vomiting
Anaphylaxis12,13
Anaphylaxis is a severe and potentially life-threatening allergic reaction that can occur within seconds to up to 2 hours after exposure to an allergen. 15 It can, among other things, cause a sudden drop in blood pressure and impaired breathing. If your child has known allergies, make sure you speak to your physician or allergist to get an emergency plan in place so that you are always prepared.
15 It can, among other things, cause a sudden drop in blood pressure and impaired breathing. If your child has known allergies, make sure you speak to your physician or allergist to get an emergency plan in place so that you are always prepared.
Wondering if your little one has lactose intolerance or a milk protein allergy? Reach out to our team of registered dietitians and lactation consultants for free! They’re here to help on our free to live chat from Monday – Friday 8am - 6pm (ET). Chat Now!
Diagnosis of cow’s milk protein allergyIf you feel your little one has an allergy, speak with their healthcare provider immediately. Their doctor will ask about their diet and when the symptoms tend to show up.
Tests that may help identify a milk protein allergy:
Skin prick test: usually done by an allergist
IgE test: a blood test that can help diagnose an allergy
Diet elimination: Taking out all dairy from the diet for 3 to 4 weeks to see if symptoms improve12
A diet elimination should be done with the help of a dietitian to ensure that your little one continues to get the nutrients they need for growth and development even when eliminating a food group.
Formula fed babies will likely need to switch to a non-dairy formula. Note that soy formula may or may not be a good alternative as some babies with CMA may also have a reaction to soy protein.16
When breastfeeding an infant allergic to cow’s milk protein, all dairy will need to be eliminated from your diet. When eliminating dairy, whether from your own diet or for an allergic toddler, reading labels is critical.
The following list includes some of the ingredients that indicate the presence of milk in the product:
Milk, cheese, cottage cheese, yogurt, sour cream
Lactose, lactulose, lactoferrin, lactic acid starter
Whey
Casein and caseinates
Curds
Milk by-products (like butter, ghee, and buttermilk)
Dry milk solids or powder, condensed or evaporated milk17
You may wonder how you or your child’s nutritional status may be impacted when foregoing dairy products.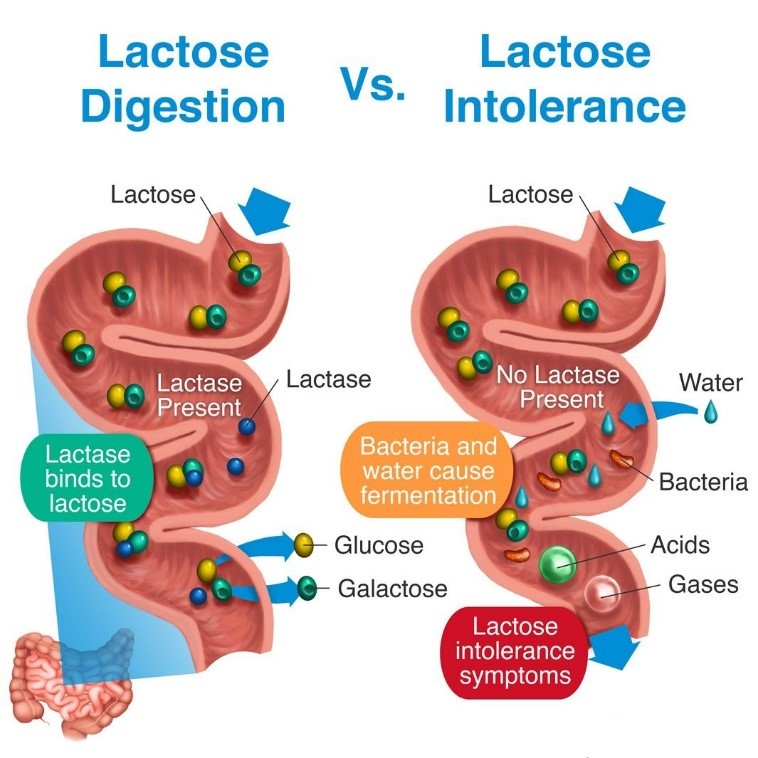 Fortunately, there are many foods that can supply the important nutrients that dairy provides, such as protein, calcium, magnesium, and vitamin D.18
Fortunately, there are many foods that can supply the important nutrients that dairy provides, such as protein, calcium, magnesium, and vitamin D.18
All whole fruits, vegetables, legumes, nuts, seeds, meat, poultry, fish, grains, and eggs are dairy free. When it comes to meeting your and your child’s nutritional needs, choose a variety of these non-dairy-containing foods.
Food sources of calcium: Fortified plant-based milk alternatives, fortified orange juice, canned sardines and salmon with bones, fortified dairy alternatives such as a non-dairy yogurt, tofu, soybeans, spinach, kale.19
Read more: Why Calcium Matters for Babies, Tots, and Mama
Food sources of vitamin D: Salmon, fortified plant-based milk alternatives, fortified cereals, egg, canned light tuna, portabella mushrooms – but most importantly: sunlight!20
Read more: Why Vitamin D Matters for Babies, Tots, and Mama
Food sources of protein: Fish, poultry, meat, beans, legumes, peas, nuts, seeds, tofu, eggs, whole grains.
Read more: Protein: Getting Enough and the Best Sources
Second: Look for dairy alternativesThere are many non-dairy substitutes on the market, such as coconut yogurt, plant-based milk alternatives such as almond- and oatmilk; and even vegan dairy-free butter! These allow you to still cook and bake dairy-free with ease, as well as enjoy dairy-like foods in your day.
If you are choosing a plant-based milk alternative, look for ones that are fortified with calcium and vitamin D.
Read more: What Type of Milk Should my Toddler Drink?
Reach out to your child’s healthcare providerIf you suspect that your child has lactose intolerance or a cow’s milk protein allergy, call their healthcare provider immediately. They can make sure you and your little one are getting the support you need and help you make informed decisions for moving forward. They may also recommend further testing or recommend your child be seen by an allergist.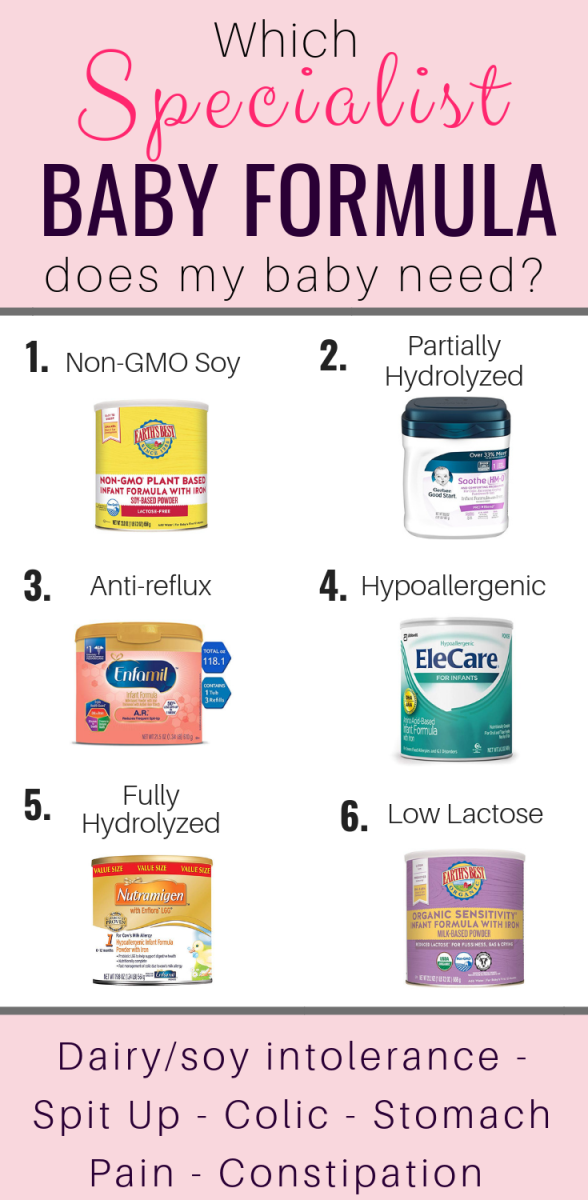
Remember that if your baby does not have an allergy to milk protein, that lactose intolerance in babies is not very common. Check in with a lactation consultant to help determine if what your baby is experiencing may be lactose overload, and what to do if it is.
Let's Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday - Friday 8am - 6pm (ET).Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles and recipes:Nutrients to look for at 6-12 months
Guidance when raising a child with food allergies
Introducing Major Allergens to your Infant
Does my Child Have a Food Allergy or a Food Intolerance?
Sources
Nutrition advice for lactose and milk intolerance in adults
"Why do I have such a reaction to milk?" - It is with this question that patients often come to visit a gastroenterologist. Let's figure it out!
Let's figure it out!
Milk is an emulsion and therefore a very favorable product for the digestive tract due to its physical properties. It has viscosity and enveloping properties, which often has a good effect on the digestive system and the body as a whole.
Milk is a multicomponent product: proteins, fats, carbohydrates. How many sides a product has, so many variants of problems can be. Claims to fat content are usually rare, but the carbohydrate composition most often causes criticism, mainly due to the main sugar of milk - lactose!
Lactose intolerance (lactase deficiency) in adults is a fairly common phenomenon and depends both on hereditary predisposition, and on the place of residence and tradition of drinking milk for food. For example, in northern Europe, lactose intolerance in adults occurs in 25% of the population, and among the indigenous peoples of Africa, Southeast Asia, North and South America, living closer to the equator, its frequency reaches 95%.
Lactase deficiency in adults is divided into secondary and primary. Primary lactase deficiency can manifest itself in childhood, may develop with age. Secondary occurs under the influence of intestinal infections and other causes that cause damage to the cells of the small intestine of various origins.
According to the degree of severity, it is divided into hypolactasia - a partial deficiency of the enzyme, and alactasia - its complete deficiency.
What is the difference between lactose and lactase?
Lactose (milk sugar) is a carbohydrate of organic origin, which consists of two molecules of glucose and galactose and is one of the main constituents of mammalian and human milk. In its unsplit form, lactose cannot be absorbed by the intestinal cells. Therefore, for its assimilation in the small intestine, a reaction is produced that separates lactose into components - glucose and galactose, which, penetrating into the cells of the small intestine, enter the general circulation, and then to the liver. In the liver, they are used for the synthesis and storage of glycogen, which is the fuel for the processes occurring in our body.
In the liver, they are used for the synthesis and storage of glycogen, which is the fuel for the processes occurring in our body.
Useful properties of lactose
- acts as a prebiotic, improving the composition of microflora;
- is involved in the synthesis of B vitamins;
- affects the absorption of calcium, magnesium and other microelements and its own enzymatic activity;
- is the power source.
Lactase is a special enzyme produced by cells in the small intestine that controls the breakdown of lactose. When the production of this enzyme decreases or stops, undigested lactose enters the large intestine, where a fermentation reaction occurs with the participation of bacteria, in which an abundance of gases is formed. In addition, if the use of dairy products regularly causes loosening of stool or pain, spasms, then an inflammatory reaction is triggered, which in the future can lead to prolonged duodenitis or functional disorders of the gastrointestinal tract, changes in the intestinal microflora.
Symptoms of lactose intolerance
The main clinical symptoms are loose stools (diarrhea), bloating, and gastrointestinal disturbances that occur immediately or within a day after ingestion of milk or dairy products.
In addition, in the presence of intestinal dysbacteriosis, substances formed during the microbial breakdown of lactose in the large intestine have a toxic effect and can cause general malaise, headaches, and, according to some reports, even mental disorders.
People with lactose intolerance are concerned about
- diarrhea and loose stools;
- rumbling in the intestines;
- flatulence;
- abdominal cramps and pains;
- nausea and vomiting;
- fatigue;
- weakness.
The intensity of symptoms depends on the quantity and amount of lactose obtained from food and lactase produced by the cells of the small intestine.
For information on the types of lactose intolerance and how to correct them, as well as the influence of microflora on lactose tolerance , see the video :
What foods contain lactose?
Milk and dairy products of animal origin naturally contain lactose, and many manufactured products may contain added milk sugar. Any product containing milk, lactose, whey, cottage cheese, milk powder contains lactose, so before buying products, you must familiarize yourself with the ingredients listed on its packaging.
Prepared foods that usually contain lactose include:
- cakes, biscuits and pastries;
- cheese sauce;
- pureed soups;
- custard;
- milk chocolate;
- pancakes;
- omelet;
- certain types of mashed potatoes.
Some products may contain "hidden lactose" and may not be declared on the packaging. Examples of products with hidden lactose:
- muesli bars;
- bread;
- breakfast cereals;
- margarine;
- certain instant soups;
- lozenges, chocolates and chocolates;
- ham or sausage;
- sauce or salad dressing and mayonnaise.

About 20% of prescription drugs, such as birth control pills, and about 6% of over-the-counter drugs, such as heartburn, contain lactose. Therefore, people with lactose intolerance (especially alactasia) should report lactose intolerance to their doctor when prescribing new medications.
What can replace milk with lactose intolerance?
Dairy products are a good and affordable source of calcium, protein and vitamins. Therefore, people with lactose intolerance need to use their alternative sources.
Some people with reduced lactase production retain some lactase activity and can include varying amounts of lactose in their diet without experiencing symptoms. For example, they have difficulty digesting fresh milk but eat certain dairy products, such as cheese or yogurt, without discomfort. These products are made using fermentation processes that break down most of the lactose in milk. In this case, yoghurts with live cultures, cheeses in which lactose is already fermented by bacteria, or low-lactose dairy products are recommended.
If it is necessary to completely exclude milk, you can use lactose-free milk, in which lactose is already split into glucose and galactose, as well as its vegetable alternatives - nut (almond, cashew, etc.), flaxseed, from cereals (oatmeal, rice, buckwheat, etc. ), coconut or soy milk. Grocery stores often offer a wide variety of lactose-free alternatives to various foods.
Instead of milk, you can add to the diet sources of calcium plant and animal origin:
- sesame;
- nuts and seeds;
- soy milk and curd;
- legumes;
- greens - dill, parsley;
- fatty fish such as salmon, tuna and mackerel;
- eggs.
Alternative sources of vitamin A include:
- carrots, broccoli, sweet potatoes, pumpkin,
- melon, apricot, papaya, mango;
- legumes;
- liver, eggs.
Vitamin D levels can be increased by exposure to natural sunlight, oily fish, eggs, fish oil, and some fortified foods.
Guidelines for the lactose-free diet
For both primary and secondary lactose intolerance, a lactose-free diet is the mainstay of treatment. Successful adherence to it ensures recovery and the cessation of disturbing symptoms.
The diet is selected individually depending on the severity of symptoms and provides for the restriction or elimination of products containing lactose from the diet. The duration of the diet also depends on the cause of the disorder and the severity of the symptoms. The rate of lactose that can be consumed without harm to health depends on the nature of the disorder. Many people retain residual activity of the lactase enzyme, so everyone should determine their individual lactose tolerance threshold after consulting a doctor.
When using a product with lactose, two factors are taken into account - the amount of milk sugar in it and its volume. To draw up a diet, it is convenient to use tables with a lactose content in 100 g of the product.
Lactose-free foods form the basis of a lactose-free diet. Lactose-free dairy products are a good substitute for the usual products.
Can expand diet and add some dairy products low lactose :
- fatty foods - butter, cream;
- fermented products - cheeses, yoghurts, full-fat cottage cheese.
The higher the fat content, the lower the milk sugar content.
Almond milk, soy milk, oat milk and any other plant-based drinks can replace regular milk in cooking. Alternative milk can be used to make not only drinks, such as smoothies or shakes, but also pancakes, omelettes, waffles and pastries.
The diet of a person with lactose intolerance should be balanced and make up for the lack of protein, vitamins and calcium, which he is deprived of, excluding dairy products.
If you are concerned about the symptoms of lactose intolerance, do not go on a lactose-free diet without consulting your doctor. It is possible that these symptoms may be due to other causes, and in particular inflammatory bowel disease. Nutritional supplements (enzymes containing lactase) can be an addition to the diet, they are taken in capsules or added to milk, used in home-made lactose-free fermented milk products.
Nutritional supplements (enzymes containing lactase) can be an addition to the diet, they are taken in capsules or added to milk, used in home-made lactose-free fermented milk products.
Nutritional intolerance to cow's milk protein in adults
It remains to discuss the last facet of milk - protein . We will mainly discuss cow's milk protein as the most common one consumed in our country.
Most often, as a "foreign" protein for our body, it can trigger allergic reactions that are detected even in childhood due to the brightness of manifestations - rashes, itching, vomiting or Quincke's edema after drinking cow's milk or products from it.
In adulthood, food intolerance to cow's milk protein is more common - this is a slow reaction of the immune system with a sluggish, but no less inconvenient symptomatology: bloating, unstable stools, cramps, pain, belching, mild periodic incomprehensible skin itching, general weakness, aching pains in the joints.
In the case of this reaction, the main thing is that, against the background of the symptom, local inflammation does not start - the gastrointestinal tract or systemic.
For these purposes, elimination (exclusion) diets or restriction in the use of certain food groups are used. The timing should be determined by the doctor, it is also important to prevent a lack of protein, D vitamins, calcium in the diet and to choose the optimal affordable replacement for all components of cow's milk and fermented milk products made from it.
You can get advice from a nutritionist-gastroenterologist specializing in the management of patients with milk intolerance (lactase deficiency and food intolerance to milk protein) at the Expert Gastroenterology Center. For express diagnostics of the above conditions, we suggest using the comprehensive LactoCheck program developed by the center's specialists.
Feeding a child with lactase deficiency
Lactase deficiency in a baby gives rise to many questions and fears in parents. The reason is the lack of lactase enzyme in the child's body. Lactase is responsible for the breakdown of milk sugar (lactose) into simpler substances that are absorbed and used by the body as a source of energy and nutrients.
The reason is the lack of lactase enzyme in the child's body. Lactase is responsible for the breakdown of milk sugar (lactose) into simpler substances that are absorbed and used by the body as a source of energy and nutrients.
It is divided into primary - congenital (transient) in immature newborns and adult LN (genetic defect) and secondary - when intestinal cells are damaged by infection, celiac disease, etc.
) against the background of immaturity of the gastrointestinal tract, after suffering an intestinal infection, allergies and other causes. Congenital complete lactase deficiency is rare, occurring in 5-6% of cases. These are lifelong lactose-free mixtures or ready-made lactase enzyme in breast milk.
Nutrition recommendations for lactase deficiency
If the child is lactose intolerant, lactase dissolved in warm milk is given before meals, then breastfeeding. If artificial feeding - lactose-free mixtures in a short course or low-lactose, sour-milk, which the doctor selects, according to the condition of the child.
If the baby has already received complementary foods of cottage cheese and yogurt, then as the intestines recover, fermented milk products are slowly introduced - yogurt, but not kefir.
If the child is after a year after suffering an intestinal infection, then during the period of manifestations, milk is also removed from the diet, we cook cereals without milk, instead of milk, you can use lactose-free mixtures for medical nutrition older than a year (clinutren junior, nutrini).
You can have a little hard cheese (parmesan), it does not contain lactose, as the condition improves, slowly yogurt (not kefir, not snow) and cottage cheese in the form of a casserole.
What to do if the child has lactase deficiency
If parents see that the child has signs of lactase deficiency, the first thing to do is contact a specialist. Only an experienced pediatrician will be able to figure out why the baby has colic or green stools, what the numbers in the tests say, and what is the norm for one baby and the pathology for another.











