Lactose intolerant baby food
Lactose-Free Baby Formula | Types, Reasons and Benefits
Lactose-free baby formula is a cow’s milk-based formula made for infants who have trouble digesting lactose, the sugar found in milk. Examples of lactose-free formulas include Similac Sensitive, Similac Alimentum, Enfamil NeuroPro Sensitive and Enfamil A+ Lactose Free.
What Is Lactose-Free Baby Formula?
Lactose-free baby formula is a cow’s milk-based formula that is specially processed to remove lactose, the sugar found in milk. Manufacturers then replace the lactose with another type of carbohydrate, such as corn syrup, to make it easier for babies with lactose intolerance to digest.
Lactose-free baby formula options include:
- Enfamil A+ Lactose Free
- Enfamil NeuroPro Sensitive
- Enfamil Simply Plant-Based
- Gerber Good Start Gentle Soy
- Similac Sensitive
- Similac Alimentum
Because most lactose-free formula is still made with cow’s milk, these formulas are not suited for babies with cow’s milk allergy, or CMA. Lactose intolerance and CMA are two different issues, though they may share similar symptoms that can include diarrhea, tender bellies, gas and fussiness.
CMA is an immune reaction, while lactose intolerance is a digestive issue, according to Nestlé Health Science. Babies with CMA would do better with a soy-based or hypoallergenic baby formula.
There are several varieties of lactose-free formula, low-lactose formulas and nondairy alternatives available in the U.S. Parents and caregivers should speak to their pediatrician to make sure a particular brand of lactose-free formula is right for their baby, especially if their baby requires preemie formula or has a condition called galactosemia.
Similac
Similac baby formulas are some of the most popular in the U.S. Two of their lactose-free formulas are Similac Sensitive and Similac Alimentum. These are milk-based formulas that are processed for lactose-intolerant infants.
However, Abbott Laboratories — the makers of Similac — issued a recall on baby formula in February 2022 for some lots of Similac made in its Sturgis, Michigan, factory because of potential bacterial contamination. If you purchased or plan to purchase Similac baby formula, make sure you check the recalled formula list.
If you purchased or plan to purchase Similac baby formula, make sure you check the recalled formula list.
Enfamil
Enfamil brand baby formula made by Mead Johnson is another popular brand of formula. Its lactose-free brands include Enfamil NeuroPro Sensitive and Enfamil A+ Lactose Free. Enfamil NeuroPro uses corn syrup as a replacement carbohydrate.
Unlike Similac, Enfamil brands haven’t been recalled recently.
Lactose-Free Dairy Alternatives
Some parents and caregivers may opt for lactose-free dairy alternatives, which are naturally free of lactose and aren’t made with cow’s milk. They are more suitable for babies with lactose intolerance and cow’s milk allergies.
These formulas are made with soy, rice or other types of plant-based protein. Formulas sold in the U.S are regulated by the U.S. Food and Drug Administration and have the same nutrition as cow’s milk-based formulas. Examples include Gerber Good Start Gentle Soy or Enfamil Simply Plant-Based.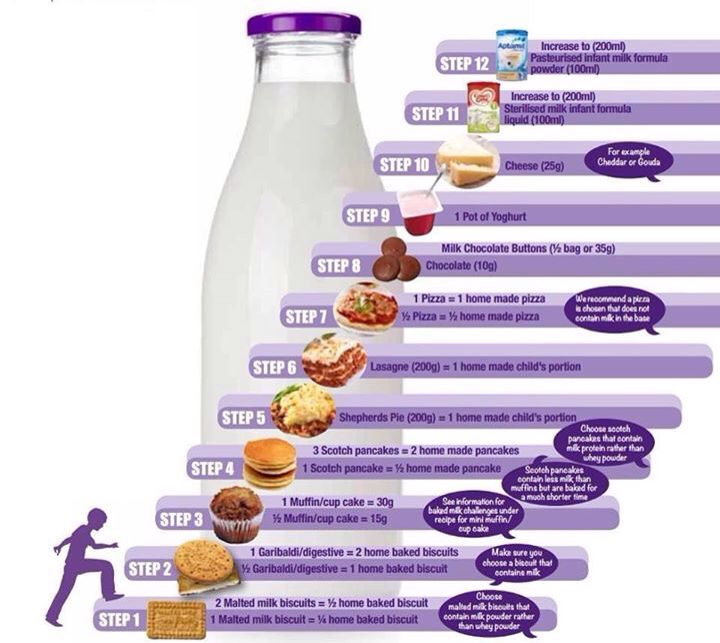
Low-Lactose Formulas
Low-lactose formula has reduced levels of lactose but may have higher levels than lactose-free brands. Many popular formulas fall in the low-lactose category.
Examples include Similac 360 Total Care Sensitive, which has 98% less lactose than Similac Total Care, and Enfamil A+ Gentlease which is advertised as a low-lactose brand, not lactose-free.
Babies Who Might Use Lactose-Free Formula
Only babies diagnosed with lactose intolerance should use lactose-free formulas. Most babies will tolerate regular cow’s milk formula well, and this is the type of formula many pediatricians recommend.
Babies with diagnosed cow’s milk allergies shouldn’t use lactose-free formulas since they still contain milk and milk protein, which are the causes of allergic reactions in babies with CMA. Mothers with babies who are lactose intolerant can still breastfeed, though mothers of babies who are sensitive to cow’s milk should refrain from consuming dairy while breastfeeding.
Parents and caregivers shouldn’t assume a fussy baby has lactose intolerance without consulting their baby’s doctor. Lactose intolerance in babies is very rare in children younger than 5 years of age.
Potential Side Effects of Lactose-Free Baby Formula
The potential side effects of lactose-free baby formula are similar to those of regular baby formula and are usually related to digestion or formula contamination. Symptoms include bloated bellies, loose stools and colic.
Symptoms of bacterial infection from contaminated formula include crying, fatigue, fever and poor feeding.
If a baby with a severe cow’s milk allergy or rare genetic disorder called galactosemia consumes a lactose-free formula that still contains cow’s milk or traces of lactose, the side effects can be life-threatening. The safest formula for these babies is one derived from plants and naturally lactose-free.
Formulas made with cow’s milk, including lactose-free brands, may cause a higher risk of necrotizing enterocolitis, or NEC, especially in premature babies. NEC is a rare but potentially deadly disease that causes intestinal tissue to die. Some parents have filed Similac and Enfamil baby formula lawsuits after their babies developed NEC and died.
NEC is a rare but potentially deadly disease that causes intestinal tissue to die. Some parents have filed Similac and Enfamil baby formula lawsuits after their babies developed NEC and died.
Lawsuit Information
Lawsuits are being filed by parents whose children were diagnosed with necrotizing enterocolitis (NEC) after consuming cow's milk-based formula. Learn more.
View Lawsuits
Possible Benefits of Lactose-Free Baby Formula
Possible benefits of lactose-free baby formula include better weight gain, less fussiness and less discomfort for the baby. Babies may be less likely to have reflux or spit-ups.
Because lactose intolerance can cause diarrhea, switching to lactose-free baby formula could relieve diarrhea and stop babies from becoming dehydrated.
Some babies see an improvement in symptoms in a few days, and in others it may take weeks.
Switching to Lactose-Free Baby Formula
If you think your baby may be lactose intolerant, don’t switch to lactose-free baby formula without first consulting with your child’s pediatrician.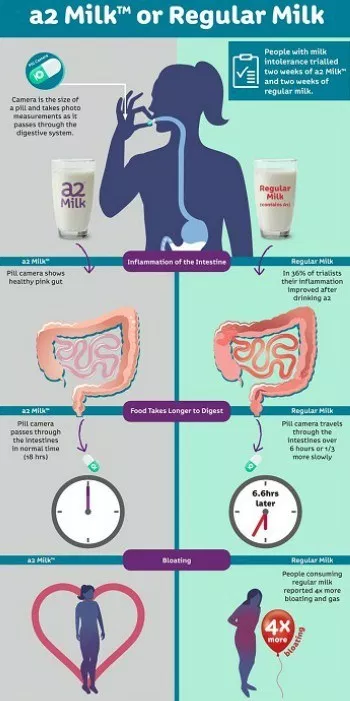 It’s important to get an actual diagnosis before switching formulas because your baby may have a genetic disorder or cow’s milk allergy.
It’s important to get an actual diagnosis before switching formulas because your baby may have a genetic disorder or cow’s milk allergy.
Once your child’s doctor has confirmed lactose intolerance, they will help you choose a formula that will work for your baby. Sometimes pediatricians have samples of formula for parents to try before committing to buying an entire container. If you have a formula you would like to try, let your baby’s doctor know so they can check the nutrients and ingredients.
Babies with digestive issues may initially have more challenges transitioning to another type of formula or from breastfeeding. Formula has a thicker consistency and is harder to digest than breastmilk. Highly processed formulas also have a more bitter taste.
A pediatrician may recommend slowly introducing the new formula and weening babies off the old formula or breast milk. After transitioning, make sure you monitor your baby for any signs of discomfort or symptoms and keep your pediatrician informed.
Please seek the advice of a medical professional before making health care decisions.
TELL US WHAT YOU THINK
Did You Find Drugwatch Helpful?
Yes No
Thank you for your feedback. Do you have any thoughts you'd like to share about Drugwatch.com?
This article changed my life!
This article was informative
I have a question
How can we improve this page?
This article contains incorrect information
This article doesn't have the information I'm looking for
I have a question
How can we improve this page?
Thank You for Your Feedback
We appreciate your feedback. One of our content team members will be in touch with you soon.
We appreciate your feedback. One of our content team members will be in touch with you soon.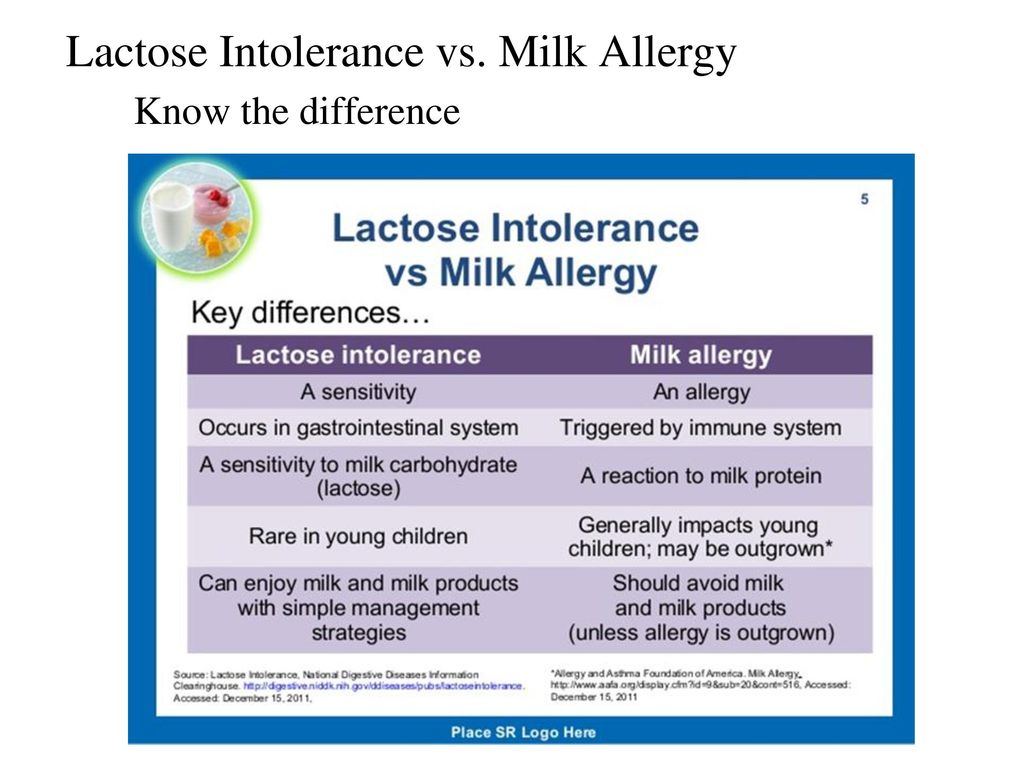
Lactose intolerant babies and toddlers
Read time: 8 minutes
What to know about the difference between a cow’s milk protein allergy and lactose intolerance in babies and toddlers:
What is lactose intolerance and how can it be managed in babies and toddlers?
Learn the difference between lactose intolerance and lactose overload in babies
Understand what a cow’s milk protein allergy is and how to help your baby or toddler eat while avoiding dairy.
Some babies can’t tolerate dairy, whether through the mother’s diet in breast milk, in formula, or once they’ve started solids. But how do you know if it’s lactose intolerance, a dairy allergy, or something else entirely?
Read on to learn how to figure out if your little one may be intolerant to lactose, or if their symptoms may indicate a milk protein allergy.
What is a lactose intolerance?Lactose itself is the sugar naturally found in dairy products. 1 People with lactose intolerance do not have enough of the enzyme lactase, which helps the body break down and digest this milk sugar. Without lactase, bacteria break down the excess lactose, creating more fluid and gas, which is where the symptoms of lactose intolerance come from.2
1 People with lactose intolerance do not have enough of the enzyme lactase, which helps the body break down and digest this milk sugar. Without lactase, bacteria break down the excess lactose, creating more fluid and gas, which is where the symptoms of lactose intolerance come from.2
Symptoms of lactose intolerance include:
Gas
Bloating, cramping, abdominal pain
Diarrhea
Nausea or even vomiting1,2
Symptoms usually show up between 30 minutes and 2 hours after having dairy.6
What causes lactose intolerance?A lack of the digestive enzyme lactase is sometimes genetic.2 Other times lactose intolerance may occur as a result of infections in the intestines or other illnesses such as Crohn’s disease, Celiac disease, or Irritable Bowel Syndrome; or as a temporary symptom of a virus your child may have. 3,4
3,4
One of the most common causes of lactose intolerance, however, is the slow natural decline of lactase that happens over time.5 This may start to occur after the age of 5 years.
Premature babies born before 34 weeks may also experience temporary lactase deficiency.5 Though this normally improves fairly quickly.4
Babies born at full term usually have plenty of lactose since it is a primary component of breastmilk (just like all mammalian milks).5,7 For this reason, lactose intolerance is generally not common in babies, but may start showing up in toddlers sometime after the age of three years.1
Read more: Is Your Baby Reacting to Something in Your Breastmilk?
Diagnosis of lactose intoleranceIf you suspect your little one has lactose intolerance, call their health care provider. Sometimes just a medical and diet history can help their doctor figure out if your baby is not able to digest lactose well.4 Other times, more tests may be needed.
Sometimes just a medical and diet history can help their doctor figure out if your baby is not able to digest lactose well.4 Other times, more tests may be needed.
Tests that may help identify lactose intolerance:
Hydrogen breath test. If your toddler is not able to digest lactose, there will be more hydrogen in their breath than usual.
Stool acidity. Taking a stool sample may help the doctor see if your little one is not digesting lactose. The stool will be more acidic.4
If your baby or toddler is diagnosed with lactose intolerance, the best treatment is avoiding or limiting dairy products and choosing lactose free products when they are available.2
While lactose intolerance is very rare in babies, should you feel your little one has a problem with lactose there is no need to stop breastfeeding. Simply minimize dairy in your diet and continue to breastfeed. However, keep in mind that your baby’s symptoms might actually be ‘lactose overload’ or cow’s milk protein intolerance. Keep reading to learn more about these alternate diagnoses.
Simply minimize dairy in your diet and continue to breastfeed. However, keep in mind that your baby’s symptoms might actually be ‘lactose overload’ or cow’s milk protein intolerance. Keep reading to learn more about these alternate diagnoses.
For a baby on formula, you may consider a low lactose (‘sensitive’) formula to see if that is helpful. The pediatrician can help guide this decision.
The good news is that most people who are lactose intolerant can in fact continue to drink or eat a certain amount of dairy without it causing symptoms.2 Some people may be able to have one serving of dairy, while others may tolerate a little more or less. Try different amounts to see if your toddler can still have a bit of dairy in their diet.
There are also dairy products that naturally have less lactose in them or are manufactured to be lactose-free which your toddler may be able to tolerate, including yogurt, cow’s milk, as well as hard cheeses such as cheddar or swiss. And of course, always be sure to provide your baby or toddler with foods in a texture they are developmentally ready to eat!
And of course, always be sure to provide your baby or toddler with foods in a texture they are developmentally ready to eat!
Read about: What Type of Milk Should my Toddler Drink?
What is lactose overload?Some women overproduce breastmilk, causing their little ones to take in a high volume of milk before they’re able to get a decent amount of the fat from the feed.8 This may cause something called ‘lactose overload’, or too much lactose for baby’s little tummy to digest at one time.8
Many times, lactose overload is mistaken for lactose intolerance, but with some changes in breastfeeding this issue can be managed and resolved.8,9
Symptoms of lactose overload include frothy or explosive stools that are a bit smelly and more than 10 urine diapers per day.8,9 A baby with lactose overload may have good or even higher-than-average weight gain. 9
9
Interestingly, a baby who is suffering from lactose overload may always seem hungry, even though they are gaining enough weight.9 This is because when baby is not getting enough fat, they are not registering the fullness and satisfaction that fat triggers in the brain.8
Management of lactose overloadThe most important thing is to first figure out if oversupply is the main culprit. The help of a lactation consultant will be important to get to the bottom of lactose overload.
If oversupply is the issue, the lactation consultant may recommend block feeding for a few days.8,9 This will help baby more fully empty a breast and get higher-fat feeds. Once symptoms are relieved, it’s time to go back to regular breastfeeding.9
For some mothers, the issue is not oversupply but rather feeding on a schedule or not feeding often enough.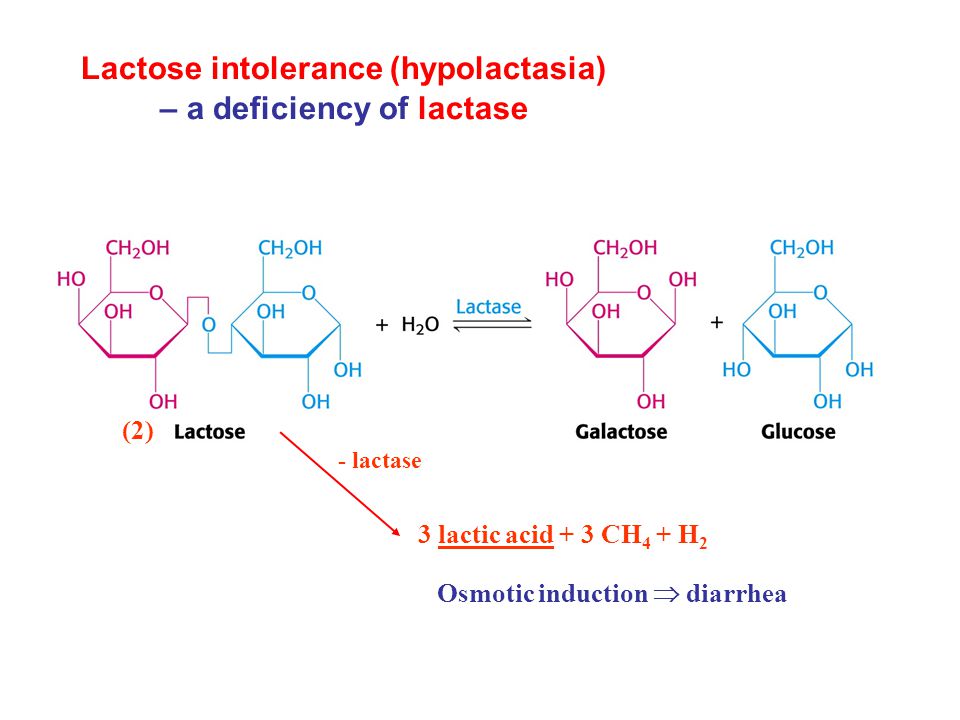 8,9 All of these may allow the breasts to fill up too much and provide baby with too much lactose and not enough fat.
8,9 All of these may allow the breasts to fill up too much and provide baby with too much lactose and not enough fat.
Be sure to feed your little one on demand, or when baby asks to feed.11 This is normally anywhere between 8 and 12 times per 24 hours depending on baby’s age.10
Read more:
What is Breastmilk Oversupply and How to Manage it
Should I Breastfeeding On Demand or on a Schedule
What is a cow’s milk protein allergy?While lactose intolerance is rare in babies, some little ones believed to have lactose intolerance may actually have an allergy or intolerance to the cow’s milk proteins whey and casein.
A cow’s milk protein allergy (CMPA or CMA) or intolerance (CMPI) happens when the body has an overreactive immune response to the protein, triggering an allergic reaction.12 CMA is one of the most common allergies in young children, affecting about 1 to 3% of babies and toddlers. 13,14
13,14
Fortunately, most children will eventually outgrow this as they get older and their digestive and immune systems mature.16
Symptoms of a cow’s milk protein allergyReactions usually happen within 1 to 2 hours after being exposed to cow’s milk protein, whether from breastmilk, formula, or from eating it in a meal.13 Reactions may range from mild to life-threatening.
In babies, symptoms of a milk protein allergy may include:
Colic, crying
Gassiness, bloating, discomfort
Eczema
Blood or mucous in the stool
Frequent stools
Vomiting16
In toddlers, symptoms of a milk protein allergy may include:
Red, itchy hives on the skin
Coughing and wheezing
Swelling of the lips, tongue, or throat
Vomiting
Anaphylaxis12,13
Anaphylaxis is a severe and potentially life-threatening allergic reaction that can occur within seconds to up to 2 hours after exposure to an allergen.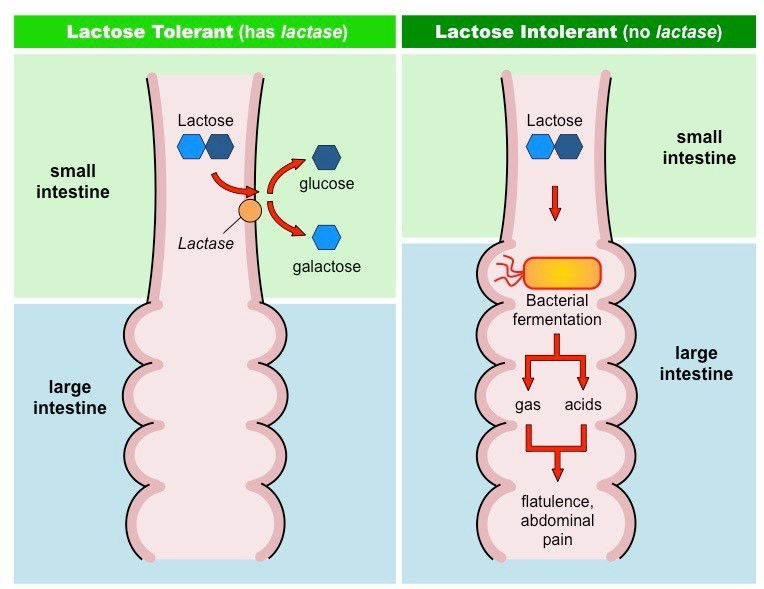 15 It can, among other things, cause a sudden drop in blood pressure and impaired breathing. If your child has known allergies, make sure you speak to your physician or allergist to get an emergency plan in place so that you are always prepared.
15 It can, among other things, cause a sudden drop in blood pressure and impaired breathing. If your child has known allergies, make sure you speak to your physician or allergist to get an emergency plan in place so that you are always prepared.
Wondering if your little one has lactose intolerance or a milk protein allergy? Reach out to our team of registered dietitians and lactation consultants for free! They’re here to help on our free to live chat from Monday – Friday 8am - 6pm (ET). Chat Now!
Diagnosis of cow’s milk protein allergyIf you feel your little one has an allergy, speak with their healthcare provider immediately. Their doctor will ask about their diet and when the symptoms tend to show up.
Tests that may help identify a milk protein allergy:
Skin prick test: usually done by an allergist
IgE test: a blood test that can help diagnose an allergy
Diet elimination: Taking out all dairy from the diet for 3 to 4 weeks to see if symptoms improve12
A diet elimination should be done with the help of a dietitian to ensure that your little one continues to get the nutrients they need for growth and development even when eliminating a food group.
Formula fed babies will likely need to switch to a non-dairy formula. Note that soy formula may or may not be a good alternative as some babies with CMA may also have a reaction to soy protein.16
When breastfeeding an infant allergic to cow’s milk protein, all dairy will need to be eliminated from your diet. When eliminating dairy, whether from your own diet or for an allergic toddler, reading labels is critical.
The following list includes some of the ingredients that indicate the presence of milk in the product:
Milk, cheese, cottage cheese, yogurt, sour cream
Lactose, lactulose, lactoferrin, lactic acid starter
Whey
Casein and caseinates
Curds
Milk by-products (like butter, ghee, and buttermilk)
Dry milk solids or powder, condensed or evaporated milk17
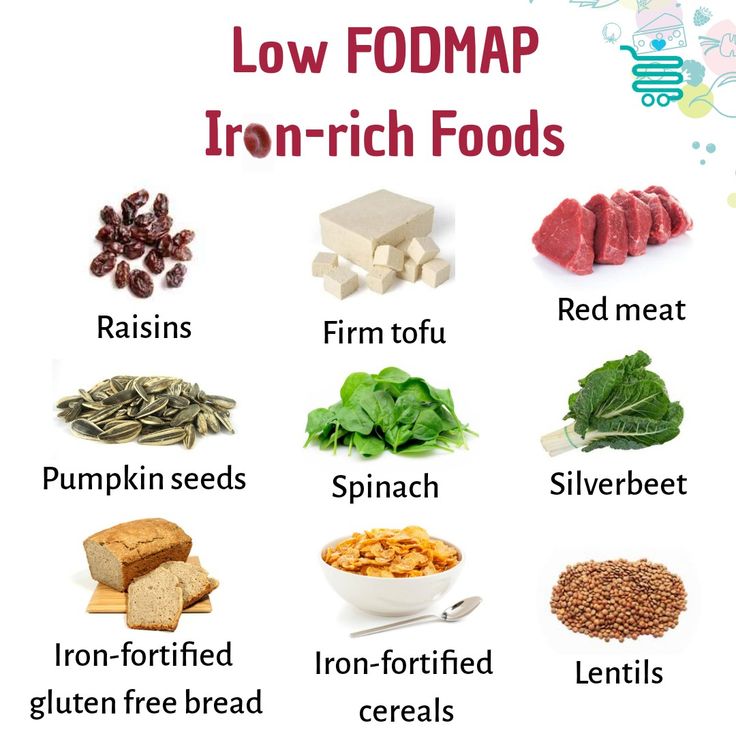
You may wonder how you or your child’s nutritional status may be impacted when foregoing dairy products.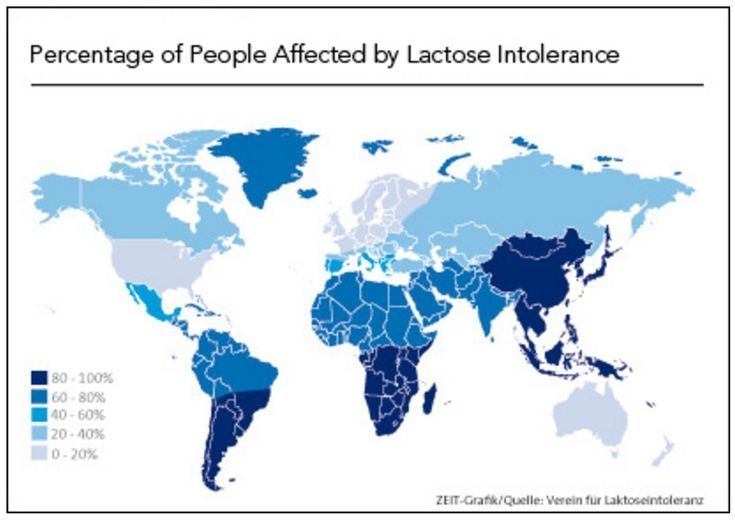 Fortunately, there are many foods that can supply the important nutrients that dairy provides, such as protein, calcium, magnesium, and vitamin D.18
Fortunately, there are many foods that can supply the important nutrients that dairy provides, such as protein, calcium, magnesium, and vitamin D.18
All whole fruits, vegetables, legumes, nuts, seeds, meat, poultry, fish, grains, and eggs are dairy free. When it comes to meeting your and your child’s nutritional needs, choose a variety of these non-dairy-containing foods.
Food sources of calcium: Fortified plant-based milk alternatives, fortified orange juice, canned sardines and salmon with bones, fortified dairy alternatives such as a non-dairy yogurt, tofu, soybeans, spinach, kale.19
Read more: Why Calcium Matters for Babies, Tots, and Mama
Food sources of vitamin D: Salmon, fortified plant-based milk alternatives, fortified cereals, egg, canned light tuna, portabella mushrooms – but most importantly: sunlight!20
Read more: Why Vitamin D Matters for Babies, Tots, and Mama
Food sources of protein: Fish, poultry, meat, beans, legumes, peas, nuts, seeds, tofu, eggs, whole grains.
Read more: Protein: Getting Enough and the Best Sources
Second: Look for dairy alternativesThere are many non-dairy substitutes on the market, such as coconut yogurt, plant-based milk alternatives such as almond- and oatmilk; and even vegan dairy-free butter! These allow you to still cook and bake dairy-free with ease, as well as enjoy dairy-like foods in your day.
If you are choosing a plant-based milk alternative, look for ones that are fortified with calcium and vitamin D.
Read more: What Type of Milk Should my Toddler Drink?
Reach out to your child’s healthcare providerIf you suspect that your child has lactose intolerance or a cow’s milk protein allergy, call their healthcare provider immediately. They can make sure you and your little one are getting the support you need and help you make informed decisions for moving forward. They may also recommend further testing or recommend your child be seen by an allergist.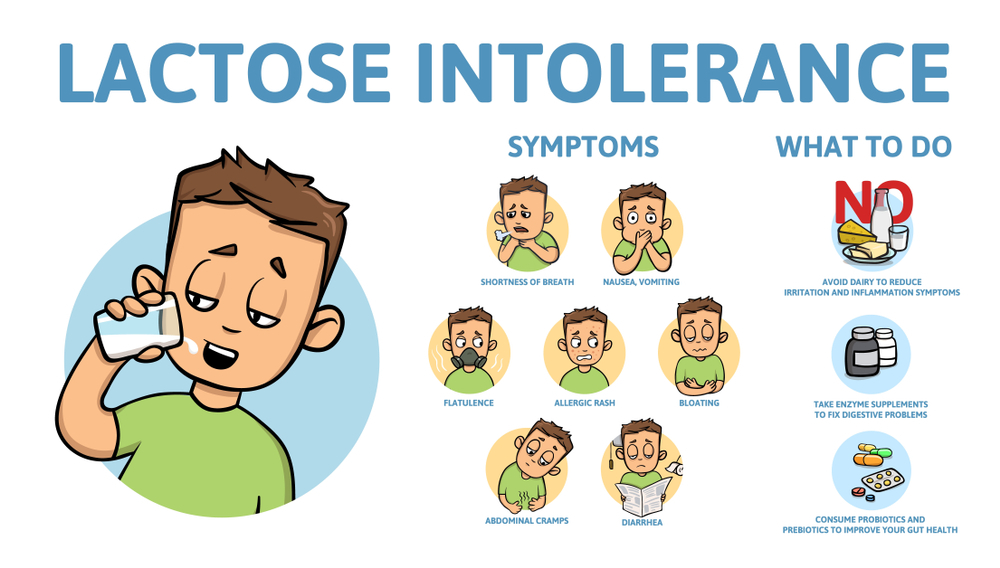
Remember that if your baby does not have an allergy to milk protein, that lactose intolerance in babies is not very common. Check in with a lactation consultant to help determine if what your baby is experiencing may be lactose overload, and what to do if it is.
Let's Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday - Friday 8am - 6pm (ET).Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles and recipes:Nutrients to look for at 6-12 months
Guidance when raising a child with food allergies
Introducing Major Allergens to your Infant
Does my Child Have a Food Allergy or a Food Intolerance?
Sources
Lactose Free Infant Formula | What does it mean and which is better
In the article we will talk about lactose-free baby food.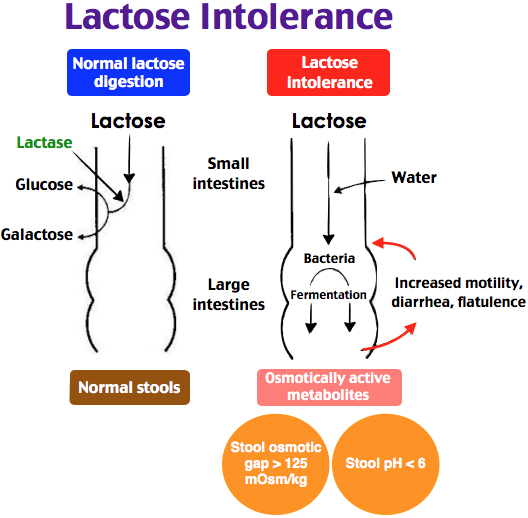 Pediatricians prescribe it for medical reasons. You will find out in what cases a lactose-free mixture is used, and why it is useful to have it even in a house where there is a healthy baby.
Pediatricians prescribe it for medical reasons. You will find out in what cases a lactose-free mixture is used, and why it is useful to have it even in a house where there is a healthy baby.
Lactose-free formula is a lifesaver for lactase deficiency and rotavirus
Lactose is milk sugar. Or the carbohydrate found in animal milk. It takes part in the absorption of vitamins and calcium, is a breeding ground for the reproduction of beneficial bacteria in the intestines. Lactose is the main source of energy for newborns. nine0003
Lactase is an enzyme that is produced in the intestines of an infant and helps digest lactose. Sometimes this enzyme is not produced enough. Then lactose is not completely broken down. This leads to bloating, diarrhea and restlessness of the baby.
Pediatricians diagnose lactase deficiency.
It is important to know that lactase deficiency is congenital - it is a very rare hereditary disease. At risk are babies whose next of kin suffer from lactose intolerance.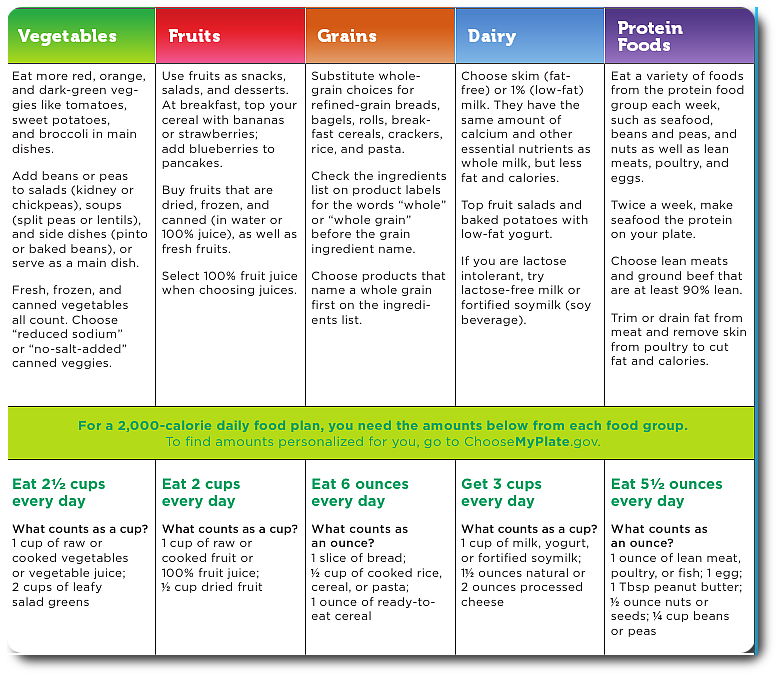 Parents, knowing this, need to be on the alert. nine0003
Parents, knowing this, need to be on the alert. nine0003
Much more often lactase deficiency - acquired - due to illness or other causes. Her symptoms go away after treatment and elimination of the cause. And you can again give the child dairy products.
Infants who are artificially and sometimes breastfed are transferred to a lactose-free or low-lactose diet temporarily or until they switch to adult food.
When lactose-free formula is prescribed
Unlike a low-lactose formula, which is recommended for temporary lactase deficiency, a lactose-free diet is used in cases of serious health problems. These are congenital lactase deficiency - galactosemia or rotavirus infection. nine0003
Lactose-free formula for rotavirus
Formula-fed babies with rotavirus need to switch to a lactose-free diet. With rotavirus infection, dairy products aggravate the symptoms of the disease, therefore, are prohibited.
If your baby is an artificial baby, stock up on a jar of soy formula for an emergency.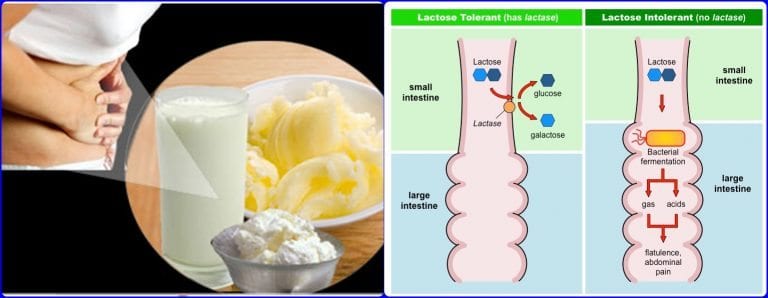 After all, with an intestinal infection, the last thing you want to do is waste time looking for food for your child. And if it is not useful, cook porridge on it for the baby when he grows up. nine0003
After all, with an intestinal infection, the last thing you want to do is waste time looking for food for your child. And if it is not useful, cook porridge on it for the baby when he grows up. nine0003
Nature has taken care of babies who receive mother's milk. It contains immunoglobulins and other substances that facilitate the course of the disease.
Therefore, pediatricians recommend not to interrupt breastfeeding during the period of rotavirus.
Lactose free formula - which is better
Mothers sometimes worry about whether a lactose-free diet can provide a child with all the necessary substances. There is no doubt that lactose-free formula, like any other, is a complete baby food. After all, this issue is under the control of the state. Activities for the production of baby food are subject to mandatory certification. nine0003
Lactose-free mixtures are of two types: on vegetable protein, for example, soy or hypoallergenic.
If the child is not allergic to soy, then it is better to use soy.
What does hypoallergenic formula mean? This means that they cannot cause allergies. All components are selected in such a way that they will be sure to be absorbed by the body. Hypoallergenic mixtures or hydrolysates are a product where proteins are partially broken down and are better absorbed. But hydrolysates are prescribed in the most difficult cases. They are bitter, and babies are reluctant to eat them. nine0003
Do not rush to transfer the child to a hypoallergenic diet, unless there are serious indications.
The line of Israeli baby food includes low-lactose and soy formulas:
Materna Extra Care Comfort - low lactose;
Materna Soy 0+ and 12+ are soy nutrition with an improved composition, adapted to the age characteristics of newborns and toddlers from one year old.
Give us a call and a free consultation will help you determine what nutrition your child needs. nine0003
All Materna baby food is made without palm oil, without sugar and without GMOs.
How to switch a child to lactose-free formula
The transition scheme depends on the cause. If you are transferring your child to a dairy-free diet due to rotavirus, then you need to change the diet at once. Just replace your food with soy. The baby may have a period of getting used to a new product. But this is a lesser evil than to continue to feed him with milk. nine0003
If the transition to soy nutrition is planned, we recommend introducing it according to our scheme.
Reaction to lactose-free formula
When transferring a child to another diet, watch his reaction. If soy was chosen as the lactose-free mixture, and an undesirable reaction occurred to it, an allergy to soy should be ruled out. To do this, take a blood test and consult a doctor.
Feeding a child with lactase deficiency
Lactase deficiency in a baby gives rise to many questions and fears in parents. The reason is the lack of lactase enzyme in the child's body.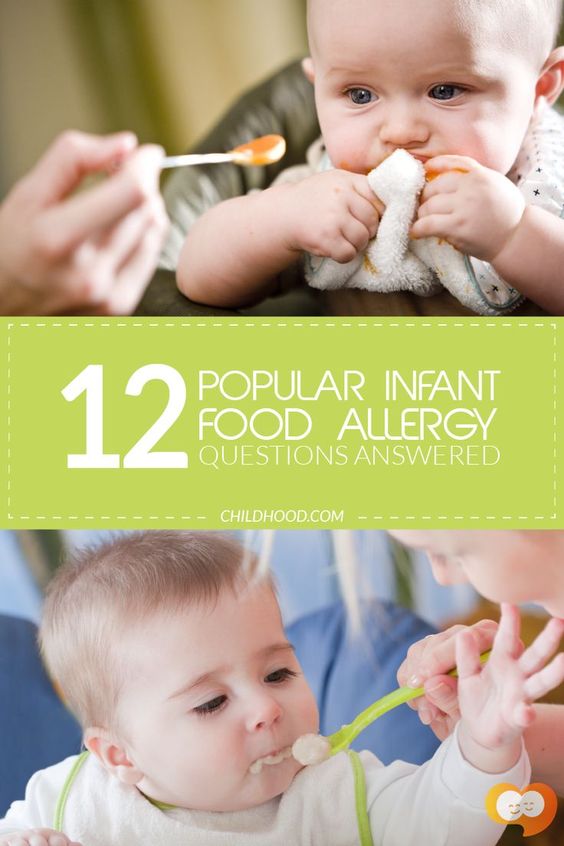 Lactase is responsible for the breakdown of milk sugar (lactose) into simpler substances that are absorbed and used by the body as a source of energy and nutrients.
Lactase is responsible for the breakdown of milk sugar (lactose) into simpler substances that are absorbed and used by the body as a source of energy and nutrients.
It is divided into primary - congenital (transient) in immature newborns and adult type LN (genetic defect) and secondary - when intestinal cells are damaged by infection, celiac disease, etc.
In children of the first months of life, lactose deficiency is more often transient (temporary) against the background of immaturity of the gastrointestinal tract, after an intestinal infection, allergies and other causes. Congenital complete lactase deficiency is rare, occurring in 5-6% of cases. These are lifelong lactose-free mixtures or ready-made lactase enzyme in breast milk.
Recommendations for nutrition in case of lactase deficiency
If the child is breastfeeding, then before eating, give lactase dissolved in warm milk, then breastfeed. If artificial feeding - lactose-free mixtures in a short course or low-lactose, sour-milk, which the doctor selects, according to the condition of the child.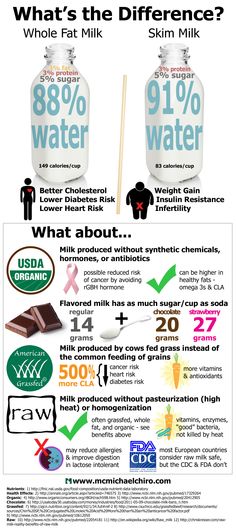 nine0003
nine0003
If the baby has already received complementary foods of cottage cheese and yogurt, then as the intestines recover, fermented milk products are slowly introduced - yogurt, but not kefir.
If a child after a year after suffering an intestinal infection, then during the period of manifestations, milk is also removed from the diet, we cook cereals without milk, instead of milk, you can use lactose-free mixtures for medical nutrition older than a year (clinutren junior, nutrini).
You can have a little hard cheese (parmesan), it does not contain lactose, as the condition improves, slowly yogurt (not kefir, not snow) and cottage cheese in the form of a casserole. nine0003
What to do if the child has lactase deficiency
If parents see that the child has signs of lactase deficiency, the first thing to do is contact a specialist. Only an experienced pediatrician will be able to figure out why the baby has colic or green stools, what the numbers in the tests say, and what is the norm for one baby and the pathology for another.