Lazy baby feeding
Common Newborn Breastfeeding Problems and Solutions
Common Newborn Breastfeeding Problems and Solutions Common Newborn Breastfeeding Problems and Solutions – Itzy Ritzy- Home
- OUR BLOG
- Common Newborn Breastfeeding Problems and Solutions
Liz Denfeld | November 21, 2022
Many new moms don’t give much thought to breastfeeding. At face value it seems like there’s not a lot that can go wrong —it’s nature, right? While women have been breastfeeding babies for hundreds of thousands of years, it doesn’t come without its challenges. From reflux to sore nipples to engorgement, there are a host of complications that might interfere with your nursing experience. The good news is, most breastfeeding hurdles can be overcome with the right help and we’re here to share some of the most common breastfeeding problems as well as solutions to make breastfeeding easier.
Nipple Pain
Yikes, that sounds pretty scary, right? If we had a dollar for every time someone told us “breastfeeding shouldn’t hurt,” we’d be rich. While we do agree that after the first few weeks you should be able to breastfeed pain-free, there is an adjustment period for your nipples as you and baby both figure out correct positioning and latch. Having said that, if your nipples are actually cracked, blistered or bleeding (not just sore), that is most likely a sign that you need some extra help.
The most common culprit of nipple pain is usually a poor latch. A lactation consultant can evaluate your situation and help you figure out the best positioning for you and baby will help tremendously. Using a nursing pillow can be a game-changer, especially in those first few weeks when getting the perfect nursing position is so important. We also highly recommend using gel pads or lanolin to help soothe nipple soreness. If the cracking is bad enough, you might even consider using a nipple shield while your nipples heal.
If you aren’t sure if the pain you are experiencing warrants some extra help, we love the advice Lindsay from Lactation Link gives: “Use the “30 second” rule. If your pain disappears within 30 seconds after latching, you can safely ignore it. If your pain lasts longer than that, gently insert your finger into the corner of your baby’s mouth to break the suction and unlatch baby, then try again. If you’re not able to get a latch that is comfortable for the majority of feeding session, your pain is severe, and/or you notice any damage to the nipple, you should seek help right away.”
If your pain disappears within 30 seconds after latching, you can safely ignore it. If your pain lasts longer than that, gently insert your finger into the corner of your baby’s mouth to break the suction and unlatch baby, then try again. If you’re not able to get a latch that is comfortable for the majority of feeding session, your pain is severe, and/or you notice any damage to the nipple, you should seek help right away.”
Plugged ducts feel like a lump in the breast and can affect milk production. Frequent feedings and hand expressions can help break up the clog. Warm compresses and massaging in the warm shower can also help. Plugged milk ducts can also cause mastitis or breast infection.
Breast EngorgementThis is a big one that rarely gets talked about, but if you’ve ever been engorged you understand what a big issue it can be. When your milk finally comes in about 2-5 days after birth, you will most likely experience engorgement. You’ll know you’re engorged because your breasts will “become larger and feel heavy, warmer and uncomfortable.” Your tell-tale sign, though, is that the area around your nipple will be hard and feel like it’s stretched to capacity, which could affect the latch that baby can get. If your baby isn’t nursing well and you can tell he/she can’t latch on effectively because you are engorged, you can self-express just enough to soften the nipple and help get that proper latch back. You can also use heat on your breasts 10-20 minutes before a feed to help relieve pain and soften things up, then after the feed use ice packs for up to 20 minutes. These are all effective tools in helping you maintain a proper latch so baby can remove as much milk as possible, which is the key to getting through engorgement.
You’ll know you’re engorged because your breasts will “become larger and feel heavy, warmer and uncomfortable.” Your tell-tale sign, though, is that the area around your nipple will be hard and feel like it’s stretched to capacity, which could affect the latch that baby can get. If your baby isn’t nursing well and you can tell he/she can’t latch on effectively because you are engorged, you can self-express just enough to soften the nipple and help get that proper latch back. You can also use heat on your breasts 10-20 minutes before a feed to help relieve pain and soften things up, then after the feed use ice packs for up to 20 minutes. These are all effective tools in helping you maintain a proper latch so baby can remove as much milk as possible, which is the key to getting through engorgement.
A baby falling asleep at the breast may almost seem like a good thing, but it’s actually the opposite. You need baby to stay awake and remove milk so they can get a full feeding instead of significantly more small snacks throughout the day/night. For some moms it becomes somewhat of a full-time job keeping their newborns awake for a feed. If baby starts dozing off you can tickle his/her feet, take a burping break, strip them down to nothing but a diaper so they aren’t too warm and cozy and if they really won’t wake up, you can even try running a wet wipe down their back (that one really wakes them up!).
For some moms it becomes somewhat of a full-time job keeping their newborns awake for a feed. If baby starts dozing off you can tickle his/her feet, take a burping break, strip them down to nothing but a diaper so they aren’t too warm and cozy and if they really won’t wake up, you can even try running a wet wipe down their back (that one really wakes them up!).
f you seem to be doing everything “right” and you still can’t seem to get a good latch with baby, you might want to get your baby checked for a tongue or lip tie. Some common symptoms of tongue or lip tie are a poor latch, a clicking sound while nursing, gassiness, reflux, colic, poor weight gain or baby gagging on milk or popping off your breast frequently to gasp for air. This is one breastfeeding issue that often goes undiagnosed or misdiagnosed, so our biggest piece of advice is to follow your gut. If something feels off for you and baby, get a second or third opinion if you need to.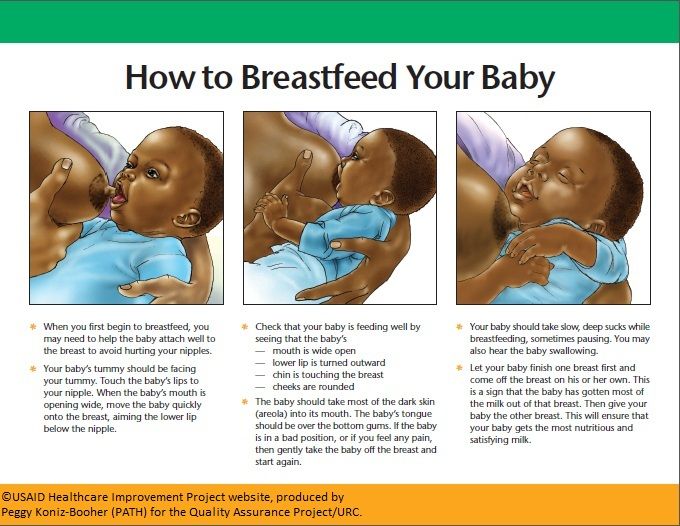
Reflux can be an extremely complicated issue and can range in severity. Generally speaking, spitting up is normal for babies — both breastfed and bottle-fed. Babies will spit up when they get too much milk too fast and it most often happens right after they eat. As long as your baby is gaining weight and doesn’t seem uncomfortable, you can consider them a “Happy Spitter.” The problems arise when baby is gagging, choking, experiencing pain while spitting up, or inconsolable or severely fussy while feeding and not gaining weight.
If you suspect your baby has reflux you should immediately speak with your pediatrician about your concerns to see if reflex medication is necessary. It is often recommended that reflex babies sit upright for at least 20 minutes after every feed. It’s also helpful to keep baby more upright while feeding.
Low Milk SupplyNot producing enough milk is a common worry for new moms. The baby needs to be gaining weight and regularly pooping when getting enough breast milk. Speaking with a lactation consultant can help you increase milk production.
Speaking with a lactation consultant can help you increase milk production.
Our biggest advice for you first-time breastfeeding mamas is this: If something feels off or you are in pain or feeling frustrated and discouraged — GET HELP. There are so many amazing lactation resources available to women now. Check out our Breastfeeding Essentials to see more products that can help you survive and thrive during your breast or bottle-feeding phase.
We especially love KellyMom.com as a resource as well as Lactation Link’s amazing online courses that cover the above mentioned problems and more.
If you’re looking for a more comfortable way to breastfeed or bottle-feed, we recommend our soft and stylish nursing covers.
Share this post:
Follow Us
FEATURED PRODUCT
Sold Out
Quick View
Chelsea + Cole for Itzy Ritzy Studded Itzy Mini Diaper Bag
You'll look amazing when you use this mini backpack as a diaper bag or as a going out bag for nig.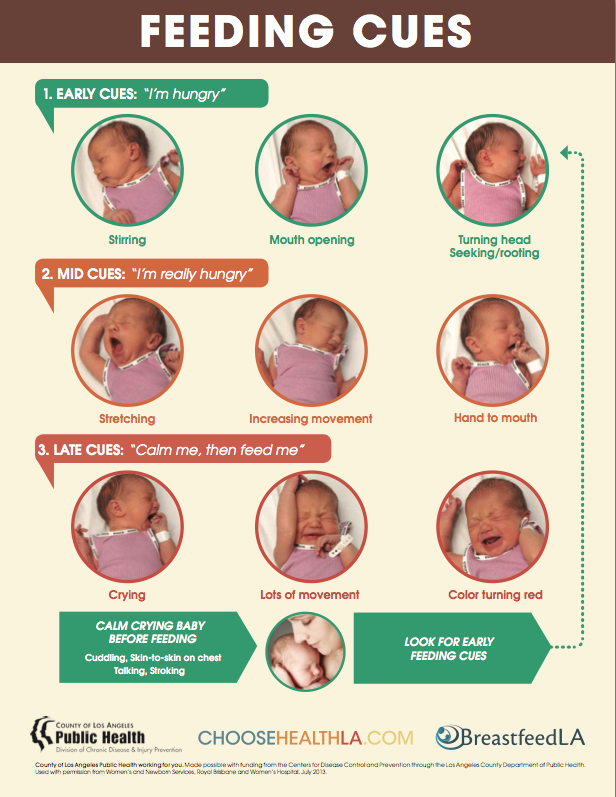 ..
..
Recent Articles
Top Breastfeeding Essentials: Must-Have Products for Nursing Moms
November 21, 2022
Hospital Bag For Dad or Partner: The Ultimate Checklist For What to Pack
October 31, 2022
Travel Gift Guide For This Summer
June 14, 2022
MORE NEWNESS
Boss Plus™ Large Diaper Bag Backpack
The sister to the Boss Backpack, the Boss Plus is a silhouette...
Bitzy Bespoke™ Ritzy Activity Gym™
Itzy Mini Wallet™ Card Holder and Key Chain Charm
Keep your necessities close with your new Itzy Mini Wallet! Ma...
Chelsea + Cole for Itzy Ritzy Boss Plus™ Diaper Bag Backpack
The comfortable backpack straps on this diaper bag are padded ...
Pack Like A Boss™ Packing Cubes
Staying organized has never been easier or more stylish! Our s...
Dream Weekender™ Hospital & Travel Bag
Whether you need a spacious hospital bag, a roomy overnight to...
Sweetie Soother™ - Pacifier 2-Pack
These 100% food grade silicone pacifiers come in multiple styl. ..
..
Itzy Mini™ Diaper Bag
This baby diaper bag has eight pockets — four apiece inside an...
Join our mailing list
First-time customers get 15% off!
Diaper Bags
New
Best Sellers
Outlet
Shop All
Parent
Baby
Gifting
Under $200 Under $100 Under $50 Under $20 Gift Cards
Collab
Chelsea and Cole
Guide
Account
Sign in Create account
It appears that your cart is currently empty! Continue Browsing
0" >
Quick buy
Register to receive an email notification when this item becomes available.
Something went wrong. Please try again
You have successfully subscribed!
See full details >>
Register to receive an email notification when this item becomes available.
Something went wrong. Please try again
You have successfully subscribed!
My Baby Won’t Breastfeed - La Leche League GB
This page is about young babies who have never breastfed or who get very upset when offered the breast. If your baby was breastfeeding well but is now refusing, see our page on “nursing strikes”. Sometimes, a new difficulty with feeding is the first sign that the baby is becoming unwell. If you are not sure that your baby is well, please contact your doctor.
When a baby doesn’t breastfeed after birth, it can be upsetting, confusing and frustrating. You might wonder whether you’re doing something wrong, or even whether your baby likes you. It’s hard not to take it personally!
It’s hard not to take it personally!
Babies are ‘hardwired’ to breastfeed – it is an essential survival behaviour. When a baby doesn’t breastfeed, it’s never because they don’t want to. Something is making it hard for them. Babies are never “lazy” or “difficult” – they always do the best they can. So do their mothers!
When it’s taking time for breastfeeding to get going:
- Keep your milk flowing
- Keep your baby fed
- Keep your baby close
If you do this, your baby is very likely to breastfeed when they are ready. Time, patience, and good feeding support are usually all you need.
This useful summary of the “3 Keeps” can be downloaded as a free A4 poster here.
You can read more about getting breastfeeding on track after a difficult start here.
Why isn’t my baby breastfeeding?
After a straightforward birth, most well, full-term babies will start feeding within an hour or so. Not all babies have such an easy start, though. Babies can take longer to start breastfeeding if:
Not all babies have such an easy start, though. Babies can take longer to start breastfeeding if:
- They had a more complicated birth. Babies born with the aid of forceps, for example, often take a few days to recover and feed well. If you had pain medication in labour, your baby may be sleepy and uncoordinated at first.
- Your baby was born early, or small for their gestational age. See also breastfeeding premature babies and late preterm babies (those born between 34 and 37 weeks). Even being born one or two weeks early can mean that your baby takes longer to start breastfeeding. It might take until around your baby’s due date, or a little longer, before they are ready to feed well.
- You and your baby were separated after birth because one or both of you needed medical care.
- Your baby is very sleepy and doesn’t yet have enough energy to breastfeed. See also sleepy baby and newborn jaundice.

- Your baby is unwell.
- Your baby is uncomfortable, e.g., some babies have a sore head or sore shoulder after birth.
- Your baby has low muscle tone (hypotonia).
- Your baby has a physical challenge such as tongue-tie.
You have plenty of time
Parents sometimes worry that if their baby isn’t breastfeeding well, or at all, in the first few hours, days or weeks after birth, it will never happen. While breastfeeding in the first hour after birth is ideal, the window of opportunity for babies to start breastfeeding is much longer than this. The feeding reflexes, which keep babies seeking and attaching to the breast, last for at least two to three months after birth. We have seen many babies start breastfeeding older than three months, too! There are even reports of children over a year old starting to breastfeed, when placed for adoption with a lactating mother. Where there is milk, there is always the possibility of breastfeeding.
Photo: Jen Valsler
First things first
Sorting out breastfeeding problems can feel overwhelming. There seems to be so much to do, and you might feel you have to do it all at the same time! It is helpful to know what is urgent and what can wait. This can help you to work out what to do in what order, and how best to use your time and energy. Feeding at the breast is the least urgent thing, at this stage.
If your goal is to have a full milk supply (enough milk to meet all your baby’s needs) but you need to use donated breastmilk or formula at the moment, or if your baby is not growing well just on your milk, then making more milk is the top priority. This is more urgent than your baby starting to feed at the breast.
If your baby is not breastfeeding at all yet, or is not breastfeeding effectively, you can express your milk. This gives you milk to feed your baby now and encourages your breasts to make plenty of milk for the weeks and months to come.
Your breasts may temporarily become swollen and uncomfortable, starting around 2-4 days after birth. This is called “engorgement” and is a sign that your breasts are becoming more active (though not all mothers feel it). It is important to treat engorgement, to keep your breasts comfortable and your milk flowing well. Read more here: Engorged breasts – avoiding and treating.
This is called “engorgement” and is a sign that your breasts are becoming more active (though not all mothers feel it). It is important to treat engorgement, to keep your breasts comfortable and your milk flowing well. Read more here: Engorged breasts – avoiding and treating.
Read here about how milk production works and how to increase your milk supply.
You can find information here on how to use bottles and other feeding tools.
Exclusive Expressing
Expressing all the milk your baby needs is known as “exclusive pumping” or “EP”. You can read more here. Some mothers choose to do this; many do it because their babies are not able to breastfeed. You might find it helpful to join an online support group for “EP mums”.
If you need to express your milk for a baby who is not breastfeeding yet, it is important to work with a skilled breastfeeding supporter. You might also want to connect with other mothers who have needed to express milk – they can be your best cheerleaders while you do this important job! Your local La Leche League group would love to support you.
Setting the scene for breastfeeding – happy time at (or near) the breast
Most babies need only time, patience, and gentle encouragement to help them start breastfeeding. Babies are born expecting to breastfeed, with a set of reflexes to help them do it. We need to keep them well fed (with expressed or formula milk), give them lots of relaxed time near the breast, and…. give the baby time.
Here are some ideas to try:
- Hold your baby skin-to-skin. Babies use their whole bodies to feed. The more of their skin they feel against yours, the more likely they are to find the breast and start feeding. Undress your baby down to their nappy and move your clothes out of the way. If you are cold, you can put a blanket round both of you. Even if your baby doesn’t breastfeed yet, it feels lovely, and helps your baby get used to being at or near the breast. Holding your baby against your skin helps you make more milk, too! If your baby can’t tolerate being held in a feeding position, try holding them against your shoulder.

- Avoid holding your baby in a feeding position during medical procedures, especially if your baby will be having lots. Offer the breast afterwards instead, if it calms them.
- Try “laid-back” breastfeeding. Try putting your baby tummy-down, on the slope of your body as you recline comfortably (as if you are lying on a sun lounger). Placed like this, they can use their arms and legs to help themselves find the breast and attach well for feeding. This can work better than trying to “put” the baby to the breast, especially if they have already had difficult experiences of this. This video shows you how. The safest place to do this is in a bed that has been set up following safe sleep guidance. See our article on safer sleep.
- Turn up the smell! Newborn babies don’t recognise the breast well by sight, though they do recognise your face, and love looking at it. They find the breast mostly by feel and smell. The little bumps around your nipple (Montgomery’s glands) make a scented oil which helps your baby find the breast and encourages them to feed.
 You can give your baby extra help by expressing a bit of milk and rubbing it on and around your nipples. This can encourage your baby to feed by increasing the smell and giving them something to lick as they approach the breast!
You can give your baby extra help by expressing a bit of milk and rubbing it on and around your nipples. This can encourage your baby to feed by increasing the smell and giving them something to lick as they approach the breast! - Try “drip-drop feeding”. Your partner or supporter uses a cup and spoon to drip milk (expressed milk or formula) onto the breast as you hold your baby. This can encourage babies to attach and feed. You can watch a video here.
- Take a bath with your baby. When placed skin-to-skin with their mother in a warm bath, some babies find the breast and feed for the first time. Some mothers even describe it as “a second chance at giving birth”. You could set the scene with low lighting, a candle or soft music. Whether or not your baby is ready to breastfeed yet, sharing a bath can help you and your baby relax together and enjoy each other. Have another adult with you to help you get in and out safely, put the baby on you and wrap them in a warm towel when they are ready to get out.

- “Wear” your baby. Babies who are kept close in a sling or soft carrier cry less, are calmer and warmer than babies who are put down by themselves. Being carried is good for babies’ physical & emotional development and helps parents and babies make strong connections. If your baby is not breastfeeding yet, carrying them close, as much as you want, is an excellent way to help them feel comfortable near the breast. Always follow the instructions for your sling or carrier and the rules for safe babywearing. You can read more about babywearing in this book.
- Feed your baby at or near the breast. If your baby will go to the breast at all, consider using a nursing supplementer so your baby can have extra milk while they breastfeed. This can be helpful when milk supply is low and/or your baby is frustrated by the speed of milk flow at the breast. If your baby is fed by cup or bottle, try feeding them skin-to-skin with their cheek against your breast.
 Let your baby end the feed by sleeping with their cheek pillowed on the breast.
Let your baby end the feed by sleeping with their cheek pillowed on the breast. - Consider sleeping with your baby. Some babies will attach and feed in their sleep if the breast is near enough to smell and feel. Always consider sleep safety before sleeping with your baby in your bed. It is never safe to sleep with a baby on a sofa. You can read more about sleep safety and normal baby sleep in LLL’s book Sweet Sleep.
Babies with low muscle tone (hypotonia)
A baby who has been diagnosed with a condition that makes them hypotonic, or ‘floppy’, may show little interest in breastfeeding. To make feeding easier:
- Support your breast. Tuck a rolled-up cloth under your breast close to your chest wall, or support your breast with your thumb on one side of the areola, fingers on the other side.
- Support your baby’s chin. If your thumb is parallel to your baby’s upper lip, you can use your index finger to put gentle pressure just behind the bony part of the chin while your baby feeds.

- Try upright positions. A hypotonic baby often feeds better held with their head higher than their bottom.
- Breast compression can also be helpful, but you may also need to give some expressed milk until your baby’s muscle tone improves. Breast compressions are explained in more detail in “My baby needs more milk”.
If your baby suddenly becomes floppy and you don’t know why, seek medical advice.
Baby steps
When you are keen to breastfeed, but your baby isn’t yet ready, it can be frustrating. Don’t forget to celebrate how far you have already come! Every time your baby enjoys being held close to your body, or falls asleep near your breast, they are taking another “baby step” towards breastfeeding. Your baby is doing the best they can for now, and so are you.
When breastfeeding is stressful
When breastfeeding is difficult for your baby, it may become stressful for both of you. Babies who have had unhappy experiences at the breast can develop negative associations with breastfeeding.![]() This might happen, for example, when:
This might happen, for example, when:
- A baby is in pain or discomfort e.g. from birth injury or allergy.
- A sensitive baby is handled at the breast in a way they don’t like, e.g., if a helper tries hard to “put” the baby to the breast when they aren’t ready.
- Milk supply is low.
- A baby has a physical restriction (e.g., tongue tie) that makes attaching and sucking difficult.
A baby who is finding feeding difficult may become upset:
- A short time into the feed, when milk flow slows down.
- At the start of the feed, when milk doesn’t come straight away.
- When offered the breast.
- When put in a breastfeeding position.
- When they see the breast.
When feeding isn’t going well, babies may come to associate the breast with hunger and frustration. They may develop a preference for another feeding method, such as a bottle, if they associate it with feeling full and satisfied. You can find some ideas on how to keep your baby’s relationship with the breast positive here: using donor milk & formula milk to support breastfeeding
The ideas in the previous section (“Setting the scene for breastfeeding – happy time at (or near) the breast”) can help your baby learn that the breast is a lovely place to be, and to associate it with calm, relaxation, comfort, and satisfaction rather than hunger and frustration.
Take a break
If breastfeeding has become very stressful for you and your baby, you might need a “breastfeeding break”. You could stop trying for a few days, whilst expressing your milk to keep your baby fed and keep your milk flowing. When you’re both ready, you can try again. There is no rush! Dr Christina Smillie, an American doctor who specialises in breastfeeding medicine, calls this “rebooting the baby”.
What if my baby is still not breastfeeding?
When you are eager to breastfeed, it is hard to wait. It is not uncommon for babies to need time to begin breastfeeding well. You might be encouraged by hearing the stories of other parents whose babies took time to get going.
If your baby is still not breastfeeding even with time, patience and some of the tips in this article, there will be a reason why. A skilled breastfeeding supporter can help you find out, and work towards breastfeeding. Some babies need medical care, some benefit from feeding tools such as nipple shields and a few need treatment for tongue tie. Many just need a little more time.
Many just need a little more time.
A few babies never do breastfeed. Some have a medical condition that makes it impossible. Very rarely, we never find out why. You don’t have to feed your baby directly from the breast to give them the many benefits of your milk or to nurture them at your breast. We can support you to have a close, happy feeding relationship with your baby, whatever form that takes.
La Leche League Leaders (breastfeeding counsellors) can help. You can find your local group, and LLL Zoom Meetings all over the country, at https://www.laleche.org.uk/find-lll-support-group/
Jayne Joyce, LLL Oxfordshire & Karla Napier, LLL Edinburgh, April 2022
A baby is too lazy to suckle, or "Lazy sucker"
- Alla Anatolyevna, what kind of baby is called "lazy sucker"?
- There is no such condition and concept in the international classification of diseases, this is Russian "know-how". "Lazy sucker" - a baby who is too lazy to suckle. Such a child was born in good condition, has no special problems with digestion and health. He is simply lazy and refuses to breastfeed because sucking requires effort.
Such a child was born in good condition, has no special problems with digestion and health. He is simply lazy and refuses to breastfeed because sucking requires effort.
— Why does the baby suckle poorly and resist breastfeeding?
- The reasons lie in individual characteristics. All children are different, like snowflakes - some suck with appetite, others refuse to breastfeed. But such children do not have health problems, they just do not want to work hard to get milk from the breast. The bottle contains easily accessible food, which they eat well.
Most often, "lazy suckers" are found among newborns who in the first month of life have not yet got used to their mother. But if the baby was breastfed up to 4-6 weeks, then most likely he will continue to breastfeed. The first weeks are a difficult period to go through.
— What are the signs that a baby does not want to suckle?
— With complaints that the baby is not suckling well, more often mothers come who have good lactation, but the children do not gain weight well. Therefore, in order to understand the reasons for what is happening, you first need to find out if the mother has enough milk. If, according to the results of pumping, the amount of milk that the baby should eat according to the doctor’s calculations is sufficient, but less than half is sucked out according to the control weighing figures, then he simply does not want to suck.
Therefore, in order to understand the reasons for what is happening, you first need to find out if the mother has enough milk. If, according to the results of pumping, the amount of milk that the baby should eat according to the doctor’s calculations is sufficient, but less than half is sucked out according to the control weighing figures, then he simply does not want to suck.
Another “litmus test” is a bottle. Lazy babies want to eat, but refuse to suckle at the breast, and at the same time, with great pleasure, they eat everything that is in the bottle, from which the liquid flows well.
— How can you tell a reluctance to suckle from an allergy or gastrointestinal problem?
- "Lazy sucker" - a normally healthy baby who always gets his breast milk. Most often, parents lose their nerves, and they supplement the baby. Therefore, he normally puts on weight, sleeps, eats, but does everything possible to get a bottle instead of a breast.
A sick child with food allergies or gastrointestinal problems typically has skin rash, regurgitation, abdominal pain, colic, mucus, blood in stools, poor weight gain, feeding anxiety, flatulence, and other symptoms painful condition.
— What to do if the baby is too lazy to breastfeed? Fight with it? Or will the problem go away without the intervention of parents and doctors?
— There is no need to fight this with the help of medicines. The main recommendation in this case would be frequent breastfeeding. The baby sucked a little on the breast, fell asleep, woke up in half an hour, and the mother again had to offer him the breast. This is quite difficult, especially during the recovery period and complex hormonal changes after childbirth. A tired mother only gets used to the baby, but must feed him on demand at short intervals. And this is normal: application stimulates lactation, starts the connection between mother and baby.
The main struggle with the “lazy sucker” is not to “break down” to his desires and not to give a bottle from which it is easy to suck and swallow milk. During this period, the mother should spend as much energy as possible to maintain breastfeeding.
— What mistakes of parents lead to the fact that later the child is too lazy to suck on the breast and pacifier? Is it true that nipples with large holes provoke reluctance to suckle?
- The main mistake of a mother who has enough milk is to feed or supplement her baby from a bottle with expressed milk. The baby in this case receives breast milk, but at the same time does not bother to get it from the breast. So it’s easier for mom - to quickly express and be calm that her child is fed and has received healthy nutrition, plus you don’t need to look at his whims ... But doing this, it’s very difficult to establish a natural process later.
The baby in this case receives breast milk, but at the same time does not bother to get it from the breast. So it’s easier for mom - to quickly express and be calm that her child is fed and has received healthy nutrition, plus you don’t need to look at his whims ... But doing this, it’s very difficult to establish a natural process later.
The bottle nipple is selected according to age: the holes are small for babies and larger for older ones. A properly selected nipple creates comfortable conditions for sucking.
— How to make a baby suckle if mother constantly refuses to breastfeed?
- Mom needs to actively breastfeed a lazy baby. Of course, this takes time, and sometimes it takes a month to teach a baby to suckle and receive food from the breast. But you don't have to stop breastfeeding.
If the baby is unable to attach to the breast or does not latch on to the nipple, a lactation assistant should be called in. Online schools for moms also show how to teach a baby to suckle, to breastfeed properly while sitting, lying down, with problem nipples, in order to put the baby to the breast in the future for a long time and with pleasure.
— And if the child refuses not only the breast, but also the bottle with expressed milk?
- Sooner or later the child will eat, because he will get hungry. They offered a bottle, but the baby refused - carry him in your arms or hold him in a column, do gymnastics, then offer a bottle again.
There are no children who do not eat for a day, and you can do without food for an hour or two, nothing will happen to the child's health. Even if then the newborn sucks a little, falls asleep for half an hour and sucks again - this is normal when accustoming to breastfeeding. At the same time, the mother can change the child's regimen in the right direction, making food fractional, but not frequent.
"Lazy sucker" is not a disease. This is the name of healthy children who do not want to breastfeed. If the child begins to be lazy, do not bottle feed him. It is better to put the baby to the breast as often as possible in order to maintain breastfeeding and teach him to suck his mother's milk.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
Positions for breastfeeding | Medela
For most mothers, breastfeeding is a skill that needs to be learned. Therefore, mothers may need extra help in teaching breastfeeding skills. In particular, they may need guidance on how to position the baby and how to attach it to the breast in a way that is comfortable for both mother and baby. There are many breastfeeding positions that can suit every breastfeeding mother. It is very important that the mother always feels comfortable while breastfeeding. As a rule, the baby should be positioned so that his face is turned towards the mother's body, and the head, shoulders and hips are in line. The most commonly used postures are cradle, cross cradle, grip, and side lying.
As a rule, the baby should be positioned so that his face is turned towards the mother's body, and the head, shoulders and hips are in line. The most commonly used postures are cradle, cross cradle, grip, and side lying.
Share this information
Cradle position
Cradle position is the most common position for feeding a baby.
The mother's hand supports the baby at the breast. The baby's head lies next to the mother's elbow, while her arm supports the baby along the back and neck. The baby's chest should be turned to the mother's chest.
Cross cradle position
In the cross cradle position, the mother takes the child with her other hand (relative to the cradle position), supporting his head and neck. With the other hand, she can support the breast and, if necessary, squeeze it, so that it is more convenient for the child to grab the nipple.
In this position, the mother can easily guide the baby to the breast when he is ready to take her.
“Capture” position
The baby is located on the side of the mother, his body and legs are at her fingertips. The mother holds the baby's head in her hand. In this position, you can also put your hand on a pillow.
This position may be optimal for mothers who have had a caesarean section as there is little or no pressure on the chest and abdomen in this position.
This position may also be suitable for babies who are born with a low birth weight or who have problems latching on as the baby's head is fully supported in this position.
Side-lying position
Mother lies on her side facing the baby. The baby's mouth is on the same level as the nipple.
Mom can also use a pillow to support her back and neck.
This position may also be optimal for mothers who have had a caesarean section, as there is little or no pressure on the chest and abdomen in this position.
Literature
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists.