Mother feed milk baby video
Breastfeeding: Mini Parenting Master Class
Transcript of 'Breastfeeding: Mini Parenting Master Class' video
"Did you know that your nipples have good bacteria? So you don’t need to wash them before breastfeeding.
My name is Dr. Michele Griswald, and this is my Mini Parenting Master Class on breastfeeding."
Is breastfeeding easy?
"Sometimes mothers get messages that breastfeeding is natural and it’s easy. Sometimes breastfeeding can be easy with the first baby, and hard with the second baby for the same mother. So it really just depends."
Does breastfeeding hurt?
"You shouldn’t stop breastfeeding if your nipples hurt. You should keep breastfeeding but you should get help to see why it’s hurting."
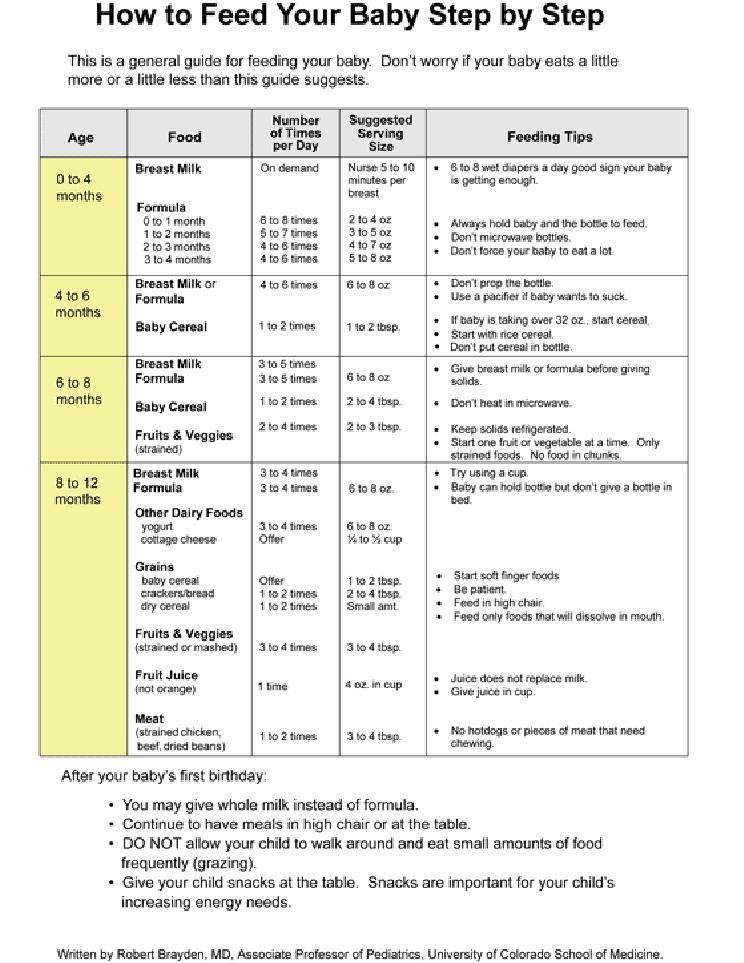
How much should my baby eat?
"They should see signs of hunger about 8 to 12 times in 24 hours. Newborn babies need to eat a lot because they’re growing rapidly. They double their birth weight in the first six months of life, or before. So you can imagine how much you would need to eat if you had to double your weight."
Should I wash my nipples before breastfeeding?
"It’s not necessary to wash your nipples before you breastfeed, because the breasts and the skin around the nipple actually produces good bacteria. And it’s that good bacteria that helps to prevent infections on the mother’s breast."
When should I start breastfeeding?
"The first hour after birth is a very important time for the mother and the baby. Breastfeeding is a very organized, neurological behavior. And so right after birth, keeping them against the mother’s skin can help them to be calm enough to start to seek the breast. And if we do just leave mothers and babies like that after birth, then they will usually start to go towards the breast on their own. Within about 30 minutes to one hour."
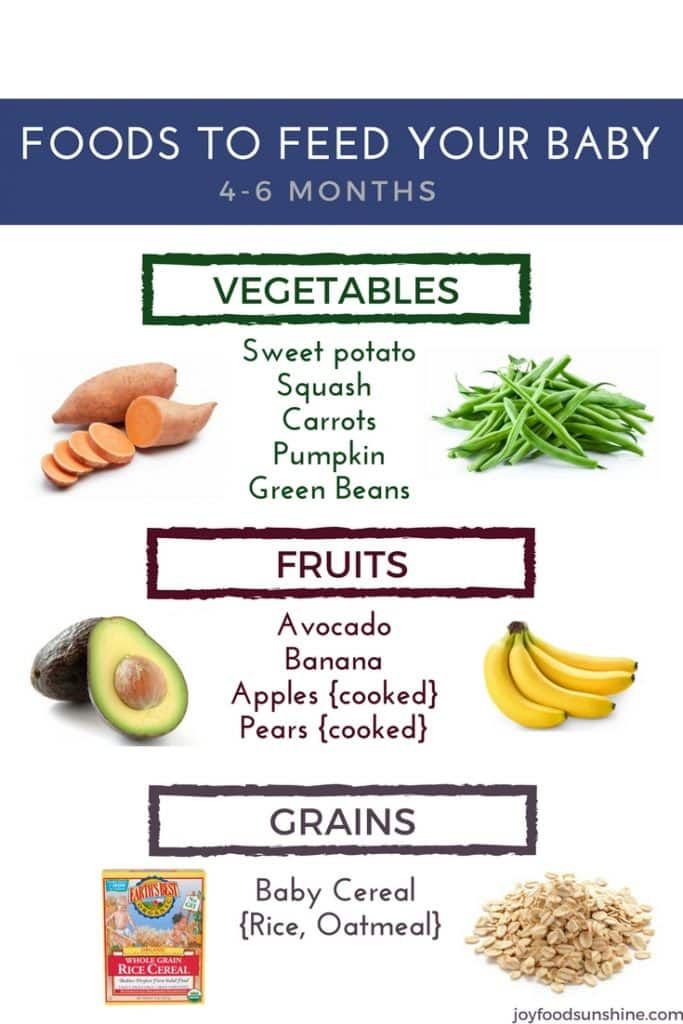
What should I eat while breastfeeding?
"Most mothers can eat anything they want when they breastfeed. They can follow their normal diet. And the interesting thing is whatever they eat, the babies will taste through their milk and start to get them ready for table foods when they’re about 6 months old."
And the interesting thing is whatever they eat, the babies will taste through their milk and start to get them ready for table foods when they’re about 6 months old."
When should I wean my baby?
"Babies will naturally wean starting around one year of age or so because developmentally, they’re changing so much. They’re becoming less focused on their mother, and more focused on learning about the world around them."
Will I have to wean my baby when I got back to work?
"We would hope that mothers who return to work do not have to wean their babies. Mothers need time and they need support to continue to breastfeed their babies. They need the support of their family, they need the support of their workplace, their employers, they need the support of their entire community.
Breastfeeding not just about food. It’s part a nurturing care package that helps children to grow and thrive throughout their entire life."
UNICEF Mini Parenting Master Class with Dr. Michele Griswold PhD, MPH, RN, IBCLC. Dr Griswold is a lactation consultant, registered nurse, breastfeeding researcher and advocate. She represents the International Lactation Consultant Association to the WHO/UNICEF Global Breastfeeding Collective, which calls on governments and society as a whole to provide mothers the support they need to breastfeed.
Michele Griswold PhD, MPH, RN, IBCLC. Dr Griswold is a lactation consultant, registered nurse, breastfeeding researcher and advocate. She represents the International Lactation Consultant Association to the WHO/UNICEF Global Breastfeeding Collective, which calls on governments and society as a whole to provide mothers the support they need to breastfeed.
Breastfeeding: is my baby getting enough milk?
When you first start breastfeeding, you may wonder if your baby is getting enough milk.
It may take a little while before you feel confident your baby is getting what they need.
Exclusive breastfeeding (breast milk only) is recommended for around the first 6 months of your baby's life. Introducing bottle feeds will reduce the amount of breast milk you produce.
Read Unicef's checklist How can I tell if breastfeeding is going well? for more guidance.
Credit:
IAN BODDY/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/294115/view
Signs your baby is well attached
- Your baby has a wide mouth and a large mouthful of breast.
- Your baby's chin is touching your breast, their lower lip is rolled down (you can't always see this) and their nose isn't squashed against your breast.
- You don't feel any pain in your breasts or nipples when your baby is feeding, although the first few sucks may feel strong.
- You can see more of the dark skin around your nipple (areola) above your baby's top lip than below their bottom lip.
Signs your baby is getting enough milk
- Your baby starts feeds with a few rapid sucks followed by long, rhythmic sucks and swallows with occasional pauses.

- You can hear and see your baby swallowing.
- Your baby's cheeks stay rounded, not hollow, during sucking.
- They seem calm and relaxed during feeds.
- Your baby comes off the breast on their own at the end of feeds.
- Their mouth looks moist after feeds.
- Your baby appears content and satisfied after most feeds.
- Your breasts feel softer after feeds.
- Your nipple looks more or less the same after feeds – not flattened, pinched or white.
- You may feel sleepy and relaxed after feeds.
Other signs your baby is feeding well
- Your baby gains weight steadily after the first 2 weeks – it's normal for babies to lose some of their birth weight in the first 2 weeks.

- They appear healthy and alert when they're awake.
- From the fourth day, they should do at least 2 soft, yellow poos the size of a £2 coin every day for the first few weeks.
- From day 5 onwards, wet nappies should start to become more frequent, with at least 6 heavy, wet nappies every 24 hours. In the first 48 hours, your baby is likely to have only 2 or 3 wet nappies.
It can be hard to tell if disposable nappies are wet. To get an idea, take an unused nappy and add 2 to 4 tablespoons of water. This will give you an idea of what to look and feel for.
Ways to boost your breast milk supply
- Ask your midwife, health visitor or breastfeeding specialist to watch your baby feeding. They can offer guidance and support to help you properly position and attach your baby to the breast.
- Avoid giving your baby bottles of formula for the first 6 months or a dummy until breastfeeding is well established.

- Feed your baby as often as they want and for as long as they want.
- Expressing some breast milk after feeds once breastfeeding is established will help build up your supply.
- Offer both breasts at each feed and alternate which breast you start with.
- Keep your baby close to you and hold them skin to skin. This will help you spot signs your baby is ready to feed early on, before they start crying.
Things that can affect your milk supply
- Poor attachment and positioning.
- Not feeding your baby often enough.
- Drinking alcohol and smoking while breastfeeding – these can both interfere with your milk production.
- Previous breast surgery, particularly if your nipples have been moved.
- Having to spend time away from your baby after the birth – for example, because they were premature.

- Illness in you or your baby.
- Giving your baby bottles of formula or a dummy before breastfeeding is well established.
- Using nipple shields – although this may be the only way to feed your baby with damaged nipples and is preferable to stopping feeding.
- Some medicines, including dopamine, ergotamine and pyridoxine. Read more about breastfeeding and medicines.
- Anxiety, stress or depression.
- Your baby having a tongue tie that restricts the movement of their tongue.
With skilled help, lots of these problems can be sorted out. If you have concerns about how much milk your baby is getting, it's important to ask for help early.
Speak to your midwife, health visitor or a breastfeeding specialist. They can also tell you where you can get further support.
Got a breastfeeding question?
For fast, friendly, trusted NHS advice anytime, day or night, talk to the Start4Life Breastfeeding Friend on Amazon Alexa, Facebook Messenger or Google Home.
Video: Is my baby getting enough milk?
In this video, a health visitor talks about the signs your baby is getting enough milk.
Media last reviewed: 1 November 2022
Media review due: 1 November 2025
Page last reviewed: 6 September 2022
Next review due: 6 September 2025
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly.
 Proper grip is the key to comfort when breastfeeding.
Proper grip is the key to comfort when breastfeeding. - If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time. ”
”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors. Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Mastitis: symptoms and treatment | Philips Avent
search support iconSearch Keywords
- one of the most natural processes for a woman, but it is not always easy. Along with the individual aspects of breastfeeding, there are some general problems that new breastfeeding mothers may face.
One of these is mastitis, an inflammatory disease that causes tenderness and tenderness in the breast tissue.
The frequency of lactational mastitis among women in different countries ranges from 2% to 33% and averages about 10%*.
Mastitis in breastfeeding women is caused by a bacterial infection of the milk ducts that enters through cracks, irritation of the nipple, or a nipple piercing.
Lactational mastitis is dangerous because it can cause pain while breastfeeding, interfere with the bonding process between mother and baby, or even interfere with milk production.
To protect the health and comfort of mother and child, and the mother's milk supply, this problem must be addressed urgently.
So, here are the answers to the most frequently asked questions about mastitis and the fight against it: “How does mastitis occur?”, “What are the symptoms of mastitis?” and "Is it possible to breastfeed with mastitis?".
Ask your doctor for more information.
Signs of mastitis
What does mastitis feel like? In addition to pain and discomfort, symptoms of mastitis can also include fatigue and a feeling of exhaustion.
How mastitis manifests:
- fever (>38.5°C) and/or flu-like symptoms;
- nausea;
- vomiting;
- yellowish discharge from the nipple;
- chest warm or hot to the touch;
- pink or red breasts.

These symptoms of mastitis are similar to the symptoms of breast engorgement, but there is a fundamental difference between these conditions. Mastitis differs from engorgement in that it usually only affects one breast, not both.
Causes of mastitis
Mastitis can develop in a new mother at any time, but it usually occurs within the first two to three weeks after childbirth. A common cause of this disease is long breaks between feedings - for example, when the baby begins to sleep through the night.
Other possible causes of mastitis are:
- incorrect breastfeeding;
- incomplete outflow of milk from the mammary glands, for example, due to blockage of the milk duct;
- unattended breast engorgement;
- regular pressure on some part of the breast, wearing tight clothing;
- chest injury caused by injury or impact.
In short: mastitis usually develops as a result of too much milk in the breast, known as milk stasis. Stagnation of milk provokes the growth of bacteria, which causes mastitis and symptoms of pain and fever. Therefore, to prevent mastitis and stagnation of milk, it is important to make sure that it is removed from the breast properly.
Stagnation of milk provokes the growth of bacteria, which causes mastitis and symptoms of pain and fever. Therefore, to prevent mastitis and stagnation of milk, it is important to make sure that it is removed from the breast properly.
Blockage of the milk ducts can also be the cause. Mastitis is indeed caused by milk stagnation or too long milk in the breast, but this condition and the subsequent symptoms of mastitis - fever and pain - are precisely due to the rapid multiplication of bacteria due to milk stagnation.
Prevention of mastitis while breastfeeding
The good news is that there are many ways to prevent mastitis. Below you will find some tips on how to avoid mastitis.
1. Care for your breasts to prevent nipple irritation. Proper breast care can help prevent mastitis by gently massaging and keeping your nipples dry with soft bra pads.
Find out more about breast care in our article here.
2. Feed your baby often. For complete emptying of the breast, it is important to feed regularly and on time. Even if the baby is sleeping, it should be woken up when it's time for feeding. If the mother cannot be with the baby during feeding, she should express milk from the breast using a breast pump.
Feed your baby often. For complete emptying of the breast, it is important to feed regularly and on time. Even if the baby is sleeping, it should be woken up when it's time for feeding. If the mother cannot be with the baby during feeding, she should express milk from the breast using a breast pump.
Choose an easy-to-use breastpump, such as a single electric breastpump. It allows you to express gently and naturally thanks to its special Natural Motion technology. Many of the complications of breastfeeding can be avoided if the baby latch on properly. Try different breastfeeding positions to find one in which the baby will properly latch onto the breast. This will help prevent mastitis and other problems. We talk more about breastfeeding positions in the article at the link.
4. Wean your baby gradually. To minimize the chance of complications, it is necessary to reduce milk production by gradually reducing the number of breastfeeds.
If you're interested in stopping breastfeeding, check out our tips for weaning your baby in the article here.
Treatment of mastitis in women
One of the most common questions that breastfeeding mothers face with mastitis is: “Can I continue to breastfeed?” Answer: yes. What's more, breastfeeding for mastitis can help clear the infection without causing harm or side effects.
An important point: if you have symptoms of mastitis, contact your doctor immediately. Doctors usually prescribe antibiotics (eg, acetaminophen or ibuprofen) to relieve the symptoms of mastitis after making sure the drug is safe for breastfeeding.
Mastitis can be uncomfortable, but there is no reason to panic or despair. This is a common problem that many new mothers experience when breastfeeding for the first time. By following the advice in this article, you can reduce the likelihood of developing mastitis, but if something bothers you, you should seek the help of a specialist.
Articles and tips from Philips Avent
*Lactational mastitis and lactostasis: tactical contraversion.