Newborn baby formula feeding guide
Amount and Schedule of Baby Formula Feedings
- In the first week after birth, babies should be eating no more than about 1 to 2 ounces (30 to 60 ml) per feed.
- During the first month, babies gradually eat more until they take 3 to 4 ounces (90 to 120 ml) per feed, amounting to 32 ounces per day. Formula-fed babies typically feed on a more regular schedule, such as every 3 or 4 hours. Breastfed babies usually take smaller, more frequent feedings than formula-fed infants.
If your baby sleeps longer than 4 to 5 hours during the first few weeks after birth and starts missing feedings, wake them up and offer a bottle.
By the end of the first month: Your baby will be up to at least 3 to 4 ounces (120 mL) per feeding, with a fairly predictable schedule of feedings about every 3 to 4 hours.
By 6 months: Your baby will consume 6 to 8 ounces (180–240 mL) at each of 4 or 5 feedings in 24 hours.
Formula feeding based on body weight
On average, your baby should take in about 2½ ounces (75 mL) of infant formula a day for every pound (453 g) of body weight. But they probably will regulate their intake from day to day to meet their own specific needs, so let them tell you when they've had enough. If they become fidgety or easily distracted during a feeding, they're probably finished. If they drain the bottle and continues smacking their lips, they might still be hungry.
There are high and low limits, however. If your baby consistently seems to want more or less than this, discuss it with your pediatrician. Your baby should usually drink no more than an average of about 32 ounces (960 mL) of formula in 24 hours. Some babies have higher needs for sucking and may just want to suck on a pacifier after feeding.
On-demand feeding
Initially it is best to feed your formula-fed newborn a bottle on demand, or whenever they cry with hunger. As time passes, your baby will begin to develop a fairly regular timetable of their own. As you become familiar with their signals and needs, you'll be able to schedule their feedings around their routine.
As time passes, your baby will begin to develop a fairly regular timetable of their own. As you become familiar with their signals and needs, you'll be able to schedule their feedings around their routine.
Eating & sleeping patterns
Between 2 and 4 months of age (or when the baby weighs more than 12 lb. [5.4 kg]), most formula-fed babies no longer need a middle-of-the-night feedings. They're consuming more during the day, and their sleeping patterns have become more regular (although this varies considerably from baby to baby). Their stomach capacity has increased, too, which means they may go longer between daytime feedings—occasionally up to 4 or 5 hours at a time.
If your baby still seems to feed very frequently or consume larger amounts, try distracting them with play or with a pacifier. Sometimes patterns of obesity begin during infancy, so it is important not to overfeed your baby.
Getting to know your baby's feeding needs
The most important thing to remember, whether you breastfeed or bottlefeed, is that your baby's feeding needs are unique. No book―or website―can tell you precisely how much or how often they need to be fed or exactly how you should handle them during feedings. You will discover these things for yourself as you and your baby get to know each other.
No book―or website―can tell you precisely how much or how often they need to be fed or exactly how you should handle them during feedings. You will discover these things for yourself as you and your baby get to know each other.
More information
- How Often and How Much Should Your Baby Eat?
- Making Sure Your Baby is Getting Enough Milk
- Is Your Baby Hungry or Full? Responsive Feeding Explained (Video)
- Remedies for Spitty Babies
- Last Updated
- 5/16/2022
- Source
- Adapted from Caring for Your Baby and Young Child: Birth to Age 5 7th Edition (Copyright © 2019 American Academy of Pediatrics)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
How Often and How Much Should Your Baby Eat?
By: Sanjeev Jain, MD, FAAP
One of the most common questions new parents have is how often their baby should eat. The best answer is surprisingly simple: in general, babies should be fed whenever they seem hungry.
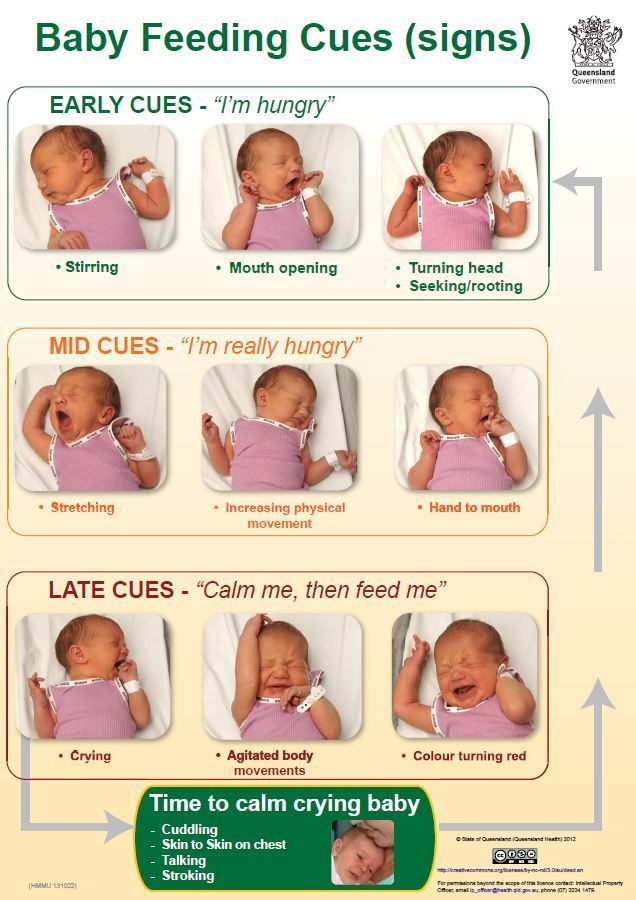
How do I know when my baby is hungry?
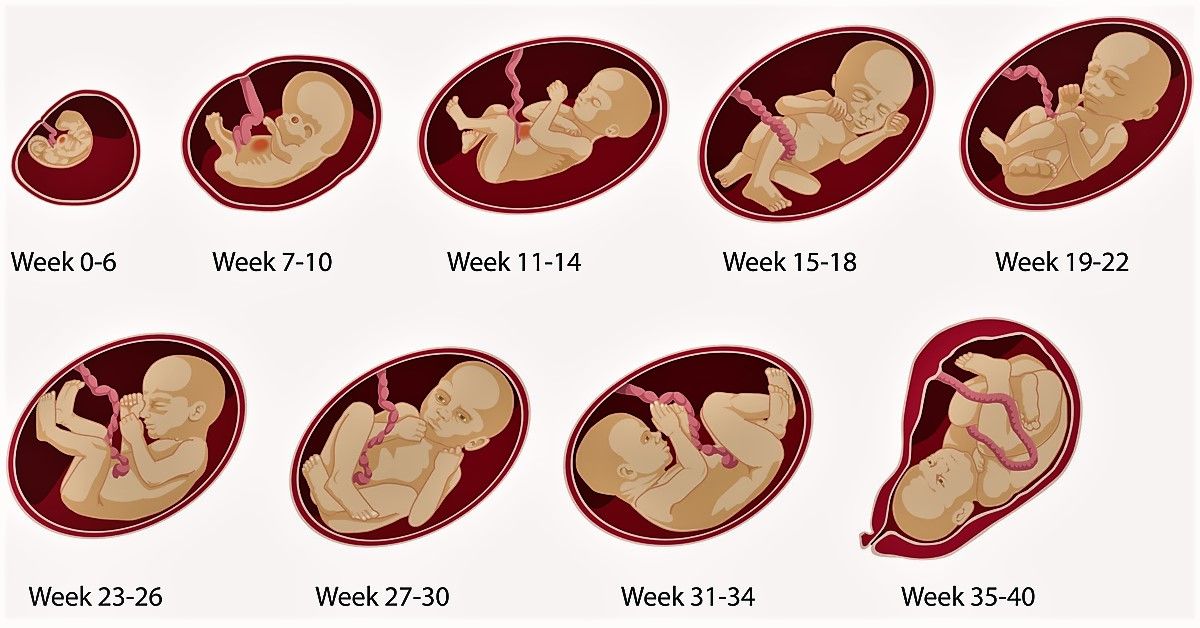
For babies born
prematurely or with certain medical conditions, scheduled feedings advised by your pediatrician are best. But for most healthy, full-term infants, parents can look to their baby rather than the clock for hunger cues. This is called feeding on demand, or
responsive feeding.
Hunger cues
A hungry baby often will cry. But it's best to watch for hunger cues before the baby starts
crying, which is a late sign of hunger and can make it hard for them to settle down and eat.
Some other typical hunger cues in babies:
Licking lips
Sticking tongue out
Rooting (moving jaw and mouth or head in search of breast)
Putting his/her hand to mouth repeatedly
Opening her mouth
Fussiness
Sucking on everything around
It is important to realize, however, that every time your baby cries or sucks it is not necessarily because he or she is hungry. Babies suck not only for hunger, but also for comfort; it can be hard at first for parents to tell the difference. Sometimes, your baby just needs to be cuddled or changed.
General guidelines for baby feeding
It is important to remember all babies are different―some like to snack more often, and others drink more at one time and go longer between feedings. However, most babies will drink more and go longer between feedings as they get bigger and their tummies can hold more milk:
Most newborns eat every 2 to 3 hours, or 8 to 12 times every 24 hours.
 Babies might only take in half ounce per feeding for the first day or two of life, but after that will usually drink 1 to 2 ounces at each feeding. This amount increases to 2 to 3 ounces by 2 weeks of age.
Babies might only take in half ounce per feeding for the first day or two of life, but after that will usually drink 1 to 2 ounces at each feeding. This amount increases to 2 to 3 ounces by 2 weeks of age.At about 2 months of age, babies usually take 4 to 5 ounces per feeding every 3 to 4 hours.
At 4 months, babies usually take 4 to 6 ounces per feeding.
At 6 months, babies may be taking up to 8 ounces every 4 to 5 hours.
Most babies will increase the amount of formula they drink by an average of 1 ounce each month before leveling off at about 7 to 8 ounces per feeding. Solid foods should be started at about 6 months old.
Concerns about overfeeding or underfeeding your baby
Too full?
Babies are usually pretty good at eating the right amount, but they can sometimes take in more than they need. Infants who are
bottle feeding may be more likely to overfeed, because drinking from a bottle may take less effort than
breastfeeding.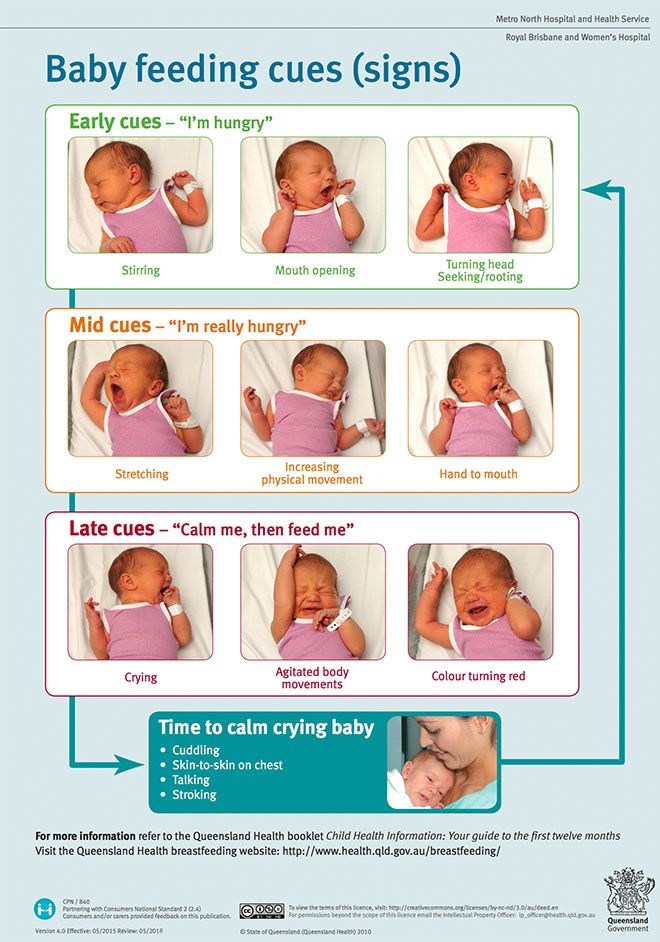
Overfed babies can have stomach pains, gas, spit up or vomit and be at higher risk for obesity later in life. It's better to offer less, since you can always give more if your baby wants it. This also gives babies time to realize when they're full.
If you are concerned your baby wants to eat all the time―even when he or she is full―talk with your pediatrician. Pacifiers may be used after feeding to help sooth healthy-weight babies who like to suck for comfort, rather than nutrition. For babies who are breastfed, it's best to wait to offer pacifiers until around 3 to 4 weeks of age, when breastfeeding is well-established.
Trouble gaining weight?
Most babies will double their birth weight by 5 months of age and triple their birth weight by their first birthday. If your baby is having trouble gaining weight, don't wait too long between feeding―even if it means waking your baby. Be sure to talk with your pediatrician about how often and how much to feed your baby.
How do I know if my baby is getting enough to eat?
Daily diapers
A newborn's diaper is a good indicator of whether he or she is getting enough to eat. In the first few days after birth, a baby should have 2 to 3 wet diapers each day. After the first 4 to 5 days, a baby should have at least 5 to 6 wet diapers a day. Stool frequency is more variable and depends whether your baby is breastfed or formula fed.
Growth charts
During regular health check-ups, your pediatrician will check your baby's weight and plot it on a growth chart. Your baby's progress on the growth chart is one way to tell whether or not they are getting enough food. Babies who stay in healthy growth percentile ranges are probably getting a healthy amount of food during feedings.
Remember
Talk with your pediatrician if you have any questions or concerns about your baby getting the right amount to eat.
More information:
- Making Sure Your Baby is Getting Enough Milk
- Amount and Schedule of Formula Feedings
- Is Your Baby Hungry or Full? Responsive Feeding Explained (Video)
- Remedies for Spitty Babies
- Ask the Pediatrician: With the baby formula shortage, what should I do if I can't find any?
- Ask the Pediatrician: How should we feed our baby if we're running low on money?
-
Airplane Choo Choo: A Feeding Guide for Children (National Dairy Council)
About Dr.
 Jain:
Jain:
Sanjeev Jain, MD, FAAP, is a Clinical Associate Professor of General Pediatrics and Adolescent Medicine at the University of Wisconsin School of Medicine and Public Health. Within the American Academy of Pediatrics, he is a member of the Section on International Child Health and the Wisconsin State Chapter.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
newborn diet on IV, how to properly feed a baby with formula from a bottle
The desire for a child to grow up strong and healthy is natural for mothers. And the health of a newborn begins with proper nutrition. Mother's milk has always been considered the best option for feeding - the most healthy and nutritious food for infants. However, in some cases, breastfeeding is not possible. And then mixtures come to the aid of mothers.
And then mixtures come to the aid of mothers.
Contents: Hide
- In what cases is the transition to artificial feeding
- How to choose a mixture of
- Basic rules of artificial feeding
- Food mode
- Main errors under artificial feeding
in what cases is required an artificial feeding 29000 Medical Medical Medical Medical to breastfeeding. There are a number of diseases in which breast milk is prohibited. On the mother's side, these are HIV, an open form of tuberculosis, dangerous infections, and a serious state of health. On the part of the child, these are leucinosis, galactosemia, and individual food intolerance. It is not necessary to take tests after hearing the terrible names of diseases. All newborns are checked in maternity hospitals for their presence. But allergies are not so easy to identify. Many newborns have skin rashes and redness, which may be due to a reaction to an aggressive environment. Only a strict diet for the mother can help here, so that her milk does not contain allergens, monitoring the baby and consulting a doctor.
Lack of lactation or its complete cessation. This is the second objective reason for transferring a child from breast milk to formula. Lactation does not always come in the right amount and it can be increased. It happens that milk disappears a few days after the birth of the crumbs. This often depends on the individual characteristics of the mother's body. So that the child does not starve, he is first transferred to mixed, and then completely to artificial feeding.
Insufficient nutritional value of mother's milk. Usually this problem can be solved without resorting to the transition to IoT, but this is not always possible. A woman may have a lot of milk, but it will be like water in both color and consistency. In such cases, doctors give advice to the mother on nutrition in order to increase the fat content of milk and its usefulness. If the milk remains watery, the child stops eating, cries of hunger, loses weight. The only way out in this situation is the transition to the mixture.
Impossibility of regular feeding. Children who, for a number of reasons, are separated from their mother for long periods of time are transferred to artificial feeding: the woman is in a hospital, going to work or study, business trips, etc. If the break in breastfeeding is one-time, then restoring lactation and breastfeeding is still possible . However, more often in such cases, breastfeeding has to be abandoned.
Mother's personal wish. Unfortunately, there are cases when a woman, having every opportunity to breastfeed her baby, refuses to breastfeed for various subjective reasons. In this case, lactation is interrupted, and the baby is transferred to the mixture.
Read also: Newborn weight gain by month
How to choose a formula
If you are going to transfer your baby to artificial feeding, then the first thing you will encounter will be the choice of nutrition. Today there are a large number of different mixtures: adapted and non-adapted, dairy and sour-milk, dry and liquid. There are mixtures against regurgitation, hypoallergenic, for premature babies, etc. How to choose the optimal replacement for mother's milk from such a variety?
There are mixtures against regurgitation, hypoallergenic, for premature babies, etc. How to choose the optimal replacement for mother's milk from such a variety?
- Make your choice only after consulting a pediatrician. The doctor will examine the baby and give all the necessary recommendations.
- Monitor your child. When adapting to a new diet, the child may have small rashes, but they disappear if the body begins to absorb the mixture normally. The baby eats with appetite, he has a normal stool and no colic. Otherwise, the mixture must be changed.
- If it is necessary to replace the mixture with a thicker formula (anti spit up), choose the same brand of food that was previously used.
- Consider the age of the baby. All mixtures have a gradation by months of life.
- Prefer adapted formulas, they are usually easier to digest
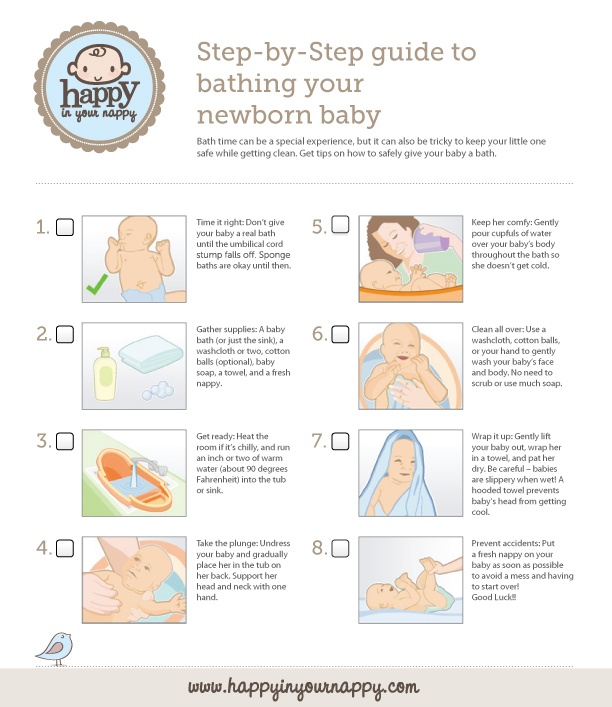
Basic rules for artificial feeding save you a lot of problems.
1. Choose proven blends. This applies not only to the choice of brand, but also to the packaging itself. Look at its integrity, check the expiration date.
This applies not only to the choice of brand, but also to the packaging itself. Look at its integrity, check the expiration date.
2. Observe the storage conditions for opened packaging at home (in a dry and cool place, but in no case in the refrigerator, the mixture must not become damp). Remember that the open mixture is stored for three weeks. After this period, it can no longer be used.
3. Strictly follow the instructions when preparing meals. It is indicated on the packaging. Water for the preparation of the mixture must be purified and boiled. The optimal temperature for preparing the mixture is 36–37 °C. You can cook food right in the bottle. This is quite convenient, since baby bottles have a volume scale that makes it easier to calculate the right amount of scoops. The mixture must be stirred until completely dissolved, and then cooled to an acceptable temperature so that the baby can drink without burning himself. You can check if the milk is hot by dropping it on your wrist - there the skin is most tender and sensitive. If the temperature is almost not felt, then the mixture can be given to the child.
If the temperature is almost not felt, then the mixture can be given to the child.
4. Sterilize baby dishes. Baby bottles and nipples should be thoroughly rinsed using a special brush so that no food residue remains. You can use children's dishwashing detergents. Do not wash bottles with common cleaning products that you are used to using, no matter how good they are. After washing, be sure to place the dishes in boiling water. This helps to kill harmful bacteria. It is recommended to sterilize children's dishes during the entire first year of a baby's life. Then you can limit yourself to just a thorough wash.
5. Hold the bottle in a semi-vertical position when feeding. The milk should completely fill the nipple. This prevents the child from swallowing air. After feeding, it is necessary to hold the baby in a column for several minutes to avoid spitting up.
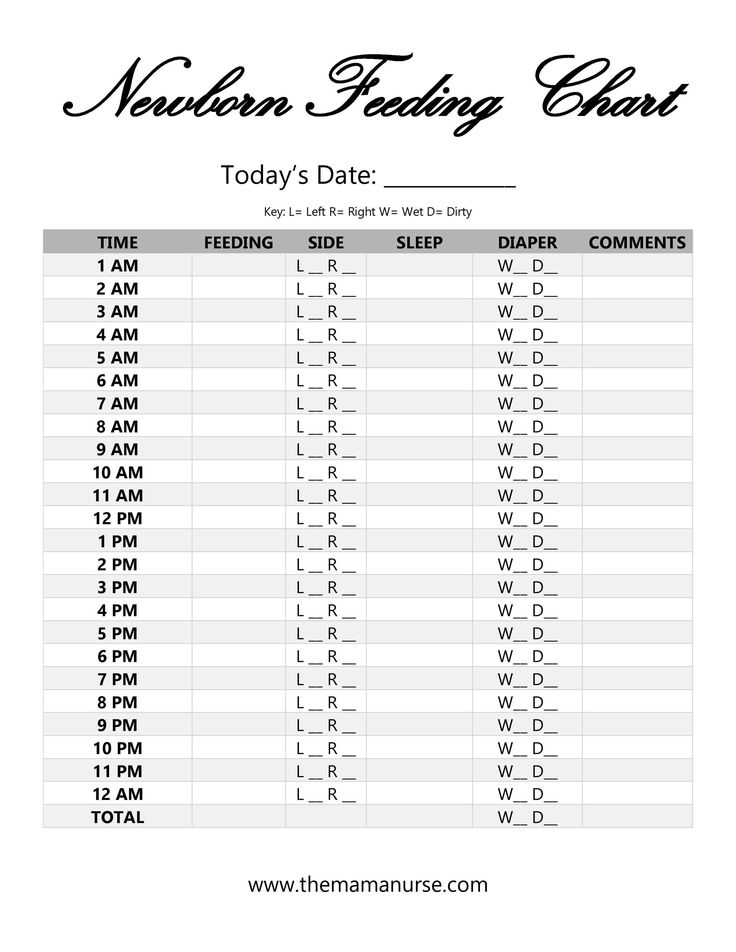
6. Monitor the amount of formula consumed and the feeding schedule. Maintaining a balance is extremely important for the healthy and full development of the baby.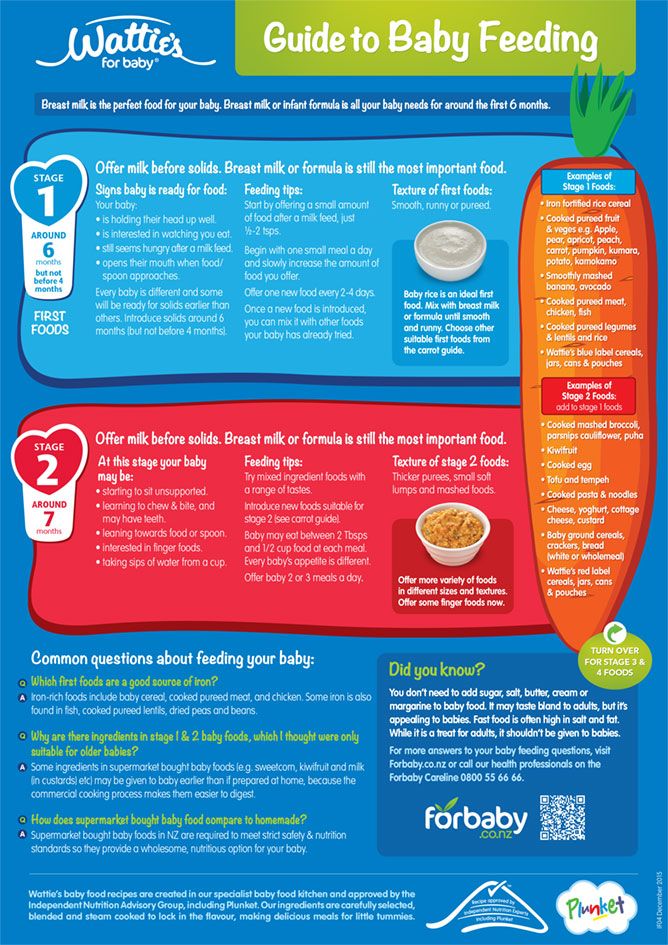
- Calculate the amount of formula to be prepared based on the baby's weight. It is body weight, and not the age of the crumbs, that is the main indicator when calculating the daily nutritional intake. You can find out the required volume of the mixture for feeding either at a pediatrician’s appointment, or on your own (it is recommended to use Maslov’s caloric method when calculating).
- Observe breaks between feedings. During the day they should be 3.5 hours, at night - 6. Try not to break the schedule.
- Give your child water. Supplementation with water is a necessity for artificial feeding. Water should be given somewhere in the middle of the interval between feedings or 10-15 minutes after it. Avoid supplementation before meals.
Major mistakes in artificial feeding
Overfeeding. The desire to feed the child is understandable, but in the case of mixtures, feeding must be approached strictly. On artificial feeding, the child is normally gaining weight very well. Excess body weight is an additional burden on the body and health problems. Even an adult can find it difficult to cope with problems from being overweight. What to say about the tiny weak body of a newborn? Follow the diet and control the daily milk intake. Fortunately, you can always see how much the child ate.
Excess body weight is an additional burden on the body and health problems. Even an adult can find it difficult to cope with problems from being overweight. What to say about the tiny weak body of a newborn? Follow the diet and control the daily milk intake. Fortunately, you can always see how much the child ate.
Unreasonable mixture change. If the child eats the current mixture well, then it is not necessary to change it. The baby will have to go through a difficult period of adaptation again, and it’s not a fact that his body will accept new food just as well.
Use of old mix. The child's food must be fresh. If the child has not finished eating, then literally after half an hour the milk can only be poured out. Milk mixtures are an excellent environment for the life of pathogenic bacteria.
Pet milk feeding. Do you think this is a more natural option than artificial mixtures? This is an erroneous opinion. For a child under one year old, cow or goat milk, even boiled, is strictly prohibited. The composition of such milk is very different from that of women, which can lead to the development of allergies, diseases, problems with the skeletal system in the baby.
The composition of such milk is very different from that of women, which can lead to the development of allergies, diseases, problems with the skeletal system in the baby.
If you have any doubts about your baby's nutrition, please consult neonatologists and paediatricians. Do not rush to make decisions without expert advice. After all, nothing is more important than your baby's health.
#Nutrition for children up to a year
Breast milk and formula: what do they have in common?
1 Cribb VL et al. Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. EUR J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Klin Nutr. 2012;66(1):104.
Yur J Klin Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity." Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells. " Adv. 2014;5(6):770-778.
" Adv. 2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clinic Transl Immunology . - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby. " Glycobiology (Glycobiology). 2012;22(9):1147-1162.
" Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development." J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR. Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child.2010;95(12):1004-1008.
" Arch Dis Child.2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis.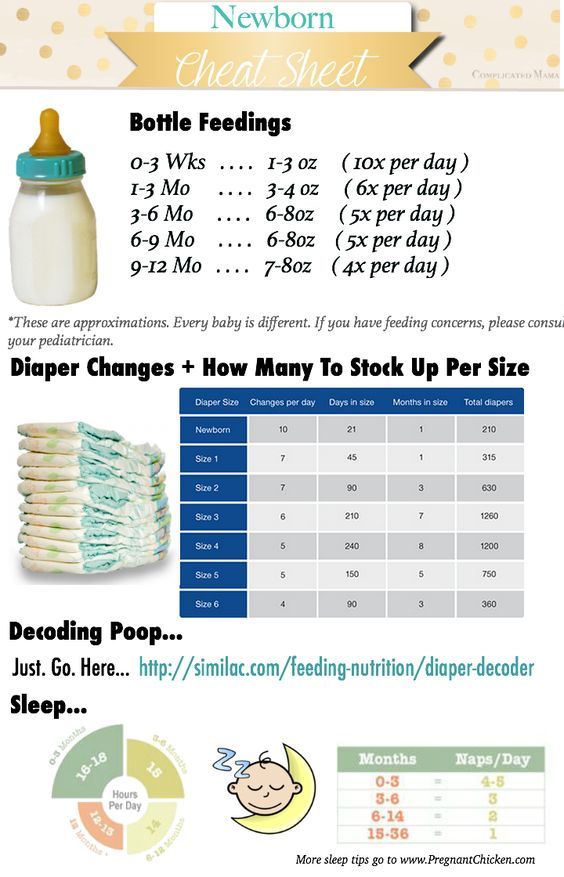 Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263. - Lund-Blix N.A. et al., Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: a MIDIA study ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review01 JAMA Pediatr 2015;169(6): e 151025. - Amitai I. L., Keinan-Bocker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrics 2015;169(6):e151025.
L., Keinan-Bocker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrics 2015;169(6):e151025.
25 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatrician. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects".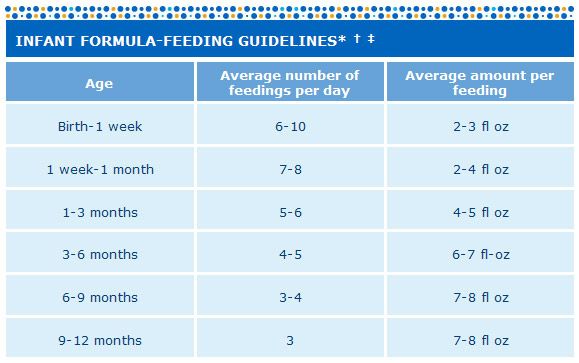 Lancet (Lancet). 2016;387(10017):475-490.
Lancet (Lancet). 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginecol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas W Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
31 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, 20 January 2011 [cited 4 April 2018]
32 Doan T et al. Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs . 2007;21(3):200-206. - Dawn T. et al.