Newborn baby not feeding enough
Is My New Baby Eating Enough? What is the Right Amount?
Written by Stephanie Booth
In this Article
- How Much Do Babies Eat?
- Signs That Your Baby Is Eating Enough
- Signs That Your Baby Isn’t Eating Enough
No matter how prepared you think you are, you’ll still have questions once your newborn arrives. One of the most common worries new parents have? Whether their little one is eating the right amount.
Every baby is unique, but there are some basic guidelines to keep in mind when it’s time for a feeding.
How Much Do Babies Eat?
Newborn to 2 months: During their first month, babies need to eat 8-12 times each day. That’s about once every 2-3 hours. Some who are breastfeeding, though, can eat every 1.5 hours, and up to 15 times a day. If your baby isn’t waking up on their own for a feeding during the first few weeks, you should get them up to eat on schedule.
If you’re breastfeeding, your little one will spend about 10 to 20 minutes on your breast. Some may nurse for longer, but make sure they are actually sucking and swallowing the whole time.
Giving formula? Plan on your baby drinking 1.5 to 3 ounces at each feeding.
After about a month, they’ll start eating at least 4 ounces at each feeding. As breastfed babies get the hang of nursing, they’ll get more milk from you, too. You may not notice, though, since they’ll do it in less time.
Whether you’re nursing or bottle feeding, as your baby keeps growing, so will their appetite.
At 2 months, they may drink 4-5 ounces at each feeding, 3-4 hours apart.
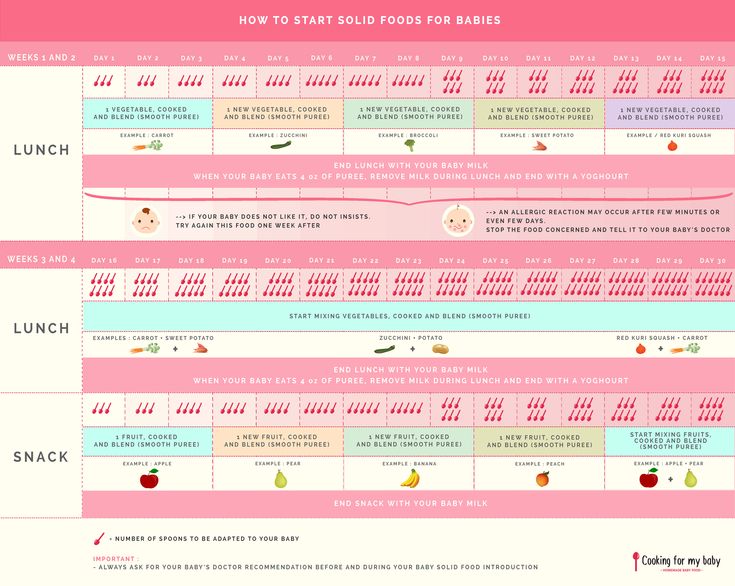
At 4 months, they may need up to 6 ounces every time. The pediatrician may encourage you to start to introduce solid foods - or advise you to wait if you are still exclusively breastfeeding.
By 6 months, some babies drink as much as 8 ounces of breastmilk or formula even as they go longer between feedings.
Remember: The exact amount your little one drinks will vary from day to day.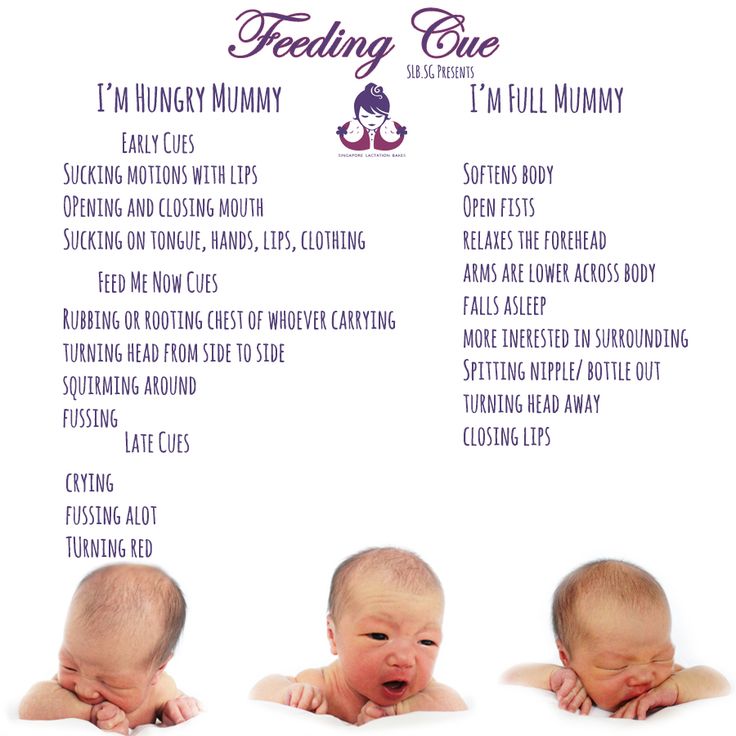 For instance, they may want to eat more than normal when they are going through a growth spurt. Trust your baby to know how much food they need.
For instance, they may want to eat more than normal when they are going through a growth spurt. Trust your baby to know how much food they need.
You can watch for a few signs that they are full:
- They pull away from your breast or their bottle
- They fall asleep during a feeding
- They shake their head or keep their mouth closed
Those signs can also help you know that you’re not overfeeding your little one. And at regular checkups, your pediatrician will let you know if your baby’s growth (height and weight) is on track.
Signs That Your Baby Is Eating Enough
When they are getting the right amount of food, you’ll see:
Plenty of wet diapers. The first few days after birth, they may only wet one or two diapers each day. After that, they should need six to eight cloth (five or six disposable) diaper changes every 24 hours, plus have two to five poopy ones each day.
Steady weight gain. After the first 2 weeks, your baby should gain about 4-7 ounces per week until their sixth month, and 3-5 ounces from 6 to 18 months.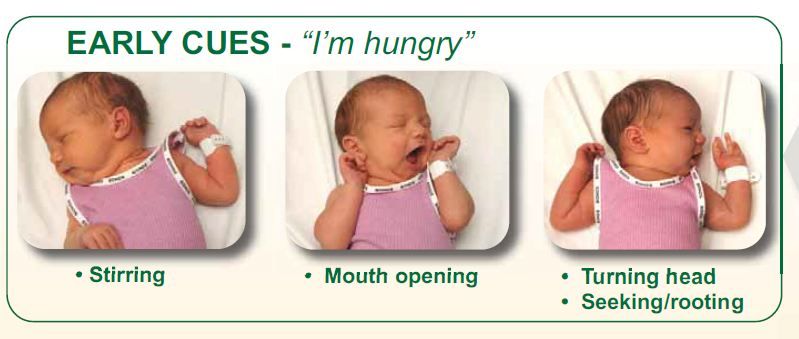
Your baby is active and happy. A child that’s eating well will look alert and be active. They’ll also seem content between feedings.
Signs That Your Baby Isn’t Eating Enough
Reasons to call your doctor include:
- Dark pee or orange crystals in their diaper
- They would rather sleep than eat
- They won’t latch onto your breast, or they pull away from you
- They are fussy right after feedings
- They wet fewer diapers
As a new parent, it’s key to learn to trust your instincts. If you have any concerns about your baby’s eating, check in with their doctor.
Signs baby isn’t getting enough breastmilk
Every parent wants to do everything they can to help their child grow healthy and strong. And breastfeeding is one of the best things you can do for your baby. But it doesn’t always go smoothly, especially when you’re just starting out. So, you may wonder at some point: Is my baby getting enough breastmilk? How can I tell?
Try not to worry. We have a team of breastfeeding and lactation experts to help you and your baby work through breastfeeding challenges.
We have a team of breastfeeding and lactation experts to help you and your baby work through breastfeeding challenges.
Read on to learn how to tell if baby is getting enough breastmilk, some suggestions to help make sure baby gets enough to eat, and when you should make an appointment with your baby’s doctor or a lactation consultant.
How do I know if my newborn is eating enough?
If you’re exclusively feeding your baby from the breast, rather than pumping to bottle feed, it’s hard to tell exactly how much your baby is eating. Here are six signs your baby is getting enough breastmilk.
1. Baby is feeding regularly
Babies breastfeed frequently and often in clusters. Frequent, effective feedings help your baby grow, and help ensure you have enough breastmilk for the next feeding.
During the first two months, expect your baby to nurse 10 to 12 times in a 24-hour period. In the beginning, each breastfeeding session will likely take between 20 to 45 minutes. If you are feeding your baby less than eight times a day, or if the sessions are very short or very long, you should talk to your baby’s doctor.
If you are feeding your baby less than eight times a day, or if the sessions are very short or very long, you should talk to your baby’s doctor.
As your baby grows comfortable with nursing and gets a little older, they’ll be able to get what they need in a shorter amount of time – and with fewer nursing sessions.
2. Baby is swallowing during feeding
When baby first latches onto your breast, they will suck rapidly to get the milk flowing. But once things are going, the sucking will become slower and deeper as they pull the milk into their mouth and swallow.
Watch baby’s jaw for movement and listen for swallowing sounds. If you see baby’s jaw move or hear them swallowing, they’re getting at least some breastmilk.
If baby isn’t getting enough milk, their sucking may not progress to that slower, rhythmic pulling. Baby may also fall asleep at the breast, take long breaks while breastfeeding or give up within a couple minutes.
3. Baby is content and happy
If your baby seems satisfied after breastfeeding, they’re likely getting enough milk. But if they always want to nurse, it may be a sign that baby is still hungry after breastfeeding – especially if they appear sluggish or they’re losing weight.
But if they always want to nurse, it may be a sign that baby is still hungry after breastfeeding – especially if they appear sluggish or they’re losing weight.
4. Your breasts feel softer and not as full after feeding
Your breasts should feel softer at the end of a feeding. Emptying as much milk from your breasts as possible will help create more supply for the next feeding.
If you’re worried about your milk supply or that you’re not eating the right things for breastfeeding, here’s some good news: Nearly all moms produce enough breastmilk to feed baby without any major changes to their diet.
Breastfeeding can be uncomfortable at times, but it shouldn’t be painful. Pain in the breasts or nipples can be cause for concern. So if you are experiencing pain, talk to your baby’s doctor or a lactation consultant about it.
5. Baby is gaining weight as expected
It’s normal for a newborn’s weight to fluctuate during the first few days of their life. Typically, by day 10, a baby’s weight has rebounded to their birth weight. Until 6 months of age, babies usually gain between 5 and 8 ounces a week. At five months, your baby’s weight should be double what it was at birth.
Until 6 months of age, babies usually gain between 5 and 8 ounces a week. At five months, your baby’s weight should be double what it was at birth.
6. You’re changing a lot of diapers each day
Diaper duty starts small but, before you know it, those diapers pile up.
How many dirty diapers should a newborn have per day? And what about poopy diapers? One thing that’s helpful to remember is that during their first week, your baby will have about the same number of wet and poopy diapers as the days of their life. After that, parents can expect to change eight to 10 diapers each day.
- Day 1: At least one wet and one poop
- Day 2: At least two wets and two poops
- Day 3: At least three wets and three poops
- Day 4: At least four wets and four poops (from this point, poops should be yellowish in color)
- Day 5 and beyond: At least 5-6 wets and 3-4 poops
[ Click on the image below to enlarge and view it in a new window ]
That’s a lot of dirty diapers! To keep baby’s skin healthy, change them as soon you can and make sure to get into all the folds of baby’s skin when cleaning out the poop.
Also pay attention to your little one’s bottom. If you notice redness, bumps or signs of severe diaper rash, talk to your baby’s doctor about what you can do.
How to help your baby feed more effectively
It’s often said that timing is everything. This is certainly true when it comes to breastfeeding sessions, as well as when to introduce bottle feeding and pacifiers.
Watch for cues that your baby is hungry
You can help make sure your baby is eating enough by looking for opportunities to breastfeed, rather than waiting until baby is upset and crying.
If your baby is hungry, they’ll let you know in a variety of ways ranging from subtle suggestions to outright demands. We talk about these in terms of early cues, mid cues and late cues.
Early hunger cues can include stirring from sleep, opening their mouth or turning their head toward your breast when you stroke the corner of their mouth.
If you don’t respond to these early cues, baby has other ways to let you know – which brings us to mid cues. Some common mid cues are stretching, becoming more physically active and bringing their hand to their mouth.
Some common mid cues are stretching, becoming more physically active and bringing their hand to their mouth.
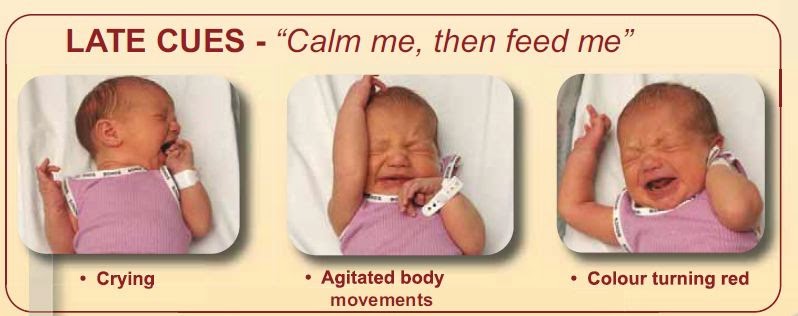
If these mid-cues don’t result in a breastfeeding session, baby will take drastic measures to let you know that they are really, really hungry. They’ll cry and howl. They’ll flail their arms and legs around. They’ll turn red from all the exertion. These are late feeding cues and at this point, baby is often too upset to eat. So, you’ll need to calm them before you can feed them.
By feeding your baby when you see an early cue, you can help keep feedings calm and effective. It’s so much easier for baby to focus on getting enough to eat if they aren’t using all their energy expressing the big emotions they’re feeling.
This poster shows what baby’s feeding cues may look like.
[ Click on the image below to enlarge and view it in a new window ]
Only introduce a bottle or pacifier when the time is right
Bottles and pacifiers encourage a different type of sucking than breastfeeding. So you’ll want to wait until your little one is fully comfortable with breastfeeding before introducing either.
So you’ll want to wait until your little one is fully comfortable with breastfeeding before introducing either.
Most babies really latch on to breastfeeding by about two to four weeks after their birth. But for some, especially those who were born early, it can be longer.
You also don’t want to wait too long for baby’s first bottle. Introducing a bottle too late can be one reason why babies refuse a bottle. A lactation consultant or your child’s doctor can help you figure out the best way to start the breast to bottle transition.
Pacifiers are great for soothing and a recommendation for safe sleep for babies, but like with the bottle, hold off until baby has gotten really good at breastfeeding – usually about a month.
Signs your baby
isn’t getting enough breastmilkBreastfeeding is a little different for every parent and baby. But there are a few signs baby may not be getting enough to eat to watch for:
- Baby is sluggish or sleeping longer than usual.
 This is especially something to watch for in newborns. Because they are so little, newborns need to eat every 2-4 hours.
This is especially something to watch for in newborns. Because they are so little, newborns need to eat every 2-4 hours. - Feedings are too long or too short. If baby’s not getting enough milk, they may quickly give up on nursing after a couple minutes. Or, they may keep trying for over an hour.
- Latching is really painful for you or it appears that baby hasn’t latched deeply enough.
- Baby is not producing stools or their urine is not pale.
- Baby isn’t gaining weight.
What to do if baby isn’t eating enough breastmilk
If you think your baby isn’t getting enough breastmilk, get breastfeeding support from your baby’s doctor or a lactation consultant. They can help you and your baby work through latching problems, low milk supply and feeding positions, and identify any underlying problems like tongue-tie. Just like you support your baby with breastmilk, they’re here to support you!
Choose a location and call to make an appointment with a lactation consultant
The birth of a small child is not uncommon today. Often, such babies are born on time or a little earlier, but due to a lack of weight, they can significantly lag behind their peers in development. Pediatricians and neuropathologists closely monitor the child's condition, because a child's body weight deficiency is a risk factor for changes in the neurological status, functional disorders of the cardiovascular and autonomic nervous systems. But because of their weakness, underweight children do not eat well, and the rate of weight gain in children born with low body weight determines their further physical and psychomotor development and the formation of the immune system.
Often, such babies are born on time or a little earlier, but due to a lack of weight, they can significantly lag behind their peers in development. Pediatricians and neuropathologists closely monitor the child's condition, because a child's body weight deficiency is a risk factor for changes in the neurological status, functional disorders of the cardiovascular and autonomic nervous systems. But because of their weakness, underweight children do not eat well, and the rate of weight gain in children born with low body weight determines their further physical and psychomotor development and the formation of the immune system.
How much should a newborn gain in weight?
To assess the development of your child and the compliance with the norm of the main indicators (height, weight), you can contact a pediatrician or independently - according to existing tables. In the first months, the child is actively growing, adding up to 25-60 grams per day. Small children with adequate nutrition can increase body weight more intensively than their peers. For the first month of life, children should gain up to 1.3-1.7 kg. After 5-6 months of life, the intensity of weight gain decreases somewhat - in 30 days, the increase can be only 400-700 grams.
For the first month of life, children should gain up to 1.3-1.7 kg. After 5-6 months of life, the intensity of weight gain decreases somewhat - in 30 days, the increase can be only 400-700 grams.
The length of the child's body during the first month increases by 4-7 cm, and after 5-6 months of life, growth is added less intensively - by 2-3 cm. But parents should understand that these figures are approximate. Each child is individual. Its weight and height depend on many factors: heredity, the quality of the mother's nutrition, the state of health of the newborn, the severity of childbirth.
Why is the child not gaining weight well?
The main cause of underweight in the neonatal period is the baby's refusal to breastfeed. Small children have poor appetite and spend most of the day sleeping. Often, parents have to wake up the child for a long time, and after a few minutes of sucking on the breast or a bottle of formula, the newborn falls asleep again. Children are especially sleepy, in whom pronounced physiological jaundice was observed in the first days of life.
As a result, after the next weighing, the doctor can tell the mother that the newborn has not gained weight at all or the increase is insignificant. If the situation does not improve for several months, the mother and baby may be hospitalized for a comprehensive examination and tube feeding in a hospital setting.
Sometimes the cause of low weight gain lies in non-compliance with breastfeeding tactics. Pediatricians recommend applying the baby to only one breast during feeding so that it sucks out the "hind" milk, which is of particular energy value and rich in nutrients. Due to their inexperience, mothers offer both breasts to newborns. In this case, the child sucks the upper milk without making any effort and quickly falls asleep, slightly satisfying his hunger.
If the baby has had an infectious disease, has been ill for a long time, suffered from a high temperature or an intestinal disorder, then the monthly weight gain may be significantly less than usual.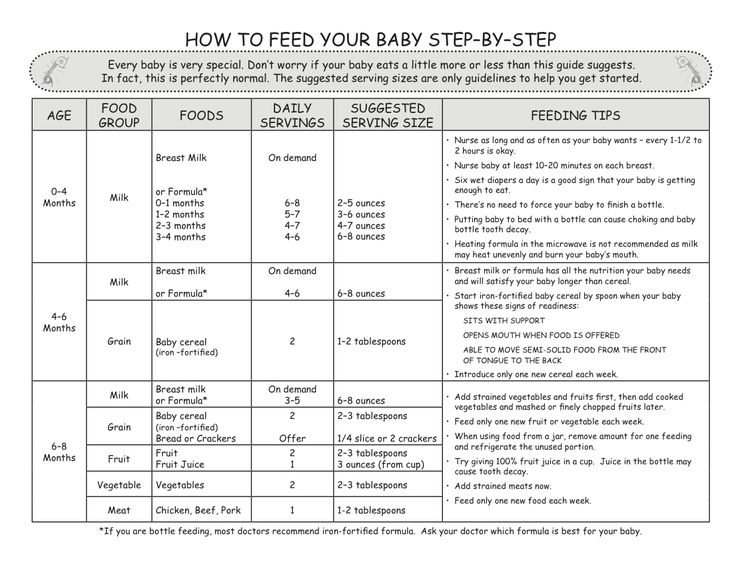 In this case, the timing of the introduction of complementary foods is also shifted, and during the period of illness, in general, many children practically refuse to eat, which is reflected in their weight. Parents should actively communicate with the pediatrician, if necessary, ask him questions of interest and adhere to all recommendations.
In this case, the timing of the introduction of complementary foods is also shifted, and during the period of illness, in general, many children practically refuse to eat, which is reflected in their weight. Parents should actively communicate with the pediatrician, if necessary, ask him questions of interest and adhere to all recommendations.
How to help a child gain weight and catch up with his peers in his development?
If you are breastfeeding, pay special attention to your diet. Drink as much liquid as possible: low-fat milk, compotes, hypoallergenic juices. Your diet must include boiled or baked meat. Take extra vitamins (as advised by the doctor). Breastfeed your baby immediately after waking up, when he is active, in a good mood and does not want to sleep.
But sometimes women's milk is produced in insufficient quantities or the baby does not have enough strength to suck it out. In this case, it is necessary to start supplementing with special infant formula as soon as possible. For children prone to allergic reactions, special hypoallergenic products are intended, which can be bought at a pharmacy, having previously discussed the mixture option with a pediatric nutritionist or pediatrician. Small babies are not adapted to intensive sucking, so the nipple on the bottle must be soft and pliable so that the child can fill up without problems.
For children prone to allergic reactions, special hypoallergenic products are intended, which can be bought at a pharmacy, having previously discussed the mixture option with a pediatric nutritionist or pediatrician. Small babies are not adapted to intensive sucking, so the nipple on the bottle must be soft and pliable so that the child can fill up without problems.
In addition, in order to increase the rate of weight gain and, accordingly, for the proper growth and development of the child, it is recommended to give courses of preparations containing L-carnitine (levorcarnitine), an essential vitamin-like substance that has anabolic properties and has proven itself to normalize body weight in case of its deficiency. In addition, by increasing the secretory and enzymatic activity of gastric and intestinal juices, appetite and digestion improve. One of these drugs is Elkar, containing an aqueous solution of L-carnitine. Elkar is included in the "National program for optimizing the feeding of children in the first year of life" as a means of correcting malnutrition of the II degree.
In children, in contrast to the adult body, where levocarnitine is among the substances produced, the synthesis of this compound covers only 1% of the required amount. Of course, the required amount of L-carnitine is found in breast milk, but if natural feeding is impaired or impossible, the drug must be added to the diet.
In underweight children, psychomotor development is often retarded, which can subsequently manifest itself in the form of speech defects, instability of the nervous system. Elcar improves the energy supply of brain activity, which will help to avoid or reduce the degree of development of functional failure in various areas of the child's neuropsychic response (motor, emotional-motivational, vegetative, cognitive spheres).
Another very important point: levocarnitine improves immunity, which is vital for small children, since almost all of them are predisposed to the development of infectious diseases.
The rate of weight gain is influenced by many external and internal factors. The task of parents is to help the crumbs get stronger as soon as possible. Walk more with your child in the fresh air so that his body receives the necessary amount of oxygen. And don't forget to visit your pediatrician. Small children need professional medical supervision and the attention of loved ones.
The task of parents is to help the crumbs get stronger as soon as possible. Walk more with your child in the fresh air so that his body receives the necessary amount of oxygen. And don't forget to visit your pediatrician. Small children need professional medical supervision and the attention of loved ones.
dysbacteriosis, lactase deficiency and culture of milk for sterility
MainLibraryHelp for motherNewborn diseases: dysbacteriosis, lactase deficiency ..?
Once I received a task from my management to answer the question of our American colleague, a breastfeeding consultant from the La Lache League: "At parental conferences on the Internet, Russian mothers very often discuss three issues: lactase deficiency, dysbacteriosis and sowing milk for sterility . What is meant?"
The first two conditions are reminiscent of what they, in LLL, call foremilk imbalance and hindmilk imbalance and dysbiosis. But these conditions are not a terrible pathology, and on the sites they are discussed from this point of view. About sowing milk for sterility - the American asked at all, why is it carried out??
About sowing milk for sterility - the American asked at all, why is it carried out??
I'll start in order.
Lactase deficiency (or lactose intolerance)
According to specialized literature, carbohydrate metabolism diseases associated with changes in the activity of enzymes that break down sugars, including lactose, are extremely rare in the population. The data for different countries are different. The frequency of such diseases varies from 1 in 20,000 to 1 in 200,000 children. Why do pediatricians talk about lactose intolerance in almost every second child?
How could mankind survive if this disease, which leads, for example, to malnutrition in the absence of treatment and death, occurs in most infants? Mankind has been able to survive to this day because true lactose intolerance, which is genetically determined and associated with the complete absence or serious deficiency of essential enzymes, is very rare. What happens very often? What are modern doctors constantly faced with? With lactose intolerance, formed as a result of improperly organized breastfeeding.
If a mother feeds a child 6-7 times a day, “saves” milk for feeding, expresses after feedings, transfers the child to one or the other breast during feeding, the likelihood of developing lactose intolerance is very high. This is the same lactose intolerance, the cause of which is an imbalance between the "front" and "back" portions of milk. It turns out that the child feeds mainly on the "front" portion of milk, more liquid, containing a large amount of lactose. In the breast between feedings, mainly “front” milk is also collected, “hind” milk, thick, more fatty, is formed mainly during the sucking of the child. If the mother shifts the baby 5-10 minutes after the start of feeding to the other breast, he will suck the front milk out of it. Mom is pumping her hind milk. The baby will not put on weight very well, sometimes just a little. He may have loose stools with greens and foam. Mom will think that she has bad milk, although there is a lot of it.
The same situation can occur if the mother restricts the child from suckling, for example, strictly for 15-20 minutes.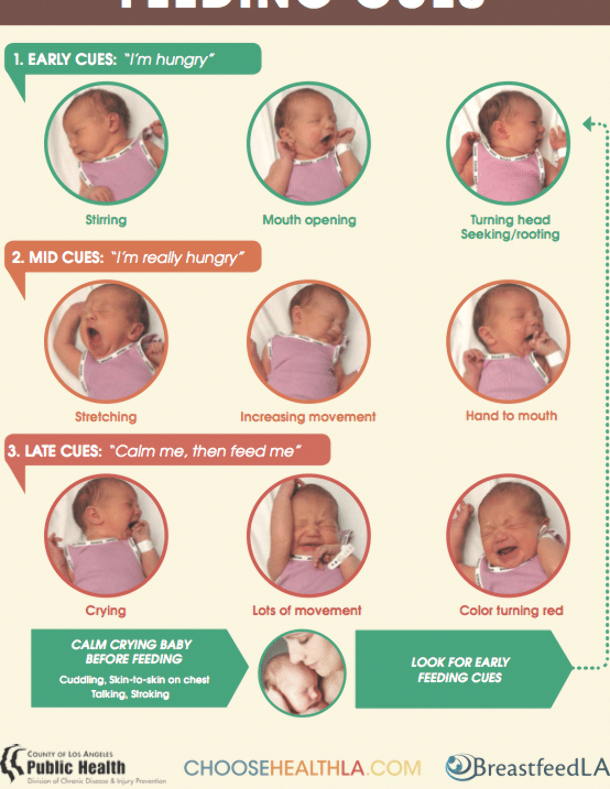 The baby often does not have time to get to the "hind" milk. And besides, he does not sufficiently stimulate the breast to produce milk if he sucks 6-7 times a day for 15-20 minutes. Therefore, in parallel, in the situations described above, a lack of milk will develop. When a child begins to be fed with a lactose-free formula, he will begin to get fat, everyone will breathe a sigh of relief, and the myth that milk can be bad and is generally scarce in modern women will be strengthened in the mind. There is also transient, temporary lactase deficiency. A child on properly organized breastfeeding, with a good weight gain, in general with good health, in the first 2-3 months of life (and sometimes longer) has a frothy stool. If mom tells the doctor about this, an examination will be scheduled, sugars will be found in the analysis. The baby will be switched to a lactose-free formula. However, incomplete absorption of lactose is common for a breastfed baby!!! (66% of children at 6 weeks of age and 60% of children at 3 months of age).
The baby often does not have time to get to the "hind" milk. And besides, he does not sufficiently stimulate the breast to produce milk if he sucks 6-7 times a day for 15-20 minutes. Therefore, in parallel, in the situations described above, a lack of milk will develop. When a child begins to be fed with a lactose-free formula, he will begin to get fat, everyone will breathe a sigh of relief, and the myth that milk can be bad and is generally scarce in modern women will be strengthened in the mind. There is also transient, temporary lactase deficiency. A child on properly organized breastfeeding, with a good weight gain, in general with good health, in the first 2-3 months of life (and sometimes longer) has a frothy stool. If mom tells the doctor about this, an examination will be scheduled, sugars will be found in the analysis. The baby will be switched to a lactose-free formula. However, incomplete absorption of lactose is common for a breastfed baby!!! (66% of children at 6 weeks of age and 60% of children at 3 months of age).
One mother, for example, was told in such a situation: “Your child is in severe pain! Look at his gas formation! And you continue to feed him with your milk! It is poison for him!!!” I am not saying that all doctors act this way. I know pediatricians who, seeing that the child is quite well, do not begin to treat him, relying only on the laboratory results obtained, and do not even prescribe unnecessary examinations! Let's remember that for the past 50 years, doctors have dealt primarily with children who were fed formula. Accordingly, much knowledge and laboratory tests are applicable only to this group of children. The presence of sugar in the stool of a formula-fed baby is a pathology. The presence of sugar in the stool of a breastfed baby is normal!
A significant amount of sugar may be the result of incorrect recommendations for feeding the child (frequent breast changes during feeding, limiting the duration of suckling, pumping after feeding), because. the baby gets plenty of lactose-rich foremilk. Lactose intolerance and a newborn baby - an unheard of combination!!!
Lactose intolerance and a newborn baby - an unheard of combination!!!
Neonatal dysbacteriosis
This condition is unusually popular. The baby, as you know, is born with a sterile intestine. If, from the moment of birth, nothing enters his mouth except the mother's nipple (which, by the way, is only designed by nature), then quite quickly the child's gastrointestinal tract is sown with normal microflora. Colostrum and breast milk contain factors that promote the growth of normal microflora and suppress the pathogenic one. In the event that breastfeeding was organized incorrectly (and this case, unfortunately, is the most common), if already on the first day after childbirth, before getting to know the maternal microflora, the baby began to receive various liquids through the mouth, colonization of the intestines is far from ideal.
But even in this case, mother's milk will help to cope with problems. The most interesting thing happens when the baby comes home. The normal stool of a breastfed child is liquid, yellow, with white lumps, it can be 7-10 times a day, a little bit, or 1 time in several days, but in large volume.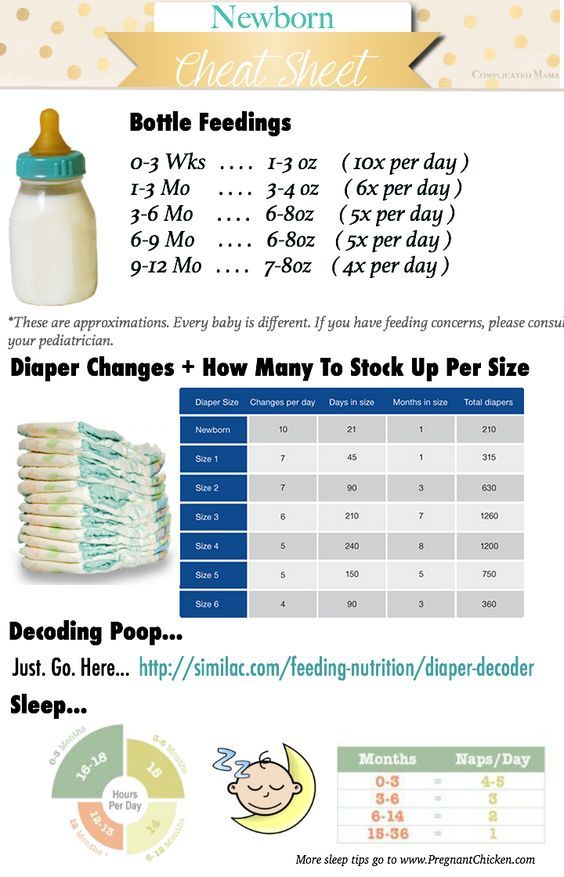 Most often, the chair is 3-5 times a day, in babies in the first months of life. District pediatricians call these normal children's poop diarrhea and send their mother to take a stool test for dysbacteriosis.
Most often, the chair is 3-5 times a day, in babies in the first months of life. District pediatricians call these normal children's poop diarrhea and send their mother to take a stool test for dysbacteriosis.
This does not take into account the fact that the baby for the first six months of life has the right to dysbiosis in his intestines and to any stool, especially if he grows and develops well. Then treatment begins, one of the main points of which is the transfer of the child, for example, to fermented milk formula. The pediatricians are not to blame. They are accustomed to the stool of a bottle-fed baby - thicker and more uniform. An even more interesting situation occurs later, when, despite drinking, for example, various biological products, the child continues to inoculate microorganisms that are not suitable for his intestines. In this case, the mother is told that it's all about her milk, and they insist on stopping breastfeeding.
The following case is indicative in this respect. In a breastfed baby, Candida fungi and hemolyzing Escherichia coli were constantly sown in large quantities. No treatment had any effect on these microorganisms. Mom was told all the time that milk was to blame. Having fed the child up to a year, the mother took him away from the breast. The child began to get sick often, and mushrooms and sticks remained in the same quantities.
In a breastfed baby, Candida fungi and hemolyzing Escherichia coli were constantly sown in large quantities. No treatment had any effect on these microorganisms. Mom was told all the time that milk was to blame. Having fed the child up to a year, the mother took him away from the breast. The child began to get sick often, and mushrooms and sticks remained in the same quantities.
Sowing milk for sterility
When sowing milk for sterility, various microorganisms are sown in 50-70% of cases, most often staphylococcus aureus and epidermal. Very often, when these organisms are found, the mother is prescribed a course of antibiotic treatment, at which time the child is fed formula for a week, after which he usually refuses to breastfeed. This is the worst option, but the most common one. Either mother and child begin to be treated using biological products, or mother and child drink chlorophyllipt. Meanwhile, the presence of staphylococci in milk does not mean anything! Both Staphylococcus aureus and epidermal Staphylococcus aureus live on human skin, and are also found on most of the surrounding objects.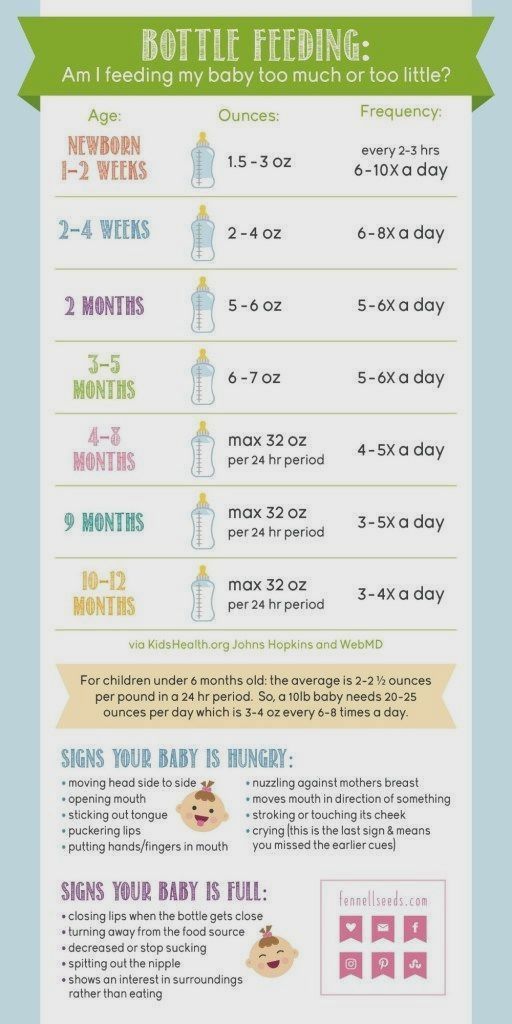 For example, staphylococcus has a tropism for cotton fabric. When moving a stack of diapers, the number of staphylococci in the air increases dramatically! Together with mother's milk, the child receives specific antibodies that help him cope with staphylococcus aureus if necessary.
For example, staphylococcus has a tropism for cotton fabric. When moving a stack of diapers, the number of staphylococci in the air increases dramatically! Together with mother's milk, the child receives specific antibodies that help him cope with staphylococcus aureus if necessary.
It turns out that mother's milk staphylococcus comes to the child along with protection from it. It is not dangerous for the child! Moreover, the child needs, in the first hours after childbirth, to be populated by his mother's staphylococcus aureus. From this staphylococcus, he will be protected by his mother's antibodies, which he will receive with colostrum and milk, and which he has already received transplacentally! The entire microflora of the mother's body is already "familiar" to the child's immune system, thanks to antibodies penetrating the placenta. It is dangerous for a child to be populated by the microflora of the maternity hospital, including hospital strains of staphylococcus resistant to antibiotics! He is not familiar with these microorganisms and their colonization of his skin and gastrointestinal tract is dangerous for the baby.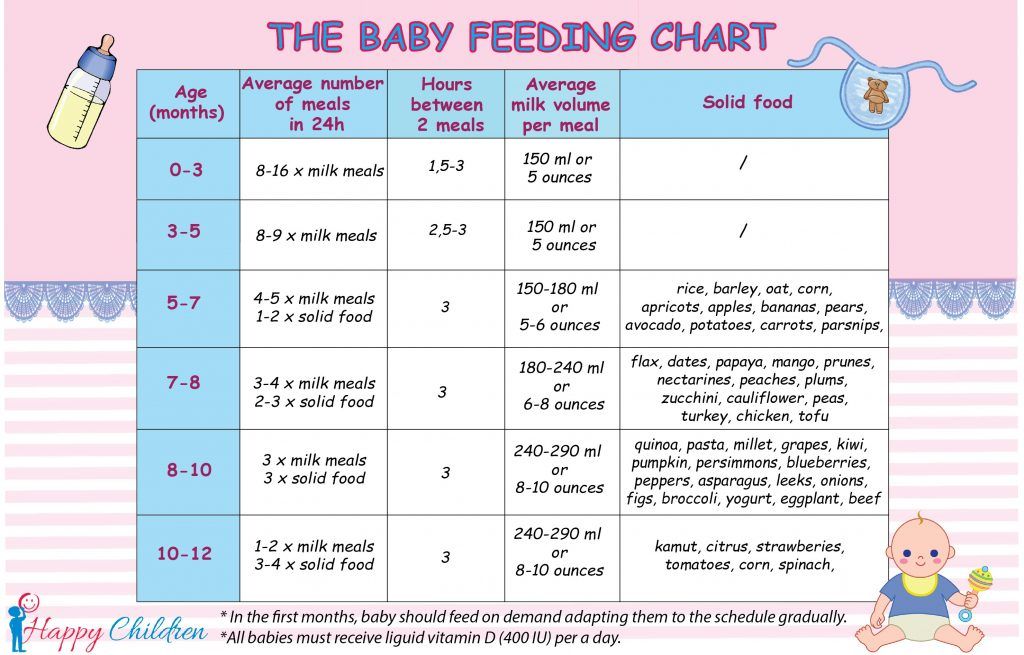 If a child does not have the opportunity to "populate" with his mother's microflora, he is populated by what is around. As they say, a holy place is never empty. If it is not possible for a “home” strain of Staphyloccocus aureus to settle on an infant, a hospital strain will take its place. But this is not scary for a breastfed child, the mother's body, by producing appropriate antibodies, will help the child. Unless, of course, in the life of a child there will be a place for breastfeeding.
If a child does not have the opportunity to "populate" with his mother's microflora, he is populated by what is around. As they say, a holy place is never empty. If it is not possible for a “home” strain of Staphyloccocus aureus to settle on an infant, a hospital strain will take its place. But this is not scary for a breastfed child, the mother's body, by producing appropriate antibodies, will help the child. Unless, of course, in the life of a child there will be a place for breastfeeding.
The presence of staphylococcus in milk does not affect its quality in any way. Staphylococcal enterocolitis, which is often used to scare mothers, convincing them to stop feeding their “poisonous” milk, is an extremely rare condition that occurs with diseases of the immune system, and which is facilitated by artificial feeding! It must be assumed because even if the baby, for some internal reasons, has weakened immunity, he will still receive significant support with mother's milk. When transferred to artificial feeding, he loses this support.
Appeal to pediatricians
Dear colleagues! If the somatically healthy breastfed child you are observing is not gaining weight well, has green, unstable stools, skin problems, before transferring him to artificial feeding, prescribing an examination and treatment, try to find out if breastfeeding of this child is properly organized. baby? Breastfeeding is a very simple process, if not elementary. But! Only if the breastfeeding mother follows a few simple rules and actions.
These rules and practices related to the culture of motherhood have been widely known and used for thousands of years. And now almost lost. Without knowledge of these rules, full breastfeeding cannot take place.
If a mother feeds her baby 6-7 times a day, uses a pacifier, gives her baby tea or water to drink, expresses herself, does not feed her at night, she performs actions for which neither the child nor she herself is designed by nature. It is impossible to establish a natural process by acting unnaturally! If a child has improper attachment to the breast, and no one notices this, this is very sad, because.