Newborn baby vomiting after feed
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug. Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant. Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting. Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug. Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant. Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting. Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Regurgitation and vomiting in children
Regurgitation syndrome is one of the most common reasons for parents of young children to visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism.
The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism.
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc.
Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc.
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes.
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life.
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia. If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation.
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age of the child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc. In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.
In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.
Experienced pediatricians and surgeons are on duty around the clock at the EMC Children's Clinic, providing emergency and planned care to children of all ages, starting from the first days of life.
If surgical treatment is required, the method of choice in our clinic is minimally invasive endoscopic surgery, which in most cases allows the child to go home on the day of the operation. The operation is accompanied by an experienced anesthesiologist, who individually selects modern and safe anesthesia for each child. Postoperative wards are equipped with high-tech equipment, where round-the-clock monitoring systems are installed, and a separate nurse continuously monitors the condition of small patients.
The operation is accompanied by an experienced anesthesiologist, who individually selects modern and safe anesthesia for each child. Postoperative wards are equipped with high-tech equipment, where round-the-clock monitoring systems are installed, and a separate nurse continuously monitors the condition of small patients.
In the comfortable hospital of the EMC Children's Clinic, parents can stay with their child all the time, round-the-clock visits are open for relatives and friends, which ensures maximum comfort for the child and parents.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason to see a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside.![]() When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.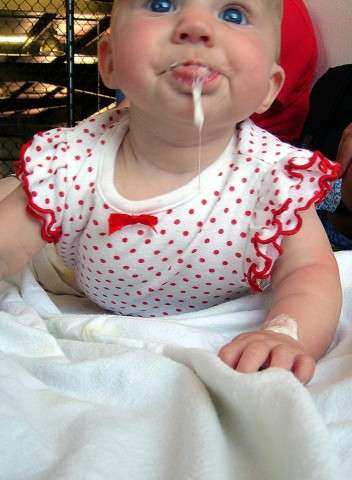
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause.