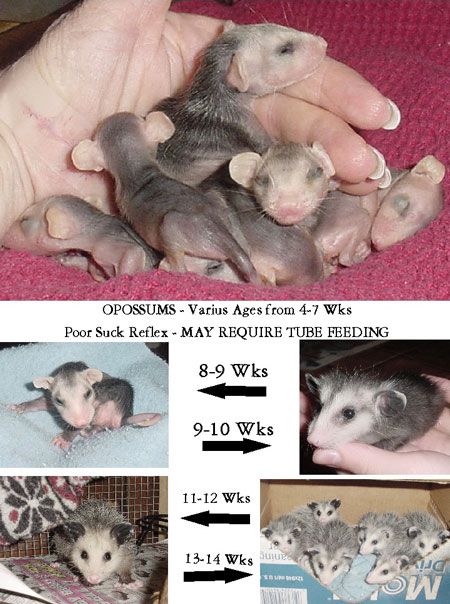
Ng tube feeding for babies
Nasogastric Tubes (Insertion and Feeding)
Nationwide Children’s Hospital
Nasogastric (NG) tubes are used to feed babies and children who cannot take in enough calories by mouth. The NG tube is placed in the nose or mouth and slid into the stomach. The formula is put into the tube and flows to the stomach. Some NG tubes have a guidewire for easier insertion. The guidewire is removed after the tube is placed in the stomach.
You Will Need
- Feeding tube
- Scissors
- 60 mL Enfit® syringe
- Doctor-prescribed formula
- Tape, DuoDERM®, or Tegaderm®
- Water soluble lubricant like K-Y® Jelly or Surgilube®
Preparing to Place the Tube
- Wash your hands.
- Cut a piece of tape, DuoDERM, or Tegaderm that is long enough to secure the tube from your child’s nose.
Put the tape on their cheek.
This will help protect your child’s skin under the tube. - Refer to Picture 1 for the following instructions. Take the tube from the tip of the nose (A) to the earlobe (B), then to the middle of the belly (C), which is halfway between the bottom of the breastbone and the belly button. Mark the tube at point C with a marker or piece of tape. This will let you know how far to insert the tube to reach the stomach.
- Children should be placed in a sitting position. Place babies on their backs. You may need to wrap your baby in a blanket so they don’t grab the tube.
Placing the Tube
- Put a small amount of water-soluble lubricant on the tip of the tube. Never use Vaseline® or any other oil-based substance.
- Put the tube slowly into the nose while aiming toward the ear. Using gentle pressure, keep putting the tube in until the mark you made on the tube reaches the nose.
- If the tube does not go in easily, remove it.
 Never force the tube. Change your child’s position, lubricate the tip of the tube, and try again.
Never force the tube. Change your child’s position, lubricate the tip of the tube, and try again. - Encourage your older child to swallow the tube. The tube may go into place easier for a baby if they suck on a pacifier.
- If the tube does not go in easily, remove it.
- Put the tube on the tape, DuoDERM, or Tegaderm on your child’s cheek. Then, secure the tube with another piece of tape (Picture 2).
- The tube may be coiled up and taped to your child's back. You may also use tape to secure the tubing to their clothing.
Placement for NG Tube With a Guide Wire
- When using an NG tube with a guide wire, carefully remove the guide wire after the tube is in place. Use the free end of the tape on your child’s cheek to keep the tube in place.
- NEVER put the guide wire back into the NG tube after the tube is in your child.
Check to make sure the tube is in the stomach each time before a feeding. To check the placement of an NG tube:
To check the placement of an NG tube:
- Look at your child after the tube has been placed and they have calmed down. If they are gagging, coughing, or turning blue, it may not be in the right spot. Remove it.
- If you’re still worried about placement, insert a syringe into the end of the tube and pull back gently. If you get stomach contents in the syringe, the tube is in the correct position.
- Make sure the mark on the tube is still at your child’s nose. If it’s not, the tube should be re-inserted to the correct position. Check again to make sure your child is not gagging or coughing after the tube is in place.
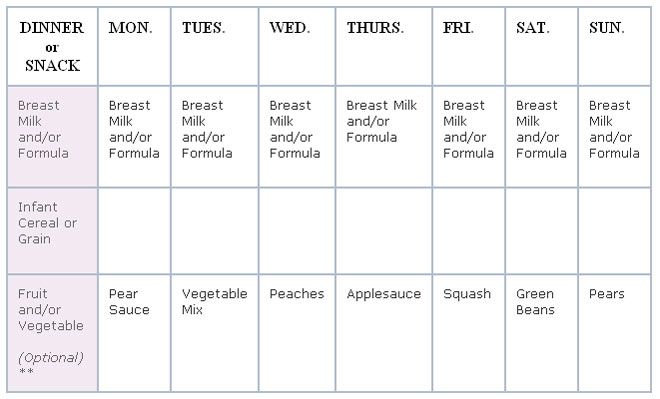
You can feed your child after checking tube placement. The doctor or health care provider will tell you how much formula to use for each feeding and how often.
- If the formula is in the refrigerator, take it out and let it sit at room temperature for 30 minutes before feeding.
 You may also warm the formula by putting the container or bottle in a bowl or cup of warm water.
You may also warm the formula by putting the container or bottle in a bowl or cup of warm water. - Pour a drop of the formula on the inside of your wrist to test the temperature. Be sure it is warm, not hot.
- NEVER WARM FORMULA IN THE MICROWAVE.
- Hold your child while feeding. You may give your child a pacifier to suck on during feedings. This helps your baby learn feeding skills. They will start to connect sucking with the feeling of being full.
- Remove the plunger from the syringe or open your feeding bag.
- If your child is getting gravity feeds by syringe:
- Put the tip of the syringe into the open end of the feeding tube. Hold the tip of the syringe no higher than 10 inches above the child’s head.
- The height of the syringe affects how fast the formula goes in.
- Holding it higher may feed your child too fast. Your child may throw up (vomit).
- Pinch the tube while you pour the formula into the syringe.

- Release the tube and let the formula enter the stomach slowly. Add more formula as the syringe empties (Picture 3). Feed your child slowly over 15 to 20 minutes.
- If the formula does not flow, change your child’s position. If it still does not flow, put the plunger into the syringe and gently push enough so the formula will flow again.
- Remove the plunger.
- If your child starts to vomit during a feeding, stop right away. Keep their head upright and their face turned to the right side. Wait for vomiting to stop before feeding again.
- If they keep vomiting, take the NG tube out and call your child’s doctor or the nurse helpline at (614) 355-1100.
- Put the tip of the syringe into the open end of the feeding tube. Hold the tip of the syringe no higher than 10 inches above the child’s head.
If your child is getting feeds by pump, a person from the equipment supply company will teach you how to use it. The pump can help feeds go in slower than gravity feeds.
After the Feeding- For syringe feeds, pour 5 to 10 mL of water into the syringe after the formula is gone.
 This clears the tube to prevent clogging. This helps prevent infection.
This clears the tube to prevent clogging. This helps prevent infection. - Remove the syringe and place the cap on the tube. Babies should be burped every 2 to 3 ounces and after feedings.
- If you put your child to bed after the feeding, put them on their back without stuffed animals, toys, or a blanket (Picture 4). This is the safest position for your baby.
- If your child begins to vomit, turn their head to the side and open the cap to the tube.
Cleaning the Equipment
- Place a clean paper towel on an empty tray.
- Rinse the syringe and measuring container with cold water.
- Then, wash them in hot, soapy water.
- Rinse and dry.
- Place the clean items on the tray.
- Cover with a paper towel and store out of the reach of children and pets.
Removing the Tube
- Your child’s doctor may want you to remove the tube.
 If you need to remove it, loosen the tape. Pinch the tube to prevent breathing in (aspirating) stomach contents.
If you need to remove it, loosen the tape. Pinch the tube to prevent breathing in (aspirating) stomach contents. - To remove the tube, loosen the tape on the face. Pinch the tube to prevent your child from breathing in stomach contents and gently remove the tube from the nostril.
- If the NG tube needs to be replaced, a new NG tube should be inserted. If a new tube is not available, the tube can be washed and reused (see cleaning instructions). If the NG tube uses a guide wire, replace the guide wire in the NG tube before replacing. Remove the guidewire upon placement.
- Change which nostril is used each time you replace the NG tube.
- Change the tube once a month unless it becomes clogged, dirty, or damaged.
Warning
- The feeding set tubing can get wrapped around a child’s neck. This can lead to choking (strangulation) or death.
- DO NOT leave the feeding set tubing where infants or children can get tangled up in it.

- Talk to your child’s doctor or health care provider:
- If your child has been tangled in their tubing before.
- To learn steps you can take to help make sure the tubing does not get wrapped around your child’s neck, such as keeping the tubing away from the child as much as possible.
- Any other concerns you may have about the risk of strangulation from feeding set tubing.
- If your child is injured by feeding set tubing, please report the event to the FDA. Your report can provide information that helps improve patient safety. The website to make a report is: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home
Other Tips and Advice
- If the doctor or health care provider has ordered liquid vitamins, put the correct dose into the formula.
- If feeding by mouth (oral) was suggested, feed your baby after placing an NG tube.
 Feeding before placing the tube may cause vomiting.
Feeding before placing the tube may cause vomiting. - Do not change your baby’s formula. Do not give them more than the doctor ordered.
- If your child seems hungry after feeding, ask the doctor about increasing feedings.
- You can use the same tube for up to 1 month unless it gets clogged, dirty, or damaged. Always have a spare tube with you for back-up.
- Ask if there are recommendations for your child’s specific condition.
If you have questions, ask your child’s doctor or health care provider.
Nasogastric Tubes (Insertion and Feeding) (PDF)
HH-II-32 8/84, Revised 4/22 Copyright 1984, Nationwide Children's Hospital
You Might Also Be Interested In
Pediatrics Nationwide
Swallowing Functions Remain Worse in Preterm Infants Even at Full-Term Equivalent Age
Pediatrics Nationwide
Feeding Difficulties in Opioid-Exposed Infants – Mechanics and Possible Causes
Condition
Feeding Disorders
Nasogastric (NG) Tube Feeding
Article Translations: (Spanish) (Somali)
What is a nasogastric tube feeding?
A nasogastric (NG) tube is a small tube that goes into the stomach through the nose. Breast milk, formula, or liquid food is given through the tube directly into the stomach, giving your child extra calories. Feeding this way helps your child get enough nutrition to grow, develop, recover from illness, play, and learn.
Breast milk, formula, or liquid food is given through the tube directly into the stomach, giving your child extra calories. Feeding this way helps your child get enough nutrition to grow, develop, recover from illness, play, and learn.
Tube feeding can be done for children of any age. Some children will depend on tube feeding only until they are able to eat by mouth. Using the gastrointestinal (GI) tract for feeding keeps it healthy and working normally.
Other children can continue to eat as usual, and also get tube feedings for extra calories.
There are several ways to give NG feeding. The type of tube, how often it needs to be changed, type and amount of formula, and length of feeding time will be decided by the doctor and dietitian, depending on your child's needs.
Follow only the checked instructions in this sheet.
Your child's special instructions:Type and size of feeding tube: ___ Change the feeding tube every: ___ Do not change the feeding tube yourself. What to feed: Amount to feed: How often to feed: Method: ___ bolus ___ continuous Type of pump: Rate of feeding: Flush the feeding tube at the end of each feeding with ml of warm water. Other: Measurement: Marking at nostril: _____cm Nostril to beginning of the hub: _____cm Care of feeding bag and tubing:___ Change every day. If the bag and tubing do not clean easily, try using a solution made of equal amounts of white vinegar and cool water (for example 1 cup vinegar with 1 cup water). Rinse well and store in refrigerator. Throw away the feeding bag and tubing after 1 week; sooner if you cannot get it clean or if it begins to leak. |
Definitions
| aspiration | getting fluid (stomach contents for formula) into the lungs, which can cause trouble breathing |
| bolus | feeding over a short time |
| continuous | feeding over an extended time at a slower rate |
| GI tract | the esophagus, stomach, and intestines |
| lubricant | water-soluble substance such as K-Y® jelly, used to help the tube slip in more easily - do not use Vaseline® |
___ Inserting the feeding tube
It takes time and practice to learn how to insert the tube, so be patient with yourself.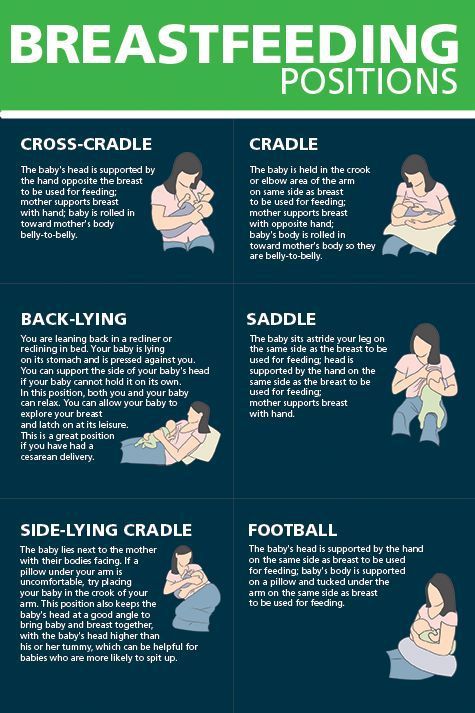 Do this by yourself only after you have done it successfully with the nurse present.
Do this by yourself only after you have done it successfully with the nurse present.
Get ready:
- Wash your hands.
- Gather supplies:
- feeding tube
- tape measure
- With your fingers, find your child's sternum (breastbone). Gently feel the bone in the center of the chest, and then find its bottom edge. It will be below nipple level, and you will feel the bottom of the rib cage curving away to each side.
- Now imagine a spot on your child's belly that is midway between the belly button and the bottom edge of the breastbone. Keep that spot in mind.
- Using a tape measure, measure from the tip of your child's nose to the bottom of the earlobe, then down to that spot midway between belly button and breastbone edge. Write that number down: we will call it "your child's measurement." Measurement:
In this picture, the child's measurement is 12 inches (3 inches from nose to ear, plus another 9 inches down).
- Now, from the tip of the tube, measure the distance of your child's measurement (in the pictured example this would be 12 inches). Mark that spot on the tube using a permanent marker. Now you are ready to insert the feeding tube.
- Now, measure from the mark you made to the beginning of the hub. That is the Extra Tube Length.
Insert the tube:
- Wash your hands.
- Gather equipment:
- feeding tube
- formula
- gauze if needed
- water for lubrication or other lubricant
- pH testing strips
- syringe, size:
- tape, type:
- water for rinsing if needed
- Position the child.
___ Swaddle an infant (wrap with the arms secured in a blanket). Put your infant on their back, either in an infant seat or on a bed, with the head raised.
___ Older children should be placed in a comfortable position, and may be held by an adult if they wish. Some children may vomit when the tube is put in. Be sure the child can be turned easily if this happens.
Be sure the child can be turned easily if this happens. - Lubricate the tube with water or put a small amount of lubricant on the end of the tube if you have been taught to do so. Most tubes have a coating that is activated with water, making the tube easier to slide in.
- Insert the tube into the nostril, pushing the tube gently down until the mark on the tube is at the tip of the nose. Older children can drink or swallow to help the tube go down. Infants may suck on a pacifier or your fingers during tube insertion. This can be uncomfortable for your child and it is normal for them to cough or sneeze while the tube is being inserted. It may be best to have someone help you.
After the tube is inserted, remove the tube right away if:
- coughing
- gagging
- sneezing
- vomiting
- wheezing
- changing color
- cannot catch a breath
- change in respiratory rate
- change in oxygen needs
- decrease in pulse oximeter readings
- increased restlessness
- unexplained irritability, discomfort, or abdominal pain
- or you see the tube coming out of the mouth
- Cuddle and comfort your child for a few minutes, and try again.

- Once the tube is in place, secure it with tape as shown by the nurse.
- Check the tube placement (see below).
Checking the tube placement
To prevent aspiration, you must check the tube placement before each feeding, to be sure it has not moved. The stomach should be as empty as possible when checking for placement, so plan each placement check before medicine or feedings.
- Look at your child. Is your child comfortable and breathing normally? If your child appears distressed, gagging, sneezing, vomiting, wheezing, changing color, cannot catch a breath, change in respiratory rate, change in oxygen needs, decrease in pulse oximeter readings, increased restlessness, unexplained irritability, discomfort, or abdominal pain, cannot talk, or you see the tube coming out of the mouth: Do not start the feeding.
- Make sure that the mark on the tube is at the nostril. Measure the tube from the mark at the nostril to the beginning of the hub and make sure it matches the "extra tube length" number you wrote down earlier.
 (See "Get ready," step 7, above.) If you cannot see the mark or the length has changed, do not start the feeding.
(See "Get ready," step 7, above.) If you cannot see the mark or the length has changed, do not start the feeding. - Check placement with a pH strip. Try to pull out some stomach fluids with the syringe. Using a small syringe (3 to 5 ml) will make this easier. Test the acidity of the stomach fluids with a pH strip. A pH between 1-5.5 indicates proper placement. A pH of 6 or higher may indicate incorrect placement. If you get a pH of 6 or higher, DO NOT START THE FEEDING. Call Children’s Home Care to have the tube replaced.
- If having trouble getting pH, place your child on their left side for 15 minutes to allow stomach fluids to pool at the end of the tube.
- Write down pH level.
- Gently flush the tube with the amount of water prescribed by your provider.
- If unable to obtain pH but length, measurement and child's condition are unchanged, you may start the feeding.
Paying careful attention to these signs will help you to be sure the tube is placed correctly. If you have any doubts, it is best to remove the tube and replace it.
If you have any doubts, it is best to remove the tube and replace it.
Safety Precautions
- Be aware the feeding set tubing can get wrapped around a child's neck, which could lead to strangulation or death.
- When running a feeding for your child, place the tubing in a way the tubing cannot get tangled around your infant or child. Place the tubing through your child's clothing or towards the foot of the bed. This will help the tubing from getting wrapped around your child's neck if they are to turn or move.
- If your child is injured by feeding set tubing, report the event to the FDA at [email protected] or call 1-800-638-2041.
Giving the feedings
___ Bolus feeding
It may be helpful to have 2 people to do this type of tube feeding. One person can hold and comfort the child while the other gives the feeding.
- Wash your hands.
- Measure the correct amount of formula and warm it to the desired temperature.
 Do not use the microwave to warm the feeding.
Do not use the microwave to warm the feeding. - Check tube placement as above (observing mark on NG tube and pH testing).
- Pinch the tube.
- Attach a syringe to the feeding tube.
- Pour the formula into the syringe.
- Unpinch the tube.
- Allow the formula to run for the same amount of time as it would take the child to drink it by mouth, or as prescribed by the doctor.
- Ways to help the feeding flow:
Try to start the feeding when the child is calm. You may have to "push" the feeding to get it started. To do this, place a plunger into the syringe and push slightly. Remove the plunger gently and allow the formula to flow in by gravity. If your child is crying, you may need to repeat the push several times.
___ A pacifier may help calm a young child and also helps to connect sucking with stomach-filling.
___ For older children, use activities to distract them, or involve the child with the feeding, such as holding the syringe.
- During the feeding, keep the bottom of the syringe no higher than 6 inches above the child's stomach. The height of the syringe controls the feeding rate or speed.
- Continue adding formula into the syringe until the prescribed amount is given.
- When the syringe is empty, flush the tube with the prescribed amount of warm water.
- After the feeding:
___ Close the cap on the tube.
___ Leave the tube open to air. Tape a piece of gauze over the syringe to keep fluids from splashing out.
___ Burp your child.
___ Infants and young children may be most comfortable with their head and upper body raised, or lying on their left side.
___ Older children may be up and playing.
___ Continuous feeding with a feeding pump
- Wash your hands.
- Measure enough formula for 4 hours and warm it if needed. Do not use the microwave to warm feeding.
- Pour formula into the feeding bag. Run formula to the end of the pump tubing.

- Set up the pump and pump tubing according to the directions from the medical supply company. Be sure the rate is set correctly.
- If a new feeding tube is to be inserted, see "Getting ready to insert the tube" and "Inserting the tube."
- Check placement if external tube length measurement is unchanged, exit site mark is visible and there are no changes in your child's condition, continue feedings without interruption (see "Checking the tube placement"). If vomiting or respiratory distress occurs at any time, tube placement should be verified.
- Connect the pump tubing to the child's feeding tube.
- Turn on the pump. Check to make sure the formula is dripping.
- As the bag empties every 4 hours, add more formula.
- Hold and/or talk to your child often during waking hours. Have your child's head raised during the entire feeding.
- Watch your child carefully to make sure there is no change in breathing or behavior. Make sure the mark on the tube is still at the nostril.
 It is also a good idea to measure it every few hours, because sometimes the tube can slip under the tape. Stop the feeding if the mark changes and recheck placement.
It is also a good idea to measure it every few hours, because sometimes the tube can slip under the tape. Stop the feeding if the mark changes and recheck placement. - If your doctor tells you to, after the feeding period, flush the tube with the prescribed amount of warm water.
- If you are told to stop the continuous feeding:
___ Plug or clamp the tube.
___ Leave the tube open to air. Tape a piece of gauze over the syringe to keep fluids from splashing out.
___ Burp your child.
___ Have child's head raised for about 30 minutes after the feeding is done.
___ Removing the feeding tube (if ordered)
- Remove the tape.
- Pinch the tubing and pull the tube out in one quick motion.
- Hold, cuddle, and comfort your child. If your child is an infant, burp him or her.
Skin care
Clean your child's skin around the tube often with warm water, removing any secretions. If the nostril is reddened or the skin is irritated, remove the tube and replace it in the other nostril, if possible.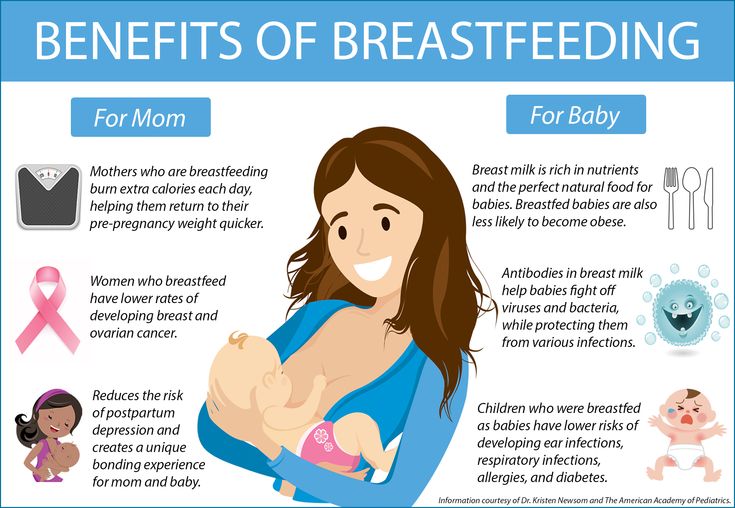
If you have used a transparent dressing on your child's face, remove it by loosening it with mineral oil and gently working the dressing off. If you use adhesive remover to loosen the dressing, be sure to wash the skin with water to remove all residue, as this can be very irritating.
Problem solving
| Problem | What to do |
| Clogged or plugged feeding tube (follow only the checked instructions) |
|
| Feeding tube falls out |
|
| Coughing while tube is in place |
|
| Diarrhea and cramping |
|
| Nausea (upset stomach) or vomiting (throwing up) |
|
| Skin around the nose is irritated |
|
| Cannot obtain pH reading |
|
When should I call the doctor?
- fever
- vomiting or diarrhea that does not stop
- fussiness, hard to console
- pain or unusual distension in abdomen
- questions about using the tube
- trouble breathing - call 911
If you are concerned about your child for any reason, call your doctor to discuss the symptoms.
Questions?
This is not specific to your child, but provides general information. If you have any questions, please call your doctor, home care nurse, or dietitian.
If you have any questions, please call your doctor, home care nurse, or dietitian.
Children's Minnesota
Reviewed 10/2022
Back To Top
Tube feeding a newborn baby
Target : provide for a newborn baby necessary amount of food when natural nutrition through the mouth impossible.
Equipment :
- rubber gloves;
- scarf, mask;
- measured required amount of milk per heated food 37-38°C;
– sterile gastric catheter;
- clamp;
– sterile syringe 20 ml;
- tray for equipment;
— electric suction or a rubber bulb.
Mandatory conditions : the size of the gastric catheter depends from the body weight of the child: weight less than 1000 g - No. 4 nasal or No. 6 oral; weight 1000-2500 g - No. 6 nasal and oral; weight over 2500 g — No. 6 nasal or No. 10 oral
premature newborn baby before and after feeding needs to be done oxygen therapy to prevent apnea attacks.
| Stages | Justification |
| Preparation to procedure | |
| •Explain mother / relatives goal and move procedure | •Provision parental rights to information |
| • Prepare necessary equipment | • Security clarity of procedure |
| • Put on scarf, mask • Wash up and dry hands, put on gloves | •Provision infectious safety |
| • Lay down baby on side with raised head end, fix this position with roller | •Warning suction |
| Performance procedures | |
| • measure depth of catheter insertion from the lobe ear to the tip of the nose and from the tip of the nose to the end of the xiphoid process. | •Provision insertion of a catheter into the stomach |
| •Connect to the syringe probe and check it patency, passing through it air Note: make sure that the free end of the catheter was permanently fixed by hand | • Security effectiveness of the procedure |
| •Remove plunger from syringe • Insert syringe to the left hand and skip the attached catheter between index and middle fingers of the left hand, placing it blind end up | • Warning leakage of milk from the catheter its further filling |
| • Fill syringe for 1/3 volume of breast milk | |
| • Take blind end of the probe in the right hand and, carefully lowering it down, fill milk (until the first drop appears milk from a hole in the area blind end of probe) | • crowding out air from the catheter warns air entering the baby's stomach |
| • Return probe in the left hand to the starting position Note: in tube filling time make sure that the blind end of the probe constantly raised up | |
| • clamp catheter clamp at a distance of 5-8 cm from syringe side • Ring clamp placed on the thumb left hand • Right take the probe with your hand at a distance of 7-8 cm from blind end • wet its in milk | • Exception leakage from a milk catheter • Warning slipping of the catheter from the syringe • Wet probe is easier to insert • Injury prevention mucous membranes |
| • Insert probe through the nose along the inferior nasal walk or mouth in the midline of the tongue to the mark (when inserting the probe, do not make an effort and see if shortness of breath, cyanosis, etc. | • Exception probe entering the respiratory tract |
| • Add into syringe milk • Lifting syringe, remove the clamp from the catheter and slowly (by adjusting the height of the syringe) inject milk into the baby's stomach | • Slow prevents milk supply sharp increase in peristalsis stomach and vomiting |
| • At reaching the mouth of the syringe with milk, again clamp the catheter Note: if as a result of the activities not all metered was entered amount of milk - refill them a syringe and insert it into the child's stomach | • Warning air entering the stomach |
| •Clamp catheter large and forefinger fingers of the right hand at a distance 2-3 cm from the mouth and fast pull it out with a tissue | • Prevention vomiting |
| Completion procedures | |
| • Put child on the right side with raised head end | • Decreases likelihood of aspiration • Facilitated gastric emptying |
| •Remove gloves, wash and dry hands • Tools used place in disinfectant solution | •Provision infectious safety |
Enteral nutrition (tube feeding)
What is enteral nutrition?
Sometimes during treatment and recovery, children with cancer cannot get the calories and nutrients they need orally. Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
The probe is usually inserted in two ways:
- Through the nose (non-surgical method)
- Through a small incision in the abdomen (surgical method)
Most commonly used are nasogastric tubes and gastrostomy tubes. But there are several types of enteral feeding tubes that differ in the method of insertion and location in the digestive tract.
Sometimes the patient is simply not able to eat enough calories or protein. There is no fault in this. It is important to help your child understand that nutritional support is not a punishment. Most children get used to the enteral feeding tube quickly. It is important that the child does not touch or pull the phone. Follow skin care instructions at the insertion site to avoid irritation or infection.
A nasogastric tube is inserted into the stomach or small intestine through the nose and throat.
Types of enteral feeding tubes
An enteral feeding tube connects to the stomach or small intestine. The location depends on how the patient tolerates the formula and how well their body is able to digest the nutrients. If possible, they try to place the probe in the stomach so that digestion occurs naturally.
There are 5 types of enteral feeding tubes:
Nasogastric Tube . A nasogastric tube is inserted into the stomach through the nose. It passes through the throat, esophagus and into the stomach.
Nasojejunal Probe . A nasojejunal tube is similar to a nasogastric tube but passes through the entire stomach into the small intestine.
Gastrostomy Tube (Gastrostomy Probe) . A gastrostomy tube is inserted through a small incision in the skin. The probe in this case passes through the wall of the abdominal cavity directly into the stomach.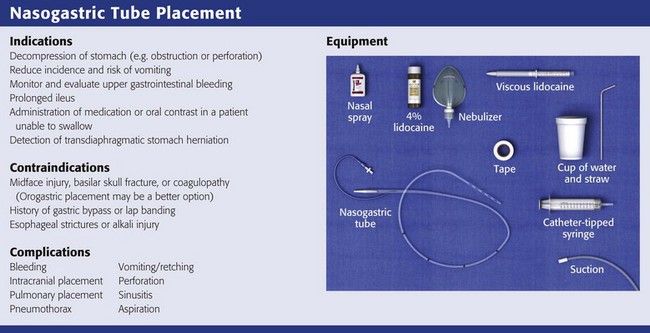
Gastrojejunostomy tube (gastrojejunostomy probe) . The gastrojejunostomy tube is inserted into the stomach like a gastrostomy tube, but passes through the stomach into the small intestine.
Jejunostomy Probe . A jejunostomy tube is inserted through a small incision in the skin and passed through the abdominal wall into the small intestine.
Nasal tubes, including nasogastric and nasojejunal tubes, are generally used for short-term enteral feeding, usually not more than 6 weeks. The probe comes out of the nostril and is attached to the skin with adhesive tape. Nasogastric and nasojejunal tubes have a number of advantages, such as a low risk of infection and a simple insertion procedure. However, the probe must be attached to the face, and this worries some children. Other children may have problems with the nasogastric tube due to chemotherapy, which irritates the skin and mucous membranes.
Surgical insertion tubes - gastrostomy tube, gastrojejunostomy tube and jejunostomy tube - are used for longer periods of time or if a nasal tube cannot be placed in the child.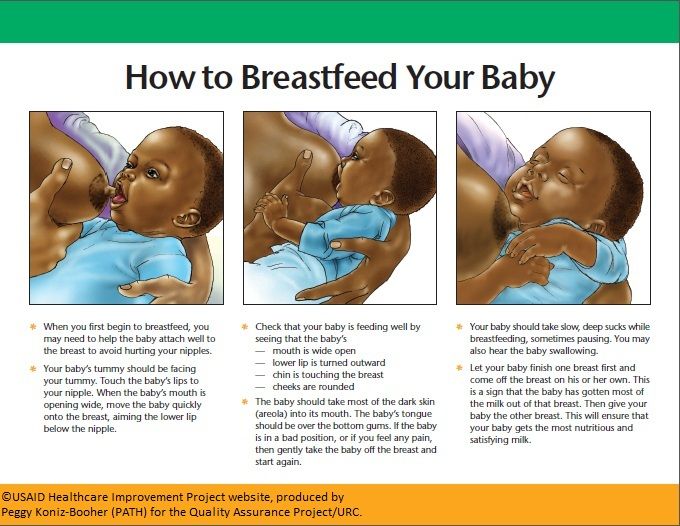 The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
-
Insertion of nasogastric and nasojejunal tubes
-
Gastrostomy, Gastrojejunostomy and Jejunostomy Insertion
After healing, the stoma usually does not hurt. The child can perform most daily activities.
Side effects of enteral nutrition
The most common side effects of enteral nutrition are nausea, vomiting, stomach cramps, diarrhoea, constipation and bloating.
There may be other side effects:
- Infection and irritation at the insertion site
- Probe misaligned or falling out
- Lung feeding formula
Most side effects can be avoided by following the care and nutrition instructions.
Feeding babies with tubes in place
It is the responsibility of the nutritionist to provide the baby with all the necessary nutrients. In children with cancer, an enteral feeding tube is often used in addition to what the child can eat normally. However, some patients have to enter all the nutrients through a tube.
The patient is prescribed a mixture containing:
- Calories
- Fluid
- Carbohydrates
- Fats
- Protein
- Vitamins and minerals
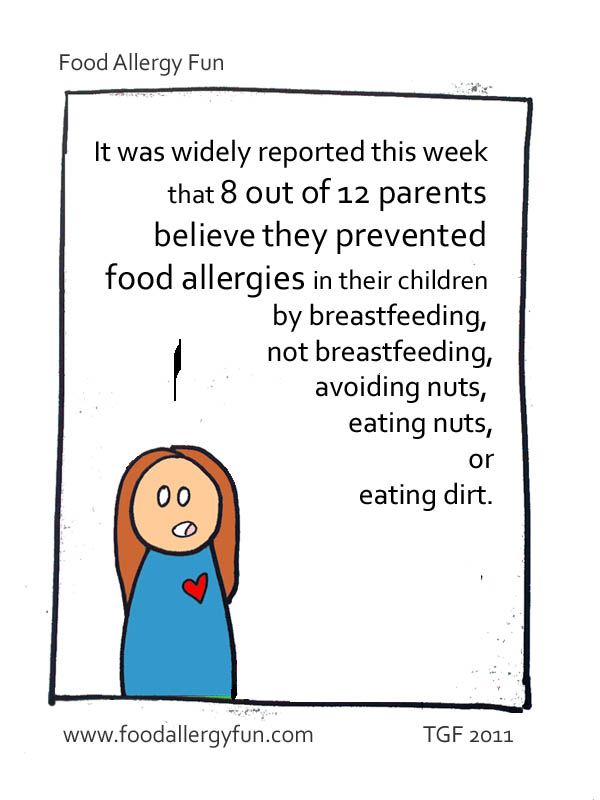
Standard formulas are suitable for many patients. For babies, it is preferable to use breast milk. Some children need special formulas that take into account their characteristics: the presence of allergies, diabetes or digestive problems.
It is very important for family members to work closely with a nutritionist. Nutritional needs may change due to changes in the child's health or side effects such as vomiting or diarrhea.
Types of enteral feeding
There are three types of enteral feeding - bolus, continuous and gravity flow.
Bolus feeding - large doses of the mixture are given to the patient by tube several times a day. This species is closest to the usual diet.
Continuous Power - Electronic pump delivers small doses of formula over several hours. Some children may need continuous feeding to reduce nausea and vomiting.
Gravity Feeding - A bag of formula is placed on the IV stand and a predetermined amount of formula is dripped through the tube at a slow rate. The duration of such nutrition depends on the needs of the patient.
Enteral feeding at home
Children can go home with a feeding tube. The doctors will ensure that family members know how to feed and care for the probe. Family members need to pay attention to the following issues:
- Weight gain or loss
- Vomiting or diarrhea
- Dehydration
- Infection
Formulas, Supplies, and Equipment Required:
- Formula: Most enteral formulas are sold ready-made.
 Some are available as a powder or liquid to mix with water.
Some are available as a powder or liquid to mix with water. - Syringe
- Adapter tube (if the child has a button tube for long-term enteral feeding)
- Pump (with continuous power)
- Feeding formula bag with tubing (for continuous feeding)
- IV Stand (Gravity Feed)
General tips for enteral feeding at home:
- Always wash your hands with soap and water before feeding your baby.
- Make sure the baby's head is above the stomach.
- Throw away any pre-mixed or homemade formulas that have been opened and kept in the refrigerator for 24 hours or more.
- Store mixed formulations in the refrigerator and discard after 24 hours.
- Ready-to-use formulas do not need to be refrigerated.
- Do not empty the syringe completely during feeding.
- Wash the syringe (and transfer tube, if used) with warm water and dishwashing detergent after each use.
- Watch for signs of nausea, vomiting, bloating or irritability while feeding.





 Make a label. Note: you can measure the depth of the catheter as follows: from the tip of the nose behind ear and up to the top of the sternum
Make a label. Note: you can measure the depth of the catheter as follows: from the tip of the nose behind ear and up to the top of the sternum  )
)