Nhs baby food allergy
Food allergy - NHS
A food allergy is when the body's immune system reacts unusually to specific foods. Although allergic reactions are often mild, they can be very serious.
Symptoms of a food allergy can affect different areas of the body at the same time. Some common symptoms include:
- an itchy sensation inside the mouth, throat or ears
- a raised itchy red rash (urticaria, or "hives")
- swelling of the face, around the eyes, lips, tongue and roof of the mouth (angioedema)
- vomiting
Read more about the symptoms of food allergies.
Anaphylaxis
In the most serious cases, a person has a severe allergic reaction (anaphylaxis), which can be life threatening.
Call 999 if you think someone has the symptoms of anaphylaxis, such as:
- breathing difficulties
- trouble swallowing or speaking
- feeling dizzy or faint
Ask for an ambulance and tell the operator you think the person is having a severe allergic reaction.
What causes food allergies?
Food allergies happen when the immune system – the body's defence against infection – mistakenly treats proteins found in food as a threat.
As a result, a number of chemicals are released. It's these chemicals that cause the symptoms of an allergic reaction.
Almost any food can cause an allergic reaction, but there are certain foods that are responsible for most food allergies.
Foods that most commonly cause an allergic reaction are:
- milk
- eggs
- peanuts
- tree nuts
- fish
- shellfish
- some fruit and vegetables
Most children that have a food allergy will have experienced eczema during infancy. The worse the child's eczema and the earlier it started, the more likely they are to have a food allergy.
It's still unknown why people develop allergies to food, although they often have other allergic conditions, such as asthma, hay fever and eczema.
Read more information about the causes and risk factors for food allergies.
Types of food allergies
Food allergies are divided into 3 types, depending on symptoms and when they occur.
- IgE-mediated food allergy – the most common type, triggered by the immune system producing an antibody called immunoglobulin E (IgE). Symptoms occur a few seconds or minutes after eating. There's a greater risk of anaphylaxis with this type of allergy.
- non-IgE-mediated food allergy – these allergic reactions aren't caused by immunoglobulin E, but by other cells in the immune system. This type of allergy is often difficult to diagnose as symptoms take much longer to develop (up to several hours).
- mixed IgE and non-IgE-mediated food allergies – some people may experience symptoms from both types.
Read more information about the symptoms of a food allergy.
Oral allergy syndrome (pollen-food syndrome)
Some people experience itchiness in their mouth and throat, sometimes with mild swelling, immediately after eating fresh fruit or vegetables. This is known as oral allergy syndrome.
This is known as oral allergy syndrome.
Oral allergy syndrome is caused by allergy antibodies mistaking certain proteins in fresh fruits, nuts or vegetables for pollen.
Oral allergy syndrome generally doesn't cause severe symptoms, and it's possible to deactivate the allergens by thoroughly cooking any fruit and vegetables.
The Allergy UK website has more information.
Treatment
The best way to prevent an allergic reaction is to identify the food that causes the allergy and avoid it.
Research is currently looking at ways to desensitise some food allergens, such as peanuts and milk, but this is not an established treatment in the NHS.
Read more about identifying foods that cause allergies (allergens).
Avoid making any radical changes, such as cutting out dairy products, to your or your child's diet without first talking to your GP. For some foods, such as milk, you may need to speak to a dietitian before making any changes.
Antihistamines can help relieve the symptoms of a mild or moderate allergic reaction. A higher dose of antihistamine is often needed to control acute allergic symptoms.
Adrenaline is an effective treatment for more severe allergic symptoms, such as anaphylaxis.
People with a food allergy are often given a device known as an auto-injector pen, which contains doses of adrenaline that can be used in emergencies.
Read more about the treatment of food allergies.
When to seek medical advice
If you think you or your child may have a food allergy, it's very important to ask for a professional diagnosis from your GP. They can then refer you to an allergy clinic if appropriate.
Many parents mistakenly assume their child has a food allergy when their symptoms are actually caused by a completely different condition.
Commercial allergy testing kits are available, but using them isn't recommended. Many kits are based on unsound scientific principles. Even if they are reliable, you should have the results looked at by a health professional.
Even if they are reliable, you should have the results looked at by a health professional.
Read more about diagnosing food allergies.
Who's affected?
Most food allergies affect younger children under the age of 3.
Most children who have food allergies to milk, eggs, soya and wheat in early life will grow out of it by the time they start school.
Peanut and tree nut allergies are usually more long lasting.
Food allergies that develop during adulthood, or persist into adulthood, are likely to be lifelong allergies.
For reasons that are unclear, rates of food allergies have risen sharply in the last 20 years.
However, deaths from anaphylaxis-related food reactions are now rare.
What is food intolerance?
A food intolerance isn't the same as a food allergy.
People with food intolerance may have symptoms such as diarrhoea, bloating and stomach cramps. This may be caused by difficulties digesting certain substances, such as lactose. However, no allergic reaction takes place.
However, no allergic reaction takes place.
Important differences between a food allergy and a food intolerance include:
- the symptoms of a food intolerance usually occur several hours after eating the food
- you need to eat a larger amount of food to trigger an intolerance than an allergy
- a food intolerance is never life threatening, unlike an allergy
Read more about food intolerance.
Page last reviewed: 15 April 2019
Next review due: 15 April 2022
Food allergy - Living with
The advice here is primarily written for parents of a child with a food allergy. However, most of it is also relevant if you're an adult with a food allergy.
Your child's diet
There's currently no cure for food allergies, although many children will grow out of certain ones, such as allergies to milk and eggs.
The most effective way you can prevent symptoms is to remove the offending food – known as an allergen – from their diet.
However, it's important to check with your GP or the doctor in charge of your child's care first before eliminating certain foods.
Removing eggs or peanuts from a child's diet is not going to have much of an impact on their nutrition. Both of these foods are a good source of protein, but this can be replaced by alternative sources.
A milk allergy can have more of an impact, as milk is a good source of calcium, but there are many other ways you can incorporate calcium into your child's diet, such as with green leafy vegetables. Many foods and drinks are also fortified with extra calcium.
See your GP if you're concerned that your child's food allergy is affecting their growth and development.
Reading labels
It's very important to always check the ingredients list on any pre-packed food or drinks your child has.
Under EU law, any pre-packed food or drink sold in the UK must clearly state on the label if it contains any of these 14 ingredients that can cause an allergy:
- celery
- cereals that contain gluten – including wheat, rye, barley and oats
- crustaceans – including prawns, crabs and lobsters
- eggs
- fish
- lupin (common garden plants) – seeds from some varieties are sometimes used to make flour
- milk
- molluscs – including mussels and oysters
- mustard
- tree nuts – such as almonds, hazelnuts, walnuts, brazil nuts, cashews, pecans, pistachios and macadamia nuts
- peanuts
- sesame seeds
- soybeans
- sulphur dioxide and sulphites (preservatives used in some foods and drinks) – at levels above 10mg per kg or per litre
Also look out for voluntary "may contain" labels, such as "may contain traces of peanut". Manufacturers sometimes put this label on their products to warn consumers that they may have become accidentally contaminated with another food product during the production process.
Manufacturers sometimes put this label on their products to warn consumers that they may have become accidentally contaminated with another food product during the production process.
Be careful with foods labelled as vegan. There is no legal definition of vegan, which means that foods labelled vegan are not always completely free of animal products. If you have food allergies to milk, eggs, fish, crustaceans or molluscs, read the ingredients list carefully on vegan food products. And look out for labels with warnings such as "may contain".
Read more detailed information about allergen labelling on the Food Standards Agency website.
Some non-food products contain allergy-causing food:
- some soaps and shampoos contain soy, egg and tree nut oil
- some pet foods contain milk and peanuts
- some glues and adhesive labels used on envelopes and stamps contain traces of wheat
Again, read the labels of any non-food products your child may come into close physical contact with.
Unpackaged food
Currently, unpackaged food does not need to be labelled in the same way as packaged food. The law requires food businesses to tell customers if their food products contain any of the 14 allergens, but this can be done in different ways.
A business could provide full allergen information on a menu, or they could have a sign advising customers to ask a member of staff for this information. This can make it more difficult to know what ingredients are in a particular food.
Examples of unpackaged food include food sold in:
- bakeries – including in-store bakeries in supermarkets
- delis
- buffets
- salad bars
- "ready-to-eat" sandwich shops
- takeaways
- cafes, canteens and restaurants
- market stalls
If you or your child have a severe food allergy, you need to be careful when you eat out.
The following advice should help:
- let the staff know – when booking a table at a restaurant, make sure the staff know about any allergies.
 Ask for a firm guarantee that the specific food will not be in any of the dishes served. The Food Standards Agency (FSA) offers chef cards that provide information about allergies, which you can give to restaurant staff. As well as informing the chef and kitchen staff involved in cooking your food, let waiters and waitresses know so they understand the importance of avoiding cross-contamination when serving you.
Ask for a firm guarantee that the specific food will not be in any of the dishes served. The Food Standards Agency (FSA) offers chef cards that provide information about allergies, which you can give to restaurant staff. As well as informing the chef and kitchen staff involved in cooking your food, let waiters and waitresses know so they understand the importance of avoiding cross-contamination when serving you. - read the menu carefully and check for hidden ingredients – some food types contain other foods that can trigger allergies, which restaurant staff may have overlooked. Some desserts contain nuts (such as a cheesecake base) and some sauces contain wheat and peanuts.
- prepare for the worst – it's a good idea to prepare for any eventuality. Always take anti-allergy medicine with you when eating out, particularly an adrenalin auto-injector. Read more about using an auto-injector on our page about treating food allergies.
- use what's known as a taste test in older children – before your child begins to eat, ask them to take a tiny portion of the food and rub it against their lips to see if they experience a tingling or burning sensation.
 If they do, it suggests that the food will cause them to have an allergic reaction. However, the taste test does not work for all foods, so it should not be used as a substitute for the above advice.
If they do, it suggests that the food will cause them to have an allergic reaction. However, the taste test does not work for all foods, so it should not be used as a substitute for the above advice.
Further advice
Here's some more advice for parents:
- notify your child's school about their allergy – depending on how severe their allergy is, it may be necessary to give the staff at their school an emergency action plan in case of accidental exposure. Arrange for the school nurse or another staff member to hold a supply of adrenalin. Food allergy bracelets, which explain how other people can help your child in an emergency, are also available. Both the Anaphylaxis Campaign and Allergy UK provide advice on working with schools if your child has an allergy.
- let other parents know – young children may easily forget about their food allergy and accept food they should not have when visiting other children. Telling the parents of your child's friends about their allergy should help prevent this.

- educate your child – once your child is old enough to understand their allergy, it's important to give them clear, simple instructions about what foods to avoid and what they should do if they accidentally eat them.
Can food allergies be prevented?
It used to be thought that avoiding eating peanuts during pregnancy and when breastfeeding could help reduce the risk, but this theory has now been questioned.
There's some evidence that introducing peanuts early in life may reduce the risk of peanut allergy, but this may not apply to all children and requires confirmation from further studies.
It's important to follow the standard recommendations for pregnancy and breastfeeding, whether or not you have a family history of food allergies.
Further information
- Foods to avoid in pregnancy
- Breastfeeding and diet
- Food allergies in babies and young children
Page last reviewed: 15 April 2019
Next review due: 15 April 2022
Feeding for cow's milk protein allergy
- Nestlé Health Science
- health care
- Feeding with CMPA
Feeding and treatment of CMPA
The appearance of allergy symptoms in an infant always causes fear in parents. The first step is to consult a doctor who will conduct an examination, make the correct diagnosis and prescribe competent treatment. With the right approach, most symptoms will disappear within 2-4 weeks.
The first step is to consult a doctor who will conduct an examination, make the correct diagnosis and prescribe competent treatment. With the right approach, most symptoms will disappear within 2-4 weeks.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
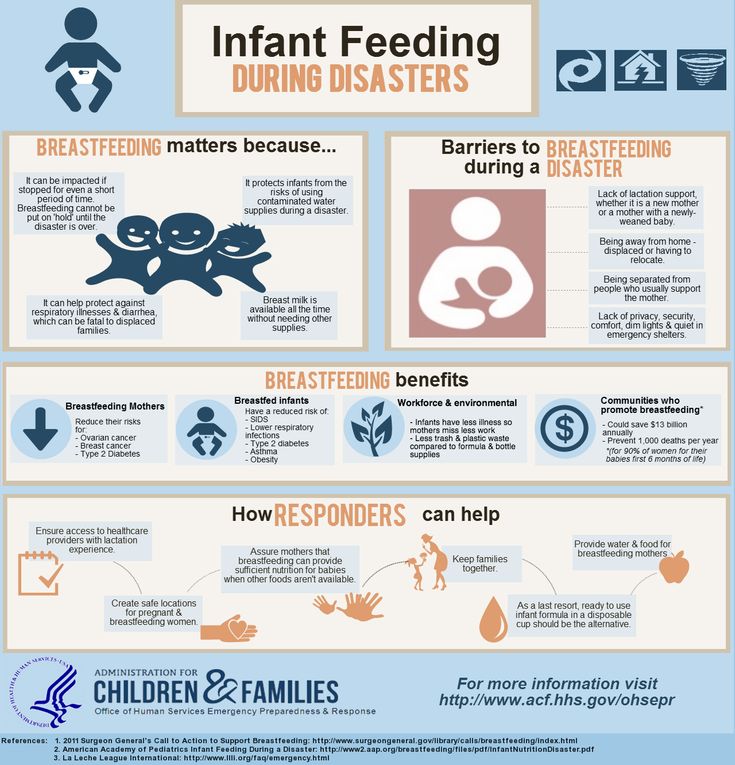
Breastfeeding is the best nutritional option for you and your baby. Even if your baby has been diagnosed with CMPA, breastfeeding should continue. Based on the severity of the symptoms and the presence of other types of food allergies in the child, the doctor will help determine the most appropriate diet for your child to quickly resolve the symptoms of the allergy.
Continue breastfeeding
A diagnosis of CMPA should not affect breastfeeding. Breastfeeding is the best nutritional option for your baby. Breast milk contains all the nutrients your baby especially needs during the first 6 months and continues to be beneficial for a long time to come. In addition to nutritional properties, breast milk contains antibodies, leukocytes and immune complexes, which together form the baby's immunity. In rare cases where the baby's immune system reacts to cow's milk proteins in breast milk, your doctor may recommend that you start a diet eliminating cow's milk proteins entirely (remember that a dairy-free diet may not be sufficient, as all traces of cow's milk must be eliminated) .
In addition to nutritional properties, breast milk contains antibodies, leukocytes and immune complexes, which together form the baby's immunity. In rare cases where the baby's immune system reacts to cow's milk proteins in breast milk, your doctor may recommend that you start a diet eliminating cow's milk proteins entirely (remember that a dairy-free diet may not be sufficient, as all traces of cow's milk must be eliminated) .
Early start: The sooner you start breastfeeding, the better. According to doctors, starting breastfeeding within 1 hour of birth ensures that your baby receives first milk (colostrum) and the protective factors it contains as soon as possible.
Emotional Benefit: Breastfeeding is an important factor in establishing and maintaining a strong emotional bond with your baby.
Long-term health benefits: Breastfeeding will also help develop your baby's immune system and thus protect your baby's health in the long term.
Protection for you and your baby: Studies have shown that breastfeeding reduces the risk of further infections in children, digestive tract diseases, diabetes, obesity and even leukemia. Breastfeeding is also good for you! Mothers who breastfeed have a reduced risk of developing diabetes, as well as breast and ovarian cancer.
Importance and benefits of breastfeeding
The sooner the better
- Breastfeeding during the first hour of birth ensures that the baby receives its first milk called colostrum
- Exclusive breastfeeding recommended for the first 6 months
Protective role for you and your child
- Breast milk is rich in protective factors that promote healthy growth and development in babies and reduce the risk of developing diseases later on.
- Mothers who breastfeed have a lower risk of developing diabetes and developing breast and ovarian cancer
Emotional Benefits
- You and your child develop and maintain a strong emotional bond.

What type of food is best for my child?
The only way to eliminate symptoms is to eliminate cow's milk proteins from the child's diet.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
If breastfeeding is not possible, or supplemented with infant formula, your doctor will help you select an appropriate infant formula that does not contain cow's milk proteins. These infant formulas are formulated with children in mind and contain all the necessary nutrients to support growth and development.
These specialized infant formulas can be based on:
- cow's milk processed in a certain way so that the proteins are no longer recognized by the baby's immune system and therefore do not cause an allergic reaction
- amino acids
The table below describes the differences between the two types of infant formula.
| SOGSB | COA | |
| What is it? | WGHB stands for "Whey Protein Hydrolysate Blend". The proteins in cow's milk that cause allergic reactions in a baby are severely broken down (hydrolyzed). | COA stands for "amino acid blend". This mixture does not contain any cow's milk proteins. |
| What does it consist of? | Cow's milk proteins have been broken down into smaller particles, which means they can no longer be recognized by the baby's immune system. Mixtures contain the macro- and micronutrients necessary for the child. | In severe forms of allergies, an amino acid mixture is used. This mixture does not contain any cow's milk proteins. The mixture is also enriched with all the necessary elements to support healthy growth and development. |
When and how to introduce complementary foods
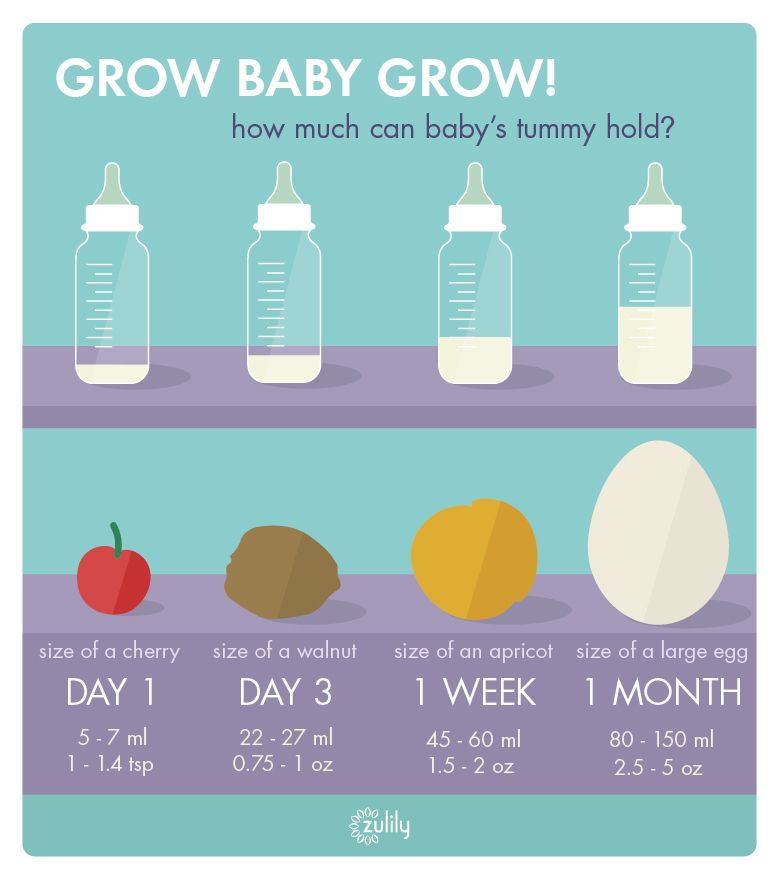
At 6 months of age, breastfeeding (or special infant formula) is no longer sufficient to fully support a child's growth and development and supplementary foods must be introduced into the diet. But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby.
But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby.
It is important to introduce complementary foods on time. The reflex responsible for moving solid foods in the mouth and swallowing them usually develops between 4 and 7 months of age. If you start solid foods too early, the baby will not be ready for it. Similarly, if you start too late, your child may not get all the nutritional support he or she needs, which increases the child's risk of developing essential vitamin and mineral deficiencies and stunting. Along with the nutritional benefits, introducing complementary foods will also provide sensory stimulation and improve your baby's motor skills.
IMPORTANT NOTE: : It is possible to continue breastfeeding if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
reaction to milk may go away, but sensitivity to peanuts will remain forever
- Main
- All about allergies
- Allergy in children
- Baby allergy: reaction to milk may go away, but sensitivity to peanuts remains forever
Contents
Allergies in children
The most common allergy in children is food. It is diagnosed in approximately 1-1. 5% of newborns. At the same time, if the baby is on artificial or mixed feeding, the risk of developing a reaction to food is higher.
5% of newborns. At the same time, if the baby is on artificial or mixed feeding, the risk of developing a reaction to food is higher.
And by the age of two, the percentage of children with food allergies, according to the American Academy of Allergy, Asthma and Immunology, is about 6%.
Among infants who are formula fed, the percentage of cases of food allergies at this age is even higher - about 7%. In addition, there is evidence that approximately 2-8% of children in the first year of life show symptoms of an allergy to cow's milk proteins. And while milk allergy usually subsides by the age of three, in some cases it can persist until the age of seven or eight.
What's more, children with milk allergies are more likely to develop other allergies in the future, such as seasonal allergic rhinitis, allergies to other foods, or even asthma.
Therefore, for the first six months of a baby's life, pediatricians recommend, if possible, to exclusively breastfeed the baby, and then gradually add a variety of complementary foods to the food, gradually increasing the number of new products. Such early prevention of food allergies has become recommended by doctors only recently. However, it doesn't always work either.
Such early prevention of food allergies has become recommended by doctors only recently. However, it doesn't always work either.
Causes of allergies in a child
Causes of allergic manifestations
If one of the parents has a food allergy, the risk of developing the same sensitivity in a child doubles. If both parents have food allergies, the risk is even greater. The seasonal allergic rhinitis and asthma mentioned above are also among the ailments that contribute to the development of sensitivity in a child to certain foods.
What foods can a baby be allergic to?
Although there are over 160 foods that can trigger allergies, 90% of all food reactions are caused by just eight of them. These include:
- Cow's milk
- Eggs
- Peanuts
- Tree nuts (e.g. walnuts, hazelnuts or almonds)
- Fish
- Shellfish
- Soya
- Wheat
At the same time, often up to 85% of all reactions are caused by just one allergen - cow's milk proteins. Next come eggs, peanuts and nuts.
Next come eggs, peanuts and nuts.
Pediatricians have previously advised against introducing potential allergens to an infant's diet until the age of two or three. Today, the American Academy of Pediatrics believes that there is no evidence that such waiting prevents food allergies. Moreover, there is a hypothesis that early exposure to allergens (not earlier than 6-7 months of age) may contribute to the development of tolerance to them. Therefore, the child is advised to introduce the same peanuts (in the form of a paste) up to 12 months, with an egg - about 7-8 months, but the introduction of whole milk is best done after 12 months, not only because of its allergenic potential, but also its severity digestion. You also need to do with honey, which can be the causative agent of infant botulism. It is better to refrain from him until 1-2 years.
In addition, when introducing a new product to a child, one should strictly adhere to certain rules, and not give several types of food unfamiliar to the baby at the same time.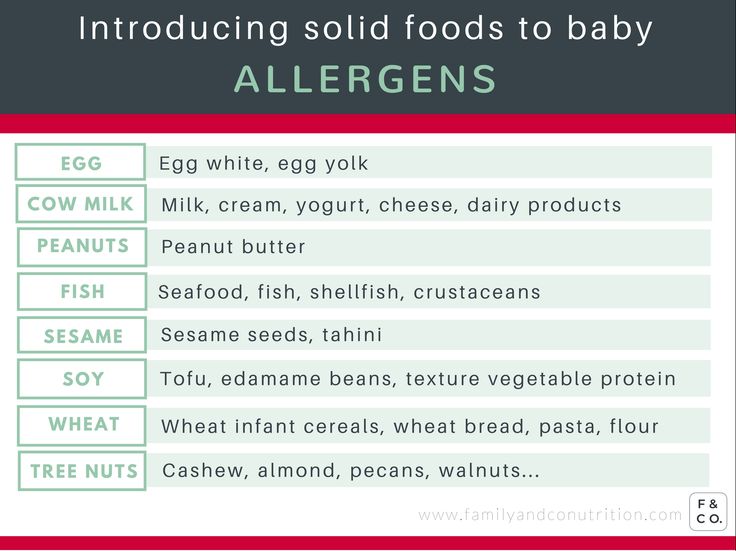 Each new ingredient is introduced no more than with a 3-5 day interval, and the introduction of products with a high level of allergic risk is better to "stretch" for a week. Such a scheme, in the event of a reaction, will help answer the frequent question of young parents: "How to understand what a child is allergic to?"
Each new ingredient is introduced no more than with a 3-5 day interval, and the introduction of products with a high level of allergic risk is better to "stretch" for a week. Such a scheme, in the event of a reaction, will help answer the frequent question of young parents: "How to understand what a child is allergic to?"
After all, observing the following recommendations, with changes in the behavior of the baby, the parents will have one specific "suspect". It is he who should be temporarily excluded from the menu in the event of a child's reaction. If the reaction occurs again - with the repeated introduction of food - the child should be shown to the doctor.
However, if it is too early for a formula-fed infant to introduce complementary foods and the infant still has a food reaction, or if the reaction persists despite avoiding various foods, it is possible that "baby milk" is the cause of the allergy. .
Baby allergy symptoms
How do you know if a baby is allergic to formula and not, for example, digestive problems or contact dermatitis due to detergents? There is no single answer. After all, the symptoms in some babies can develop immediately, while others may take hours, or even days. But the following symptoms will help you understand what an allergy looks like in young children.
After all, the symptoms in some babies can develop immediately, while others may take hours, or even days. But the following symptoms will help you understand what an allergy looks like in young children.
First, your baby may have gas. Due to the swollen and tense tummy, the child may often raise his legs up. If the baby cries at the same time, this may indicate colic.
Secondly, the child may openly show negativity towards feeding: experience difficulty swallowing due to reflux (backward reflux of food from the stomach into the esophagus), vomit or spit food. By
in addition, diarrhea may occur. Watery stools with blisters and foul odors are a common sign of formula allergy, which can lead to severe dehydration, so check with your pediatrician right away. However, sometimes instead of diarrhea in children, on the contrary, constipation is observed, which can also indicate an allergy.
Persistent runny nose, shortness of breath, active breathing, phlegm in the throat and chronic cough may also be due to an allergy to infant formula.

And finally, the most direct clue that a child has an allergy is a rash. The rashes may be itchy, ooze fluid, or look like crusts.
Milk protein allergy can be diagnosed using multicomponent molecular allergy tests. With a mixture whose ingredients are not always exactly known, it can be more difficult. However, your doctor may suggest certain tests after you inform him of your symptoms. These include allergy skin tests, blood tests, and stool tests. However, even positive results of such tests are not always evidence of a real allergy. Therefore, the doctor may recommend other methods, such as an elimination diet (diet for elimination).
As the baby matures, some allergy symptoms may disappear. For example, in most children, “colic” disappears after reaching six months. If you introduce a new food to your child, watch for one or more of the following symptoms:
- urticaria
- blush skin, rash
- swelling of the face, tongue or lips
- vomiting and/or diarrhea
- cough or wheezing
- shortness of breath
- loss of consciousness
If you see mild symptoms such as hives or a rash, see your pediatrician for a follow-up evaluation.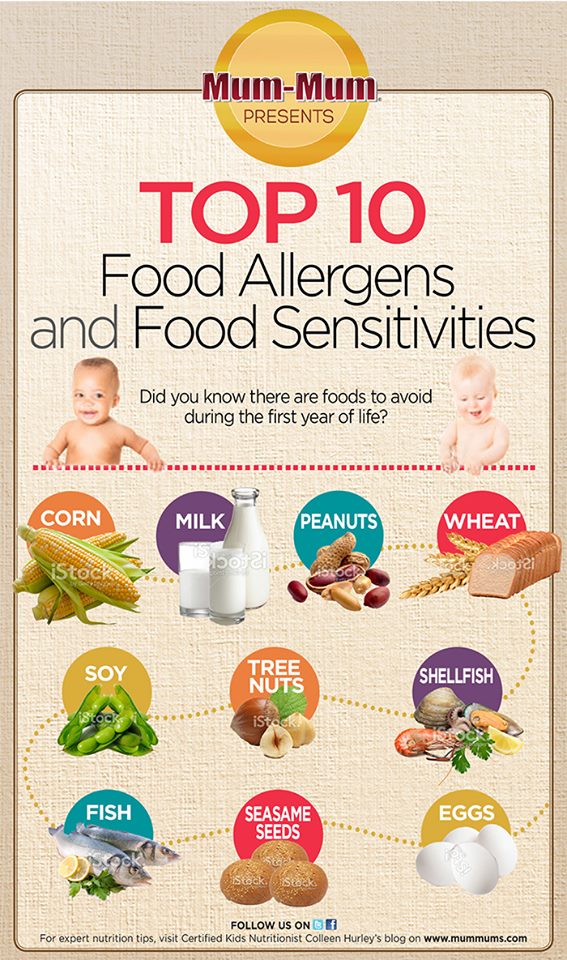
Types of rashes in children
Common types of rashes in children include:
Eczema is one of the most common skin conditions in newborns. There are different types of eczema, but atopic eczema is one of the most common in infants and young children. An eczema rash may consist of tiny red bumps or may look like scaly, dry skin. Babies under 6 months of age are more likely to develop eczema-like rashes on the scalp, face, and forehead, according to the National Eczema Association. In children aged 6 months to 1 year, the rash often appears on the knees and elbows.
Papular urticaria is a localized allergic reaction to a bug bite. Bites from various insects, including mosquitoes, ticks, and bed bugs, can cause a reaction that produces small clusters of red bumps. Although the disease usually affects children aged 2-6 years, papular urticaria can also occur in newborns.
Urticaria. Skin lesions may itch and vary in shape.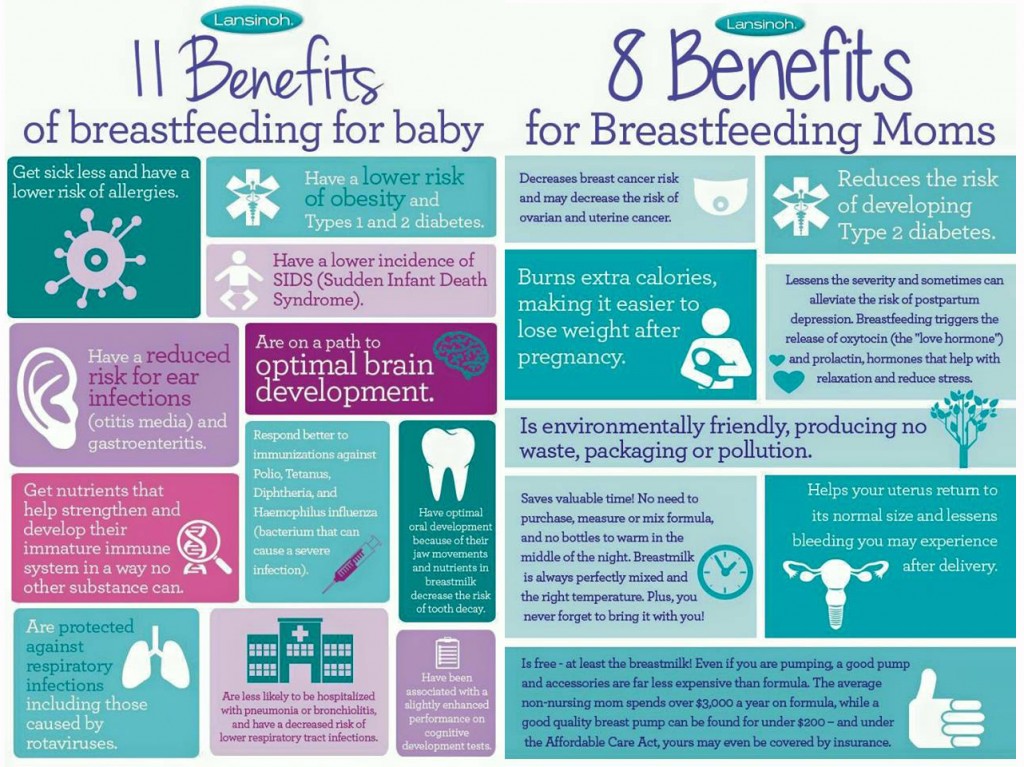 But, as a rule, they are pink or red with a thin red border. Urticaria can develop anywhere on the body.
But, as a rule, they are pink or red with a thin red border. Urticaria can develop anywhere on the body.
And when a child develops a rash after touching something, it is called allergic contact dermatitis . Its presence is evidenced by redness and itching, spots on the skin, etc. Nickel, metal in fasteners and buttons, poison ivy or hogweed, cosmetics, chemical dyes, skin medications such as the antibiotic neomycin, antihistamines, and pain relievers can provoke such reactions.
The child may also develop angioedema . It occurs in the deeper layers of the skin along with hives or separately from it. Swelling can happen anywhere, but is most common around the eyes and mouth, and on the arms and legs.
What should I do if my newborn has allergies?
If your child has difficulty breathing/wheezing, swelling of the face/lips, or severe vomiting or diarrhea after eating, call 911 immediately as the child may go into anaphylactic shock. If in this case adrenaline is not administered on time, the consequences can be even fatal.
If in this case adrenaline is not administered on time, the consequences can be even fatal.
And if a child develops a mild allergic reaction, this is no reason not to seek medical help. True, in this case a visit to the family doctor or pediatrician will be enough. The danger is that allergy symptoms may increase and worsen after further exposure to the allergen.
Your pediatrician can refer you to an allergist who will ask more questions, do a physical exam, and give you a better diagnosis.
If your doctor detects a food allergy to a particular food, the best strategy is to avoid that allergen.
You will have to read food labels carefully and avoid them unless you are sure of their ingredients.
Some allergies go away with time, such as allergies to eggs and milk. But allergies to peanuts, tree nuts, and shellfish most often persist for life.
Baby Allergy Diet
Although formula-fed babies are at greater risk of developing allergies, sometimes even a baby who has never eaten anything other than breast milk can have a reaction. Then the cause should be sought in the diet of the mother. Allergenic proteins from foods are stored in milk for 3-6 hours after consumption.
Then the cause should be sought in the diet of the mother. Allergenic proteins from foods are stored in milk for 3-6 hours after consumption.
If a child develops a food allergy, the mother's main task will be to determine what exactly is causing the reaction. Since allergy testing in young children is often not reliable, one way to determine which foods are a problem for your child is to keep a food diary.
Most babies react to the same eight major allergens found in breast milk, most commonly cow's milk. If the reason is indeed in milk, the nursing mother will have to temporarily abandon products based on it. In this case, you will have to look for an alternative to protein among fish, beef, chicken, eggs, nuts and beans. You can also consume soy milk fortified with calcium or calcium supplements.
If the case is in another product, the same principle will have to look for a replacement for its nutritional properties.
However, you need to understand that allergens can remain in breast milk for a long time, disappearing completely only after 1-2 weeks.
The child's symptoms may start to improve at this time, or it may take a month or more. But if the child does not show signs of improvement, or symptoms worsen after a month of dieting, you may need to eliminate other foods, but before doing so, be sure to consult a doctor.
Sometimes babies are allergic to more than one food. You don't have to give up breastfeeding. After all, breast milk provides protection against infections, reduces the risk of obesity and diabetes. In addition, breastfed babies are believed to have higher IQs.
Information sources:
- https://www.parents.com/baby/health/allergy/all-about-baby-allergies/
- https://doc.ua/bolezn/allergiya/allergiya-u-grudnogo-rebenka-i-detej
- https://www.momjunction.com/articles/common-baby-skin-allergies-and-its-causes_0083576/? amp=1
- http://www.healthofchildren.com/EF/Food-Allergies-and-Sensitivities.html
- https://www.medicalnewstoday.com/articles/322484
- https://www.