Pace feeding breastfed baby
Paced Bottle-Feeding: How to Mimic Breast-Feeding
Breast-feeding offers a host of benefits for your baby, but it’s not without its challenges.
Namely, if you are on a feeding schedule with your baby, it’s likely at some point in time that you may need to utilize bottle-feedings to allow yourself to return to work or simply be less of a slave to your breast-feeding schedule.
The challenge with bottle-feedings is the risk for “nipple confusion.” While modern science has made bottles as close to the real thing as possible, there’s still little substitute for the breast. Bottle-feedings are traditionally easier for the baby and can sometimes affect a baby’s latching ability — one of the most important aspects of breast-feeding.
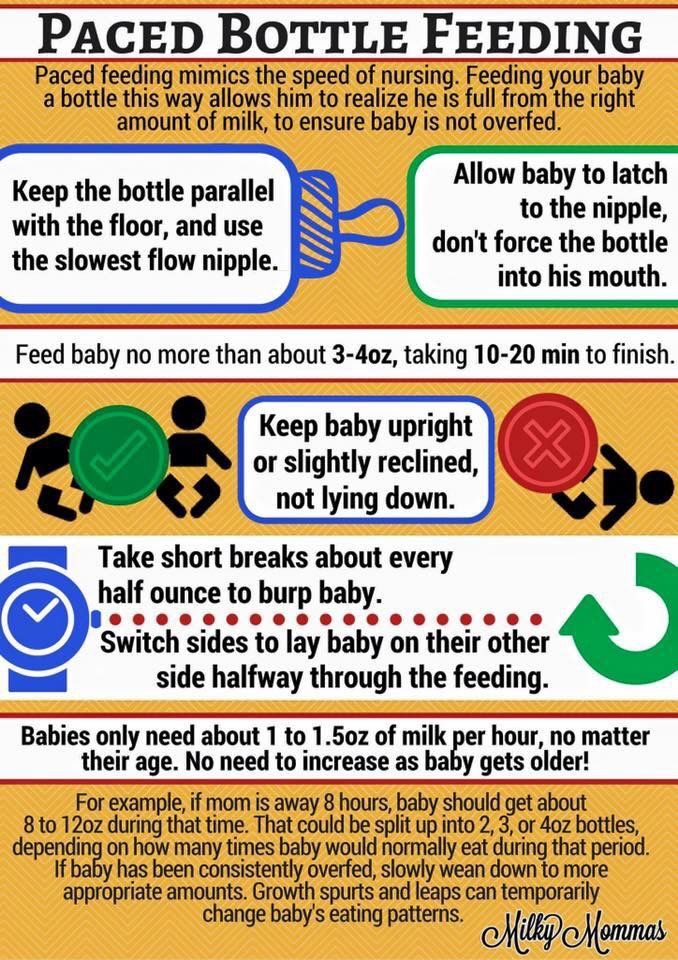
One approach to reducing the risk for nipple confusion is to use a paced bottle-feeding approach. Through paced bottle-feeding, you may be able to closely mimic nursing.
Traditional bottle-feeding involves giving babies bottles and allowing them to drink them at a steady rate.
While this accomplishes the task of feeding, a baby often receives the milk at a faster rate than when breast-feeding. This can affect a baby’s ability to return to the breast and also cause a baby to take in too much milk too quickly if you notice that your baby seems to suck without pausing using a traditional bottle-feeding method.
Paced bottle-feeding aims to slow feedings to closely mimic breast-feeding. Using techniques like keeping the bottle’s nipple half full and allowing the baby to pull the bottle’s nipple in, paced feeding can seem more like breast-feeding.
To pace feed, you will need a milk source, like formula or pumped milk. You will also need a bottle and a nipple for the bottle. Many nipple options are available on the market.
Share on Pinterest
However, for paced feedings, a wide-based, slow-flow nipple is recommended. This option can feel more like a mother’s nipple to a baby. If your baby has trouble accepting this nipple option, you may need to try a different option.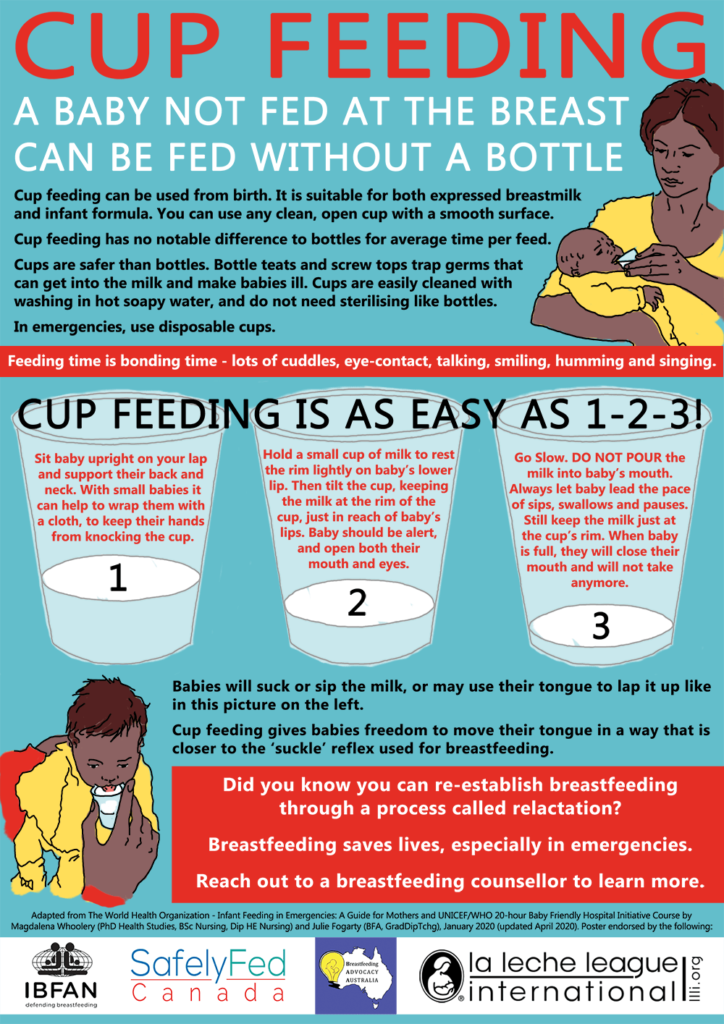
To pace feed your baby, place your baby in an upright position with plenty of head and neck support. Gently touch the bottle’s nipple to your baby’s mouth, much as you would during a breast-feeding session.
When your baby opens their mouth, gently advance the bottle’s nipple. If needed, you can stroke the baby’s cheek to encourage them to open the mouth. The ideal position will be where the nipple is at the top of the tongue, which helps to minimize air intake.
Hold the bottle parallel to the ground, and allow your baby to take in between five and 10 sucks of the bottle. The parallel position will allow for better flow control. Slightly pull the bottle backward to where the nipple is still touching the lower lip.
Allow your baby to pull the nipple back in, much like they would during a feeding. Another option is to reduce the bottle’s tilt to slow the flow until your baby starts sucking harder.
Remember to burp your baby frequently during the feeding. You can also switch the sides that your baby is held on, which can more closely mimic breast-feeding.
Paced feedings require closely watching your baby and the feeding cues that can indicate when more or less milk is needed, and when your baby is finished.
During breast-feeding, a baby is better able to control how much is eaten and the rate.
Bottle-feedings can make this process different, so it’s important to look for signs that your baby is taking in milk at too fast a rate. These include:
- body that appears to stiffen
- grimacing during feeding
- choking, gagging, or labored breathing while drinking
- lips that appear to turn blue
- milk that overflows from the mouth
- nasal flaring
- opening eyes widely
If you observe these signs, discontinue the feeding. If you resume the feeding, slow the height at which you hold the bottle.
Remember that you don’t have to finish a bottle with every feeding. Just as your baby may fall off the breast, the baby may not want to drink all of the milk available in the bottle.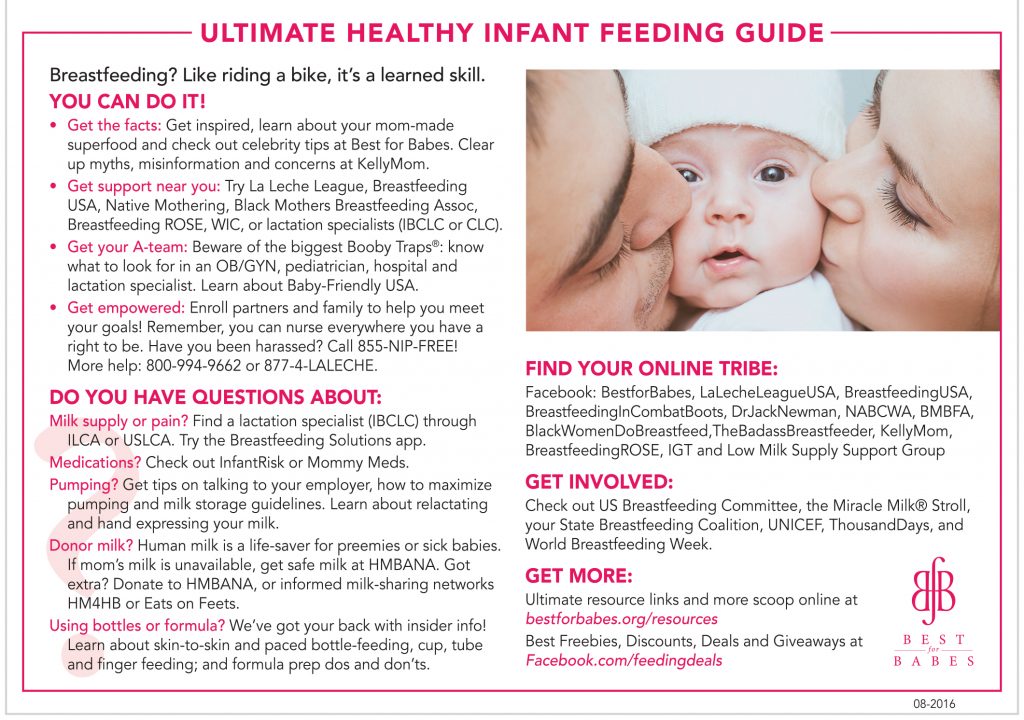
Like breast-feeding, paced feeding is a baby-controlled method for feeding your little one.
By mimicking the pattern and flow of breast-feeding, a baby is more likely to be able to switch between breast and bottle, if desired. By watching your baby’s cues, paced feedings can seem more natural to a baby.
How to Do It and Why You'd Want To
Paced bottle feeding is a method of feeding your baby that mimics breastfeeding. Find out why it’s so beneficial to feed baby this way, plus get step-by-step guidance.
If you’re planning to go back to work after baby, you’ve probably started pumping, storing milk, and have chosen a good bottle for breastfed babies. Now, you need to know how to properly feed baby with a bottle. Paced bottle feeding is the answer.
Paced bottle feeding can help reduce some of the drawbacks of bottle feeding and keep baby and mama happy and healthy.
What is paced bottle feeding?
Paced bottle feeding is a method of feeding your baby that mimics breastfeeding. As the name suggests, it involves pacing your feedings to allow baby to be in “control” of, process, and recognize his own “satiety,” or feeling of fullness. Baby is going to eat more slowly and work harder to get the milk (like he would with breast-feeding) as opposed to typical bottle feeding.
As the name suggests, it involves pacing your feedings to allow baby to be in “control” of, process, and recognize his own “satiety,” or feeling of fullness. Baby is going to eat more slowly and work harder to get the milk (like he would with breast-feeding) as opposed to typical bottle feeding.
Video of paced bottle feeding
The best way to really “describe” paced bottle feeding is to show you how it’s done…
In this video by Emerald Doulas you’ll notice that the:
- Baby is sitting more upright
- Caregiver tickles baby’s lips with bottle
- Nipple is then put into baby’s mouth
- The bottle is held horizontally, which slows the flow significantly
- After 20–30 seconds of feeding, the bottle is tipped downward or removed from baby’s mouth to stop the flow of milk (creating a similar pattern as in breastfeeding)
Get free updates on baby’s first year! – Free Updates on First Year [In-article]
Sign me up!
How to bottle feed the breast-fed baby: Paced bottle feeding
These tips are designed to replicate breast-feeding for breast-fed babies while mom’s away, but they can absolutely be helpful for formula-fed babies too!
When should baby be fed?
Whenever baby is hungry. A schedule can be helpful as a loose guideline (for example, feeding baby every 2–3 hours), but look for feeding cues first and foremost instead of going by the clock.
A schedule can be helpful as a loose guideline (for example, feeding baby every 2–3 hours), but look for feeding cues first and foremost instead of going by the clock.
Some signs baby is hungry include:
- Smaking lips
- Sucking fists
- Rooting (baby turning with mouth wide open toward any object that touches her cheek)
- Acting fussy or restless
Baby position
Hold baby in an upright position, as opposed to laying down. This helps baby to control the flow of milk better. He doesn’t have to be at an uncomfortable 90-degree angle, but only slightly reclined so that the bottle isn’t pouring down into baby’s mouth.
Offer the bottle horizontally
Lay the bottle nipple across baby’s lips (nipple pointed up) when baby starts rooting and opening his mouth. Let baby draw the nipple into his mouth and close his lips on the base of the nipple. Baby essentially is going to “latch” on the bottle nipple like he would a breast.
Once he’s latched on, keep the bottle horizontal. This allows baby to control the flow of milk better. This also helps the bottle to last the entire length of a normal feeding, usually 10–20 minutes, rather than baby gulping a bottle down in 5 minutes.
Baby learns to recognize when he’s full because he is not filling his belly before the signals of satiety can reach his brain.
You may also consider not allowing the milk to reach the nipple of the bottle for a few minutes while baby sucks. This mimics the letdown of breast-feeding and can help reduce the chances of nipple preference.
One caveat would be if you have a really fast letdown. If your baby only nurses for 5 minutes per feeding, holding bottle at a horizontal angle is not quite as important. And frankly, paced bottle feeding probably won’t be a necessity for you since your baby is already used to a fast flow.
Pausing
Babies at the breast will pause and take breaks often throughout a feeding. Baby’s caregiver should encourage pausing while bottle-feeding as well. If baby gets tense or starts gulping, lean him forward to allow the milk to flow away from the nipple to give him a break. If he pauses on his own, great!
Baby’s caregiver should encourage pausing while bottle-feeding as well. If baby gets tense or starts gulping, lean him forward to allow the milk to flow away from the nipple to give him a break. If he pauses on his own, great!
Switch sides
Just as mom does while breast-feeding, move baby from one side to the other halfway through the feeding. This helps baby avoid a side preference, and allows for new views and eye contact, which is excellent for his development.
Ending the feeding
One big drawback of bottle feeding is the risk of over-feeding. Look for cues that baby may be getting full, such as:
- Slower sucking
- Eyes wandering
- Falling asleep
- Hands are open and relaxed
When you think baby’s getting close to being full, remove the nipple from his mouth by gently twisting. Offer it again, and if he accepts, give him about 10 sucks, and repeat until he refuses. This will help teach him the feelings of satiety and reduce the chance of over-feeding.
Likewise, don’t coerce baby into drinking the last few drops of milk in the bottle. If he falls asleep, he is finished (an exception being newborns who may need to be awakened in the first few days to feed).
Benefits of paced bottle feeding
Breast-feeding is the biological design, so it makes sense that we would want to recreate this dynamic as best we can when bottle feeding. Paced bottle feeding has many benefits, which will help your child both in the short and long-term.
Baby avoids being under- or over-fed
If the caregiver is in charge of when and how much baby eats, baby is not likely to get the correct amount of milk. Paced bottle feeding helps baby be in charge, just like when he’s at the breast.
Less stressful for baby
Babies can become very stressed when laid on their backs to eat from a bottle. When baby swallows milk from a bottle, the negative pressure forces more milk out of the bottle. Baby has to keep gulping to avoid choking. Paced feeding gives baby the time and space to eat at his or her own pace.
Paced feeding gives baby the time and space to eat at his or her own pace.
Avoid colic
Proper feeding techniques and a good bottle can minimize colic-like symptoms. When milk pours into baby’s mouth, as happens with conventional bottle feeding, baby gulps to keep up, ingesting air in the process, which can cause gas.
Easier pumping for mom
If baby is being over-fed, mom needs to continually pump extra milk to replace the milk that’s being fed. Sometimes this leads to mama believing she has low milk supply. When baby is in charge, it’s much more likely that the amount mom pumps is exactly what baby needs. (Need more pumping tips? Check out this post!)
Supports breast-feeding relationship
Using a feeding technique that resembles breast-feeding is a great way to support the breast-feeding relationship and avoid a bottle preference. We are learning that babies don’t struggle as much with “nipple confusion” as with “flow preference.” If you are consistently giving a breast-fed baby fast-flowing bottles, they will probably prefer that easier, faster milk versus the breast.
May improve health later in life
One reason that breast-feeding is so great is that it allows baby to eat at his own pace, allowing him to learn his body’s cues for satiety. Studies have found that bottle feeding plays a large part in teaching overeating. Therefore, paced bottle feeding may contribute to healthier eating habits in the future.
Which is the best bottle to use?
Some lactation consultants like a narrower nipple found in traditional bottles versus the more breast-like nipples on some bottles. They prefer this style because baby can “latch” deeply on the narrower nipple, like with a breast. Other lactation consultants say it isn’t the bottle that matters as much as the pace of milk flow.
I like the breast-shaped nippled bottles because they are almost always a slow-flow bottle and the baby has to work for the milk, regardless of how you hold it (horizontal or vertical). Here’s our post on the best bottles for breastfed babies.
Will paced bottle feeding make my baby gassy?
When I first saw demos of this feeding method, I instantly thought of baby getting gassier. However, many lactation consultants say that air isn’t what causes gas. It’s more due to baby’s immature nervous and digestive systems.
If you notice an increase in gas, switch to a breast-shaped nipple bottle, which is slow flow. Also, try holding the bottle more horizontally so that less air interferes with the feeding.
Final word on paced bottle feeding
Whether you’re going back to work full-time, part-time, are exclusively pumping, or feed formula, paced bottle feeding can be a great way to support yourself, and especially, your baby.
How about you?
Have you tried paced feeding? How has it helped your baby?
References
- https://www.llli.org/docs/0000000000000001WAB/WAB_Tear_sheet_Toolkit/22_bfabreastfedbaby.pdf
- https://www.emeralddoulas.com/
Temperature while breastfeeding
07. 07.2022
07.2022
When someone develops a temperature and fever, it certainly causes excitement, and especially if such symptoms appear in a nursing mother. This is the first "bell" that something is wrong in a woman's body. The most dangerous is the temperature exceeding the threshold of 37.3 - this indicates that some inflammatory process has begun in the body, or that you do not have enough normal rest. When this happens, the first thing a woman asks herself is, is it possible to continue breastfeeding in this situation? nine0003
Many "experienced" people, having heard about the temperature of a young mother, immediately start sounding a false alarm: if a woman has a cold or falls ill with SARS, she should in no case continue to breastfeed her baby ! It is not true! Rather, on the contrary: at this time, the mother develops protective antibodies, which she can pass on to the child with milk - in this way, the baby receives a large share of its immunity .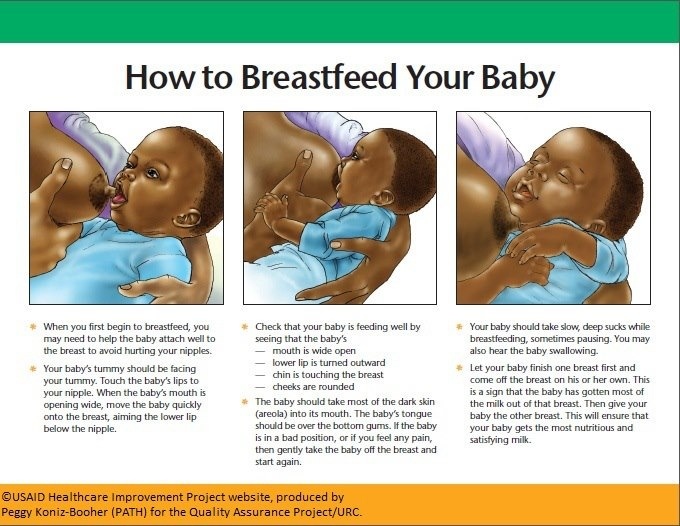 And plus, think about the fact that even weaning a child from breast , you will still be in the same room with him, play with him, feed him, pick him up, etc., that is, the infection can pass from you to the child no less.
And plus, think about the fact that even weaning a child from breast , you will still be in the same room with him, play with him, feed him, pick him up, etc., that is, the infection can pass from you to the child no less.
The chance of transmitting bacteria through saliva or hands is much higher than through breast milk. In addition, if the child is still very small, then transferring him to artificial nutrition is much more dangerous than continuing to eat milk from a mother who has a cold. After all, the woman will soon recover, but the child will be left without the most valuable food for him. Real need to stop feeding breastfeeding is very rare and is determined by specialists, and this is completely unrelated to common colds. Therefore, if the temperature during lactation is due to a mild virus, then it is not necessary to stop breastfeeding. It is better to remember that the infection should not spread to other members of your family. To protect them as much as possible, wear a gauze mask for any contact with the baby, wash your hands often and use only personal utensils and towels.
To protect them as much as possible, wear a gauze mask for any contact with the baby, wash your hands often and use only personal utensils and towels.
Why can't you stop feeding when you have a temperature?
Breastfeeding at fever should not be stopped for other reasons. Here are the main ones: If your mammary glands are not released from milk in time, then you risk earning a violation in their work. In the worst cases, such violations end with mastitis or lactostasis. Mother's milk is the best medicine for a baby. So, if you get sick and still infected the baby, then on the contrary, it is worth feeding him breastfeeding : this way you will give him all the necessary nutrients and antibodies that will ensure a speedy recovery.
If you stop breastfeeding your baby , you will still have to express milk (and you need to do this at least 6 times a day), which is especially painful when you have a temperature. The milk you express will need to be boiled, and temperature treatment, as you know, kills most of the nutrients contained in milk. If your temperature has risen above normal due to diseases of the cardiovascular system, diseases kidneys or kidney failure, due to problems with lungs and liver - then yes, in this case, breastfeeding really should be stopped. And if the temperature has risen due to menstruation or ovulation, as well as due to possible overeating and / or heavy loads, then you should not worry and you can safely continue breastfeeding. If your body temperature does not rise above 38.5 degrees, then you should not bring it down. But if the thermometer shows above this mark, then try lowering it with paracetamol or ibuprofen. Aspirin tablets can cause serious effects on a child's health, so it should not be used as an antipyretic and/or pain reliever. nine0003
The milk you express will need to be boiled, and temperature treatment, as you know, kills most of the nutrients contained in milk. If your temperature has risen above normal due to diseases of the cardiovascular system, diseases kidneys or kidney failure, due to problems with lungs and liver - then yes, in this case, breastfeeding really should be stopped. And if the temperature has risen due to menstruation or ovulation, as well as due to possible overeating and / or heavy loads, then you should not worry and you can safely continue breastfeeding. If your body temperature does not rise above 38.5 degrees, then you should not bring it down. But if the thermometer shows above this mark, then try lowering it with paracetamol or ibuprofen. Aspirin tablets can cause serious effects on a child's health, so it should not be used as an antipyretic and/or pain reliever. nine0003
Treatment with antibiotics
If the temperature has risen due to concomitant diseases such as mastitis, pneumonia or tonsillitis , then antibiotic treatment is necessary. Most modern antibiotic preparations, however strange it may seem, are still safe during lactation, although there is still a small chance of harming the baby. However, antibiotics should still be prescribed to you only by the doctor treating , and he will certainly select such pills that would be safe for breastfeeding. If you get sick and doctor has prescribed medication for you, remember the following:
Most modern antibiotic preparations, however strange it may seem, are still safe during lactation, although there is still a small chance of harming the baby. However, antibiotics should still be prescribed to you only by the doctor treating , and he will certainly select such pills that would be safe for breastfeeding. If you get sick and doctor has prescribed medication for you, remember the following:
- Take the prescribed medication before the baby sleeps for a long time, or immediately after breastfeeding : in this case, by the time of the next feeding, the concentration of the drug taken in the blood will be low.
- When using cold tablets, choose those based on a single main ingredient.
- If the treatment is not without strong drugs that are incompatible with lactation, then temporarily stop breastfeeding, but express milk: so after the course therapy you can easily continue to breastfeed your baby .

- Do not forget about folk antipyretics: hot tea with raspberries (jam or dried berries), linden tea have excellent antipyretic properties. Be careful when taking honey - although it is very useful, there is a possibility that it can cause a strong allergy in a baby .
Published in Pregnancy and Pregnancy Management, Mammology Premium Clinic
Feeding when sick | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less susceptible to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often 1 and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed? nine0093
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. nine0081 7
“Breastfeeding gives the baby everything she needs during her illness. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. nine0081 8 When your baby is sick, the level of immune-boosting cells (leukocytes) in your milk also rises sharply. 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip." nine0003
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time. If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed? nine0093
Occasionally, if a child feels unwell, they may not have an appetite or energy to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable. nine0003
You can express milk with one of our convenient breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue breastfeeding if I become ill myself? nine0093
If you feel unwell, you may not want to, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. Moreover, the antibodies contained in your milk will help reduce the risk of your baby getting the same virus 13 .
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson. nine0003
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex ** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery. nine0003
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers. Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, it is permissible to take certain medications. 9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues. nine0003
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
“I was on high doses of epilepsy medication, but I was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to ensure my son was safe and to minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged. nine0003
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.
“If the baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account. nine0003
Surgery under local or general anesthesia does not necessarily mean that breastfeeding will have to be stopped, or milk will need to be pumped and discarded. By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, in all circumstances it is best to consult your doctor or attending physician first. nine0003
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk.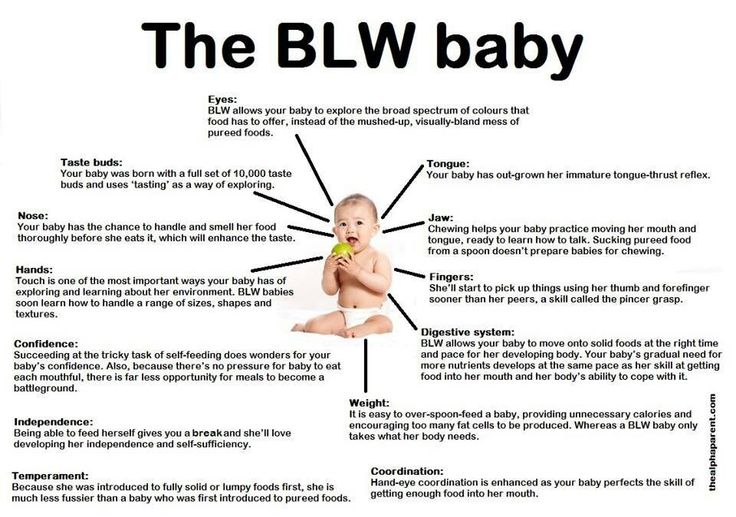 nine0081 11.12 Consult with a qualified professional about your condition to decide if breastfeeding can continue in such cases.
nine0081 11.12 Consult with a qualified professional about your condition to decide if breastfeeding can continue in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if possible. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page. nine0003
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. nine0192 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet]. "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458. nine0192
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F., Hartmann P.I., "On the threshold of a new discovery: the potential of breast milk stem cells." Adv Nutr. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0192 2017;12(9):500-506.
Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0192 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188. nine0192
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps".