Paced bottle feeding for the breastfed baby
Paced Bottle-Feeding: How to Mimic Breast-Feeding
Breast-feeding offers a host of benefits for your baby, but it’s not without its challenges.
Namely, if you are on a feeding schedule with your baby, it’s likely at some point in time that you may need to utilize bottle-feedings to allow yourself to return to work or simply be less of a slave to your breast-feeding schedule.
The challenge with bottle-feedings is the risk for “nipple confusion.” While modern science has made bottles as close to the real thing as possible, there’s still little substitute for the breast. Bottle-feedings are traditionally easier for the baby and can sometimes affect a baby’s latching ability — one of the most important aspects of breast-feeding.
One approach to reducing the risk for nipple confusion is to use a paced bottle-feeding approach. Through paced bottle-feeding, you may be able to closely mimic nursing.
Traditional bottle-feeding involves giving babies bottles and allowing them to drink them at a steady rate.
While this accomplishes the task of feeding, a baby often receives the milk at a faster rate than when breast-feeding. This can affect a baby’s ability to return to the breast and also cause a baby to take in too much milk too quickly if you notice that your baby seems to suck without pausing using a traditional bottle-feeding method.
Paced bottle-feeding aims to slow feedings to closely mimic breast-feeding. Using techniques like keeping the bottle’s nipple half full and allowing the baby to pull the bottle’s nipple in, paced feeding can seem more like breast-feeding.
To pace feed, you will need a milk source, like formula or pumped milk. You will also need a bottle and a nipple for the bottle. Many nipple options are available on the market.
Share on Pinterest
However, for paced feedings, a wide-based, slow-flow nipple is recommended. This option can feel more like a mother’s nipple to a baby. If your baby has trouble accepting this nipple option, you may need to try a different option.
To pace feed your baby, place your baby in an upright position with plenty of head and neck support. Gently touch the bottle’s nipple to your baby’s mouth, much as you would during a breast-feeding session.
When your baby opens their mouth, gently advance the bottle’s nipple. If needed, you can stroke the baby’s cheek to encourage them to open the mouth. The ideal position will be where the nipple is at the top of the tongue, which helps to minimize air intake.
Hold the bottle parallel to the ground, and allow your baby to take in between five and 10 sucks of the bottle. The parallel position will allow for better flow control. Slightly pull the bottle backward to where the nipple is still touching the lower lip.
Allow your baby to pull the nipple back in, much like they would during a feeding. Another option is to reduce the bottle’s tilt to slow the flow until your baby starts sucking harder.
Remember to burp your baby frequently during the feeding. You can also switch the sides that your baby is held on, which can more closely mimic breast-feeding.
Paced feedings require closely watching your baby and the feeding cues that can indicate when more or less milk is needed, and when your baby is finished.
During breast-feeding, a baby is better able to control how much is eaten and the rate.
Bottle-feedings can make this process different, so it’s important to look for signs that your baby is taking in milk at too fast a rate. These include:
- body that appears to stiffen
- grimacing during feeding
- choking, gagging, or labored breathing while drinking
- lips that appear to turn blue
- milk that overflows from the mouth
- nasal flaring
- opening eyes widely
If you observe these signs, discontinue the feeding. If you resume the feeding, slow the height at which you hold the bottle.
Remember that you don’t have to finish a bottle with every feeding. Just as your baby may fall off the breast, the baby may not want to drink all of the milk available in the bottle.
Like breast-feeding, paced feeding is a baby-controlled method for feeding your little one.
By mimicking the pattern and flow of breast-feeding, a baby is more likely to be able to switch between breast and bottle, if desired. By watching your baby’s cues, paced feedings can seem more natural to a baby.
How to Do It and Why You'd Want To
Paced bottle feeding is a method of feeding your baby that mimics breastfeeding. Find out why it’s so beneficial to feed baby this way, plus get step-by-step guidance.
If you’re planning to go back to work after baby, you’ve probably started pumping, storing milk, and have chosen a good bottle for breastfed babies. Now, you need to know how to properly feed baby with a bottle. Paced bottle feeding is the answer.
Paced bottle feeding can help reduce some of the drawbacks of bottle feeding and keep baby and mama happy and healthy.
What is paced bottle feeding?
Paced bottle feeding is a method of feeding your baby that mimics breastfeeding. As the name suggests, it involves pacing your feedings to allow baby to be in “control” of, process, and recognize his own “satiety,” or feeling of fullness. Baby is going to eat more slowly and work harder to get the milk (like he would with breast-feeding) as opposed to typical bottle feeding.
As the name suggests, it involves pacing your feedings to allow baby to be in “control” of, process, and recognize his own “satiety,” or feeling of fullness. Baby is going to eat more slowly and work harder to get the milk (like he would with breast-feeding) as opposed to typical bottle feeding.
Video of paced bottle feeding
The best way to really “describe” paced bottle feeding is to show you how it’s done…
In this video by Emerald Doulas you’ll notice that the:
- Baby is sitting more upright
- Caregiver tickles baby’s lips with bottle
- Nipple is then put into baby’s mouth
- The bottle is held horizontally, which slows the flow significantly
- After 20–30 seconds of feeding, the bottle is tipped downward or removed from baby’s mouth to stop the flow of milk (creating a similar pattern as in breastfeeding)
Get free updates on baby’s first year! – Free Updates on First Year [In-article]
Sign me up!
How to bottle feed the breast-fed baby: Paced bottle feeding
These tips are designed to replicate breast-feeding for breast-fed babies while mom’s away, but they can absolutely be helpful for formula-fed babies too!
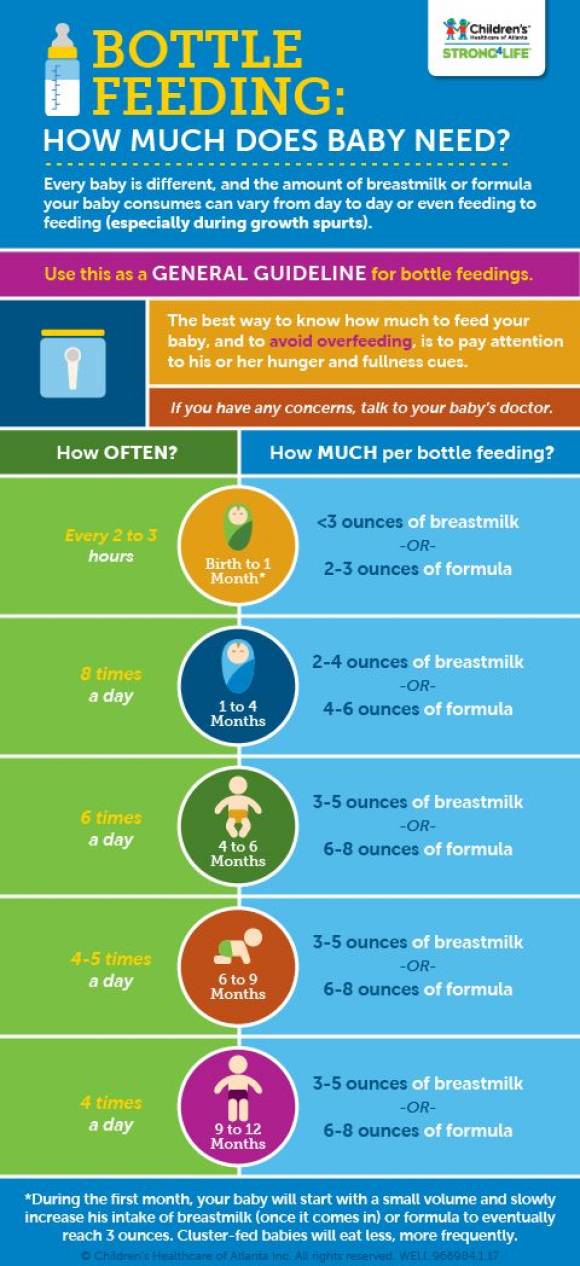
When should baby be fed?
Whenever baby is hungry. A schedule can be helpful as a loose guideline (for example, feeding baby every 2–3 hours), but look for feeding cues first and foremost instead of going by the clock.
A schedule can be helpful as a loose guideline (for example, feeding baby every 2–3 hours), but look for feeding cues first and foremost instead of going by the clock.
Some signs baby is hungry include:
- Smaking lips
- Sucking fists
- Rooting (baby turning with mouth wide open toward any object that touches her cheek)
- Acting fussy or restless
Baby position
Hold baby in an upright position, as opposed to laying down. This helps baby to control the flow of milk better. He doesn’t have to be at an uncomfortable 90-degree angle, but only slightly reclined so that the bottle isn’t pouring down into baby’s mouth.
Offer the bottle horizontally
Lay the bottle nipple across baby’s lips (nipple pointed up) when baby starts rooting and opening his mouth. Let baby draw the nipple into his mouth and close his lips on the base of the nipple. Baby essentially is going to “latch” on the bottle nipple like he would a breast.
Once he’s latched on, keep the bottle horizontal. This allows baby to control the flow of milk better. This also helps the bottle to last the entire length of a normal feeding, usually 10–20 minutes, rather than baby gulping a bottle down in 5 minutes.
Baby learns to recognize when he’s full because he is not filling his belly before the signals of satiety can reach his brain.
You may also consider not allowing the milk to reach the nipple of the bottle for a few minutes while baby sucks. This mimics the letdown of breast-feeding and can help reduce the chances of nipple preference.
One caveat would be if you have a really fast letdown. If your baby only nurses for 5 minutes per feeding, holding bottle at a horizontal angle is not quite as important. And frankly, paced bottle feeding probably won’t be a necessity for you since your baby is already used to a fast flow.
Pausing
Babies at the breast will pause and take breaks often throughout a feeding. Baby’s caregiver should encourage pausing while bottle-feeding as well. If baby gets tense or starts gulping, lean him forward to allow the milk to flow away from the nipple to give him a break. If he pauses on his own, great!
Baby’s caregiver should encourage pausing while bottle-feeding as well. If baby gets tense or starts gulping, lean him forward to allow the milk to flow away from the nipple to give him a break. If he pauses on his own, great!
Switch sides
Just as mom does while breast-feeding, move baby from one side to the other halfway through the feeding. This helps baby avoid a side preference, and allows for new views and eye contact, which is excellent for his development.
Ending the feeding
One big drawback of bottle feeding is the risk of over-feeding. Look for cues that baby may be getting full, such as:
- Slower sucking
- Eyes wandering
- Falling asleep
- Hands are open and relaxed
When you think baby’s getting close to being full, remove the nipple from his mouth by gently twisting. Offer it again, and if he accepts, give him about 10 sucks, and repeat until he refuses. This will help teach him the feelings of satiety and reduce the chance of over-feeding.
Likewise, don’t coerce baby into drinking the last few drops of milk in the bottle. If he falls asleep, he is finished (an exception being newborns who may need to be awakened in the first few days to feed).
Benefits of paced bottle feeding
Breast-feeding is the biological design, so it makes sense that we would want to recreate this dynamic as best we can when bottle feeding. Paced bottle feeding has many benefits, which will help your child both in the short and long-term.
Baby avoids being under- or over-fed
If the caregiver is in charge of when and how much baby eats, baby is not likely to get the correct amount of milk. Paced bottle feeding helps baby be in charge, just like when he’s at the breast.
Less stressful for baby
Babies can become very stressed when laid on their backs to eat from a bottle. When baby swallows milk from a bottle, the negative pressure forces more milk out of the bottle. Baby has to keep gulping to avoid choking. Paced feeding gives baby the time and space to eat at his or her own pace.
Paced feeding gives baby the time and space to eat at his or her own pace.
Avoid colic
Proper feeding techniques and a good bottle can minimize colic-like symptoms. When milk pours into baby’s mouth, as happens with conventional bottle feeding, baby gulps to keep up, ingesting air in the process, which can cause gas.
Easier pumping for mom
If baby is being over-fed, mom needs to continually pump extra milk to replace the milk that’s being fed. Sometimes this leads to mama believing she has low milk supply. When baby is in charge, it’s much more likely that the amount mom pumps is exactly what baby needs. (Need more pumping tips? Check out this post!)
Supports breast-feeding relationship
Using a feeding technique that resembles breast-feeding is a great way to support the breast-feeding relationship and avoid a bottle preference. We are learning that babies don’t struggle as much with “nipple confusion” as with “flow preference.” If you are consistently giving a breast-fed baby fast-flowing bottles, they will probably prefer that easier, faster milk versus the breast.![]()
May improve health later in life
One reason that breast-feeding is so great is that it allows baby to eat at his own pace, allowing him to learn his body’s cues for satiety. Studies have found that bottle feeding plays a large part in teaching overeating. Therefore, paced bottle feeding may contribute to healthier eating habits in the future.
Which is the best bottle to use?
Some lactation consultants like a narrower nipple found in traditional bottles versus the more breast-like nipples on some bottles. They prefer this style because baby can “latch” deeply on the narrower nipple, like with a breast. Other lactation consultants say it isn’t the bottle that matters as much as the pace of milk flow.
I like the breast-shaped nippled bottles because they are almost always a slow-flow bottle and the baby has to work for the milk, regardless of how you hold it (horizontal or vertical). Here’s our post on the best bottles for breastfed babies.
Will paced bottle feeding make my baby gassy?
When I first saw demos of this feeding method, I instantly thought of baby getting gassier. However, many lactation consultants say that air isn’t what causes gas. It’s more due to baby’s immature nervous and digestive systems.
If you notice an increase in gas, switch to a breast-shaped nipple bottle, which is slow flow. Also, try holding the bottle more horizontally so that less air interferes with the feeding.
Final word on paced bottle feeding
Whether you’re going back to work full-time, part-time, are exclusively pumping, or feed formula, paced bottle feeding can be a great way to support yourself, and especially, your baby.
How about you?
Have you tried paced feeding? How has it helped your baby?
References
- https://www.llli.org/docs/0000000000000001WAB/WAB_Tear_sheet_Toolkit/22_bfabreastfedbaby.pdf
- https://www.emeralddoulas.com/
Bottle feeding at the optimal pace for a breastfed baby
Contents
- What is stimulated bottle feeding?
- What can I do to speed up bottle feeding?
- What are the stages of stimulated bottle feeding?
- What precautions should be taken when using stimulated bottle feeding?
- Conclusion
Breastfeeding offers many benefits for your baby, but it's not without its challenges.
Namely, if you are on your baby's feeding schedule, it is likely that at some point you may need to use bottle feeding to allow yourself to get back to work or simply be less dependent on your breastfeeding schedule.
A problem with bottle feeding is the risk of 'nipple confusion'. While modern science has made bottles as close to real as possible, breast replacements are still scarce. Bottle feeding is traditionally easier on the baby and can sometimes affect the baby's ability to breastfeed, one of the most important aspects of breastfeeding.
One approach to reduce the risk of nipple confusion is to use tempo formula feeding. With Rhythmic Bottle Feeding, you can accurately mimic breastfeeding.
What is stimulated bottle feeding?
Traditional bottle feeding involves giving children bottles and allowing them to drink them at a constant rate.
While this solves the problem of feeding, the baby often receives milk faster than when breastfeeding. This can affect the baby's ability to return to the breast and also cause the baby to suck too much milk too quickly if you notice that your baby is sucking without pauses with the traditional bottle feeding method.
This can affect the baby's ability to return to the breast and also cause the baby to suck too much milk too quickly if you notice that your baby is sucking without pauses with the traditional bottle feeding method.
Stimulated bottle feeding focuses on slow feeding to mimic breastfeeding as much as possible. By using techniques such as keeping the bottle nipple half full and allowing the baby to pull the bottle nipple inward, tempo feeding can be more like breastfeeding.
What can I do to speed up bottle feeding?
For rhythmic feeding you will need a milk source such as formula or expressed milk. You will also need a bottle and a bottle nipple. There are many types of nipples available on the market.
However, for stimulated feeding, a teat with a wide base and slow flow is recommended. This option may be more like a mother's nipple to her baby. If this pacifier option is difficult for your child to accept, you may need to try another option.
What are the stages of stimulated bottle feeding?
To feed your baby at tempo, place your baby in an upright position with adequate head and neck support. Gently touch the nipple of the bottle to your baby's mouth, as you would when breastfeeding.
Gently touch the nipple of the bottle to your baby's mouth, as you would when breastfeeding.
When your baby opens her mouth, gently pull the nipple out of the bottle. If necessary, you can stroke your baby's cheek to encourage him to open his mouth. The ideal position is for the nipple to be on top of the tongue, which helps minimize air intake.
Hold the bottle parallel to the ground and let your baby take five to ten sips from the bottle. The parallel position will allow better control of the flow. Pull the bottle back slightly so that the nipple is still touching the lower lip.
Let the baby retract the nipple, as during feeding. Another option is to decrease the slope of the bottle to slow down the flow until the baby starts sucking harder.
Remember to spit up your baby frequently while feeding. You can also change the sides you hold your baby on, which can mimic breastfeeding more accurately.
Tempo feeding requires careful observation of the baby and feeding signals that can indicate when more or less milk is needed and when your baby has finished.
What precautions should be taken when using stimulated bottle feeding?
During breastfeeding, the baby has better control over the amount eaten and speed.
Bottle feeding can change this process, so it's important to look out for signs that your baby is suckling too fast. This includes:
- a body that feels stiff
- wrinkles when feeding
- choking, gagging, or difficulty breathing while drinking
- lips that appear blue
- milk that comes out of the mouth
- nasal swelling
- eyes wide open
Stop feeding if you see these signs. If you resume feeding, reduce the height at which you hold the bottle.
Remember that you don't have to finish the bottle every time you feed. In the same way that your baby may fall off the breast, the baby may not want to drink all the milk from the bottle.
Conclusion
Like breastfeeding, rhythmic feeding is a child-controlled method of feeding your baby.
By mimicking the pattern and flow of breastfeeding, the baby is likely to be able to switch between breast and bottle as desired. By observing your baby's signals, tempo feeding may seem more natural to the baby.
Baby won't take bottle | Philips Avent
search support iconSearch keywords
Home ›› What to do when your baby refuses a bottle
↑ Top
In most cases, switching a baby from breastfeeding to bottle feeding does not cause any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent bottle feeding products:
So why is your baby refusing the bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your approach and feeding technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full.
 So the child can eat at his own pace.
So the child can eat at his own pace. - Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain body contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Move while feeding.
Sometimes all it takes is a little wiggle or walk to get your baby to take the bottle. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast. Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast.
 Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Give preference to nipples with an anti-colic valve that vents air out of the bottle. Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or only bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
Refs:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 02.10.2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website.