Pumping breast milk and feeding baby
Breastfeeding FAQs: Pumping (for Parents)
Many breastfeeding moms pump their breast milk to give to their baby when they are away. Here’s some information about pumps and when and how to pump safely.
What Type of Pump Do I Need?
That really depends on how often you plan to use your pump. Manual pumps tend to be best for occasional pumping, while electric pumps are better for regular or daily pumping.
- Manual pumps. Manual (or hand-operated) pumps are small and inexpensive (less than $50) compared with electric pumps. They take more effort and more time than electric pumps to draw out milk, so they’re better for occasional use. Many women keep a manual pump as a back-up in case there’s a power outage or problem with their electric pump.
- Electric pumps. Electric (or automatic) pumps can be easier to use than manual pumps because they don't require as much physical effort and can draw out the milk faster.
Many models let you pump both breasts at once, which is a real time-saver. This also may increase your milk supply. Electric pumps come in many sizes. Most can be plugged in or are battery-operated.
Most insurance plans will cover a breast pump. Call to find out if you can receive a free pump. If not, you can buy or rent a breast pump from lactation consultants, hospitals, retail stores, and online. If you don't have the money to buy or rent a pump, contact Women, Infants, and Children (WIC) to find out about their free or low-cost pump program and see if you qualify.
Are Used Pumps OK?
It's not a good idea to borrow or buy someone else's used pump. This is because bacteria and viruses from the previous owner can get trapped inside the pump. They are potentially hazardous to your baby's health, even with repeated sterilization and cleaning.
Hospital-grade pumps, though, are meant for more than one user. These pumps let women use their own accessory kits, which lowers the risk of contamination.
Why Would I Need to Pump Right After Birth?
If your baby can’t eat due to an early birth or illness, or if you are separated from each other, you can pump your milk. In the first 2 hours after birth, hand-express your breast and then begin pumping every 2–3 hours. Use a hospital-grade pump or an electric pump, if possible. You will make only small amounts of colostrum (a rich “pre-milk”) until your milk fully comes in. Keep pumping and your supply will slowly increase.
If your baby is exclusively breastfeeding and gaining weight as expected, there’s no need to pump right away. It can be tempting to build up a supply of milk for later. But this isn’t a good idea because it can cause an over-supply of milk and keep your breasts engorged (over-full) for a longer period of time than expected.
When Can I Begin Pumping to Build Up a Milk Supply?
If you'll return to work after maternity leave or plan to spend time away from your baby, start pumping a couple of weeks before. This will give you time to practice with the pump and get comfortable using it. It also gives your baby time to learn how to drink from a bottle.
This will give you time to practice with the pump and get comfortable using it. It also gives your baby time to learn how to drink from a bottle.
How much milk women can express with a pump varies. Don’t be discouraged if it takes a few pumping sessions for you to express enough milk for a full bottle. Some women find that they express more milk when their baby is close by, if they look at a picture of the baby, or if they smell a piece of the baby’s clothing. While it may take time to get the hang of pumping, it’s a great way to ensure that your baby continues to get breast milk even when you’re not there.
If you have questions or concerns about how much milk you are expressing, talk to a lactation consultant or your health care provider.
What Can Make Pumping Easier?
It can take a little practice and time for your body (and your mind) to get used to producing milk without your baby's help. These tips can make things easier:
- Find a comfortable spot and relax.
 Your let-down reflex (when milk is released) can be affected if you're frustrated, anxious, or rushed. So sit in a comfortable spot and try not to think about other things you need to do. Listening to soothing music can help. Find out what works best for you so that you can relax.
Your let-down reflex (when milk is released) can be affected if you're frustrated, anxious, or rushed. So sit in a comfortable spot and try not to think about other things you need to do. Listening to soothing music can help. Find out what works best for you so that you can relax. - Massage your breast before and during pumping. Using your hands to massage and compress the breast can help empty them more efficiently. This can be hard if pumping both breasts at once so consider wearing a hands-free bra.
- Hold something that reminds you of your baby, like a picture or video on your phone, or has your baby's scent, like a blanket or piece of clothing. This can help you get in the right frame of mind and trigger let-down.
- Place the breast shield (flange) correctly over your breast. The breast shield is the plastic cup that goes over the nipple and areola (the dark circle of skin around your nipple) when you pump.
 Make sure it’s covering your entire nipple and areola (not just the top of your nipple) and get a good seal. If this doesn’t happen, you may be uncomfortable and less likely to get the milk you need.
Make sure it’s covering your entire nipple and areola (not just the top of your nipple) and get a good seal. If this doesn’t happen, you may be uncomfortable and less likely to get the milk you need. - Find the right size breast shield for your breast. While pumping, your nipple should move freely inside the tunnel of the breast shield without too much of your areola being drawn in. If this is happening or pumping is uncomfortable, try a different flange size. Most pumps come with different flange sizes, so find the best fit.
- Adjust the speed and suction to the level that's comfortable for you when using an electric pump. This will help prevent any discomfort. It’s best to use the lowest setting that allows milk to flow comfortably.
Where Can I Pump at Work?
If you're pumping at work, find a discreet place where you feel comfortable.
Many companies offer their employees pumping and nursing areas. If yours doesn't, ask your supervisor or the human resources department about an office or other private area that might be suitable. Employers are required by law to provide an appropriate area (that's not a bathroom) for employees to pump breast milk and reasonable time to do so.
Employers are required by law to provide an appropriate area (that's not a bathroom) for employees to pump breast milk and reasonable time to do so.
How Do I Clean Pump Parts?
Before their first use, wash and then sterilize breast pump supplies (for example, the breast shields and any other part that touches your breasts or your milk) by boiling them for 5 to 10 minutes. Check the manufacturer's directions about how long to boil the parts.
You also can sterilize the parts with a countertop or microwaveable sterilizer, but boiling works just as well and costs nothing. After that, wash the bottles, nipples, and pump supplies in hot, soapy water (or run them through the dishwasher) after every use. They can spread bacteria if not cleaned properly.
Pumping Milk - La Leche League International
There are times when mothers are separated from their child for work or for school. It is important to know that you can still provide milk for your child when you are away and you can maintain your breastfeeding relationship.![]()
How long you are apart from you baby influences this decision. Ideally, you would pump as often as your baby would nurse. This may not be possible with your work/ school schedule. Most mothers find that pumping every 2-3 hours maintains their milk supply and does not cause them to become uncomfortably full.
For example, if a mother worked an 8 hour work day, she would nurse her child before coming to work, then pump mid-morning, at lunchtime and then mid-afternoon. She would nurse her baby when she returned home.
Should I single or double pump?Using a pump that can express milk from both breasts at the same time will save the most time. It may take about 15 minutes to pump both breasts instead of 30 minutes or more to pump each breast separately. Double pumping also provides very strong stimulation to keep a good milk supply. Prolactin, which is an important hormone for making milk, becomes very elevated when mothers double pump.
If it is possible for you to go home at lunch, or have someone meet you on your break with your baby, you can breastfeed instead of pump. Some employers have onsite child care and this could allow you to take your breaks with your baby.
Some babies develop a pattern known as “reverse cycle breastfeeding.” (Gale Pryor / Nursing Mother, Working Mother). This means that your baby will sleep more while you away and breastfeed more when you are together. If this happens, you may find you need to pump less when you are away from your baby. Keep your baby near you at night, so that you may nurse easily and get as much sleep as possible.
How Do I Choose a Breast Pump?They type of breast pump you need depends very much on your situation. Your ability to pump well will depend on matching your specific needs to the best pumping system that meets those needs.
If you do need to leave your baby because you are returning to work or school, a good pump will be needed. There are many options to choose from. It is important to choose one that will meet your specific needs. Some things to consider are cost, efficiency, how easy it is to transport and how much noise it makes.
If you only need to pump occasionally, a hand operated pump may be the right one. They are small, easy to carry and use and are not very expensive (for example they may cost $20-50 in the US). One pump that is no longer recommended is the “bicycle horn” style manual pump. This pump did not work well and many mothers found it to be uncomfortable to use.
If you will only be away a few hours a day and only need to pump once or twice, a small electric pump may be appropriate. The cost of these range from about $50 to $150 in the US. Some are double pumping styles, others will pump one breast at a time. Some of them are fairly quiet, but some are rather noisy. These can be plugged into the wall or use batteries. Some have AC adapters.
These can be plugged into the wall or use batteries. Some have AC adapters.
If you will be away for 8 or more hours, a double electric pump is likely the best choice. These are recommended if the time you have to pump is limited and/or you will be pumping 3 or more times per day. These pumps are automatic and they have a suck release cycle that mimics the pattern of a baby nursing. They can be fairly large, and come in carrying cases that resemble a large handbag. These cases hold all of the accessories needed. They are usually quiet. They cost between $200 – 300 in the US and are classified as single user pumps by the manufacturers.
The last option is the hospital grade pump, also called the multi user pump (USFDA). This is a very strong pump and is used when mother and baby are separated, such as pumping milk for a premature baby in the hospital, or if mother needs strong stimulation to increase her milk supply. These are rarely purchased. Most mothers rent them from a hospital or from a Durable Medical Equipment Company.
Many mothers find it helpful to talk with their friends about whether or not a pump is needed, and if so, what kind worked best. Be sure to ask what features worked well and what didn’t.
My friend no longer needs her pump and said I can use it. Is this okay?It is important to know that most breast pumps are considered single user. Milk can flow backwards into the pump mechanism and cause contamination. For this reason, sharing or borrowing single user pumps is not recommended.
Pumping TipsPumping while away from your baby can be tricky. Finding the time and space to do it, as well as relaxing while you do it can be easier said than done.
Mothers who have successfully pumped are a great resource and can provide many suggestions to make the process easier. Here are some of those suggestions:
* Find a quiet place where you are not likely to be interrupted. You may want to look around your work area before you go out on leave to find the best place. It does not have to be fancy, but it should be private. The restroom is not an acceptable place to be asked to pump. Be aware that there are laws in place in some countries to protect you.
It does not have to be fancy, but it should be private. The restroom is not an acceptable place to be asked to pump. Be aware that there are laws in place in some countries to protect you.
*Relaxing is important. Many mothers look at pictures of their babies, listen to music, drink water or have a snack. Some use their phones to watch videos of their babies or face time the baby and caregiver.
*Some mothers find that hand expressing for 1-2 minutes before using the pump gives them better results. The warmth of their hands and “Skin on skin” first provides good stimulation so that their milk is released better.
* Stay hydrated. Drink plenty of fluids so that you do not become overly thirsty. If you can snack as well as get a good meal break, this is helpful as well.
*Invest in a hands free pumping bra. There are several on the market or you can make your own. If you make your own, simply use a sports bra and cut holes where the flanges will go through. You can use duct tape to seal the edges so they don’t fray.
*Invest in a good pump. It will be cheaper than formula in the long run and it will be more comfortable for you. Most manufacturer’s have various sizes of flanges. Be sure your flange is not too tight, nor too loose.
The law
UK
ACAS have produced a comprehensive guide for employers on Accommodating Breastfeeding in the Workplace.
http://www.acas.org.uk/media/pdf/2/i/Acas-guide-on-accommodating-breastfeeding-in-the-workplace.pdf
LLLGB also have useful information on pumping at work:
https://www.laleche.org.uk/working-and-breastfeeding/
USA
There are federal laws in place in the United States to protect you when pumping:
https://www.dol.gov/whd/regs/compliance/whdfs73.htm
Fact Sheet #73: Break Time for Nursing Mothers under the FLSA
This fact sheet provides general information on the break time requirement for nursing mothers in the Patient Protection and Affordable Care Act (“PPACA”), which took effect when the PPACA was signed into law on March 23, 2010 (P. L. 111-148).
L. 111-148).
Cleaning and Sanitizing Pumping Accessories
Hand Expressing
Feeding Breastmilk From a Bottle
Feeding with expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast. There is not enough scientific data on this yet, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding.
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after delivery. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How can I feed my baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs.
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2.3 Calma was developed with the help of breastfeeding experts from the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preserving natural sucking habits allows baby to transition easily from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible.
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature.
Dip the nipple in milk
Try dipping the nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
You can even try to shift it from one hand to another during feeding.
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much pumped milk should I give my baby?
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
How can I keep my baby safe when bottle feeding?
Always clean and sterilize your pump and bottles according to the manufacturer's instructions.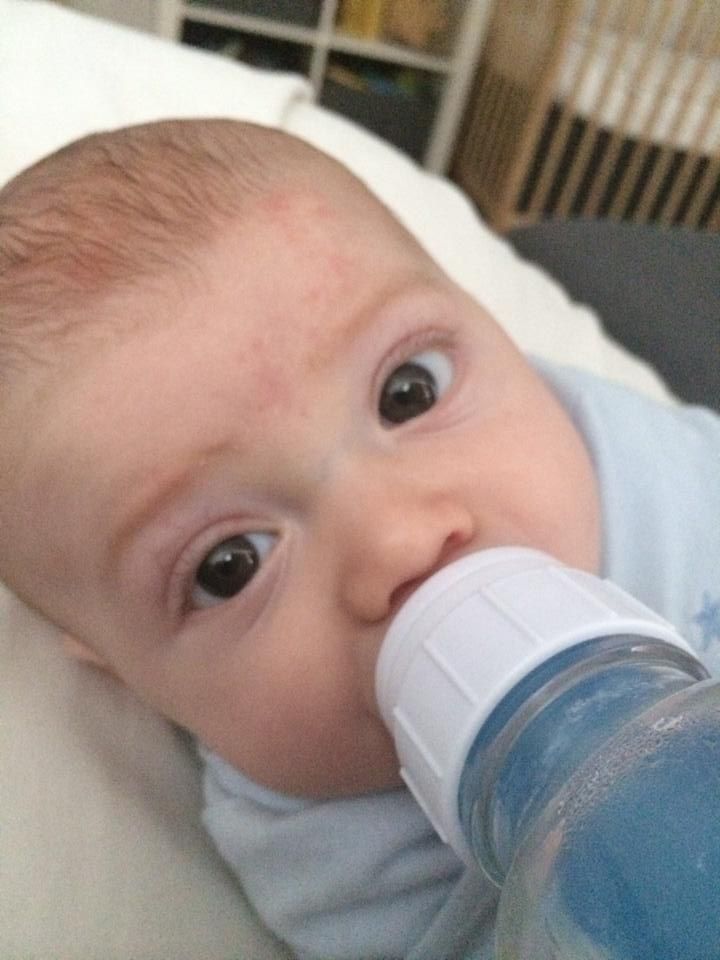 Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, the baby will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it. In general, in these cases, they say that the child confuses the nipple with the breast.
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist.
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." Zh Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Hum Dev . 2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
Airlie Hume Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J. Perinatol. 2013;33(4):319-323. - Segami I. et al., "Perioral movements and sucking during bottle feeding with a new experimental nipple are very similar to sucking from the breast." Zh Perinatol (Journal of Perinatology). 2013;33(4):319-323.
4 Sakalidis VS et al. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. Int J Pediatr. 2012;2012:130769. - Sakalidis V.S. et al., "Oxygenation and Coordination of Sucking, Swallowing, and Breathing in the Term Infant During Breastfeeding and Feeding from a Purely Vacuum Teat". Int J Pediatrician 2012;2012:130769.
Read instructions before use.
 Consult a specialist about possible contraindications.
Consult a specialist about possible contraindications. * RC № ФСЗ 2010/07353 of 07/19/2010
Storage, freezing and thawing of breast milk
Expressed breast milk is the best food for your baby when you are not around. How to store and use breast milk correctly?
Share this information
If you go to work, go to the gym or simply ask your partner to feed your baby and you want to get some sleep yourself, you can express breast milk so that the baby can eat even when you are not around. Most of the beneficial properties are retained in expressed breast milk, so if you are forced to skip breastfeeding, it will be a better replacement than any formula. But an important guarantee of the safety of expressed milk for your baby is hygiene. Read the article to learn how to properly store breast milk.
What is the best way to store breast milk?
Any type of breast milk is better for the baby than formula. But freshly expressed breast milk is better than chilled, and chilled breast milk is better than frozen. The fact is that freshly expressed milk fights bacteria better, it contains more antioxidants, vitamins and fats than chilled or frozen milk 4 .
But freshly expressed breast milk is better than chilled, and chilled breast milk is better than frozen. The fact is that freshly expressed milk fights bacteria better, it contains more antioxidants, vitamins and fats than chilled or frozen milk 4 .
How long expressed breast milk lasts
Once your breast milk is properly collected in a clean container, you can store it at room temperature, in the refrigerator or in the freezer, depending on how soon you plan to use it. Follow the guidelines below:
Recommendations for storing expressed breast milk (for feeding healthy term babies) 2, 3
| Storage location | Room temperature | Refrigerator | Freezer | Pre-frozen |
| Safe shelf life | Up to four hours Up to six hours for milk expressed under extra clean conditions* | Up to three days Up to five days for milk expressed under extra clean conditions* | Up to six months Up to nine months for milk expressed under extra clean conditions* | Up to two hours at room temperature Up to 24 hours refrigerated Do not freeze again! |
* "Very clean environment" refers to strict adherence to the instructions in the article on cleaning and sterilizing the Medela 9 breast pump0104 .![]() These instructions for storing and thawing breast milk are guidelines only. For more information, contact a lactation consultant or healthcare professional.
These instructions for storing and thawing breast milk are guidelines only. For more information, contact a lactation consultant or healthcare professional.
If the baby is in the neonatal intensive care unit (NIU) or intensive care unit, stricter cleaning and storage guidelines may apply in accordance with the hospital's internal policies.
Before placing expressed milk in the refrigerator or freezer, be sure to mark the bottles or bags with the amount of milk and the date of expression. This will make it easier to manage your pumped milk supply.
Recommendations for feeding expressed breast milk
During storage, breast milk usually separates into layers and the fats (cream) it contains rise to the top. Shake the bottle lightly to mix the layers before giving it to your baby. Strong mixing and shaking can destroy some of the nutritional and protective components of breast milk 5 .
When a baby is fed expressed breast milk from a cup or bottle, bacteria from the mouth naturally enters the milk.![]() Therefore, it is best to throw out all the unfinished milk one to two hours after the first feeding. In order to waste as little expressed milk as possible, it is best to store it in small portions and use just enough for one feeding 2 .
Therefore, it is best to throw out all the unfinished milk one to two hours after the first feeding. In order to waste as little expressed milk as possible, it is best to store it in small portions and use just enough for one feeding 2 .
How to Store Breast Milk in the Refrigerator
2, 3Follow the guidelines below to safely store expressed milk in the refrigerator.
- Refrigerate breast milk as soon as possible after pumping.
- Store milk in clean BPA-free breast milk bottles or breast milk storage bags. Its long-term effects on the human body are not well understood and manufacturers are now moving away from the use of this chemical in plastic containers and covers.
- After pre-cooling, a small amount of expressed milk can be added to the milk container stored in the refrigerator. Do not add warm breast milk to already chilled milk.
- Store breast milk in the coldest part of the refrigerator, on the back of the shelf above the vegetable drawer.
 Do not store milk in the refrigerator door where the temperature is not as constant.
Do not store milk in the refrigerator door where the temperature is not as constant.
How to store breast milk in the freezer
2, 3The following are guidelines for the safe freezing of breast milk.
- Freeze breast milk as soon as possible after pumping.
- After pre-cooling, expressed milk can be added to the already frozen milk container. Do not add warm breast milk to already frozen milk.
- To simplify defrosting and reduce waste, store milk in small portions (less than 60 ml). Once thawed, portions can be mixed.
- Make sure the breast milk container is suitable for freezing: some containers (eg glass bottles) may burst at low temperatures. Medela Breast Milk Storage Bags are ideal for storing frozen breast milk: they are ready to use, cold-resistant and easy to label.
- Do not fill bottles or bags more than 3/4 full as milk expands when frozen.
- Store frozen breast milk in the back of the freezer where the temperature is constant.
 Do not place it against the walls of freezers with automatic defrosting.
Do not place it against the walls of freezers with automatic defrosting.
Feeding frozen breast milk
2, 3Follow these guidelines when thawing breast milk to keep it safe for your baby.
- Breast milk can be thawed in the refrigerator, usually takes about 12 hours. You can place the bottle or bag of frozen milk under running warm water (max. 37 °C). Do not thaw breast milk at room temperature.
- Fully thawed breast milk can be stored for up to two hours at room temperature and up to 24 hours in the refrigerator.
- Do not thaw or reheat frozen breast milk in a microwave oven or in boiling water. This can negatively affect the nutritional and protective properties of breast milk, and due to uneven heating, the baby can burn.
- If, after defrosting, you left breast milk at room temperature, but did not feed it to the baby within two hours, the milk must be discarded.
- Do not refreeze breast milk.
How to warm up expressed breast milk
2, 3 Healthy full-term babies can be given breast milk at room temperature or heated to body temperature. Some children care about the temperature of the milk, while others drink milk at any temperature.
Some children care about the temperature of the milk, while others drink milk at any temperature.
- To warm breast milk, place the bottle or bag in a cup, mug or bowl of warm water for a few minutes until the milk is at body temperature (37°C). You can use a bottle warmer. Do not heat milk above 40°C or microwave it to avoid overheating.
- Slightly shake the milk in the bottle or bag to mix the separated fat (see above). Do not stir or shake the milk too hard.
Why does milk smell strange after storage?
Chilled or thawed breast milk may smell different from fresh
. This is due to the action of lipase, an enzyme that breaks down fats into fatty acids, preventing the growth of dangerous bacteria.
Some mothers report that their milk smells rancid or soapy after storage. But if you followed all the recommendations for safe storage given in this article, such milk is absolutely safe 2 .
Storing breastmilk on the road
If you need to transport your breastmilk from work to home or nursery, use the cool bag with ice packs 2 . For more information on pumping and storing breastmilk on the go, see the article on pumping on the go.
For more information on pumping and storing breastmilk on the go, see the article on pumping on the go.
Literature
1 US Food & Drug Administration. Using a breast pump. [Internet]. Silver Spring, MD, USA: US Department of Health and Human Services; 2018 [updated 2018 Feb 04; cited 2018 Apr 12] Available from: www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/BreastPumps/ucm061944.htm. "Instructions for using the breast pump". [Internet] Silver Spring, Maryland, USA: Department of Health and Human Services; 2018 [updated February 4, 2018; cited April 12, 2018] Article referenced: www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/BreastPumps/ucm061944.htm
3 Eglash,A., Simon,L., & The Academy of Breastfeeding Medicine. ABM clinical protocol #8: human milk storage information for home use for full-term infants, revised 2017. Breastfeed Med 12, (2017). - Eglash A, Simon L and Academy of Breastfeeding Medicine, AVM Clinical Protocol #8: Home Storage of Milk for Term Infants 2017 Revision. Brestfeed Med (Breastfeeding Medicine) 12 (2917).
Breastfeed Med 12, (2017). - Eglash A, Simon L and Academy of Breastfeeding Medicine, AVM Clinical Protocol #8: Home Storage of Milk for Term Infants 2017 Revision. Brestfeed Med (Breastfeeding Medicine) 12 (2917).
4 Human Milk Banking Association of North America. 2011 Best practice for expressing, storing and handling human milk in hospitals, homes, and child care settings. (HMBANA, Fort Worth, 2011).- North American Breast Milk Banks Association. Fort Worth: SABGM; 2011.
5 García-Lara NR et al. Effect of freezing time on macronutrients and energy content of breastmilk. Breastfeeding Medicine. 2012;7(4):295-301. - Garcia-Lara N.R. et al., "Effect of Freezing Duration on Macronutrients and Energy in Breast Milk". Brestfeeding Honey (Breastfeeding Medicine) . 2012;7(4):295-301.
6 Office on Women’s Health.