Supplementary feeding baby
Supplementary feeding your breastfed baby: 5 steps to success
Whether you’re returning to out-of-home work, experiencing an illness, or your baby isn’t always able to feed directly from the breast, there may be times when you want or need to introduce bottle-feeding to your breastfed baby.
What exactly is supplementary feeding?Supplementary feeding, or complementary feeding, just means giving your baby formula or additional breast milk on top of breastfeeding. This may be recommended because of breastmilk supply issues, or attachment issues. Supplementary feeding is usually done by offering baby a bottle but other methods can include using a cup or breastfeeding supplementing tube.
Will supplementing throw my hard work out the window?Understandably, many mums can have a range of feelings and fears around introducing bottles to their breastfed baby. Perhaps you’ve spent a lot of time and energy getting breastfeeding off to a good start, or maybe you’re still in the process of figuring out how to make breastfeeding work successfully for you. Either way, you don’t want anything get in the way of good breastfeeding.
Babies use a completely different sucking action when they’re feeding from a bottle compared to feeding from the breast. If you’re having concerns, it helps to know how the mechanics work so you can encourage your baby to happily become accustomed to feeding from both.
Lactation consultant and author, Pinky McKay, explains, “A baby has a suck, swallow, breathe reflex. With a newborn baby, they can’t control a bottle if you’re lying them flat on their back … as soon as their mouth fills with milk, they swallow – and they gulp down a whole bottle of milk and the poor mother thinks they don’t have a good milk supply! Also, because the baby has drunk so much, it’s going to sleep for a long time, and again that sews doubt in the mother’s mind.”
Hot tip: Offer the breast after the bottlePinky says that timing can play a part in successfully combining bottle feeding with breastfeeding, “Unless you need to bottle feed for medical reasons, or you are going to be separated from your baby, it’s better to avoid bottles and dummies in the first weeks – until your baby’s mastered breastfeeding. ”
”
But for those times when you’re with your baby and adding a bottle feed, Pinky has one hot tip for keeping the breastfeeding rhythm in place, “Offer the breast afterwards if possible. If you’re supplementing because your baby’s needing some extra feeds … put the baby back on the breast afterwards.”
Have equipment on hand
Breastfeeding requires very few bells and whistles, but before you embark on any kind of bottle-feeding journey, whether with expressed breastmilk or formula, you’ll need to have the necessary equipment ready to go. The Tommee Tippee Essentials Starter Kit comes complete with six bottles and a steriliser so you’ll have everything you need. If you’re also expressing, you may want to use an an electric pump, like the Philips Avent Comfort Electric Breast Pump, that has an electronic memory of your personal pumping rhythm. Technology!
5 steps for successful supplementary feeding- Hold your baby upright and support her head and neck so your baby will be in control of the milk flow.

- Gently stroke your baby’s lip from top to bottom with the nipple, to stimulate your baby to open her mouth.
- Hold the bottle horizontal for her to feed, this mimics your baby’s experience at the breast, where she has to suck to trigger the milk to let down.
- Tilt the bottle down every now and again: this gives your baby rests.
- If she stops sucking, or turns her head away, you can take this as a sign that she’s finished.
Tip: Remember to discard any leftover milk after one hour, as bottles can get contaminated after they’ve been used.
Any change to your baby’s feeding routine may be a bit challenging at first, but by following these simple steps, you can make the experience of supplementary feeding smoother for you and your baby.
This is a sponsored post by BIG W, where you can find everything you need for pregnancy, baby and beyond.
Posted on by Bron Bates
Get more babyology straight to your inbox
Join now
Supplemental feedings for the breastfed baby
With good instruction and support, most moms can breastfeed their babies exclusively for the first six months (and continue breastfeeding beyond). Unfortunately, many U.S. newborns are still fed something other than their own mother’s milk during their initial hospital stay. These supplemental, or supplementary, feedings are typically artificial infant formula, but they may be donor human milk or glucose water. Because unnecessary supplementation in the hospital has been associated with less exclusive breastfeeding, as well as a shorter duration of any breastfeeding, the Academy of Breastfeeding Medicine (ABM) has issued guidance on when otherwise healthy babies need supplementation or not.
Unfortunately, many U.S. newborns are still fed something other than their own mother’s milk during their initial hospital stay. These supplemental, or supplementary, feedings are typically artificial infant formula, but they may be donor human milk or glucose water. Because unnecessary supplementation in the hospital has been associated with less exclusive breastfeeding, as well as a shorter duration of any breastfeeding, the Academy of Breastfeeding Medicine (ABM) has issued guidance on when otherwise healthy babies need supplementation or not.
When supplementation may not be necessary
The ABM encourages parents and health care providers to adopt a preventive approach to supplementation with:
- prenatal education
- in-hospital breastfeeding support
- breastfeeding immediately after birth
- skin-to-skin care after birth
- rooming-in
- instruction on milk expression (if necessary, such as when the mother and her infant must be separated)
In some cases, concern about a baby’s weight loss is identified as a reason for supplemental feedings. All babies do lose weight after birth. While this can be scary to new parents, it doesn’t necessarily mean that their baby isn’t feeding well; many factors influence the baby’s birth weight and weight changes, including gestational age, the method of birth (vaginal or cesarean), and the amount of fluid the mother received during labor. As long as the infant is “feeding well, urinating and stooling adequately,” and has weight loss “in the expected range” while “bilirubin levels are not of concern,” the ABM recommends adopting a watch and wait approach.
All babies do lose weight after birth. While this can be scary to new parents, it doesn’t necessarily mean that their baby isn’t feeding well; many factors influence the baby’s birth weight and weight changes, including gestational age, the method of birth (vaginal or cesarean), and the amount of fluid the mother received during labor. As long as the infant is “feeding well, urinating and stooling adequately,” and has weight loss “in the expected range” while “bilirubin levels are not of concern,” the ABM recommends adopting a watch and wait approach.
During this time, parents can focus on:
- recognizing early feeding cues
- keeping the baby safely skin-to-skin with the awake mother
- gently awakening the baby for frequent feedings
- hand expression of drops of colostrum to be fed to the baby
Parents, with the support of health care providers, should also pay attention to the baby’s feeding behavior, including the latch, positioning, and signs of discomfort. They should also look for signs of maternal fatigue, which can interfere with breastfeeding.
They should also look for signs of maternal fatigue, which can interfere with breastfeeding.
When supplementation may be necessary
There are situations in which supplementation may be necessary, even for an infant who is born full-term and seems healthy. The ABM identifies the following reasons for supplemental feeding of the infant during the hospital stay after birth:
- hypoglycemia that has been documented by lab test and is unresponsive to frequent breastfeeding; dextrose gel or intravenous (IV) glucose can be given, and breastfeeding should continue
- inadequate milk intake, as shown by significant dehydration, weight loss outside of normal range (with other factors), delayed or persistent meconium bowel movements (black, tarry stools)
- hyperbilirubinemia, sometimes with ongoing weight loss, few bowel movements, and uric acid crystals with urine; breastfeeding should continue during evaluation
- metabolic conditions of the newborn, requiring special supplements
- delayed maternal milk supply
- insufficient maternal mammary glands (estimated to affect less than 5 percent of women)
- past breast surgery affecting milk production
- medical cause, such as chemotherapy or other medication, or separation of mother and infant
- intolerable and unrelieved pain during breastfeeding
What supplement to give
Most parents find that even if they must, temporarily, give a supplement to their breastfed baby, breastfeeding can continue. The ABM ranks possible supplements in order of preference:
The ABM ranks possible supplements in order of preference:
- Mother’s own milk, gathered by hand expression or pump; use breast massage and/or warm compresses to help with letdown and consider pumping one breast while the baby breastfeeds on the opposite breast to increase milk yield.
- Donor human milk, which is preferable to artificial supplements.
- Protein hydrolysate formula, to avoid exposure to cow’s milk protein while conveying that supplementation is temporary.
- Other artificial formula, such as cow’s milk-based or soy-based formula, as determined appropriate for the baby’s age, amount needed, and potential effect on breastfeeding.
Note that glucose water is not considered an appropriate supplement, since it doesn’t provide nutrition or reduce bilirubin, and it poses a risk of hyponatremia or “water intoxication,” due to an imbalance of water and sodium in the body.
How to give a supplement
No single device has been shown to be better for all babies, and some babies may respond better to one feeding method than another. Mothers who are breastfeeding in addition to supplementing may wish to avoid bottles until 4-6 weeks after birth, since artificial nipples require different sucking patterns and can interfere with a baby’s ability to breastfeed (nipple confusion).
Mothers who are breastfeeding in addition to supplementing may wish to avoid bottles until 4-6 weeks after birth, since artificial nipples require different sucking patterns and can interfere with a baby’s ability to breastfeed (nipple confusion).
In addition to bottles, there are many options parents can use to provide supplemental feedings to their breastfed infants including:
- supplemental feeding devices (Lact-Aid or Supplemental Nursing System)
- cup
- spoon
- dropper
- syringe
When selecting how you will administer your baby’s supplemental feeding, the ABM encourages parents and health care providers to consider the following:
- cost and availability
- ease of use and cleaning (cup-feeding is preferable when hygiene is a concern)
- long-term or short-term use
- stress to the infant
- how much supplement can be fed in 20-30 minutes
- mother’s or caregiver’s preference
- expertise of health care provider
- effect on baby’s breastfeeding skills
- effect on mother’s milk supply (supplemental nursing devices provide breast stimulation, as well as skin-to-skin contact)
In most cases, supplementation is given temporarily to help you and your baby overcome a difficulty and to get back on track with breastfeeding. While your baby is receiving supplements, be sure to take steps to maintain and, if necessary, increase your milk supply.
While your baby is receiving supplements, be sure to take steps to maintain and, if necessary, increase your milk supply.
WHO | Supplementary feeding
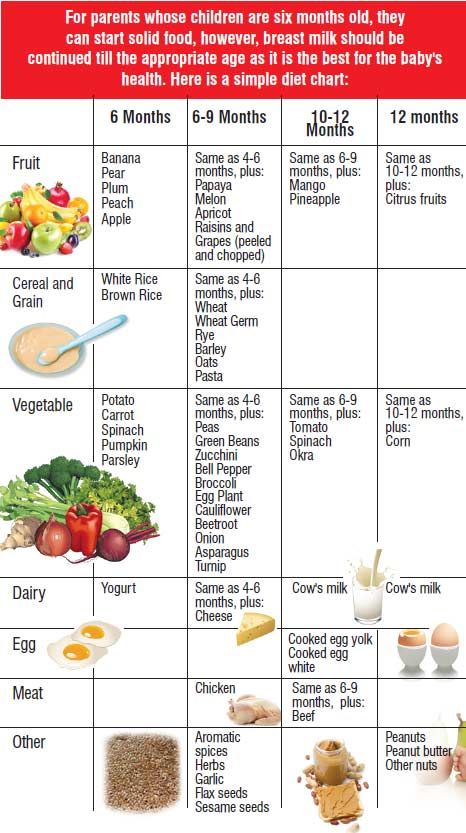
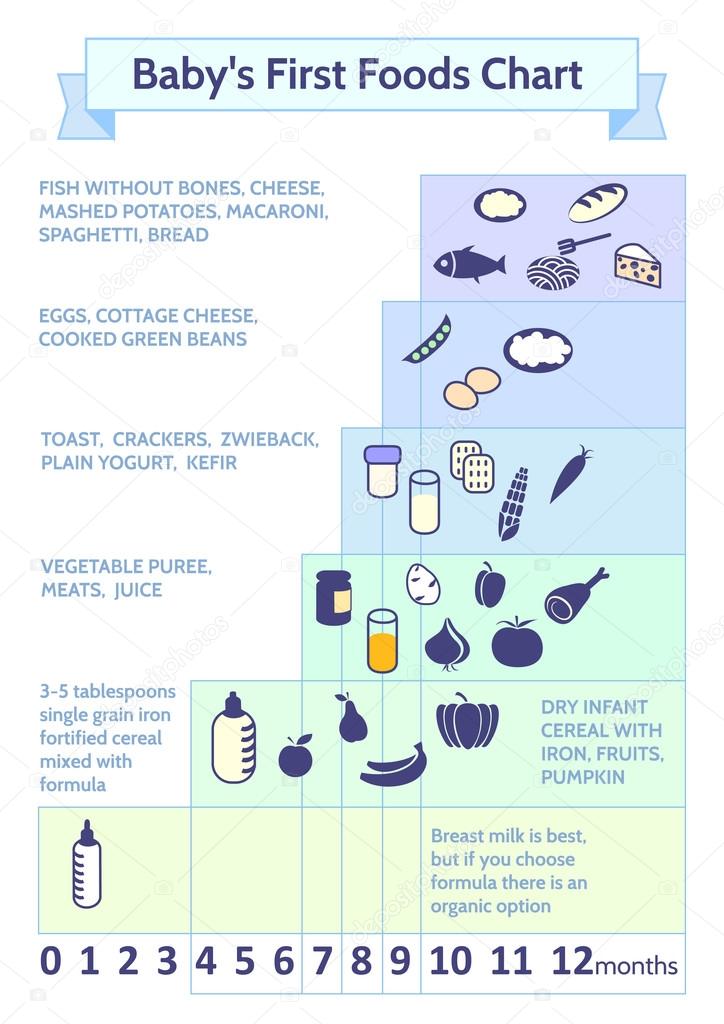
In cases where breast milk is no longer sufficient to meet the nutritional needs of the infant, supplementary food should be included in the child's diet. The transition from exclusive breastfeeding to food consumed in the family, which is called supplementary feeding, usually occurs between 6 and 18-24 months of age, which is a very vulnerable stage. This is when the onset of malnutrition in many infants is a significant factor in the high prevalence of malnutrition among children under five years of age worldwide. WHO estimates that 2 out of 25 children in low-income countries are stunted.
WHO/J. Muriel
Complementary feeding should be timely, which means that all infants should begin to receive nutrition in addition to breast milk from 6 months. It must be adequate, which means that complementary foods should be given in the quantity, frequency, sequence, and variety of foods to meet the nutritional needs of the growing baby while breastfeeding continues. Food should be prepared and served in a safe manner, that is, care should be taken to minimize the risk of pathogen contamination. And they should be fed in an appropriate way, which means that their texture should be appropriate for the age of the child and that flexible feeding is applied, following the principles of psycho-social care.
Food should be prepared and served in a safe manner, that is, care should be taken to minimize the risk of pathogen contamination. And they should be fed in an appropriate way, which means that their texture should be appropriate for the age of the child and that flexible feeding is applied, following the principles of psycho-social care.
The adequacy of complementary foods (adequacy is a shorthand for timely, adequate, safe and appropriate) depends not only on the availability of a variety of foods in the family, but also on the feeding methods used by caregivers. Feeding young children requires active care and stimulation, where the caregiver responds to the child's signals of hunger and encourages the child to eat. Such feeding is also referred to as active or flexible feeding.
WHO recommends that infants be given complementary foods from 6 months in addition to breast milk, initially 2-3 times a day at 6-8 months of age, increasing to 3-4 times a day at 9-11 months, and at 12-24 months additionally include 1-2 times a day additional nutritious food, if desired.![]()
Inappropriate feeding practices are often a more important determinant of inadequate food intake than family food availability. WHO has developed a protocol for tailoring feeding recommendations to allow program managers to find out local feeding practices, common feeding problems and suitable complementary foods. The protocol builds on existing information and suggests that improved feeding recommendations be tested in families. WHO recommends using this protocol to develop interventions to improve complementary nutrition and include it in the process of adapting the Integrated Management of Childhood Illness strategy.
Research has shown that caregivers need skilled support to feed their infants properly. Guidelines on appropriate feeding are included in the Early Childhood Feeding Advisory, Guidelines and First-Level Health Workers Training Course on Integrated Management of Childhood Illness. WHO has produced a guide, Supplementary Feeding: Family Table Food for Breastfed Children, which provides more detailed guidance for health care workers on how to support supplementary feeding.
The WHO Global Consultation on Supplementary Feeding, 10-13 December 2001, resulted in updated recommendations on good feeding practices and guidance for program managers on their implementation. Background material prepared for these consultations is published in the Special Supplement to Food and Nutrition Bulletin 24(1) 2003 and supplements the WHO/UNICEF publication Supplementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge, 1998, WHO/NUT/98.1. The Pan American Health Organization Guidelines on Complementary Feeding for Breastfed Children (2003) summarize the current scientific evidence on supplementary feeding and are intended to guide policy and programmatic action at the global, national and local levels, and The Guidelines for Feeding Non-Breastfeeding Children 6-24 Months of Age (2005) provide guidance on feeding children who are not breastfed.
Based on new knowledge, WHO, in collaboration with partners, has developed updated indicators for infant and young child feeding, including supplementary feeding.![]() As a result, three publications have been produced: definitions, measurement and country profiles.
As a result, three publications have been produced: definitions, measurement and country profiles.
Publications
- Feeding newborns and young children: publications
Related links
- Promoting adequate feeding for infants and young children
- Exclusive breastfeeding
- Global Strategy for Infant and Young Child Nutrition
- World Health Organization recommendations for infant nutrition
Introduction of supplementary food into the child's diet
Submitted by useradmin on Thu, 08/12/2021 - 21:23
Complementary food is solid or semi-solid food given to an infant in addition to breast milk when it is no longer sufficient to meet nutritional needs (or in addition to formula for infants who are breastfed with complementary foods or formula-fed) .
The introduction of solid foods helps the child learn to eat, introduces new tastes and textures of food. Eating solid foods contributes to the formation of teeth and jaws, and also develops skills that will be needed later for the development of speech.
This is the transition from milk to family meals, which babies are usually ready for at the age of one.
The introduction of solid foods not only directly affects growth and development during the first year of life. More and more scientific evidence is emerging about long-term health effects later in life. Healthy nutrition contributes to the growth of the child, determines the development of the brain, enhances the potential for learning, increases productivity in adulthood.
If children do not adopt healthy eating habits in time and do not consume a variety of foods, in the future they may be inclined to eat only certain foods, which can affect their health (lack of vegetables, deficiency of vitamins, trace elements, antioxidants; empty calories, risk of obesity and chronic diseases such as cardiovascular disease, high blood pressure, diabetes).
When is solid food introduced into an infant's diet?
The World Health Organization and UNICEF recommend that a breastfed infant should begin solid foods at about six months of age. Ideally, children should be exclusively breastfed until the age of six months. The introduction of solid foods into the diet of a child less than 17 weeks of age increases the risk of obesity as well as allergies.
Ideally, children should be exclusively breastfed until the age of six months. The introduction of solid foods into the diet of a child less than 17 weeks of age increases the risk of obesity as well as allergies.
Breastfed infants who are supplemented with formula should receive solid food from the 5th month of life (not earlier than the 17th not later than the 24th week). From the 5th month, the functions of the digestive and excretory organs become sufficiently mature, as well as motor functions, which makes it possible to feed the child with semi-solid and solid food.
How do you know if your child is ready for solid foods?
Children grow and mature at different rates. Signs that a baby is ready for solid foods are usually evident around six months of age.
Monitor if your child begins to:
- remain in a sitting position without support, lean forward and return to an upright position; his shoulder and neck muscles are strong enough to support his head
- to control the movements of the hands in order to be able to purposefully pick up a small object and put it in the mouth
- do not push food out of the mouth with the tongue, but be able to swallow it
- control saliva swallowing
Signs or signals that are NOT indicators of readiness as they could mean something else:
- the child wakes up more often at night or is restless
- easily distracted while breastfeeding
- the child is teething, salivation is observed, he gnaws fists
- he shows interest in what others eat, plays with food (but does not swallow it)
- takes food if an adult puts it in his mouth
You may mistake this behavior for a child's willingness to eat solid foods.