Top 8 food allergies in babies
Common food allergens and kids
Share:
Sharing new foods with your baby is an exciting milestone. Unfortunately, amongst the fun of watching your child experience new tastes remain questions and fears about food allergies. Recommendations of when to introduce certain foods seem to change often, and for many parents, it can be confusing to know what is best for your child at each age.
April Clark, registered dietitian with the Food Allergy Center at Children’s Health℠, offers tips on when and how to introduce the top allergenic foods.
How to decrease the chance of food allergies in kids
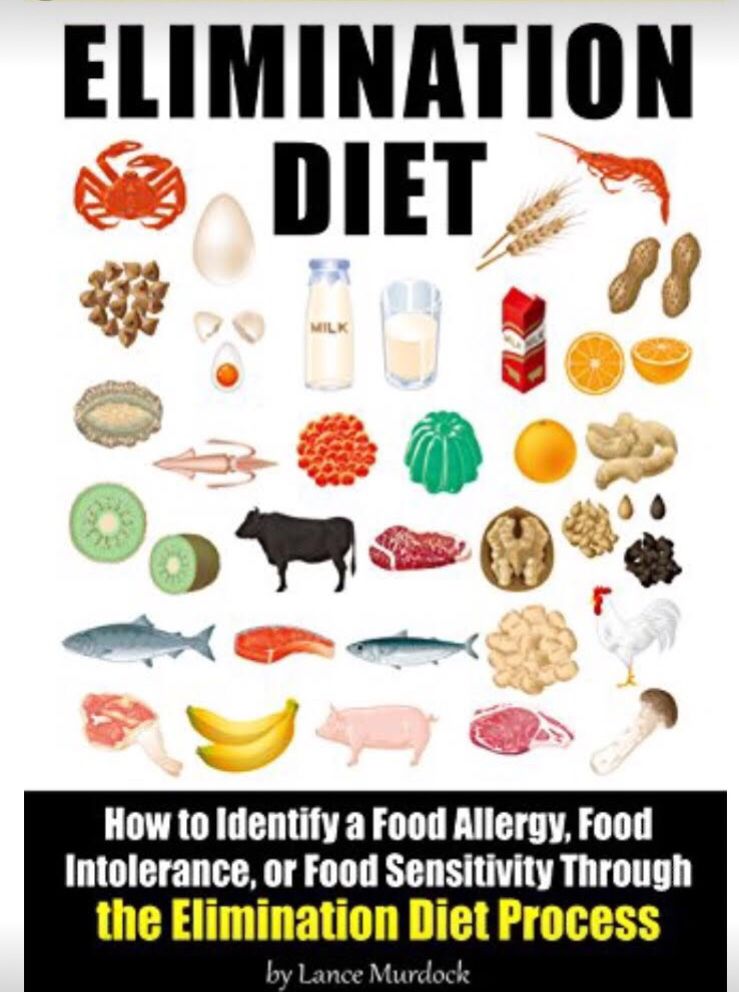
The eight most common food allergens include: cow’s milk, eggs, peanuts, soy, tree nuts, finned fish, shellfish and wheat (gluten). According to the FDA, they account for approximately 90% of all food allergies in the United States.
Previously, the American Academy of Pediatrics (AAP) recommended that the introduction of certain highly allergenic foods be delayed in high-risk children. However, the AAP now recognizes that early introduction of peanuts decreases the chance of developing peanut allergies. Clark recommends following new guidelines to slowly introduce allergenic foods after the addition of solid foods, which often occurs during a baby’s first 4 to 6 months.
Tips on introducing new foods
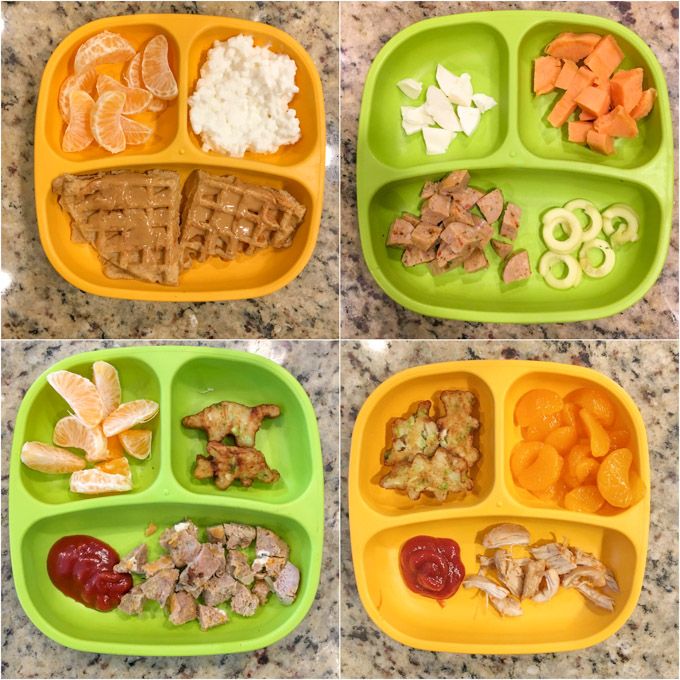
Clark recommends that any of the foods noted below should be introduced one at a time, and parents should carefully observe their child’s reactions. Foods should first be given as single ingredients – not as part of a recipe like eggs in a baked good. They can also be given with complementary fruits and vegetables that have already been proven safe.
If there isn’t an allergic reaction once a food is introduced, continue including it at least three times a week in your child’s meals to ensure the best results. There isn’t a firm deadline to stop serving the foods. Instead, Clark notes that a healthy, well-balanced diet should normally contain variations of these common foods.
- Cow’s milk (dairy) may be one of the first allergies to be noticed, as many formulas are made with milk. Unlike the other foods listed, experts recommend waiting until after age 1 to introduce cow’s (whole) milk into a child’s diet. Instead, Clark notes babies eating solid foods should try yogurt or cheeses.
- Eggs are an excellent source of protein for growing children. Clark recommends either scrambled eggs or pieces of hard-boiled eggs. Depending on the child, they may enjoy the squishy texture and prefer to feed themselves.
- Peanuts or peanut butter are another reliable source of protein. Do not give whole or even peanut pieces, as they can be a choking hazard; instead, peanut butter is a safer alternative, but the thick consistency can be difficult for most children to swallow. Clark recommends melting down the peanut butter with warm water or adding it to a fruit or veggie puree. If a child has severe eczema, and/or already has been diagnosed with egg allergy, they should be evaluated prior to peanut introduction.

- Soy is another allergy that is noticed early due to formulas with a soy base. Protein-packed tofu and edamame (soy beans) can be introduced when your child is ready. They are great options for self-feeding. Like cow’s milk, Clark says parents should not offer soy milk until after age 1.
- Finned fish and shellfish (shrimp, crab, clams, etc.) can be introduced as a puree around the 4 to 6-month mark, or in bite-size pieces once your child is ready. In addition to possible allergies, the AAP warns parents not to serve raw or undercooked items due to possible bacteria or viruses that can make your child seriously ill. Also, the AAP notes children shouldn’t eat more than 12 ounces of fish a week due to concerns about traces of mercury in fish or shellfish.
- Tree nuts (almonds, cashews or walnuts) follow the same guidelines as peanut and peanut butter above.
- Wheat (gluten) can be introduced as finger foods in teething biscuits, puffs and crackers that contain wheat.

Signs of a food allergy
Clark notes children with a first-degree relative (parent or sibling) with allergies are more likely to also have food allergies. Children (and their parents) who have a history of severe or recurring eczema and/or asthma are also at a higher risk to develop food allergies. If your child has any of these factors, you many want to consult your pediatrician for guidance on the best way to proceed.
Allergy symptoms and reactions can vary between children and may appear differently, depending on the age. Reactions can develop minutes after the food is ingested, or there may be a delayed reaction a few hours later. Clark cautions anyone can have a severe reaction at any time, and recommends following guidelines developed by Food Allergy Research & Education (FARE) to identify an allergic reaction. See FARE's list of symptoms here.
What to do if an allergic reaction occurs
Contact your pediatrician if your child has a mild allergic reaction and it is not an emergency. Call 911 immediately for severe and life-threatening reactions.
Call 911 immediately for severe and life-threatening reactions.
If you suspect your child has a food allergy, Clark recommends seeing a board-certified allergist to discuss your concerns. Bring any information about the food, the reaction and your family history to the appointment. The physician will likely take a detailed medical and diet history, and recommend appropriate testing that’s specific to your child’s symptoms and suspected food allergens. Your allergist will be able to manage the diagnosis and answer any questions. Specialists can also provide useful information like recipes and food allergy guidelines.
Download your guide to allergen-free lunches
Looking for tips to pack allergy-friendly school lunches? Download the Parents' Guide to Allergen-Free Lunches for kid-friendly recipes that are free of the top eight food allergens. Download now.
Learn more
Food allergy experts at Children’s Health can help with testing, questions and offer patient resources. Learn more about our program and services.
Learn more about our program and services.
For more information, please see the following additional references:
- Food Allergy Research & Education (FARE)
- Instructions for feeding peanut butter and recipes
- Additional information about introducing peanut butter
- LEAP study in the U.K. (Learning Early About Peanuts)
- Recommendations from the AAP for introducing food
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
Introducing the Top 8 Allergens to Infants — SDBFC
Robin Kaplan
6 mo - 9 mo, Introduction to Solids
Robin Kaplan
6 mo - 9 mo, Introduction to Solids
Written by Rachel Rothman, MS, RD, CLEC
A frequent question I encounter in my practice and in my Introduction to Solids classes, is how to introduce foods that may be allergenic to babies. The last 15 years have brought significant attention to allergens, and most parents are now keenly aware of the risks. However, a drumbeat of new research published on the causes of allergies and allergy prevention has brought new strategies to light and debunked old myths. Until 2008, the American Association of Pediatrics recommended that parents delay exposing infants to certain allergens until after one year of age. The guideline changed because after a review of research and patient outcomes, there was no evidence for waiting. I help many moms and dads make sense of this new world, as they are understandably cautious about what this all means for their child.
The last 15 years have brought significant attention to allergens, and most parents are now keenly aware of the risks. However, a drumbeat of new research published on the causes of allergies and allergy prevention has brought new strategies to light and debunked old myths. Until 2008, the American Association of Pediatrics recommended that parents delay exposing infants to certain allergens until after one year of age. The guideline changed because after a review of research and patient outcomes, there was no evidence for waiting. I help many moms and dads make sense of this new world, as they are understandably cautious about what this all means for their child.
What are the top 8?
The “top eight allergens” are: cow’s milk, eggs, peanuts, tree nuts, fish, shellfish, soy and wheat. These foods are associated with the eight most common food allergies, though it is possible for an allergy to occur with any food.
So when can I introduce these foods?
Most pediatricians will tell you that you can begin to introduce these foods soon after starting solids. I usually recommend starting solids with foods not on the top 8 list, and getting 1-2 months of solids before introducing any of these more common allergens, just to note whether baby has any reactions to other foods. That might mean you begin to offer the 'top 8' foods around 7-9 months of age. And if your child is at a higher risk for food allergies, consult with your pediatrician.
I usually recommend starting solids with foods not on the top 8 list, and getting 1-2 months of solids before introducing any of these more common allergens, just to note whether baby has any reactions to other foods. That might mean you begin to offer the 'top 8' foods around 7-9 months of age. And if your child is at a higher risk for food allergies, consult with your pediatrician.
When offering one of the top 8 allergens, it will be easiest if you only introduce one at a time, and that you observe and note any changes in baby in the first minutes, hours, or days. If all goes well, wait a few days before offering another new food so you’ll be able to isolate any food that may be causing an issue. If you’re concerned that something seems different, consult your pediatrician.
Let’s break down each of the allergens and discuss some ways to introduce:
Cow’s milk: Most of us have heard, no cow’s milk before one year of age. This refers to the fact that cow’s milk should not be a replacement for breast milk or formula before the first year. Why? Cow’s milk has different nutrient properties than breast milk/ formula, primarily a higher proportion of protein and lower amount of fats and carbohydrates, including some differences in vitamins and minerals. Breast milk contains the perfect proportion of all nutrients. Cow’s milk should not be used as a replacement for breastmilk or formula. But, cow’s milk can be used in recipes, like soups, baked goods, or other foods before the first year. Some families choose not to introduce cow’s milk, which is fine too. This is a hot topic, so stay tuned for a post dedicated to the dairy debate!
This refers to the fact that cow’s milk should not be a replacement for breast milk or formula before the first year. Why? Cow’s milk has different nutrient properties than breast milk/ formula, primarily a higher proportion of protein and lower amount of fats and carbohydrates, including some differences in vitamins and minerals. Breast milk contains the perfect proportion of all nutrients. Cow’s milk should not be used as a replacement for breastmilk or formula. But, cow’s milk can be used in recipes, like soups, baked goods, or other foods before the first year. Some families choose not to introduce cow’s milk, which is fine too. This is a hot topic, so stay tuned for a post dedicated to the dairy debate!
Eggs: Eggs are a staple in my house for my daughter, my husband, and myself. It was previously thought to hold off on egg whites before one year of age, but like the recommendations for allergens, most pediatricians say you can introduce whole egg soon after starting solids- just be sure the egg is thoroughly cooked! I love eggs as a finger food- they are so nutritious, and easy for baby to pick up and eat relatively early on. Making an egg and vegetable scramble or frittata is a great way to include vegetables in baby’s breakfast as well.
Making an egg and vegetable scramble or frittata is a great way to include vegetables in baby’s breakfast as well.
Peanuts and Tree nuts: These are among the most highly allergenic foods, so be sure to monitor for reactions when introducing peanuts and tree nuts. Keep in mind that whole nuts are a choking hazard for children until about 4 years of age. When introducing nuts, try spreading a thin amount of nut butter on a piece of bread, mixing a bit of peanut butter into oatmeal or putting a very small amount of nut butter on a spoon (too large of a scoop can be a choking hazard, as well). If your baby loves peanut butter as much as mine did, she’ll be well on her way to learning how to use a spoon!
Fish: Fish is great food for babies because of all of the nutrient benefits- just be sure fish is thoroughly cooked. Fatty fish is an excellent source of omega-3 fatty acids (specifically DHA) which baby needs for brain growth, especially under 2 years of age. You will want to choose a fish type that is lower in mercury (some fish to avoid include King mackerel, marlin, orange roughy, shark, swordfish, tilefish, ahi tuna, and bigeye tuna). The EPA has this great guide which lists the mercury content and sustainability level of many types of seafood. Flaked salmon can be a great finger food (or even mashed with avocado or sweet potato), or try making crab cakes or tilapia cakes.
You will want to choose a fish type that is lower in mercury (some fish to avoid include King mackerel, marlin, orange roughy, shark, swordfish, tilefish, ahi tuna, and bigeye tuna). The EPA has this great guide which lists the mercury content and sustainability level of many types of seafood. Flaked salmon can be a great finger food (or even mashed with avocado or sweet potato), or try making crab cakes or tilapia cakes.
Soy: Some pediatricians do recommend waiting to introduce soy until baby is tolerating other foods. If your baby has already been diagnosed with a soy allergy, you will want to speak with your pediatrician on it’s introduction, and keep in mind many packaged foods contain soy-based ingredients. Baked or sautéed tofu can be a great finger food, or try adding tofu into lasagna in place of ricotta cheese. You may want to wait until baby is about 9 or so months of age before introducing soy.
Wheat: Research and opinions are mixed on the introduction of wheat. Many pediatricians recommend waiting on introducing wheat until other grains have been introduced (like oats, rice, or barley) to see if baby has any reaction to grains. Wheat does contain gluten, and some babies might have a gluten intolerance or sensitivity, but note this will be different than a true wheat allergy.
Many pediatricians recommend waiting on introducing wheat until other grains have been introduced (like oats, rice, or barley) to see if baby has any reaction to grains. Wheat does contain gluten, and some babies might have a gluten intolerance or sensitivity, but note this will be different than a true wheat allergy.
And again, always follow your pediatrician’s recommendations and speak with your pediatrician if food allergies run in your family, as the recommendations may be different. Families of babies that have a history of an allergic condition, including a food allergy, asthma, allergic rhinitis or eczema, should absolutely speak with their pediatrician before offering any of these foods.
Want to learn more about introducing solid food to your little one? Join me at the San Diego Breastfeeding Center for my next introduction to solids class on January 28th at 10:00-11:30am. Learn more here
Rachel Rothman, MS, RD, CLEC is a mom, pediatric dietitian, and instructor at the San Diego Breastfeeding Center. Rachel specializes in working with children and families. She lives in San Diego with her husband, Ben, and daughter, Sydney. You can contact Rachel here.
Rachel specializes in working with children and families. She lives in San Diego with her husband, Ben, and daughter, Sydney. You can contact Rachel here.
References:
Introduction of Solids and Allergic Reactions. (2009, December 7). Retrieved from https://www.aap.org/en-us/about-the-aap/aap-press-room/pages/Introduction-of-Solid-Foods-and-Allergic-Reactions.aspx
Fliescher, D. M. (2013, January 28). Early introduction of allergenic foods may prevent food allergy in children. Retrieved from https://www.aappublications.org/
Greer, F. R., Sicherer, S. H., & Burks, A. W. (2008, January). Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Timing of Introduction of Complementary Foods, and Hydrolyzed Formulas. Retrieved from http://pediatrics.aappublications.org/content/121/1/183
Tagged: Introducing Solids, Introducing Allergens, Rachel Rothman
Food allergy in children - Alexandrovskaya Family Clinic
Children's allergists of the Family Clinic Alexandrovskaya
Food allergy in children.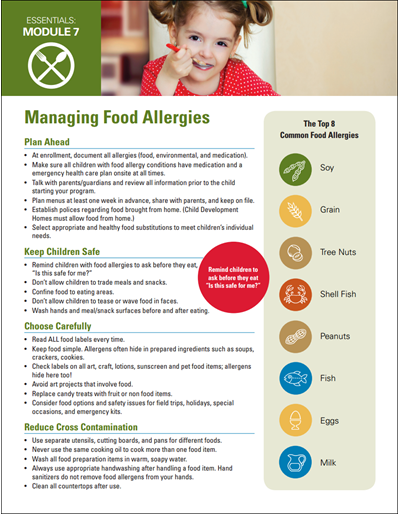 Recommendations of our best children's doctors!
Recommendations of our best children's doctors!
Diagnosis and treatment of allergies, reviews of allergists, our prices...
Currently, more and more often, children with various manifestations of allergic diseases appear at the pediatrician's appointment. Food allergy, that is, a pathological reaction of the child's body to certain foods, is becoming one of the leading factors in the development of allergic diseases and a deterioration in the quality of life of both the child and the whole family. In the truest sense of the word, food allergy is not an independent diagnosis, but in each case of an allergic disease indicates the cause of its occurrence.
How common is food allergy? There is no single answer to this question. According to scientific studies, up to 3% of the world's population have some form of food allergy. Moreover, a direct dependence on age was noted, that is, the younger the child, the more often a perverted reaction to food occurs, so at an early age up to 20% of children have various manifestations of food allergies. In addition, the risk of allergic diseases in children directly depends on the health of the parents. If a mother or father in the family has certain diseases associated with food allergies, then the probability of developing such a disease in a child approaches 50%. If both parents have manifestations of food allergies, then the risk of pathology in a child increases to 70% or more.
In addition, the risk of allergic diseases in children directly depends on the health of the parents. If a mother or father in the family has certain diseases associated with food allergies, then the probability of developing such a disease in a child approaches 50%. If both parents have manifestations of food allergies, then the risk of pathology in a child increases to 70% or more.
How does food allergy manifest in a child?
1. First of all, the development of allergic skin lesions:
- atopic dermatitis of varying severity, from slight dryness of the skin of the cheeks to the development of eczema: common weeping skin surfaces, accompanied by intense itching and sleep disturbance. Among children with atopic dermatitis, the incidence of food allergies reaches 30% - 40%.
- urticaria - an acute allergic reaction in the form of widespread urticaria bright elements, the skin as if burned with nettle leaves.
 The condition of the child is significantly disturbed, there may be an increase in body temperature, severe itching.
The condition of the child is significantly disturbed, there may be an increase in body temperature, severe itching.
- swelling of the soft tissues of the face, hands, feet with the development of Quincke's edema, a formidable complication of which can be swelling of the vocal cords, bronchospasm and a rapid increase in respiratory failure.
2. In addition to skin lesions, the pathology of the digestive tract is often among the clinical manifestations: nausea, vomiting, loose stools, abdominal pain that occurs after eating a product that is an allergen for a child.
Which foods are most often responsible for the development of allergic diseases?
1. In the first place are cow's milk proteins, they most often cause allergic diseases in infants, in the future, most babies develop tolerance, that is, immunity to these allergens, and the child recovers by school age. It is important to know that the allergic properties of cow's milk proteins do not decrease during processing (boiling, pasteurization). This problem is more significant for children who are bottle-fed. A large number of allergens enter the child's body, with still unformed enzyme systems and an immature digestive tract, penetrating into the bloodstream and causing a significant response from the baby's immune system. Yes, and a child who is breastfed is not immune from the appearance of allergic diseases in the event that cow's milk protein enters mother's milk. In addition to cow's milk, the milk of any mammal, including goat, can act as an allergen.
This problem is more significant for children who are bottle-fed. A large number of allergens enter the child's body, with still unformed enzyme systems and an immature digestive tract, penetrating into the bloodstream and causing a significant response from the baby's immune system. Yes, and a child who is breastfed is not immune from the appearance of allergic diseases in the event that cow's milk protein enters mother's milk. In addition to cow's milk, the milk of any mammal, including goat, can act as an allergen.
2. The next significant allergen is the chicken egg, mainly due to proteins, although the yolk allergen can also cause an allergic reaction. A chicken egg contains about 13 different proteins, many of them are destroyed, which means they lose their allergenic properties during intensive heat treatment, this explains the fact that if they are allergic to chicken egg proteins, many people are able to eat small amounts of this product undergone significant heat treatment.
3. Soy - causes serious allergic reactions when eating foods containing it. Therefore, changing the milk formula in a child of the first year of life to a formula based on soy does not reduce the manifestations of atopic dermatitis, but can lead to an aggravation of the situation and a deterioration in the child's condition.
4. Peanuts - is part of many products, being a "hidden" allergen. During heat treatment, the allergenic properties of the product only increase, causing the development of severe reactions.
5. Nuts - almost any kind of nuts cause the development of cross-allergic reactions.
6. Grain proteins - mainly proteins of wheat (gliadin), rye, oats and barley act as an allergen. Manifestations of allergic diseases appear in children older than 6 months, with the introduction of complementary foods. It is worth noting the fact that in most cases, by the age of 4-5, immunity to wheat gliadin develops and the child's condition improves.
7. Fish and seafood - certain fish proteins cause severe allergic manifestations when they are eaten, and they are not destroyed by heat treatment, but turn into vapor and become significant inhalant allergens, leading to serious reactions from the respiratory system. Protein allergens are similar in structure in the main fish species, so cross-allergy is very common. With age, immunity to fish proteins does not develop, so many adults continue to suffer from allergic diseases associated with its use. A very small amount of a fish or seafood allergen is enough to develop severe systemic allergic reactions, up to the development of anaphylaxis.
8. And a number of products, which include chocolate, honey, citrus fruits, coffee, cocoa, which contribute to the occurrence of allergic diseases due to the release of histamine from target cells, which triggers the inflammatory process. Such products also include a variety of canned food, fermented cheeses, sauerkraut, tomatoes.
9. In addition, it is not the product itself that can cause an allergic reaction, but substances added to it by the food industry to preserve its consumer qualities: various dyes, preservatives, nitrites, glutamates (coding E with different numbers on the product packaging).
Diagnosis of food allergy is a rather laborious process, there is no single criterion by which it is possible to speak with a high degree of certainty about the presence or absence of signs of food allergy in a particular person. When making a diagnosis, a pediatrician will rely on the data of the clinical picture, the relationship of exacerbations of the disease with a particular food product, the data of an allergological examination of a child with food allergens. The decisive stage is often the improvement in the condition of the child or his complete recovery after the appointment of a diet that provides for the complete exclusion of foods that act as an allergen in the baby.
Principles of dietary management for children with food allergies:
1. In a child of the first year of life, it is recommended to make every effort to maintain breastfeeding. With an allergy to cow's milk proteins, cow's milk, beef, and veal are excluded from the mother's diet. Given that allergic reactions are rarely caused by only one allergen, it is also recommended to exclude other products that have highly allergenic properties. Allowed: pasta, vegetables and fruits, mostly light in color, vegetable soups, turkey, rabbit, lean pork, buckwheat, corn, rice, oatmeal.
2. With mixed or artificial feeding: the child is transferred to a formula based on highly hydrolyzed protein. If within 2 weeks there is no improvement in the child's condition, then an amino acid mixture is introduced. Such nutrition is prescribed for at least 6 months, or until the child reaches the age of one year. Then, after determining the titer of specific antibodies, they try to introduce a fermented milk product containing cow's milk protein.
3. Introduction of complementary foods: complementary foods in a healthy child are introduced no later than 6 months of age, the same terms are established if the child has manifestations of food allergies. The first food can be vegetable puree or dairy-free porridge. When introducing a new product, it should be remembered that its composition should be one-component, in a small amount, no more than a teaspoon, it is necessary to introduce the product into the diet in the first half of the day in order to track changes in the child's condition. With good tolerance, the amount of the product is gradually increased and adjusted to the required age within 10-14 days.
4. In children older than one year: the composition of the diet is based on the therapeutic diet No. 5, given the fact that very often food allergies are accompanied by pathology of the digestive system. The principles of mechanical, thermal sparing of the gastrointestinal tract are used. They try to use cooking on the vara, boiled or baked. All the same significant allergens described above are excluded from the diet. If, as a result of the diet, it becomes clear that the child's diet is poor and there is a deficiency of essential nutrients, then special mixtures are introduced into the diet containing the entire necessary set of basic ingredients, including minerals and vitamins.
They try to use cooking on the vara, boiled or baked. All the same significant allergens described above are excluded from the diet. If, as a result of the diet, it becomes clear that the child's diet is poor and there is a deficiency of essential nutrients, then special mixtures are introduced into the diet containing the entire necessary set of basic ingredients, including minerals and vitamins.
5. Drug therapy is used quite rarely, and includes the appointment of antihistamines for a short period.
Thus, it becomes clear that the problem of food allergy can be solved by following the principles of the elimination diet. And the more responsible the parents approach the diet of their baby, the more carefully they follow the recommendations of the pediatrician in this matter, the more chances a small child has to grow up to be a strong and healthy person.
Make an appointment with our allergist and we will answer all your questions!
+7(922)750-61-43
+7(922)750-61-44
+7(922)744-10-03
Food allergies in young children!
Food allergies in young children!
Every mother remembers the calm days of pregnancy, where you could eat various foods in your diet without dieting. The main table during pregnancy should be as balanced as possible, fortified and the necessary ratio of proteins, fats, carbohydrates. There comes a happy moment in life, this is the birth of a baby. Acquaintance of mother and child, caring for the baby, providing the necessary conditions for caring for the baby, as well as creating the most favorable conditions.
The main table during pregnancy should be as balanced as possible, fortified and the necessary ratio of proteins, fats, carbohydrates. There comes a happy moment in life, this is the birth of a baby. Acquaintance of mother and child, caring for the baby, providing the necessary conditions for caring for the baby, as well as creating the most favorable conditions.
Very often, young parents face the first difficulties in the neonatal period (such as intestinal colic), in early childhood, such manifestations as rashes on the body, stool disorders (loose stools / constipation).
The most frequently asked questions of parents we will consider in this article:
- How does a food allergy manifest itself?
2. What is the duration of manifestation of external signs?
3. Is it worth giving up breastfeeding in favor of artificial (hydrolyzed and amino acid mixtures) or switching to goat's milk?
4. Blood streaks in the stool: is it worth going to the infectious diseases hospital for inpatient care?
Blood streaks in the stool: is it worth going to the infectious diseases hospital for inpatient care?
Food allergy is a food-induced reaction that causes a pathological reaction based on immune mechanisms (specific IgE-mediated reactions, cellular immune response (non-IgE-mediated) or a combination of both - a mixed type reaction).
As a food allergen, there can be any substances, most often of a protein nature, that stimulate the production of IgE.
The most common foods that cause allergic reactions are cow's milk, chicken eggs, peanuts, tree nuts, fish, seafood, wheat, soy, and beef.
The most significant allergen is Cow's milk protein, which according to clinical guidelines is 2-3% among infants. With age, tolerance develops in 80% of sick children, by the age of 6 years, the incidence decreases by less than 1%.
Any protein component of milk can cause sensitization, but the most common: beta-lactoglobulin, alpha-lactalbumin, bovine serum albumin and gamma globulin, alpha-casein and beta-casein.
Food allergy is a symptom complex of diseases and is not a nosological diagnosis.
Therefore, the clinical and etiological significance of food allergy is taken into account, it is included in the full clinical diagnosis after the designation of the nosological form.
- Atopic dermatitis
- Allergic urticaria
- Allergic gastroenteritis and colitis
Laboratory diagnostics:
- IgE (sIgE) - immunoglobulin E, specific immunoglobulin
The main function of IgE is to provide an individual immune response of the body to the introduction of an irritant (antigen) with a certain biological activity
- Food panel
In case of food allergy in young children, manifestations in the form of constant itching (characteristic of any age period), skin syndrome are more common. Atopic dermatitis in young children is infancy, during this period the exudative form of the disease predominates.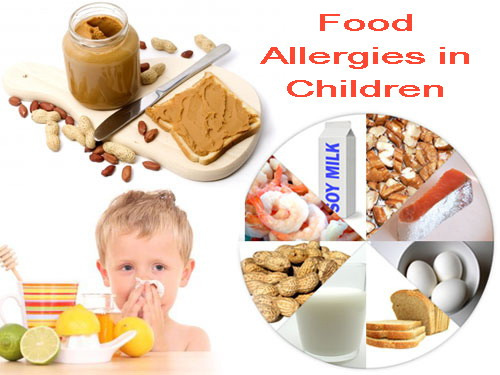 The clinical picture is represented by erythematous spots, papules, vesicles on the forehead, cheeks, scalp, accompanied by intense itching, swelling, weeping. Pronounced red dermographism. Most often, rashes are localized on the extensor and flexor surfaces of the limbs.
The clinical picture is represented by erythematous spots, papules, vesicles on the forehead, cheeks, scalp, accompanied by intense itching, swelling, weeping. Pronounced red dermographism. Most often, rashes are localized on the extensor and flexor surfaces of the limbs.
The duration of rashes depends on the timely start of treatment, as well as the complete exclusion of allergens (food). In children of the first year of life, the most common allergen is cow's milk protein.
Breastfed infants develop a clinically significant allergy to CMP due to the passage of dietary proteins into breast milk. I often see surprise in the eyes of young mothers and the rejection of the recommendation to exclude cow's milk protein. Counter questions: what exactly to use in the diet for mom? Dear mothers, a balanced diet for a nursing mother should be varied, complete and as natural as possible. The use of cereals (rice, buckwheat, corn, oatmeal, etc.), soups, meat products (turkey, chicken, pork), quail or chicken eggs, green fruits, etc. Therefore, the absence of whole cow's milk will not affect your menu variety in any way.
Therefore, the absence of whole cow's milk will not affect your menu variety in any way.
Should I stop breastfeeding?
Indeed, mothers often ask such questions. My answer is no! Breastfeeding is the key to the full development of the child. Only in the case when breastfeeding is impossible (complete hypogalactia of the mother, impossibility of breastfeeding due to congenital diseases (example: congenital malformation of cleft lip and palate), the presence of chronic infectious diseases in the mother are life-threatening for the child.
In the event that it is not possible to store the GW. The recommendations use hydrolyzed mixtures, or amino acids!
Hypoallergenic mixtures do not belong to clinical nutrition, they are prescribed only for children prone to the development of allergies (taking into account history and heredity).
Soy Blend is also not a health food and may cause a cross reaction!
Switching to goat's milk is not the smart way.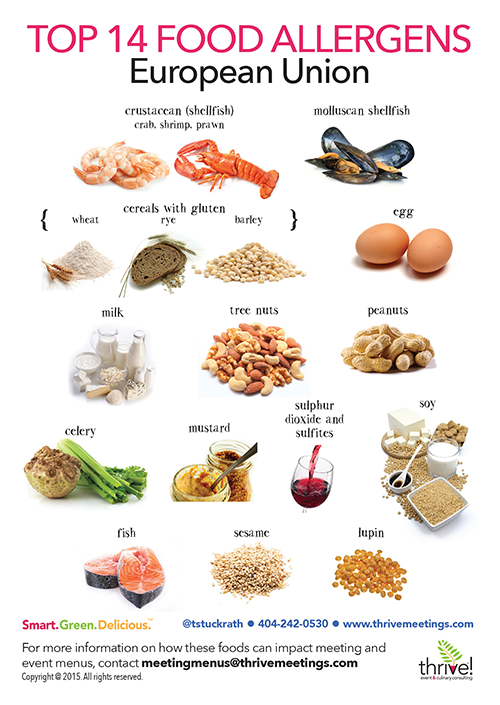 Since in this case, goat milk can act as a cross-allergen, causing cross-allergic reactions in patients with an allergy to CMP, and is an independent allergen, causing severe reactions in patients who are tolerant to cow's milk. And also the main allergens of milk practically do not lose their biological activity after boiling, pasteurization, ultra-high temperature treatment.
Since in this case, goat milk can act as a cross-allergen, causing cross-allergic reactions in patients with an allergy to CMP, and is an independent allergen, causing severe reactions in patients who are tolerant to cow's milk. And also the main allergens of milk practically do not lose their biological activity after boiling, pasteurization, ultra-high temperature treatment.
Blood streaks in the stool: is it worth going to the infectious disease hospital for inpatient care?
Gastrointestinal manifestations are manifestations of the digestive organs. Food allergies are not only when there are rashes on the body. An allergen that passes through the gastrointestinal tract can cause dyspeptic manifestations (regurgitation, intestinal colic, abdominal pain, vomiting, blood streaks in the stool). Such children very often end up in an infectious diseases hospital. Receive symptomatic therapy, which brings only temporary improvement. If not diagnosed in time, unfortunately, this can lead to irreversible consequences.