Training bottle feeding baby
When and how to introduce a bottle to your breastfed baby
Wondering how to introduce a bottle to your breastfed baby? Wait until 3 to 4 weeks postpartum to ensure your milk supply is well established. Have someone else make the first few attempts if possible. If your baby won't take the bottle, try varying the bottle and nipple temperature, moving around, and switching positions. Though some breastfed babies reject bottles vociferously, which can be a real challenge for parents and caregivers, many will come around.
You may be planning to give your breastfed baby bottles because you're pumping breast milk, supplementing with formula, or switching to formula feeding. The transition can be tricky, but there are ways to make it easier. Here's what you need to know to successfully introduce a bottle to your breastfed baby.
When to introduce the bottle to your breastfed baby
If you're breastfeeding, most experts suggest waiting until your baby is 3 to 4 weeks old and breastfeeding is well established before introducing a bottle. In addition to helping launch your milk supply, waiting a few weeks helps reduce the risk of nipple confusion, or a preference for bottles over the breast.
Exactly when to first introduce the bottle varies depending on whether you're bottle feeding because you'll be separated from your baby, or because you need to add formula to your routine.
If you're returning to work after maternity leave, start bottle-feeding several weeks before you go back. That way, you'll have plenty of time for them to adjust to the bottle.
If you're pumping breast milk, you'll want to keep up your milk supply by pumping every time your baby has a bottle. If you can, use a double electric breast pump: It's the most efficient way to express milk and stimulate milk production. (These are usually free through insurance.)
If breastfeeding isn't going according to plan for you and you're thinking about supplementing your baby's diet with formula or switching to exclusively formula feeding, try talking with a lactation consultant before making any big changes. A lactation consultant can assess why you're having trouble breastfeeding and offer tricks to address challenges.
A lactation consultant can assess why you're having trouble breastfeeding and offer tricks to address challenges.
But there's no need to feel guilty if you make the switch to formula: Healthy and happy babies can be formula-fed or breastfed. Focus on nourishing your baby and giving them the love, attention, and cuddles they need to thrive.
How to bottle feed a baby
Sucking milk from a bottle requires different mouth and tongue movements than breastfeeding, so it may take your baby a little time to get used to the change. Try these tips for a smooth transition.
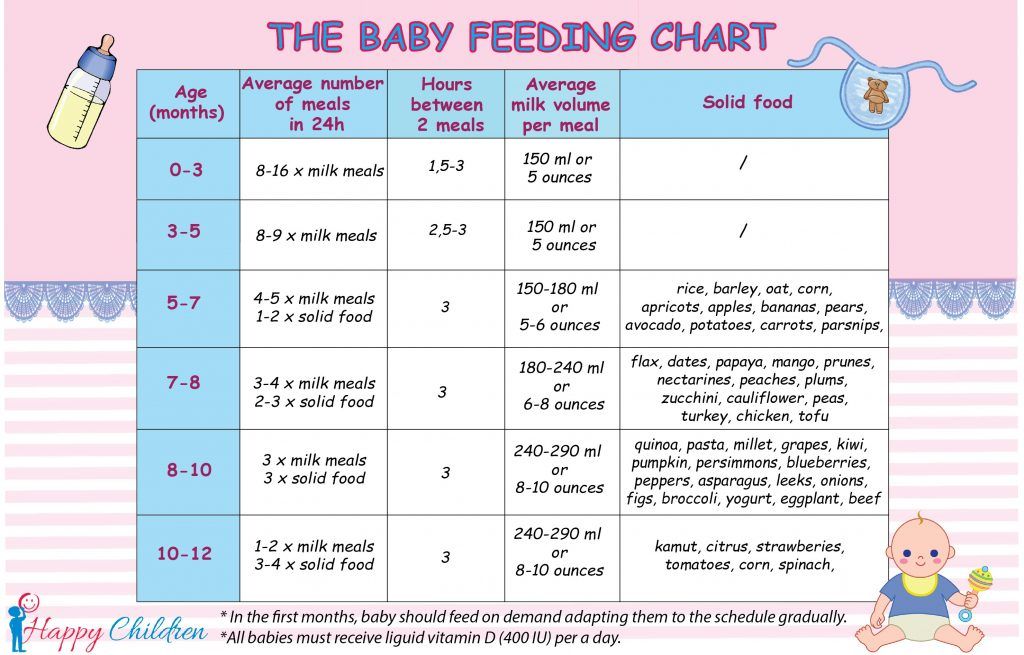
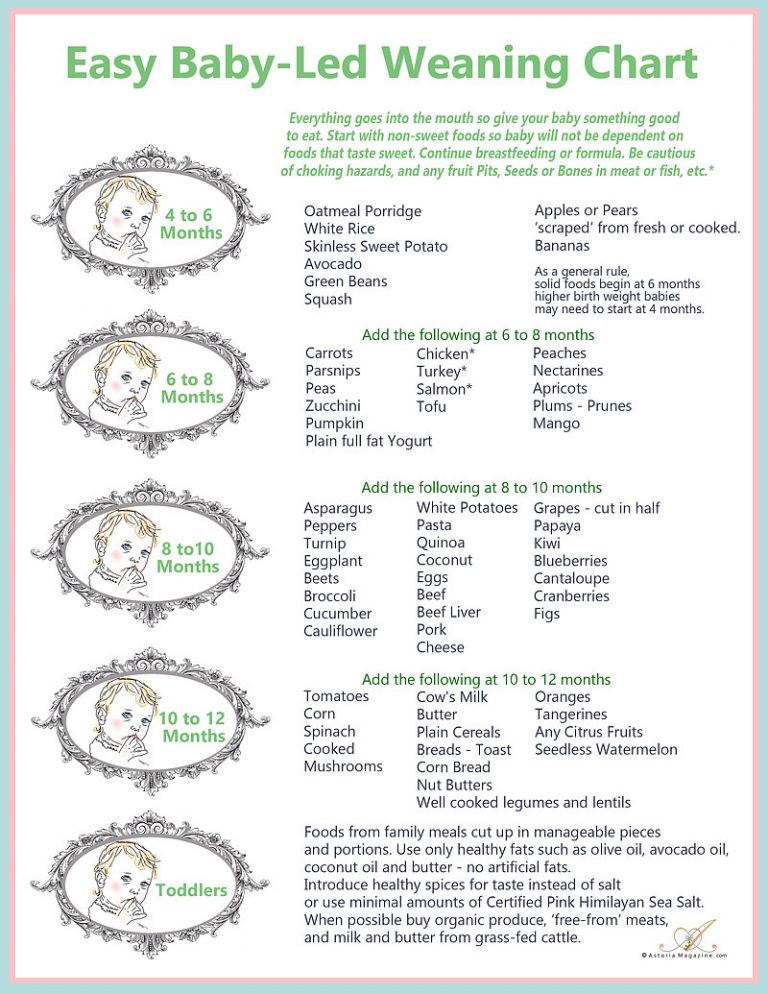
Offer a bottle in place of a regular feeding. Choose a time that your baby tends to not be too fussy at mealtime – say, in the morning. The amount of formula or breast milk you'll need to give at each feeding varies depending on your baby's age and weight. Our articles on how much formula and breast milk babies need break it down for you, and you can always ask your pediatrician for a recommendation if you're not sure.
Advertisement | page continues below
Or, offer the bottle after a regular feeding. If you're especially anxious about offering the bottle, or if your baby balked at the bottle in place of the breast on your first attempt, you may want to get them used to the nipple by offering the bottle an hour or two after they're already fed. That way your baby won't be frenzied for food and may be more open to experimenting with a new food source. Start with a small amount of breast milk – about 1/2 ounce.
Let someone else feed them the first bottle. If you try to give your baby their first bottle, they may wonder why they're not getting your breast. They may be less confused if someone else makes the introduction. Ask your partner, a grandparent, a childcare provider, or a friend to help. Choose a spot other than where you regularly breastfeed.
Make sure the bottle is the right temperature. Breastfed babies can be particular about the warmth of their milk; many prefer milk that's the temperature of your body or a bath (about 98 degrees Fahrenheit). You can soak the bottle in a bowl of hot water or use a bottle warmer to bring it up to temperature.
You can soak the bottle in a bowl of hot water or use a bottle warmer to bring it up to temperature.
Stay away. A baby can smell their mother, even from a distance, so they may know that you (and your breasts) are nearby. If your baby refuses a bottle with you nearby, try going to a different room during feedings.
Don't force it. The first time you introduce the bottle, don't force the nipple into your baby's mouth. Try tickling your baby's upper lip and nose with the nipple and then letting your baby "latch" onto the nipple as they would with your breast. If your baby seems frustrated or hasn't eaten anything after 10 minutes, stop and try again the next day.
Try paced (or responsive, or cue-based) feeding. This method slows down the flow of milk to mimic breastfeeding and reduce the chances that your baby will drink too much. Use a slow-flow nipple, keep the bottle horizontal, pause every 20 to 30 seconds during feedings, and switch sides as you would when breastfeeding.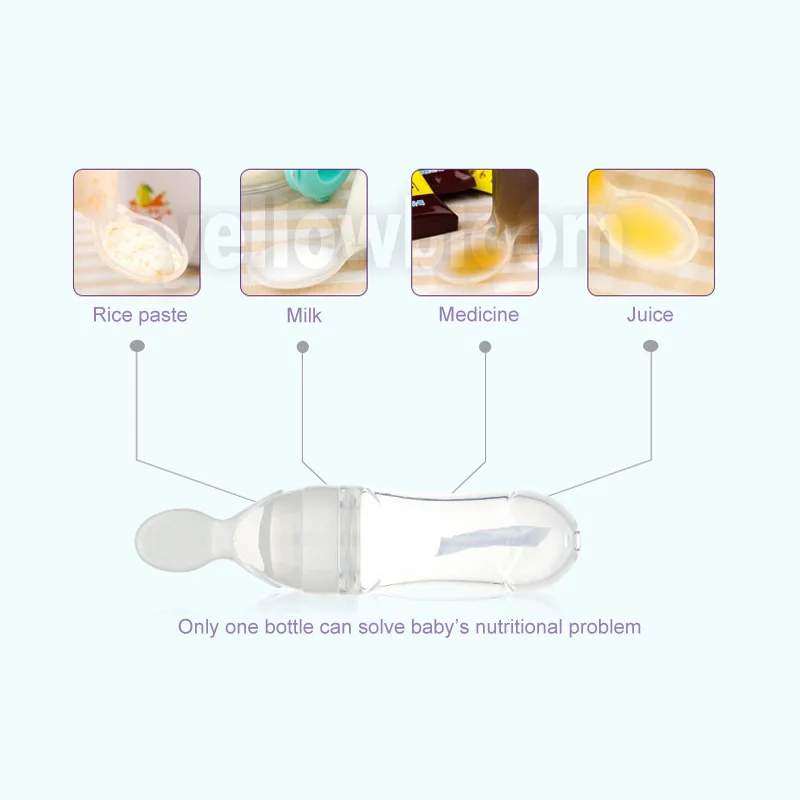 Stop feeding your baby when they show signs of being full, which include not sucking anymore and turning away from the bottle. Research suggests a responsive feeding style encourages healthy eating habits that last well beyond the bottle.
Stop feeding your baby when they show signs of being full, which include not sucking anymore and turning away from the bottle. Research suggests a responsive feeding style encourages healthy eating habits that last well beyond the bottle.
Bond with your baby. Talk to your baby and look into their eyes as you bottle-feed to bond and help them feel secure. You can even take off your shirt for skin-to-skin contact, which helps babies to relax while stimulating digestion and interest in feeding, among other benefits.
Be patient. It may take a while for your baby to accept the bottle.
Be consistent. Babies love routines, so aim to give the bottle the same time every day.
What to do if your baby won't take a bottle
Some babies take to the bottle without much fuss, but others struggle quite a bit with the transition.
Make sure you have lots of time and take it slow during this process. If your baby starts crying and pushes the bottle away, back off, comfort them, and then try again. If you've tried offering the bottle several times and your baby seems frustrated, or if they refuse to eat for 10 minutes, let it go for now. (Wait at least five minutes before breastfeeding after an unsuccessful bottle-feeding – that way they won't associate refusing the bottle with immediate gratification.)
If you've tried offering the bottle several times and your baby seems frustrated, or if they refuse to eat for 10 minutes, let it go for now. (Wait at least five minutes before breastfeeding after an unsuccessful bottle-feeding – that way they won't associate refusing the bottle with immediate gratification.)
Offer the bottle again in an hour or two, when your baby is alert and receptive but not very hungry.
If your baby is having a hard time, try these techniques:
- Test a few different nipples. Babies can be very particular about bottle nipples. If you've tried the bottle a couple of times and your baby still refuses to eat, test out a few other options. Your baby may prefer a wide-based nipple, which more closely simulates the breast. Or your baby may accept a nipple that's similar to the pacifier they use (if you use one), so try giving them a nipple that's the same shape or made out of the same material as the pacifier.
- Change the temperature of the nipple.
 If your baby is teething, they may prefer a nipple that's been chilled in the fridge. Otherwise, try warming the nipple under running water.
If your baby is teething, they may prefer a nipple that's been chilled in the fridge. Otherwise, try warming the nipple under running water. - Introduce breast milk outside of the bottle. Put a few drops of breast milk on your baby's lips or the nipple before feeding them from a bottle, to give them a preview of what's to come. When your baby tastes it, they may start sucking to get more.
- Let your baby play with the nipple so they can get familiar with it. If your baby just chews on it at first, don't worry. They may actually start sucking on it soon.
- Hold them in a different position during the feeding. Put your baby in an infant or car seat so they're semi-upright, and then feed them the bottle while you're facing each other. Or try feeding them on your lap with their back to your chest. Once your baby is used to taking a bottle, you can hold them in a more standard feeding position.
- Move around. Try walking or lightly bouncing your baby. Gentle, rhythmic movement may encourage them to take the bottle.

- Try different temperatures. Your baby might prefer milk that's slightly warmer or colder. Experiment with different temperatures to see what they prefer.
- Check the taste. Expressed breast milk sometimes has a soapy taste, so you may want to try a drop.
- Offer the bottle at other times of day. If your baby won't take the bottle during the day, offer it during a nighttime feeding or vice versa.
If your baby is still refusing the bottle
For most babies, bottle refusal is a short-lived developmental step. That's why it's best to give everyone time to transition by introducing the bottle well before you have to go back to work or otherwise be separated from your baby.
If your baby continues to refuse the bottle, keep trying: It can be frustrating, but your baby may eventually accept it. Until they do, you may have to make serious adjustments to your life. Some working moms have had to extend their maternity leave, change jobs, work from home with a nanny or sitter, or visit their child's daycare every two to three hours to breastfeed their bottle-refusing baby.
If you've tried everything, don't blame yourself if your baby still won't bottle-feed. Some babies never take to the bottle – but talk to your child's doctor to rule out a medical reason.
Some babies can learn to drink from an open cup or a sippy cup instead of a bottle. Make sure your baby can hold their head up on their own before trying (usually around 4 to 6 months), though, to reduce the risk of choking. Here's how to start using a sippy cup:
- Support your baby's head and shoulders with your arm and sit them upright in your lap.
- Place the cup on your baby's lower lip and tilt it until the milk or formula is close to their lips.
- Wait until your baby laps up the milk with their tongue, which may take a few minutes. Don't pour the milk straight into your baby's mouth.
- Continue to offer the milk until your baby turns away their head or offers other cues that they're finished.
- You may want to try this method first with another adult for practice.
 Once you're ready to test it out on your baby, be prepared with a bib and burp cloth nearby to wipe up spills.
Once you're ready to test it out on your baby, be prepared with a bib and burp cloth nearby to wipe up spills.
Eight Tips for How to Introduce Bottle-Feeding
As a nurse in the Institute for Maternal-Fetal Health at Children’s Hospital Los Angeles, I meet many moms who are intimidated when it comes to knowing when and how to introduce bottle-feeding to their babies. It can be especially intimidating because of the many myths associated with starting bottle-feeding. My experience helping moms on this issue is what inspired this post and I hope to help ease the anxiety for those who wonder when and how to introduce bottle-feeding.
There are no mandatory rules about when to add a bottle to a baby’s feeding routine, but here are some expert tips that may make the process easier. (Tweet this)
1. Add a bottle after a healthy milk volume is established from your breast. If you are exclusively breastfeeding and want to keep it that way, then only introduce a bottle after you have established a healthy milk volume and breastfeeding routine. This can take up to four weeks after birth.
This can take up to four weeks after birth.
2. Continue breastfeeding or pumping to maintain milk volume. When your baby is feeding from the bottle, make it a priority to pump (and breastfeed when your baby is not using the bottle). Decreasing the amount of times milk is expressed from your breast can lead to a decrease in the volume produced.
3. Nipple confusion versus nipple preference. Many people believe that babies don’t want to be breastfed after bottle feeding or don’t want to bottle-feed after exclusively breastfeeding because of nipple confusion. This is not true. Babies do not get confused about the different feeding methods. But they do get accustomed to the breast or bottle and establish a nipple preference, which only means that they prefer one method over the other!
4. Use a bottle nipple that is wide-based, which is similar in size and shape to your nipple. I recommend wide-based nipples. Purchase a bottle with a nipple that is more similar to the human breast. These nipples are usually wide-based with shorter nipple heights. The nipple requires that the baby take a larger amount of the nipple into its mouth, similar to breastfeeding.
Purchase a bottle with a nipple that is more similar to the human breast. These nipples are usually wide-based with shorter nipple heights. The nipple requires that the baby take a larger amount of the nipple into its mouth, similar to breastfeeding.
5. Purchase one nipple and bottle style at a time. Some babies are very picky when it comes to bottles, especially if they have been exclusively breastfeed. It is a good idea to buy one set of a certain bottle and nipple style at a time to make sure your baby can feed well before buying a larger supply. Sometimes babies will try out multiple bottles and nipples before they decide on a favorite.
6. Use a slow-flow feeding style. A slow-flow feeding style with a bottle closely resembles that of breastfeeding. Babies that breastfed are used to working for their food and it comes out at a slower rate. Whereas, bottle-feeding is easy and takes little effort. The rate is much quicker and babies can get used to this fast rate, making breastfeeding more frustrating when returning from bottle-feeding. If you are using a regular nipple allow the baby to take five to ten sucks and remove the bottle. Allow your baby to swallow and breathe. Then reinsert the bottle and start again. This process should encourage your baby to slow down their feeding. The feeding should take roughly 15 minutes, similar to that of a breastfeeding session.
If you are using a regular nipple allow the baby to take five to ten sucks and remove the bottle. Allow your baby to swallow and breathe. Then reinsert the bottle and start again. This process should encourage your baby to slow down their feeding. The feeding should take roughly 15 minutes, similar to that of a breastfeeding session.
7. It takes time. Many exclusively breastfed babies do not accept a bottle right away, so it may take a couple of attempts before your baby gets the hang of it. Be patient and continue to offer the bottle to your baby.
8. Introduce bottle-feeding two to four weeks before going back to work. By doing this, you can establish a pumping routine, allow your baby time to adjust to the bottle and give you a chance to see that your baby is able to feed from the bottle effectively. The above tips will help you a lot when you begin your journey of bottle-feeding your baby. Most of the time a baby will accept a bottle very well, but there are a few that can really make the transition frustrating. If you are having a difficult time introducing bottles or your baby does not seem to be feeding as well with a bottle, please enlist the help of a breastfeeding expert.
If you are having a difficult time introducing bottles or your baby does not seem to be feeding as well with a bottle, please enlist the help of a breastfeeding expert.
Thank you for taking the time to read my post, I hope you found this information helpful. If you want advice on a specific topics please feel free to write a comment and I can address your needs in future posts.
Bottle feeding
Target : ensure adequate nutrition for the child.
Readings : physiological satisfaction food needs.
Contraindications : no.
Equipment :
- scarf, gauze mask;
- measuring bottle;
– sterile pacifier;
- necessary amount per milk feeding mixture (or other food) temperature 36-37°С; nine0007
- thick needle for piercing the nipples;
– containers with 3% soda solution for boiling nipples and bottles.
Engineering security :
--- do not leave unattended child;
--- warn swallowing air;
--- provide feeding with formula prepared in in accordance with sanitary and hygienic norms.
Possible problems : anxiety, difficulty in feeding food, vomiting. nine0007
| Stages | Justification |
| Preparing for manipulation | |
| 1. Explain to mom purpose and course of the procedure | Security proper daily feeding baby |
| 2. Prepare necessary equipment | Security the clarity of the procedure |
| 3.Wash and dry hands Put on a scarf mask Prepare baby to feed | Security infectious safety |
| 4. | Prevention infectious diseases of the gastrointestinal tract |
| 5. If the nipple new, pierce a hole in it hot thick needle | In the presence of big hole in the nipple increased chance of hitting lots of air in stomach during feeding, with a narrow hole in the nipple - the baby will get tired quickly |
| 6. Put on a pacifier per bottle | Fluid from a horn should flow in occasional drops |
| 7. Check mixture flow rate and temperature, dropping on the back surface of your wrist joint | warm solution does not cause spasm of smooth muscles stomach, well absorbed causes mucosal burns |
| Execution manipulation | |
| 1. | Prevention suction |
| 2. Feed baby, making sure that during feeding bottle neck was constantly and completely filled mixture | A warning swallowing air (aerophagy) |
| Completion manipulation | |
| 1.Hold baby in an upright position 2-5 minutes | air removal, ingested during feeding |
| 2.Put the baby in the crib on its side (or turn your head on the side) | Prevention aspiration with possible regurgitation |
| 3.Remove from the bottle pacifier, rinse the pacifier and horn under running water, then boil in 3% soda solution 15 minutes Drain from the bottle water and store it in a closed container | Security infectious safety |
How to bottle feed your baby
For various reasons, women stop breastfeeding and introduce bottle feeding to their babies. Artificial feeding can be combined with breastfeeding and alternate with it. Numerous studies show that breastfeeding has endless physiological and emotional benefits for both mother and baby, so if breastfeeding is not possible, it is essential to create a bottle feeding environment that is not significantly inferior to breastfeeding. nine0007
Artificial feeding can be combined with breastfeeding and alternate with it. Numerous studies show that breastfeeding has endless physiological and emotional benefits for both mother and baby, so if breastfeeding is not possible, it is essential to create a bottle feeding environment that is not significantly inferior to breastfeeding. nine0007
The following aspects are important in bottle feeding:
- bottle comfort and safety,
- contents of the bottle,
- feeding technique,
- emotional state of mother and child during feeding.
Bottle safety and convenience
The European Union has declared that baby bottles containing a chemical called bisphenol A (BPA) are unsafe. In Europe, bottles containing BPA are banned for feeding. Bisphenol has been used in the manufacture of plastic bottles by various companies, as its properties make the bottles unbreakable. While breastfeeding, small amounts of BPA can pass from the plastic bottle into milk and cause health problems such as heart disease, cancer, diabetes and hormonal changes, which can then affect the reproductive system.![]() nine0007
nine0007
If you choose to use glass bottles for baby feeding because they are chemical free when properly handled, be sure to inspect them carefully before use. There is a risk of glass cracking during the heat sterilization process, which could result in glass fragments entering the milk or formula.
No matter what bottle material you choose, it must be sterilized before every feeding. Sterilization kills potentially harmful bacteria that can collect on the bottle and in the milk. Before feeding the baby, the bottle with all its parts must first be washed in clean hot soapy water and then sterilized. To sterilize baby feeding equipment, you can use a special electric steam sterilizer, a microwave oven, or a sterilizing solution. For the purpose of sterilization, you can also boil bottles and nipples in a sealed container for at least 10 minutes. nine0007
Bottle contents
If you intend to bottle feed your baby with expressed breast milk, all you need to do is keep the bottle clean: sterilize it after every feeding. If feeding is to be carried out with dry mixes, then there are a number of rules that must be followed for the correct preparation of the feed.
If feeding is to be carried out with dry mixes, then there are a number of rules that must be followed for the correct preparation of the feed.
- Boil water and let it cool for no more than half an hour.
- Pour the required amount of water into the bottle (according to the mixing instructions). nine0236
- Add to the bottle the amount of dry powder indicated on the packaging by the manufacturers. The concentration should not be reduced or increased - the instructions are designed in such a way that the contents of the mixture are well absorbed by the child. If the mixture contains an excessive amount of water, the child will not receive the necessary calories and nutrients; in the case of a high concentration of powder, the child may develop diarrhea or dehydration. nine0235 Close the bottle with a cap and shake it well to completely mix and dissolve the powder.
- Check the temperature of the mixture: put a little of the mixture from the bottle on the inside of your wrist.
 The mixture should be warm, not hot. Food can be heated in a water bath, but you should not heat it in a microwave oven, since the contents of the bottle warm up unevenly in the microwave, the mixture can warm up too much in the center and burn the baby’s mouth and esophagus during feeding. nine0236
The mixture should be warm, not hot. Food can be heated in a water bath, but you should not heat it in a microwave oven, since the contents of the bottle warm up unevenly in the microwave, the mixture can warm up too much in the center and burn the baby’s mouth and esophagus during feeding. nine0236
Feeding should take place in sessions: do not leave the bottle with formula until the next feeding, do not supplement the child several times a day from the same bottle. The prepared mixture can be stored for no more than half an hour, because after this time the food loses its homogeneity, it precipitates and bacteria grow, which, in turn, can provoke the development of diseases and disorders of the immune system.
Feeding technique
Bottle feeding is not really difficult. However, there are a few feeding rules you should remember to avoid baby tears, food spills, and other problems.
- The position taken by the feeder should resemble the natural position of the mother when breastfeeding: the baby's head should lie on the left hand.
- The nipple that enters the baby's mouth must always be full of milk or formula, otherwise the baby will swallow air which can cause colic. nine0236
- The appearance of bubbles in the bottle means that the child is eating incorrectly and you need to help him, change his position, tilt the bottle in a different way.
- Don't leave your baby alone with a bottle and don't let your baby sleep with a bottle in their mouth, both of which can lead to choking.
- It is best to feed your baby when he is in your arms - babies feel most secure in parental arms.
- Remember that the baby's head should always be slightly higher than his torso. nine0236
- Make sure that the baby does not tilt the head too far back or forward - if the head is in the wrong position, it becomes more difficult for the baby to eat, the wrong position of the head can also cause food to enter the respiratory tract.
- When a baby eats from a bottle, he swallows air with nutrition, so he may feel full, despite the fact that he ate little.
During feeding, you need to take breaks every 5 minutes so that the child has the opportunity to burp. After he releases air and some nourishment, he will feel hungry again. In order for the child to burp, you need to change his position: put the child's head on your shoulder and support his back with your hands. The child should be in a straight or semi-upright position. If the baby does not burp between feedings, the accumulated air will lead to the formation of painful gases. nine0236
The seated position is the most classic feeding position. With this feeding, the baby sits on your hips with his booty, his back leans against your left hand, and his head is in the crook of the elbow of his left hand.
Side feeding of the bottle is useful if the child suffers from gastroesophageal reflux or has a runny nose. In this option, the child lies on his side (according to the recommendations of doctors, it is better for the child to lie on his left side), and you are nearby and can also take a position lying on your side, turning to face him. nine0007
nine0007
Emotional state of mother and baby during feeding
The baby feels your emotions, so do not feed him when irritated, angry or upset. Before feeding, take a deep breath and try to relax. Take a comfortable position for you in a chair or on a bed, put a towel or wet wipes nearby in case of spilling the mixture; under the arm on which the child will lie for comfort, you can put a pillow.
While feeding, stroke the baby and talk softly to him. It is important to create for the child the same feelings that he experiences during breastfeeding - the warmth and care of the mother. nine0007
The emotional state of the baby before feeding is also important: if the baby is excited, crying or screaming, then he should be calmed down and then feeding should begin. When a baby cries or screams, the airways are not protected and formula or milk can get into the larynx.
Feeding your baby is an important part of caring for him, bring maximum care for your baby to this ordinary event and enjoy every moment spent with your baby.

 Pour into a bottle required amount freshly prepared milk formula (or other food)
Pour into a bottle required amount freshly prepared milk formula (or other food)  Arrange baby in the arms with a raised head end
Arrange baby in the arms with a raised head end