Week old baby vomiting after feeding
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
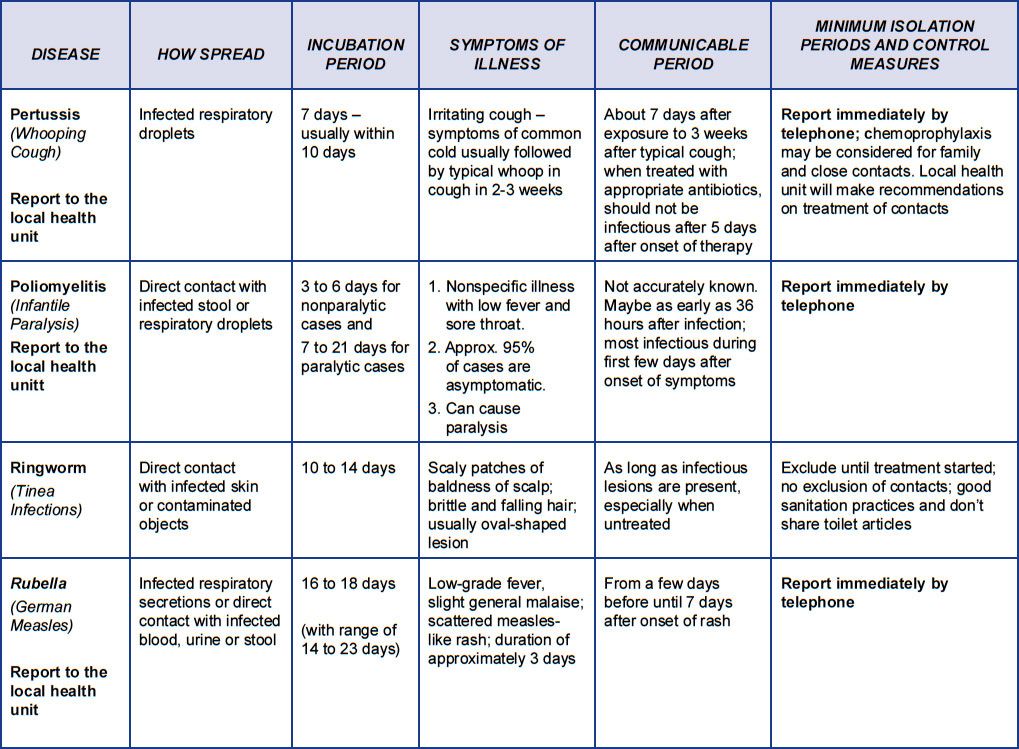
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection.
A serious cause in young babies is pyloric stenosis. See below for more on this.
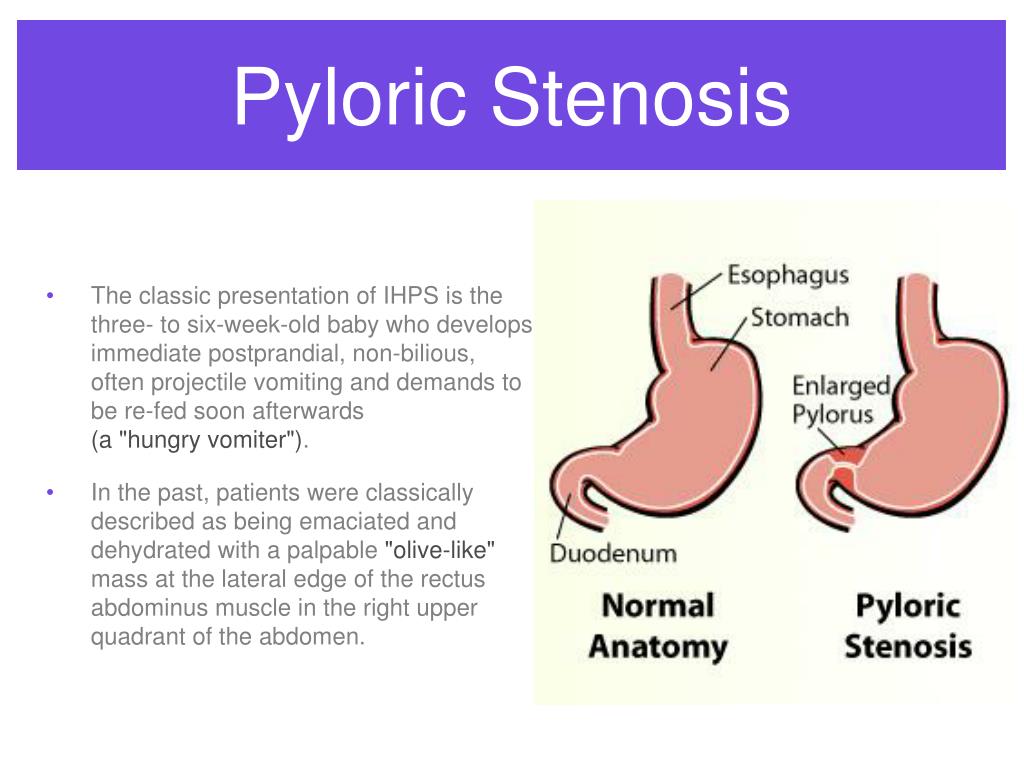
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything.
 This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting. - The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.

- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
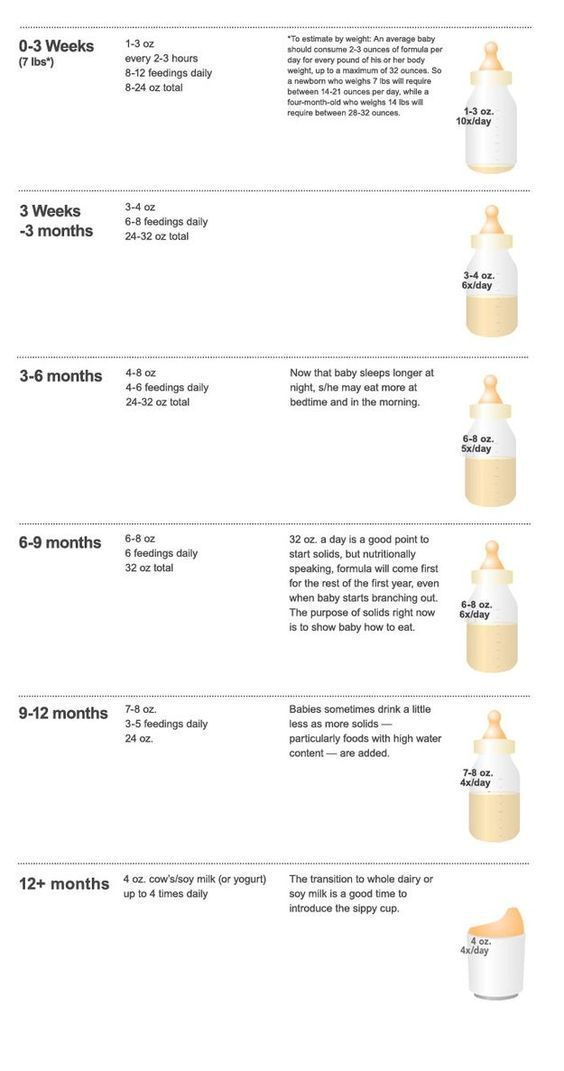
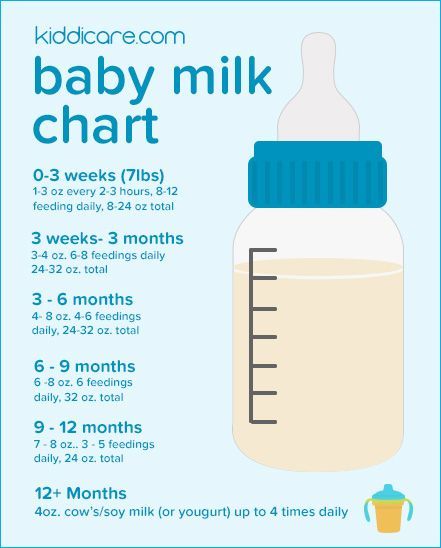
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
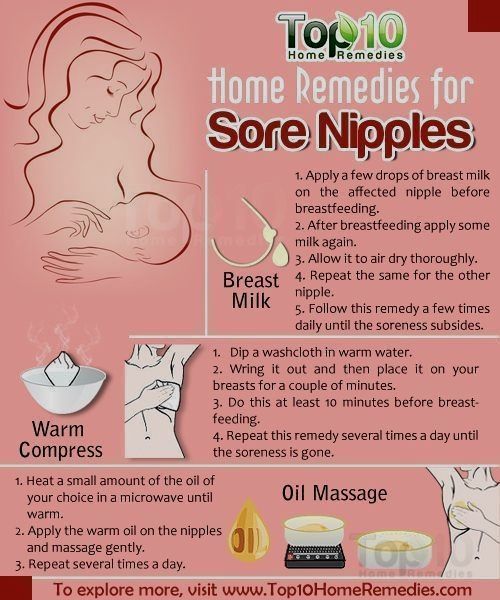
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.

- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
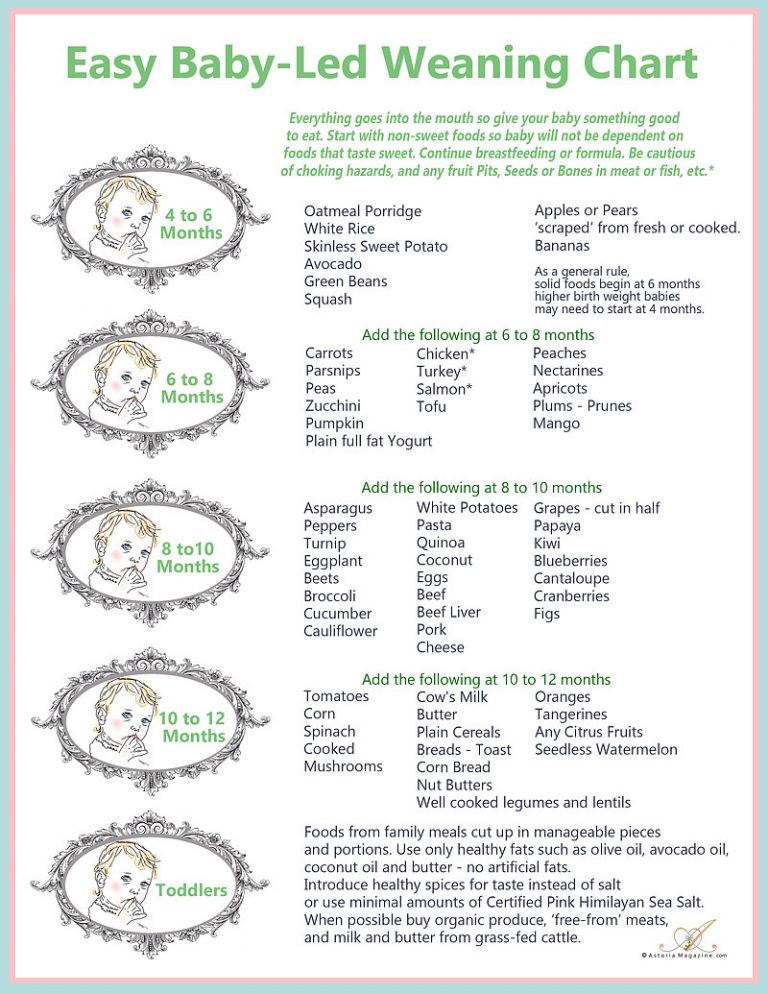
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/20/2022
Last Revised: 09/21/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Pyloric Stenosis (for Parents) - Nemours KidsHealth
What Is Pyloric Stenosis?
Pyloric stenosis is a condition that can affect the gastrointestinal tract in babies. It can make a baby vomit forcefully and often, and can lead to other problems, such as dehydration. Pyloric stenosis needs medical care right away.
What Happens in Pyloric Stenosis?
Food and other stomach contents pass through the pylorus, the lower part of the stomach, to enter the small intestine. Pyloric stenosis (pie-LOR-ik stih-NOE-sis) is a narrowing of the pylorus. When a baby has pyloric stenosis, this narrowing of the pyloric channel prevents food from emptying out of the stomach.
Pyloric stenosis (also called infantile hypertrophic pyloric stenosis) is a type of gastric outlet obstruction, which means a blockage from the stomach to the intestines.
Pyloric stenosis affects about 3 out of 1,000 babies in the United States. It's more likely to affect firstborn male infants and also runs in families — if a parent had pyloric stenosis, then a baby has up to a 20% risk of developing it. Most infants who have it develop symptoms 3 to 5 weeks after birth.
What Causes Pyloric Stenosis?
It's thought that babies who develop pyloric stenosis are not born with it, but have progressive thickening of the pylorus after birth. A baby will start to show symptoms when the pylorus is so thick that the stomach can't empty properly.
The cause of this thickening isn't clear. It might be a combination of several things. For example, use of erythromycin (an antibiotic) in babies in the first 2 weeks of life or antibiotics given to moms at the end of pregnancy or during breastfeeding can be associated with pyloric stenosis.
What Are the Signs & Symptoms of Pyloric Stenosis?
Symptoms of pyloric stenosis typically begin when a baby is around 3 weeks old. They include:
- Vomiting. The first symptom is usually vomiting. At first it may seem that the baby is just spitting up often, but then it tends to become projectile vomiting, in which the breast milk or formula is ejected forcefully from the mouth, in an arc, sometimes over a distance of several feet. Projectile vomiting usually takes place soon after the end of a feeding, although in some cases it can happen hours later.
The vomited milk might smell curdled because it has mixed with stomach acid. The vomit will not contain bile, a greenish fluid from the liver that mixes with digested food after it leaves the stomach.
Despite vomiting, a baby with pyloric stenosis is usually hungry again soon after vomiting and will want to eat. It's important to know that even with the vomiting, the baby might not seem to be in great pain or at first look very ill.

- Changes in stools. Babies with pyloric stenosis usually have fewer, smaller stools (poops) because little or no food is reaching the intestines. Constipation or poop with mucus also can happen.
- Failure to gain weight or weight loss. Most babies with pyloric stenosis will fail to gain weight or will lose weight. As the condition gets worse, they might become dehydrated.
Dehydrated infants are less active than usual, and they may develop a sunken "soft spot" on their heads and sunken eyes, and their skin may look wrinkled. Because less pee is made, they can go more than 4 to 6 hours between wet diapers.
- Waves of peristalsis. After feeds, increased stomach contractions may make noticeable ripples, which move from left to right over the baby's belly as the stomach tries to empty itself against the thickened pylorus.
It's important to call your doctor if your baby has any of these symptoms.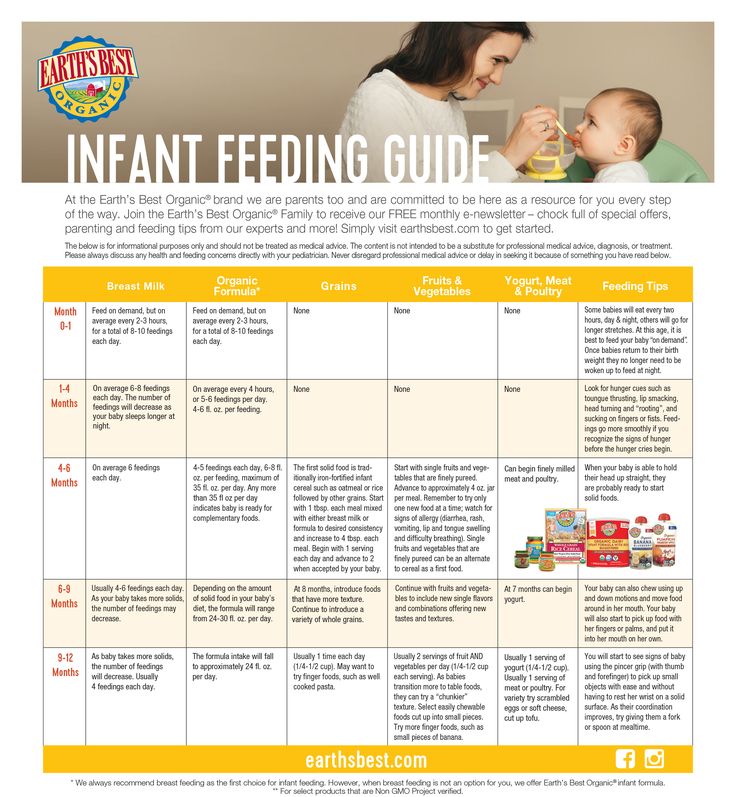
Other conditions can cause similar problems. For instance:
- gastroesophageal reflux (GER) usually begins before 8 weeks of age. GER involves lots of spitting up (reflux) after feedings, which can look like vomiting. But most babies with GER don't have projectile vomiting, and while they might have trouble gaining weight, they usually have normal poops.
- a milk protein allergy also can make a baby spit up or vomit, and have diarrhea. But these babies don't have projectile vomiting.
- gastroenteritis (inflammation in the digestive tract that can be caused by viral or bacterial infection) also can cause vomiting and dehydration. But babies with gastroenteritis usually also have diarrhea with loose, watery, or sometimes bloody stools. Diarrhea usually isn't seen with pyloric stenosis.
How Is Pyloric Stenosis Diagnosed?
The doctor will ask detailed questions about the baby's feeding and vomiting patterns, including what the vomit looks like. The doctor will do an exam, and note any weight loss or failure to maintain growth since birth.
The doctor will do an exam, and note any weight loss or failure to maintain growth since birth.
The doctor will check for a lump in the abdomen. If the doctor feels this lump, which usually is firm and movable and feels like an olive, it's a strong indication that a baby has pyloric stenosis.
If pyloric stenosis seems likely, the doctor probably will order an abdominal ultrasound. The enlarged, thickened pylorus will show on ultrasound images. The doctor may ask that the baby not be fed for several hours before an ultrasound.
Sometimes doctors order a barium swallow instead of an ultrasound. Babies swallow a small amount of a chalky liquid (barium). Then, special X-rays are done that let the doctor check the pyloric area for any narrowing or blockage.
The doctor also might order blood tests to check levels of electrolytes (minerals that help keep fluids balanced and vital organs working properly). An electrolyte imbalance often happens due to the ongoing vomiting of stomach acid and dehydration, and needs to be corrected.
How Is Pyloric Stenosis Treated?
When an infant is diagnosed with pyloric stenosis, either by ultrasound or barium swallow, the baby will be admitted to the hospital and prepared for surgery. Any dehydration or electrolyte problems in the blood will be corrected with intravenous (IV) fluids, usually within 24 hours.
Doctors do a surgery called pyloromyotomy (pie-lor-oh-my-OT-uh-me) to relieve the blockage. Using a small incision (cut), the surgeon examines the pylorus and separates and spreads the thick, tight muscles. This relaxes and opens those muscles.
The surgery can also be done through laparoscopy. This technique uses a tiny scope placed through a small cut in the belly button, letting the doctor see the area of the pylorus. Using other small instruments placed in nearby incisions, the doctor can complete the surgery.
Most babies return to normal feedings fairly quickly, usually 3 to 4 hours after the surgery. Because of swelling at the surgery site, a baby may still vomit small amounts for a day or so. If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If you're breastfeeding, you might worry about continuing while your baby is hospitalized. The hospital staff should be able to provide a breast pump and help you use it so that you can continue to express milk until your baby can feed regularly.
After a successful pyloromyotomy, your baby won't need to follow any special feeding schedules. Your doctor will probably want to examine your child at a follow-up appointment to make sure the surgical site is healing properly and that your baby is feeding well and maintaining or gaining weight.
Pyloric stenosis should not happen again after a pyloromyotomy. If your baby still has symptoms weeks after the surgery, there might be another medical problem, such as gastritis or GER, so let your doctor know right away.
When Should I Call the Doctor?
Pyloric stenosis is an urgent condition that needs immediate treatment. Call your doctor if your baby:
Call your doctor if your baby:
- has lasting or projectile vomiting after feeding
- is losing weight or not gaining weight as expected
- is less active than usual or is very sleepy
- has few or no stools (poops) over a period of 1 or 2 days
- show signs of dehydration, such as more than 4 to 6 hours between wet diapers, a sunken "soft spot" on the head, or sunken eyes
A newborn vomited up - what to do, causes and how to help
The urge to vomit in a newborn is an alarming symptom that should not be ignored. They may be the result of accidental ingestion of a small object by a baby, intoxication, acute appendicitis, intestinal obstruction, or other diseases. The most harmless reason that a child vomited is overeating.
Physiological causes of vomiting
Sometimes vomiting is a short-term phenomenon that is not associated with pathology or disease. What could be the reasons that a healthy newborn vomited:
- overeating - the baby ate too much breast milk or formula;
- the baby is teething, and vomiting is a sign of temporary malaise;
- child swallows air while feeding;
- wrong daily routine, severe fatigue;
- active play and activity immediately after eating.

If the baby feels well, you need to help him calm down and give him a drink of warm boiled water. Put the baby to sleep on the side. The baby will relax, the contents of the stomach will move into the intestines, and vomiting attacks will not recur. Try not to bathe the baby, do not shake immediately after eating. Keep track of the amount of food he gets to avoid overeating. nine0003
The introduction of a new mixture can also cause vomiting. Check with your pediatrician to make sure there are no other causes. Your doctor can help you find other foods that are right for your child.
Sometimes babies feel sick after crying for a long time, for example, the mother left, and the baby is very bored or hungry. If there are no other alarming symptoms, calm the baby as soon as possible, shake, feed, sing a gentle song. If vomiting recurs later, you need to call the pediatrician. nine0003
Symptoms and possible causes of vomiting
Most often, vomiting is a signal of diseases that can be identified by additional symptoms.
Poisoning or intestinal infections
The symptoms of poisoning and intestinal infection are very similar: the newborn is sick, his stool changes, his tummy hurts and his temperature rises. The child should be given constant water to drink so that dehydration does not occur. In any of these conditions, you need to urgently call a doctor. nine0003
Concussion
Babies are very mobile, if a child hits his head or falls, you need to urgently call an ambulance. A concussion is accompanied by vomiting, crying, temporary loss of consciousness, pallor, drowsiness, and impaired coordination of movements.
Foreign body
Swallowing a small object can also cause vomiting without vomiting in neonates. The baby may begin to salivate profusely, have breathing problems, he may vomit with mucus and blood in the vomit. If you suspect that the baby has swallowed any object, call an ambulance. nine0003
Appendicitis
This phenomenon is rare in newborns. If appendicitis is inflamed, the baby has a very sore tummy, when stroking or probing, the pain and crying intensify. There is nausea, weakness, restless behavior. Inflammation of appendicitis in infants is life-threatening, you need to urgently call an ambulance.
If appendicitis is inflamed, the baby has a very sore tummy, when stroking or probing, the pain and crying intensify. There is nausea, weakness, restless behavior. Inflammation of appendicitis in infants is life-threatening, you need to urgently call an ambulance.
Allergic reaction, food intolerance
If a child has an intolerance to certain foods or an allergy to them, vomiting is accompanied by diarrhea, skin rashes, the baby is capricious, restless. With such symptoms, you need to contact a pediatrician and an allergist. nine0003
Acute infections
SARS, pyelonephritis, pneumonia can provoke a gag reflex without vomiting in a newborn from severe coughing spells and general weakness. With a high temperature, sore throat, cough, you need to call a pediatrician at home to examine the child and prescribe appropriate treatment.
Intestinal obstruction
This is a dangerous disease. It can be congenital or acquired. Accompanied by severe bloating, bile impurities are observed in vomiting. The baby cries a lot, the stool changes to a state of red jelly. Feeding is stopped and urgently seek medical help - the disease is life-threatening. nine0003
Accompanied by severe bloating, bile impurities are observed in vomiting. The baby cries a lot, the stool changes to a state of red jelly. Feeding is stopped and urgently seek medical help - the disease is life-threatening. nine0003
Congenital pathologies of the digestive system
Congenital pathologies lead to serious digestive problems. If you notice that the child is restless during feeding, his stool is broken, his tummy is swollen, he is gaining weight poorly or losing it, consult a doctor. It is necessary to undergo an examination of the gastrointestinal tract and pass additional tests.
Neurological disorders
The main causes of gag reflex without vomiting in the newborn are neurological disorders. They occur most often in premature babies, in children with underweight. The cause of such disorders may be birth trauma, asphyxia or fetal hypoxia. With such pathologies, gag reflexes are accompanied by hyperactivity, chin tremor, strabismus, convulsions. You need to contact a neurologist and undergo inpatient treatment. nine0003
You need to contact a neurologist and undergo inpatient treatment. nine0003
Heat stroke
Heat stroke is accompanied by nausea, skin redness, dizziness, rapid breathing. Also, the child develops lethargy, dry skin. Call the doctors, before they arrive, put the child in a cool place on the barrel.
How to distinguish vomiting from regurgitation
Spitting up is a natural process. The baby spits up a few minutes after feeding. It is not dangerous, it is a normal physiological process. If the baby gets a large amount of air into the tummy (swallowed while eating), then after regurgitation the discomfort disappears, he immediately feels better. nine0003
Vomiting is the result of reflex contraction of the muscles of the abdominal cavity and diaphragm, it is accompanied by rapid breathing, profuse salivation.
The main differences between vomiting and regurgitation:
Why vomiting is dangerous
Vomiting is a protective reflex of the body. So he gets rid of foreign bodies, removes toxins, microorganisms, excess food. Most often, vomiting is a symptom of diseases that are dangerous for the baby:
So he gets rid of foreign bodies, removes toxins, microorganisms, excess food. Most often, vomiting is a symptom of diseases that are dangerous for the baby:
- Vomiting itself is dangerous due to possible dehydration of the body. The baby loses not only the liquid, but also the mineral salts dissolved in it. The water-salt balance is disturbed, this affects the general condition of the crumbs. For newborns, this is especially dangerous, because dehydration occurs rapidly, and replenishing a full supply of fluid is not so easy. nine0006
- The second danger of vomiting is the inhalation of vomit. During an attack, the baby should be held upright, for safety reasons, you need to ensure that the baby's head lies on its side in a dream.
- Weight loss due to food rejection is also dangerous. This is especially important for premature babies or babies with a small body weight.
If the baby has vomited, carefully monitor his condition and well-being. Make sure it's not spitting up. If in doubt, it is better to call a doctor anyway, rather than wait for more serious symptoms. nine0003
Make sure it's not spitting up. If in doubt, it is better to call a doctor anyway, rather than wait for more serious symptoms. nine0003
When to call a doctor
It is always better to play it safe and call a doctor if you are not sure about your baby's health. In which cases it is necessary to seek medical help:
- the baby is vomiting, but he did not poop;
- the child is crying, restless, his stomach hurts;
- repeated vomiting;
- symptoms of dehydration appear;
- vomiting accompanied by diarrhoea; nine0006
- vomiting is a fountain;
- before vomiting the child fell or hit his head hard;
- there is blood in the vomit, brown or black blotches;
- the child does not eat or drink;
- everything that the child ate and drank comes out with vomiting;
- he has a high temperature;
- baby is lethargic, sleepy.
Treatment
Vomiting in children may require enterosorbent. It is believed that this tool binds and removes from the body toxic metabolites, allergens, bacteria, viruses and other harmful compounds that can provoke vomiting. nine0003
For the smallest, that is, children under two years old, when choosing an enterosorbent to alleviate the conditions that caused vomiting, you can be guided by the statement of ANSM (France). So, in March 2019, this French regulator published information that raw materials for the production of clay-based powder enterosorbents may contain lead. This harmful substance can penetrate into the bloodstream and in certain concentrations have a depressing effect on the development of the baby.
The Russian Society of Obstetricians and Gynecologists (ROAG) designated the Russian "Enterosgel" as the first choice for the treatment of conditions requiring the use of an enterosorbent in young children, pregnant and lactating women.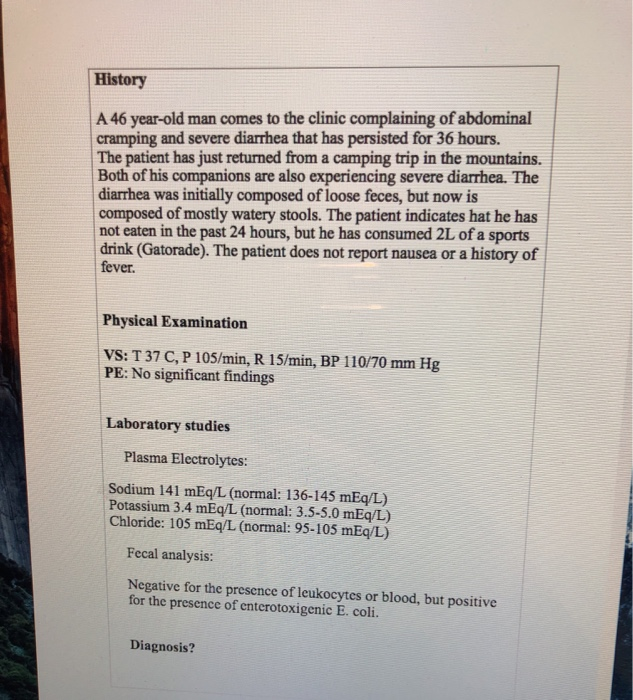 "Enterosgel" is a molecular sponge that is not absorbed into the blood and works only in the lumen of the gastrointestinal tract. A homogeneous gel-like form with a neutral smell and taste simplifies the use of "Enterosgel" even for the smallest. It is important that "Enterosgel" promotes the healing of microtraumas on the mucous membranes of the gastrointestinal tract and minimizes the risk of constipation during use due to the formula saturated with water. nine0003
"Enterosgel" is a molecular sponge that is not absorbed into the blood and works only in the lumen of the gastrointestinal tract. A homogeneous gel-like form with a neutral smell and taste simplifies the use of "Enterosgel" even for the smallest. It is important that "Enterosgel" promotes the healing of microtraumas on the mucous membranes of the gastrointestinal tract and minimizes the risk of constipation during use due to the formula saturated with water. nine0003
The main danger of vomiting is dehydration. It is urgent to call a doctor so that he establishes the cause of vomiting and prescribes the appropriate treatment. Also, the doctor prescribes electrolyte solutions, which need to replenish the fluid lost by the body.
What to do while waiting for the doctor
- make sure that the child is in an upright position;
- after each bout of vomiting, wash the child, clean his mouth and nose;
- try not to disturb the child unnecessarily, do not carry him from place to place;
- it is possible to feed milk or a mixture familiar to the baby if there are no other dangerous symptoms;
- try to give the baby some water to drink;
- do not give any medication until the doctor arrives;
- do not give the newborn prebiotics, probiotics, zinc, enterosorbents, antidiarrheal drugs (if diarrhea has joined) - the doctor should prescribe treatment, it is dangerous to experiment in the treatment of such a small child.
 nine0014
nine0014
What to give your baby to drink
Give your baby plenty of fluids to prevent dehydration. It is best to put the baby to the breast more often. If the doctor has already suggested which pharmacy solutions of electrolytes can be used, use them. If there are no such appointments, you can make the solution yourself. How to cook:
- take 1 liter of boiled water;
- add 1 level teaspoon of salt;
- 4-5 level teaspoons of sugar. nine0014
Mix everything thoroughly, store in the refrigerator for no more than a day. Give your child a few milliliters every five to ten minutes. To do this, take a syringe, remove it from it and put the tip with a needle away and gently squeeze the liquid into the baby's mouth with such a harmless piston.
Signs that the treatment is not working
Sometimes the situation does not improve or even worsens after a doctor prescribes treatment. Carefully monitor the well-being of the child. You need to re-call the doctor and change the treatment regimen if:
You need to re-call the doctor and change the treatment regimen if:
- vomiting and diarrhea do not subside within 24 hours after treatment;
- condition worsens;
- vomiting worse from drinking too much;
- the baby became lethargic and drowsy.
Pay attention to your baby's signs of illness. Call a doctor, follow the prescribed treatment. Track how the child's condition changes. With timely treatment, babies quickly recover and recover from illnesses. nine0003
Regurgitation and vomiting in children
Regurgitation syndrome is one of the most common reasons parents of young children visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc. nine0003
nine0003
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes. nine0003
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life. nine0003
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia. If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age of the child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc. In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.