What do i need to bottle feed my baby
Bottle feeding advice - NHS
If you're planning to bottle feed with expressed breast milk or infant formula, these tips will help you feed your baby and keep them safe and healthy.
If you decide to use infant formula, first infant formula (first milk) should always be the first formula you give your baby. You can use it throughout the first year.
Buying bottle feeding equipment
You'll need several bottles, teats and a bottle brush, as well as sterilising equipment, such as a cold-water steriliser, microwave or steam steriliser.
There's no evidence that 1 type of teat or bottle is better than any other. Simple bottles that are easy to wash and sterilise are probably best.
Making up bottles for your baby
Make sure you sterilise bottles and teats until your baby is at least 12 months old. Wash your hands thoroughly before handling sterilised bottle and teats.
If you're using infant formula, follow the instructions on the packaging carefully when you make up the feed.
See how to make up baby formula.
How to bottle feed your baby
Bottle feeding is a chance to feel close to your baby and get to know and bond with them. Babies will feel more secure if most feeds are given by you, your partner or their main caregiver.
Make sure you're sitting comfortably with your baby close to you. Enjoy holding your baby, look into their eyes and talk to them as you feed them.
Hold your baby in a semi-upright position for bottle feeds. Support their head so they can breathe and swallow comfortably.
Brush the teat against your baby's lips and when they open their mouth wide let them draw in the teat.
Always give your baby plenty of time to feed.
Do not leave your baby alone
Never leave your baby alone to feed with a propped-up bottle as they may choke on the milk.
Keep the bottle horizontal
Gently place the teat into the baby’s mouth. Keep the bottle in a horizontal position (just slightly tipped). This will allow the milk to flow steadily and help prevent your baby from taking in air.
If the teat goes flat while you're feeding, pull gently on the corner of your baby's mouth to release the suction.
If the teat gets blocked, replace it with another sterile teat.
Be guided by your baby
All babies are different. Your baby will know how much milk they need. Some want to feed more often than others. Just follow your baby's lead.
Feed your baby when they seem hungry and do not worry if they do not finish the bottle.
Winding your baby
Your baby may take short breaks during a feed and may sometimes need to burp.
When your baby has had enough milk, hold them upright and gently rub or pat their back to bring up any wind.
Throw away unused milk
Throw away any unused formula or breast milk after you've finished bottle feeding your baby.
Only make up the feed when needed – one feed at a time.
Help with bottle feeding
Talk to your midwife, health visitor or other mothers who have bottle fed if you need help and support.
You'll find the phone number for your health visitor in your baby's personal health record (red book).
Your questions about bottle feeding
Why if my baby does not settle after feeds?
If your baby swallows air while bottle feeding, they may feel uncomfortable and cry.
After a feed, hold your baby upright against your shoulder or propped forward on your lap. Gently rub their back so any trapped air can find its way out.
Your baby may sometimes only burp up a small amount of air.
Why is my baby sometimes sick after feeds?
It's normal for babies to bring up a little milk during or just after a feed. This is called possetting, regurgitation or reflux.
Keep a muslin square handy just in case.
Check that the hole in your baby's teat is not too big. Drinking milk too quickly can make your baby sick.
Do not force them to take more milk than they want during a feed. This may be distressing for your baby and can lead to overfeeding.
Sitting your baby upright on your lap after a feed may help.
If it happens a lot, or your baby is violently sick, seems to be in pain or you're worried for any other reason, talk to your health visitor or GP.
Can formula make my baby constipated?
When using formula, always use the amount of powder recommended on the packaging.
Do not add extra formula powder. Using too much can make your baby constipated and may cause dehydration.
If your baby is under 8 weeks old and has not done a poo for 2 to 3 days, talk to your midwife, health visitor or GP, particularly if your baby is gaining weight slowly.
Your baby should be gaining weight and have plenty of wet and dirty nappies.
Infant formula and allergies
If you think your baby might be allergic to or intolerant of formula, talk to your GP. If necessary, they can prescribe a special formula feed.
Some formula is labelled as hypoallergenic, but this is not suitable for babies with a diagnosed cows' milk allergy.
Soya formula should only be given to babies under medical supervision.
Always talk to your GP before using hypoallergenic or soya-based formula.
Read more about cows' milk allergy and lactose intolerance.
Get Start4Life pregnancy and baby emails
For information and advice you can trust, sign up for weekly Start4Life pregnancy and baby emails.
The Start4Life website also has more information and advice about expressing and bottle feeding
Bottle Feeding: Tips and Tricks
Congratulations! You’ve made the decision to bottle feed your baby. Feeding your baby is about keeping your baby happy, healthy, and well fed in a manner that supports them and you as their caregiver.
Feeding your baby is about keeping your baby happy, healthy, and well fed in a manner that supports them and you as their caregiver.
Whether you plan to use formula, breastmilk, or both, bottle feeding your baby requires certain equipment, the right know-how, and a little bit of advice about feeding on the go.
Milk Drunk consulted with Dr. Jacqueline Winkelmann (“Doctor Jacq”), board-certified pediatrician (and mom), to find out exactly what is essential for bottle feeding, what to consider when shopping for formula, how best to clean your feeding supplies, and what to do about feedings on the go.
Table of Contents
- The Basics for Bottle Feeding
- Bottles and Nipples
- Formula
- Pump
- Nursing Pillow
- Burp Cloths
- Cleaning Supplies
- Soap or Bottle Cleanser/Sterilizer
- Bottle Cleaning Brush
- Feeding on the Go
The Basics for Bottle Feeding
The decision to bottle feed means learning about bottle basics. Entering a big box baby store can feel overwhelming-who knew there were so many different types of bottles? Which one is the best?
Entering a big box baby store can feel overwhelming-who knew there were so many different types of bottles? Which one is the best?
Don’t worry. Most items will be subject to preference (i.e. do you prefer bottles that work well when breastfeeding, do you need bottles that help eliminate gas?).
We asked Dr. Jacq for her most important tip when shopping for bottle supplies:
“One thing to keep in mind when you shop: Everything should be BPA-free!”
Most bottles will be BPA-free because the FDA no longer allows them to be manufactured with this chemical. If you plan to use hand-me-down bottles, or even bottles you have from a previous baby, check with the manufacturer to ensure they were manufactured after the date of restriction, which was July 12, 2012.
How much should you buy in terms of bottle supplies?
Use this rule of thumb: five to ten bottles and accompanying supplies (nipples, etc.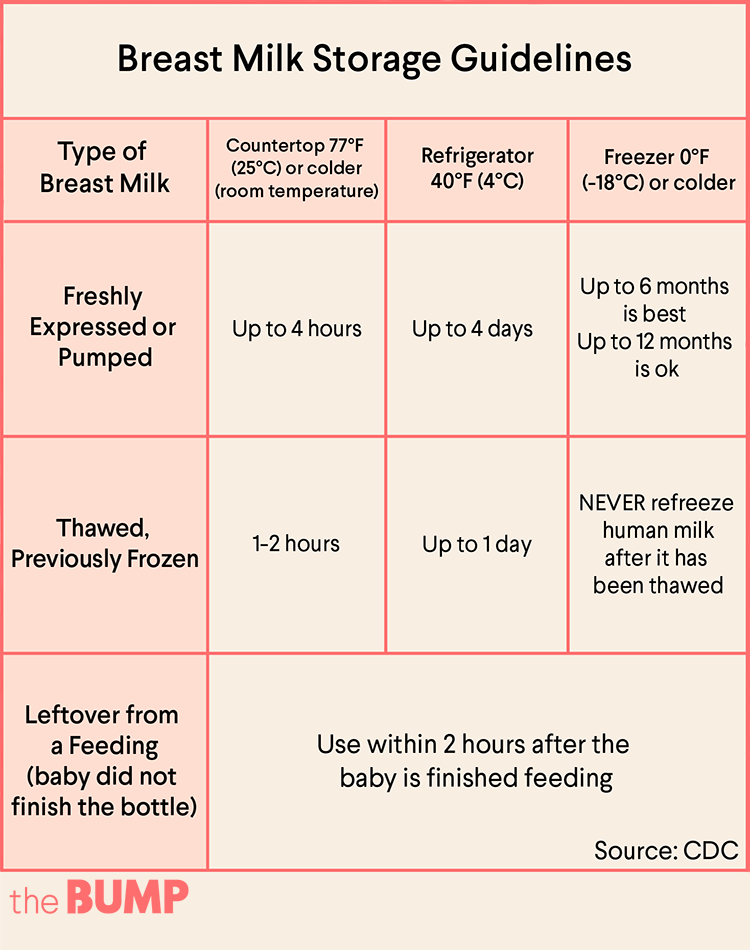 ) should work perfectly for a baby who will be exclusively bottle fed. If you plan to combo feed (breastfeed and bottle feed) you can consider buying two to three less, but you may find that having extra bottles on hand is very convenient.
) should work perfectly for a baby who will be exclusively bottle fed. If you plan to combo feed (breastfeed and bottle feed) you can consider buying two to three less, but you may find that having extra bottles on hand is very convenient.
Now that you know what to avoid (BPA) and how much you need, let’s start shopping!
Bottles and Nipples
Again, use the five to ten rule for exclusively bottle-fed babies when creating a bottle stock pile.
Here are some tips from Dr. Jacq on bottle selection that can help you wade through the sea of available options.
“Baby bottles and nipples should all be BPA free. Look for bottles that help prevent colic and air bubbles, are easy to clean, and reasonably priced.”
It isn’t necessary to spend a lot of money on your bottles as long as they are safe and effective.
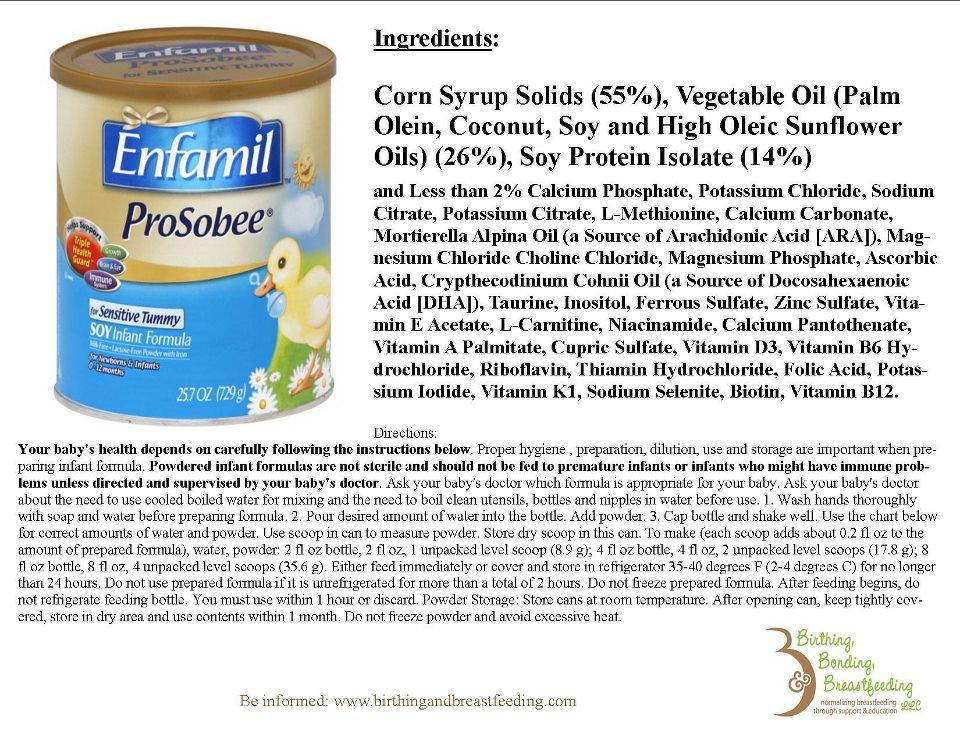
Formula
All formula will technically feed your baby, but not all formula is identical. Look for formula with clean ingredients, and if you have questions about the contents, ask your baby’s pediatrician.
When asked about formula selection, Dr. Jacq asks, “What’s important to you, as this baby’s parent or caregiver, in a formula?”
Dr. Jacq says there are things to consider when selecting a formula:
- Does my child have a special need? If your baby was born prematurely, has specific food allergies, or immune deficiencies, you may be limited to certain types of formula (i.e. non-dairy,etc.).
- Is the formula easy to find at a local store or online? You’ve read about (and love) European formula, but getting access to it can be difficult at best, and nearly impossible during a pandemic. Ultimately, you need continual, consistent access to your formula supply.
Baby Bonus: If you want the same great quality and ingredients that are provided by European formula, you don’t (and shouldn’t) have to buy it on the “formula black market.” Bobbie organic baby formula was created to meet European formula standards and is available for purchase in the U. S.
S.
- Does it meet my need for convenience? Convenience matters. If you’re a caregiver on the go, choosing formula that comes in pre-portioned packages could be a huge help. Formula is available as powder, ready to feed, and as a liquid concentrate.
- Are clean, organic ingredients important to me and my family? We get it. You’re on a budget and you may not even eat organically yourself. The most important thing is to feed your baby the proper balance of dietary macros.
Ingredients do matter, and the sources of the macros (carbohydrates, fats, and proteins) will differ between formula brands.
Baby Bonus: Bobbie baby formula is modeled after a European style recipe that is closest in composition to breastmilk. What goes into Bobbie is just as important as what doesn’t. With Bobbie, you can be confident the macros of your baby’s formula are carefully thought out and crafted from organic, high-quality ingredients.
Also, you’ll never find fillers, GMO’s,or hexane-extracted DHA in Bobbie.
- Is the formula regulated and vetted by the U.S. FDA? We asked Dr. Jacq her thoughts on FDA compliant formulas. She says,
“While all infant formulas marketed, sold, and manufactured in the U.S. must be FDA compliant, and nutritional guidelines are set for all formulas, the sourcing of ingredients, compositions and specifics on ingredients can vary greatly.
“This is an area I feel parents should spend some time researching before their baby comes, even if you plan on exclusively breastfeeding. If and when the time comes to use formula, you want to be prepared with knowledge and have an option or two you have researched and know how to get.”
If you’re still struggling to find a formula that meets the needs of your family, sites like Baby Formula Expert are great for getting the latest formula information.
Formula Dispenser
A formula dispenser is a great option for getting an accurate formula to water ratio each and every time. It’s also a huge time saver, and incredibly convenient in terms of bottle prepping.
Formula dispensers are available in travel size and as stand alone small appliances. What you use will be determined by your specific needs.
Pump
If you plan to combination feed (give your baby both breast milk and formula) you’ll need a breast pump. Even if you plan to nurse rather than give your breastmilk to your baby in a bottle, having a breast pump on standby can help if you find you overproduce or if there’s an unexpected reason you’ll be away from your child.
Nursing Pillow
Nursing pillows aren’t just for nursing! They’re great for giving your arms and back a rest while you bottle feed your baby. Most nursing pillows position around your midsection and provide a secure place for your baby to lay while keeping you in an upright (instead of hunched over) position.
Burp Cloths
Dr. Jacq says you can’t go wrong stocking up on burp cloths.
“Both breastfed and formula fed babies will spit up-a lot! Spit up is caused by an immature valve between the esophagus (feeding tube) and the stomach. It starts in the first few weeks of life, peaks at 4-5 months, and usually goes away by 12 months.”
Cleaning Supplies
Bottle feeding requires cleaning, and you can opt to handwash your bottles and nipples or opt for dishwasher safe brands. Either way, your baby’s bottles need to be sterilized. It’s especially important to sterilize bottles before the first use, if your baby is premature, very young (three months of age or younger) or has a compromised immune system.
Dr. Jacq advises that making sure your bottles and bottle parts are thoroughly dry after washing and sterilizing is key to avoiding bacteria growth.
“Bacteria love moist environments, so leaving a clean bottle wet might defeat the purpose of cleaning and sterilizing in the first place. ”
”
When cleaning your baby’s bottles, follow the CDC guidelines for cleaning and sterilizing so you know you’re doing it correctly and always offering your child a clean, sterile bottle.
If you’re starting a registry or simply want to add a bit more convenience to your bottle-feeding routine, you can grab a combo bottle sterilizer and dryer. These small appliances make it easy to ensure your baby’s bottles are fully clean, completely sterile, and ready for use.
Your Dishwasher!
Provided your bottles and nipples are designed for dishwasher use, using your dishwasher is a great way to clean and sterilize. Bonus points if your dishwasher has a specific sterilize cycle, but it isn’t 100% needed.
Soap or Bottle Cleanser/Sterilizer
You can use a mild dish soap for cleaning and sterilizing your baby’s bottles, or you can use a specialty bottle soap available from many baby stores or websites. Either way, it’s most important to ensure you remove all the soap from your baby’s bottles if washing by hand.
Bottle Cleaning Brush
A bottle cleaning brush is necessary to get inside the bottle and reach to the bottom. If you’re washing by hand, it’s impossible to properly clean a baby’s bottle with a rag. Be sure to rinse the brush thoroughly or toss it in the dishwasher every couple of days to ensure it is also sanitized and not harboring bacteria that could make your baby sick.
Bottle or Dish Drying Rack (If Washing By Hand)
As previously mentioned, a damp bottle can become a bacteria breeding ground. A bottle drying rack is designed to allow a cleaned bottle to rest upright and excess water to drain from it, allowing the bottle to dry completely before it is stored or used again.
Feeding on the Go
Dr. Jacq says the key to successful feeding on the go is to always have extra; extra formula, bottles, nipples, burp clothes, etc.
When feeding on the go, plan for the unexpected. A formula dispenser can also be a huge help, especially if you find yourself mixing formula bottles while in transit (i. e. in the car, on the plane, etc.).
e. in the car, on the plane, etc.).
It never fails — you’re away from home and preparing a bottle for your baby when you discover the nipple brought is either damaged or has spent the past three weeks floating around in the bottom of the diaper bag (oops).
Carrying a few extra nipples in a sterile container can ensure you’re never without.
Insulated Bottle Carrier/Travel Cooler
When feeding on the go, it’s crucial to ensure the formula and/or breastmilk you offer your baby is still fresh. Dr. Jacq says:
“According to the CDC, breast milk can stay out at room temperature for four hours, formula for two hours, and one hour if baby drank from it.”
She says there are other things to consider when shopping for insulated bottle carriers and travel coolers:
- Do you even need one? These items are really convenient for traveling, outings, storing breastmilk at work, taking a few bottles to daycare or grandma’s.

- Bag size. How many bottles are you planning on storing? Bags come in various sizes, from lunch bags to large backpacks.
- Degree of coldness. Look for a well insulated bag. Does it have a removable ice pack? Is it standard size?
- Cleaning. Don’t cry over spilled milk! Make sure the bag is easy to clean (or even machine washable).
- Is the bag easy to carry?
- Extra storage. Do you need/want to store additional items in the same bag? Keys, wallet, phone?
- Style. Let’s face it, it should look good, and there are numerous options available nowadays so you don’t have to settle.
Final Tips
And with that, Dr. Jacq wrapped things up with us with these final thoughts:
“With so many baby products out there, it can be overwhelming to know what you will want or need, especially as a first time parent.
“Seek the advice of friends, family, your pediatrician or health care provider, or even the internet! In the end, you will discover as you go along, what really matters to you and what makes your life easier. ”
”
Sources:
https://www.healthychildren.org/English/ages-stages/baby/feeding-nutrition/Pages/Baby-Bottles-And-Bisphenol-A-BPA.aspx
https://www.fda.gov/food/food-additives-petitions/bisphenol-bpa-use-food-contact-application
https://babyformulaexpert.com
https://www.cornucopia.org/DHA/DHA_QuestionsAnswers.pdf
https://www.cdc.gov/healthywater/hygiene/healthychildcare/infantfeeding/cleansanitize.html
https://www.cdc.gov/nutrition/infantandtoddlernutrition/formula-feeding/infant-formula-preparation-and-storage.html
The content on this site is for informational purposes only and not intended to be a substitute for professional medical advice, diagnosis or treatment. Discuss any health or feeding concerns with your infant's pediatrician. Never disregard professional medical advice or delay it based on the content on this page.
The dangers of breastfeeding promotion
- Claire Wilson
- BBC Future
Image Credit, iStock
Breastfeeding certainly has many benefits. However, the pressure sometimes placed on women through breastfeeding campaigns of all kinds, including state-sponsored ones, carries potential dangers. Browser BBC Future explains why mothers should have free choice.
However, the pressure sometimes placed on women through breastfeeding campaigns of all kinds, including state-sponsored ones, carries potential dangers. Browser BBC Future explains why mothers should have free choice.
When Suzanne Burston of Chicago was expecting her first child, she was determined to do the right thing, including breastfeeding her son.
"I even took breastfeeding courses," says the woman.
But after a few days it became clear that the baby could not breastfeed properly, and Suzanne had to express milk and bottle feed the baby.
- What does it mean to be a good mother in today's world?
- Why childbirth is so difficult and dangerous
- Russian woman who gave birth to 69 children: truth or fiction?
- Is it possible to determine the sex of a child by the size of the mother's belly?
This procedure took several hours every day, leaving the woman little time for herself. Mental and physical exhaustion led to postpartum depression.
Mental and physical exhaustion led to postpartum depression.
Susanne's son also did not feel well, he had skin rashes and bloody diarrhea.
The doctor said that it could be caused by an allergic reaction of the body to some foods in the mother's diet and suggested trying hypoallergenic milk formula.
Literally two days later, the baby's digestion improved, and all unpleasant symptoms disappeared.
It's good that everything ended like this, but remembering his suffering, Burston is indignant. Why put pressure on mothers like that? In her opinion, "the role of breastfeeding is greatly exaggerated."
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
Exaggerated? Sounds pretty weird. "Breastfeeding for the baby is the best option," the WHO, UNICEF and many other respected medical organizations advise unanimously.
"Breastfeeding for the baby is the best option," the WHO, UNICEF and many other respected medical organizations advise unanimously.
They point out that for the first six months of life, babies should be exclusively breastfed, as this has huge health benefits for both mothers and their newborns.
Breast milk is considered so beneficial that women are advised to breastfeed until the child is one or even two years old.
Recently, however, the thesis "breastfeeding at any cost" has been increasingly questioned.
Social activists, doctors and scientists argue that if the process of breastfeeding is not easy for a woman, it can have negative consequences.
In addition, some women are physically unable to produce enough milk.
If such a child's health is not addressed in time, it can lead to dehydration, sometimes even with the risk of brain damage.
The big question is not "breast or formula" but whether the baby is getting proper nutrition, freedom of choice advocates say.
"We hear a lot about the benefits of breastfeeding - great, but also talk about the risks and let women make their choice," says Amy Tater, a former US midwife and author of Push Back, in which she harshly criticized the movement for a natural approach to motherhood.
What do the facts testify to? What do the research results say?
Image copyright, Getty Images
Image caption,Before the benefits of breastfeeding became apparent, doctors and nurses actively promoted formula milk
Official attitudes towards breastfeeding today are very different from what they were in the past. When formula milk gained popularity in the first half of the 20th century, formula manufacturers advertised their products claiming that formula was better than breast milk.
Health workers discouraged women from breastfeeding, considering it old-fashioned or the lot of the lower class.
Now this seems at least strange, because we know that breast milk contains a huge amount of useful substances, in particular, antibodies to many bacteria.
In addition, the composition of milk changes from day to day, meeting the needs of the child's body in various trace elements. Even during one feeding, at first the baby receives more watery milk, which quenches thirst.
There is another issue that highlights the benefits of breastfeeding. The mixture is usually available as a powder to be diluted with water, and in poor countries there is sometimes no access to clean drinking water or the ability to boil it.
Therefore, due to the living conditions, women cannot use the product correctly. They have to use water of dubious purity or pour the mixture into unsterilized bottles.
By the early 1970s, the public around the world began to suspect that manufacturers of dry formulas for infant feeding, vigorously promoting their product in Third World countries and convincing mothers that artificial feeding was preferable to natural, were deliberately distorting the facts.
Anti-formula activists have argued that artificial baby food contributes to child suffering and even sudden death - especially in poor families.
As a result, this led to a boycott of the products of one of the largest baby food manufacturers, Nestle.
Today, in many countries (including Britain - Rev. ) advertising of breast-milk substitutes is prohibited, and medical personnel strongly recommend breastfeeding to parents.
At some point, Burston felt that she was being judged for not breastfeeding her baby. And then she started a blog called Fearless Formula Feeder to support other women in a similar situation.
In the comments on the blog, women told how they suffered from postpartum depression due to the pressure that was put on them.
Image copyright iStock
Image captionNot all moms get enough breast milk after giving birth
Of course, many people enjoy breastfeeding. However, there are women for whom this process turns into real torment. And this only exacerbates the already existing difficulties of young parents - such as lack of time for themselves and lack of sleep.
However, there are women for whom this process turns into real torment. And this only exacerbates the already existing difficulties of young parents - such as lack of time for themselves and lack of sleep.
Theoretically, a husband can help his wife feed her baby with expressed breast milk from a bottle, but, firstly, not all women can express milk, and secondly, some babies refuse a bottle. And then the burden of feeding falls entirely on the mother.
"Physical exhaustion is bad for mental health," Burston says. "I've heard a lot of horror stories. Some women were just on the verge of suicide."
And there are women who are simply physically unable to fully feed their child with their milk.
Women are usually told that this rarely happens. For example, the website of the National Health Service of Great Britain notes that "almost all women are able to produce milk."
However, according to a study by Marianne Neifert of St. Luke's Hospital in Denver, the reality is that one in seven women does not have enough milk to adequately feed a child.
Luke's Hospital in Denver, the reality is that one in seven women does not have enough milk to adequately feed a child.
Even women with good lactation do not begin to produce milk until a few days after giving birth. And in these first days, the baby may develop dehydration or jaundice - as a side effect of a lack of milk.
Barts Health London pediatrician Sasha Howard has seen many cases of dehydration in exclusively breastfed babies.
"They had to be supplemented with formula from a bottle or a nasogastric tube. And some were even given IVs," she says.
In some, although rare, cases, dehydration can lead to brain damage and death.
Ten years ago, if there were problems with breastfeeding, the medical staff suggested using formula.
However, hospitals in many countries are now following UNICEF guidelines and actively encouraging breastfeeding. In the postnatal wards of these hospitals, milk formula is stored in locked cabinets - just like, for example, morphine, which is sold only by prescription.
Image copyright, iStock
Image caption,Mothers can feel guilty about bottle feeding their baby instead of natural feeding… "says Trish McEnroe, Executive Director of Baby-Friendly USA.
She notes that in the past, doctors, regardless of the mother's wishes, would take the baby from her immediately after birth and give him a bottle. The goal of the program is to end this practice, which has interfered with the natural feeding process of newborns.
When a baby is artificially fed, he suckles less often, and the woman's milk supply decreases and the baby is deprived of many nutrients, says McEnroe. But numerous studies have proven that breastfeeding protects the baby from infectious diseases and allergies, and also increases the IQ.
True, this argument has weaknesses. First, formula supplementation has not been proven to interfere with breastfeeding. Milk will not disappear if formula is given once or twice a day.
Many women successfully combine breast and formula feeding for many months. "For some it's the best option," admits McEnroe.
Second, it is unclear whether the benefits of breastfeeding are really that significant. There are doubts about the reliability of the results obtained in the study of this problem.
Since breastfeeding is a very personal matter, scientists cannot divide the subjects into groups and force them to feed their babies only in a certain way.
Therefore, the only way is to observe the feeding process and evaluate the results afterwards.
Such studies do show an association between breastfeeding and good health, but this has not yet been proven.
Of course, we can say that running shoes improve physical fitness. Yes, there is some connection, but there is also a main factor - regular training.
When it comes to breastfeeding, income and education can be an important factor. Today, breastfeeding is more common in high-income families, both because they adhere to doctors' recommendations and because mothers can afford to go on extended maternity leave.
Today, breastfeeding is more common in high-income families, both because they adhere to doctors' recommendations and because mothers can afford to go on extended maternity leave.
Wealthier people are also healthier for a variety of reasons unrelated to breastfeeding, such as smoking less and drinking less alcohol.
So it's no surprise that breastfed babies grow up healthier. It's just a sign of the middle class.
So, in one American study, scientists observed families in which one child was breast-fed, and his brother or sister was fed formula.
The researchers were unable to prove that natural feeding gave the child a significant advantage over "artificial" feeding.
However, there are still advantages in certain situations. Breast milk contributes to the formation of healthy microflora in the intestines of a premature baby, and also reduces the risk of developing serious infections, such as sepsis.
Image copyright, iStock
Image caption,Breast milk reduces the risk of severe infections
Breastfeeding reduces the risk of infections in the first year of life and in developed countries. These data are confirmed by objective studies.
Breastfed babies are less likely to get respiratory viral infections and diarrhea.
However, this effect disappears immediately after breastfeeding is stopped, and therefore the long-term health benefits that breastfeeding advocates speculate about are unlikely to exist.
"If you ask the teachers of any kindergarten to guess which of the children in their group was breastfed and which was formula fed, they won't be able to tell," Burston points out.
Some will say that since we know about the certain benefits of breast milk, there is nothing wrong with exaggerating them a little - for the sake of advertising breastfeeding.
However, this approach calls into question the ability of every woman to make the right decision for herself. Medicine should not be paternalistic, much less coercive.
Medicine should not be paternalistic, much less coercive.
No one has the right to misinform people when they make such a difficult and personal decision. Only the woman herself can weigh the pros and cons, realizing how such a choice will affect her mental and physical health or the financial situation of her family (if she is in a hurry to go to work after the birth of a child).
After all, if a woman works full-time, even from home, breastfeeding her baby exclusively is very difficult.
Countless brochures and posters stress that breastfeeding is free, but this is only true if the mother can afford to take parental leave.
In the US, for example, women take such leave for an average of 10 weeks, and almost a third return to work almost immediately after giving birth.
The current promotion of breastfeeding certainly has its advantages. There are more opportunities to help women who have problems with lactation. There is a lot of talk in society that no one should judge a woman for breastfeeding in public.
There is a lot of talk in society that no one should judge a woman for breastfeeding in public.
But activists like Suzanne Barston want women to be free to make their own choices and not judged by anyone.
You can read the original of this article in English on the website BBC Future .
Feeding in sickness | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less prone to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the possibility of using breast milk to treat everything from conjunctivitis to cancer. 3.4
2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the possibility of using breast milk to treat everything from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed?
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. 7
“Breastfeeding gives your baby everything she needs when she is sick. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. 8 When your baby is sick, the levels of immune-boosting cells (leukocytes) also spike in your milk. 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months, my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip."
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time. If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed?
Occasionally, if a child is not feeling well, they may not have the appetite or energy to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable.
You can express milk with one of our comfortable breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue breastfeeding if I become ill myself?
If you feel unwell, you may not want to, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson.
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery.
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers. Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose.
Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose.
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, it is permissible to take certain medications. 9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues.
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor.
There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor.
“I was on high doses of epilepsy medication, but I was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to ensure my son was safe and to minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged.
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.
“If your baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account.
Having surgery under local or general anesthesia does not necessarily mean that breastfeeding has to be stopped or that milk has to be pumped and discarded. By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, in any case, it is best to consult your doctor or attending physician beforehand.
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk. 11.12 Consult with a qualified professional about your condition to decide if it is safe to continue breastfeeding in such cases.
11.12 Consult with a qualified professional about your condition to decide if it is safe to continue breastfeeding in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if possible. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page.
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet]. "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). 2017;12(9):500-506.
Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188.
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps.