What to feed babies with milk allergy
How to start introducing solids to a baby with a milk allergy
If your baby has been diagnosed with a milk allergy, you might be concerned about weaning. Read on to find out how to do it safely.With thanks to Bahee Van de Bor, paediatric dietitianStep One: How to start solids for your baby with a milk allergyIf your baby has a milk allergy, the first step is to identify the style of baby feeding that you wish to follow. Should you spoon feed or follow baby-led weaning? The choice is yours but check that your baby is ready. According to the NHS, a baby is ready around six months and when they are able to:
- sit upright and hold their head steady
- co-ordinate their eyes, hands and mouth so they can look at the food, pick it up and put it in their mouth by themselves
- swallow food, rather than spit it back out
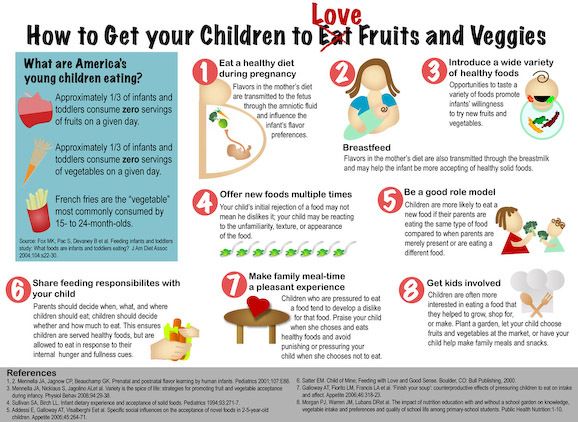
Continue to breastfeed or use your baby’s special infant formula recommended by your GP, paediatric dietitian or allergy doctor. If you’re thinking about baby-led weaning, a recent research paper showed interesting results. The researchers found that babies who followed baby-led weaning were more likely to be offered vegetables and join in with family meals. With a few tweaks to your family meals to ensure that foods available at the table are dairy free, there’s no reason why your baby with a milk allergy cannot join either. Baby led weaning is safe so if this is your preferred feeding style, then go for it! In fact, this UK paper showed that babies at increased risk of choking were those who were not given finger foods alongside their puree foods. Regardless of the type of feeding style you choose, always remain with your baby during meal times to minimise any potential risk of choking.
If your baby has been well since starting their special infant formula or whilst you’ve been following a strict milk free diet for breastfeeding, you may have forgotten the earlier signs and symptoms that your baby had when first diagnosed with a milk allergy. The first thing that you will notice if your baby is accidentally given food containing milk is an allergic reaction. Signs of a milk allergy usually show immediately or within 2 hours and include
- Swollen lips, face or eyes
- hives, urticaria
- abdominal pain, vomiting
Serious symptoms – these are rare
- swollen tongue, persistent cough, hoarse cry
- difficult or noisy breathing
- pale/floppy/unresponsive/unconscious
Symptoms for delayed cow’s milk protein allergy
- recurrent tummy pain, worsening reflux and vomiting
- food refusal
- loose frequent stools – around 6-8 per day
- or constipation 2 or less bowel motions per week
- skin reddening or itch
- worsening eczema
Start with a puree of vegetables and then fruit. Simply peel, chop and then cover with water to cook in a saucepan. Mash with a fork using the water in the pan, breast milk or your baby’s special infant formula. When your baby is ready, offer finger foods. Use very soft pieces of steamed or cooked vegetables such as carrots, broccoli, root vegetables and then move onto fruit. During this phase of weaning, focus on the variety rather than the amount that baby eats. Focus on iron-rich foods. From around 6 months of age, baby’s iron stores and the amount of iron present in breast milk starts to decline. If you are following a plant-based diet, then you can introduce lentils and beans which are good sources of iron. Recommended iron rich foods to give when starting solids for your baby with milk allergy include:
- Lentils
- Nut butter
- Meat, chicken, fish, eggs
- Green leafy vegetables
- Iron-fortified breakfast cereal
If you need to use milk in a recipe, substitute the whole milk in the recipe above with breast milk or your baby’s special infant formula.
Egg, nuts, fish and gluten may be causing you some worry and confusion. If your baby also has moderate to severe eczema your allergy doctor, GP or paediatric dietitian may recommend introducing cooked egg and peanuts to try to prevent your baby’s chances of developing an allergy to these foods. Wait at least a few days before introducing a new food and start with small amounts such as 1/4 to 1/2 teaspoon of cooked food. Gradually increase the amounts offered. If your baby accepts these foods and doesn’t have a reaction then continue to offer these foods as part of their weekly menu plan. If your baby has an allergic reaction, then please stop giving your baby the food that they react to and speak to your family doctor for further advice.
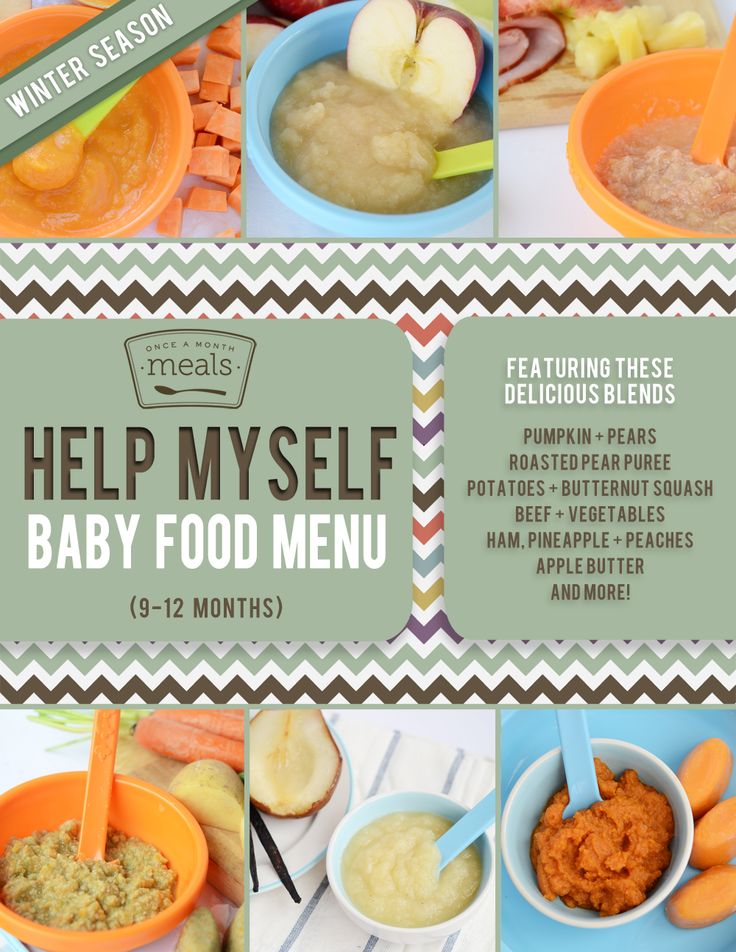
Step six: Menu planning Plan a daily menu with calcium for your baby with a milk allergy. Aim for 3 balanced mini meals per day. From around 9 months of age, you can start to use a plant milk to prepare porridge, dairy free pancakes or homemade bread for breakfast. Not all plant based milks are suitable and your dietitian may recommend using some types over others based on the source and amount of protein, the over all calories, presence of added calcium, vitamins and minerals.
It seems early to think about “meals” but you can start creating mini meals with texture.
- Use root vegetables or grains like quinoa, amaranth, oats, rice, cous cous
- Add iron-rich vegetables and green leafy choices
- Protein (meat, chicken, fish or lentils)
- Use infant formula or a calcium fortified plant drink to get the desired texture
Your baby still needs breast milk or specialist infant formula and they can have dairy-free yoghurts (check that they are calcium fortified). For finger foods, cut up pieces of bread or toast dipped into hummus or calcium-fortified yoghurt based dips. You can even make custard using a dairy free custard powder and then mix with baby’s specialist formula. Other useful foods containing added or natural sources of calcium include:
- oat based creme fraiche and cream that is also calcium fortified
- tahini paste, a plant source of some calcium
- tinned fish with it’s bones to prepare sandwiches (excellent source of calcium)
- broccoli, kale
- beans and pulses
There are many ways that milk can be labelled and it’s not always obvious. Never assume that foods from a “free from” range will be free from cow’s milk protein and remember that you are also avoiding milk and food products made from sheep, goat or buffalo as the protein is very similar to cow’s milk protein.
Bahee Van de Bor RD MBDA is a private paediatric dietitian and former Great Ormond Street Hospital for Children-trained specialist children’s nutritionist. Now based in Harley Street, you can find out more on her website. Follow her on Instagram @ukkidsnutrition or on Facebook @ukkidsnutrition. You can read more from Bahee about weaning babies with milk allergies here. Disclaimer: The views and advice given in this article are those of the guest writer and do not necessarily reflect the opinions of Weaning Week or any other organisations represented on this platform
Cow’s Milk Alternatives: Parent FAQs
By: Anthony Porto, MD, MPH, FAAP & Rachel Drake, MS, RD, CSO, CSP, CDN
Milk is a grocery list staple for many families. But some avoid it because of milk protein allergies or other health concerns. Some kids simply don't like the taste. These families may choose from a growing array of cow's milk alternatives that now fill the dairy aisle.
The nutritional content in the various dairy alternative products is important for parents to be aware of when shopping. Choices range from other animal-based beverages (such as goat's milk) to products made from nuts (such as almond milk), beans (such as soy milk), grains (such as oat) and other plants.
The American Academy of Pediatrics (AAP) knows that deciding what's best for your family can be confusing. To help you sort it all out, here are frequently asked questions from parents about cow's milk alternatives.
When do I introduce cow's milk into my baby's diet?
The AAP recommends
breast milk as the sole source of nutrition for your baby for about the first 6 months. If a baby is breastfed by a mother who is drinking cow's milk, or is formula fed with traditional infant formula, they have already been exposed to cow's milk protein. Most babies can begin consuming dairy foods around 6 months of age—after a few first
solid foods have been introduced. Plain, whole-fat or whole Greek yogurt is a good first form of cow's milk protein for babies to try. Avoid the added sugar commonly found in yogurt marketed to babies and toddlers.
Once a baby is developmentally able to eat finger foods, other dairy—such as pieces of cheese—can be added. The AAP recommends that whole cow's milk and low-iron formulas not be used during the first year of life, because babies' digestive systems under age one year old may not tolerate the cow's milk protein in large quantities. Low-iron formulas can also lead to anemia. Note: Low-iron formulas are no longer marketed routinely in the United States.
What if my baby is allergic to cow's milk?
If your formula-fed baby has a cow's milk allergy, ask your pediatrician about switching to a non-cow's milk, protein-based formula. Hypoallergenic formulas are cow's milk based; only soy formulas are not. Discuss these options with your child's pediatrician before switching.
According to a
study published in
Pediatrics, there is not enough evidence for breastfeeding mothers to routinely avoid allergenic foods—like cow's milk—while breastfeeding.
If your pediatrician diagnoses your baby with a cow's milk protein allergy, then they may recommend you remove cow's milk from your diet while breastfeeding. Be aware that it can take several weeks for the milk protein to disappear entirely. The AAP does not currently have an official recommendation on this issue.
After your baby's first birthday, they may begin using cow's milk alternatives or occasionally change to a toddler version of the formulas mentioned above. Many infants diagnosed with allergic colitis caused by cow's milk protein, including healthy babies with rectal bleeding, may safely begin cow's milk at a year or so of age. Your pediatrician can help you make this decision.
What kinds of cow's milk alternatives are available?
While soy milk has traditionally been the most commonly used cow's milk alternative, there are many options available. In addition, soy protein should also be avoided if your child is diagnosed with an allergy to cow's milk protein. This is because 50% of infants with cow's milk protein allergy may also have cross reactivity with the soy protein.
Use of tree nut milk, including almond and cashew milks, have become increasingly popular. Rice and oat milk, as well as hemp milk, are also possible alternatives. Some of these alternatives are flavored, for example with chocolate and vanilla. Keep in mind that these often contain added sugar and calories. It is best to avoid sugar-sweetened beverages for children under 2 years of age, and also limit them for older children as much as possible.
What are the differences among cow's milk alternatives?
Cow's milk alternatives often contain less protein and less calories in comparison to cow's milk. Most are fortified with vitamin D and calcium. It is important to check labels since protein and vitamin content may differ among brands. See the chart for a comparison of common unflavored milk alternatives.
Comparison of common unflavored milk alternatives | ||||||||
|
Whole Milk (1 cup) |
Rice Milk (1 cup) |
Soy Milk (1 cup) |
Coconut Milk (1 cup) |
Almond Milk (1 cup) |
Oat Milk (1 cup) |
Hemp Milk (1 cup) | Pea Milk (1 cup) | |
Energy (kcal) | 149 | 115 | 105 | 76 | 37 | 130 | 70 | 80 |
Protein (g) | 7. | 0.68 | 6.34 | 0.51 | 1.44 | 4 | 3 | 8 |
Total fat (g) | 7.93 | 2.37 | 3.59 | 5.08 | 2.68 | 2.5 | 5 | 4.5 |
Saturated fat (g) | 4.55 | 0 | 0.5 | 5.083 | 0 | 0 | 0.5 | 0.5 |
Cholesterol (mg) | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Carbohydrate (g) | 11. | 22.37 | 12 | 7.12 | 1.42 | 24 | 1 | < 1 |
Calcium (mg) | 276 | 288 | 300 | 459 | 481 | 350 | 300 | 440 |
Iron (mg) | 0.07 | 0.49 | 1.02 | 0.73 | 0.85 | 1.8 | 1.8 | 0 |
Vitamin D (IU) | 128 | 96 | 108 | 96 | 96 | 100 | 100 | 110 |
Note: Homemade almond milk or other homemade milk alternatives do not contain the same number of vitamins, because they are not fortified. | ||||||||
How much dairy is recommended for my child?
Infants' diets primarily consist of dairy to help them meet their caloric needs for growth. In addition, dairy provides enough fat needed for brain and eye development.
At one year, babies should consume approximately 2 servings of dairy per day, or about 16 to a maximum of 24 ounces of whole milk per day. Whole-fat milk is recommended for children at this age, unless there is a family history or risk for obesity or heart disease. Talk with your child's pediatrician about which milk they recommend for your one-year-old child.
Between two and three years old, children should consume 2.5 servings of dairy per day. The AAP recommends that children stay on whole milk until they are two years of age—unless there is a reason to switch to low-fat milk sooner. Whole milk contains approximately 4% milk fat. It may help to gradually switch your child from whole milk to a lower-fat milk.
Therefore, many pediatricians recommend that children get reduced fat (2%) milk for a few weeks before switching them to low fat (1%) or no fat (skim) milk. If your child cannot drink cow's milk, they can meet their dairy requirements by eating yogurt and cheese. However, they may need a vitamin D supplement since not all yogurts are fully supplemented with vitamin D. Talk with your child pediatrician before giving your child any supplements.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age. Here is a breakdown of the recommended dietary allowances (RDA) for calcium and
vitamin D.
Recommended Dietary Allowances for Calcium and Vitamin D | ||
| Age |
Amount of Calcium Per Day |
Amount of Vitamin D Per Day |
0 to 6 months | 200 mg | 400 IU |
7 to 12 months | 260 mg | 400 IU |
1 to 3 years | 700 mg | 600 IU |
4 to 8 years | 1000 mg | 600 IU |
9 to 18 year | 1300 mg | 600 IU |
More information
-
Infant Allergies and Food Sensitivities
- Why Formula Instead of Cow's Milk?
- Where We Stand: Soy Formulas
- Choosing a Formula
- Lactose Intolerance in Infants & Children: Parent FAQs
- Ask the Pediatrician:
My preschooler refuses to drink milk.
What should we do?
- The Use of Soy Protein-Based Formulas in Infant Feeding (AAP Policy Statement)
About Dr. Porto:
Anthony Porto, MD, MPH, FAAP is a board-certified pediatrician and board-certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's
Real Answers, and is the co-author of
The Pediatrician's Guide to Feeding Babies and Toddlers. |
About Ms. Drake:Rachel Drake, MS, RD, CSO, CSP, CDN is a is a registered dietitian-nutritionist practicing in Connecticut. She is a board-certified specialist in pediatric nutrition through the Academy of Nutrition and Dietetics and the former Chair of the Failure to Thrive, Gastroenterology & Allergy specialty group within the
Pediatric Nutrition Practice Group of the Academy of Nutrition and Dietetics. In 2015, Ms. Drake was honored by the Academy of Nutrition and Dietetics as the
Recognized Young Dietitian of the Year for the state of Connecticut. She lives in Connecticut with her husband and young daughter. |
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Best Recipes for Children with Milk Allergies
Cow's milk allergy affects approximately 5% of children. This product contains many components that can potentially cause an allergic reaction, but most often it occurs to cow protein. During the normal process of digestion, food that enters the stomach and then the intestines breaks down into enzymes, which are individually absorbed into the body. The imperfect digestive system of a child is sometimes unable to separate milk into enzymes. This situation creates an allergy to cow protein. It usually affects children between the ages of birth and one and a half years. And, as a rule, the symptoms of cow protein allergy go away on their own when the baby is about five years old. At this time, the functioning of the gastrointestinal tract is getting better, and it begins to produce the necessary substances to resist hostile elements. But sometimes milk intolerance persists for life. It should be noted that cow protein allergy can be true and pseudo-allergy. True implies intolerance by the body of any amount of cow's milk protein. A pseudo-allergy is a condition when an allergic reaction occurs only after the child has “overeaten”, that is, a certain amount of milk enzymes is still normally digested, but the body cannot accept the excess.
Children allergic to cow protein can be given fermented milk products - kefir, fermented baked milk, yogurt, cottage cheese. Enzymes contained in cow's milk break down into components at the time of preparation of the fermented milk product. And already these components the children's body can try to digest. Offer your baby yogurt or cottage cheese, watch his reaction. If symptoms of an allergy to cow protein appear (rash, itching, nausea or vomiting), then the product should be excluded from the diet for the time being.
See also:
- Food intolerance: how it affects weight
Menu for children with milk allergy
Composing a balanced and complete diet for a baby with milk intolerance is not so difficult, although it is a traditional component of most children's meals. And, more importantly, a very valuable food for the child. “Milk is ideal for the ratio of calcium and phosphorus for the construction of the musculoskeletal system,” says Natalya Fadeeva, nutritionist-endocrinologist, MD, author of the book “Is the child overweight?” - It contains more than 90 useful substances: 20 amino acids, 18 fatty acids, 13 vitamins, almost all enzymes found in nature, minerals and milk sugar. So that the body of a child with an allergy to milk does not suffer from a deficiency of the necessary components, the menu will have to be drawn up especially carefully.
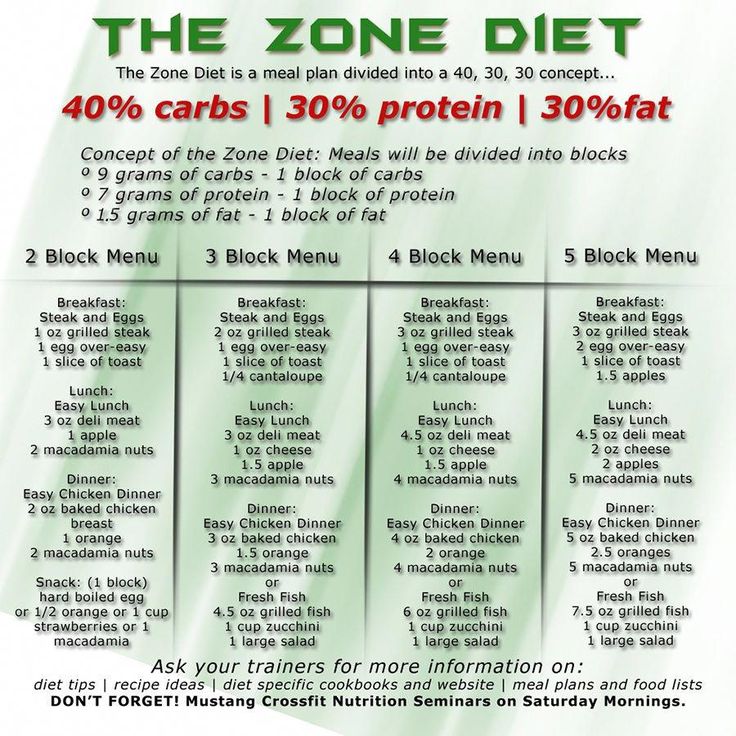
Breakfast
The most popular dishes to start the day are all kinds of cereals: oatmeal, buckwheat, pearl barley, barley, rice, corn, wheat, millet, etc. For children, they are usually boiled in milk or water with milk - it helps absorbed by vegetable proteins of cereals. In our case, you will have to cook only on water (3 parts of water are taken for 1 part of the cereal). Instead of cow's milk, you can try using soy, oat or rice milk. “Choose whole grain cereals, they are healthier: they have a lot of fiber, they are digested more slowly and provide energy for a longer period, so after them there is no feeling of hunger for a long time,” says Natalia Fadeeva. - You can use Hercules flakes instead of whole grain oatmeal, which are boiled for at least 10 minutes. Porridge cooked with water can be served with a small amount of yogurt, cottage cheese, a piece of cheese, or any fermented milk product. Do not replace whole grain cereals with refined products (muesli, cereals, instant cereals). The child quickly gets used to their sweet taste, and it is much more difficult to rebuild it to a less tasty, but much more useful training porridge than to immediately accustom it to the right food. Berries, finely chopped fruits, a small amount of honey or jam will help improve the taste of the dish.
Buckwheat groats
Ingredients: 150 g buckwheat, 175 g cottage cheese (up to 5%), 1 egg, 30 g yogurt 4% fat, 1/2 tsp. salt, 10 g butter.
Manual. Boil crumbly buckwheat porridge, add cottage cheese mashed with egg and salt. Mix everything, put on a greased baking dish and bake in the oven or microwave. Serve with yoghurt. If the dish is intended for lunch, it is good to add a vegetable salad or soup with vegetables to it.
See also:
- Delicious buckwheat: recipes from chefs
Pancakes with nuts
Ingredients: 1 tbsp. soy or rice milk, 2 quail eggs, 1 tbsp. olive oil, 1.5 tbsp. cornmeal, sugar, salt, vanilla to taste. For the filling: 5 walnuts, 1 tsp. jam.
Manual. Whisk the eggs, salt, sugar, milk, butter and vanilla in a blender. Then add flour, stirring constantly. Prepare the filling by grinding nuts in a blender and mixing them with jam. Fry pancakes in a "dry pan" without oil. They should be voluminous. Make an incision in the pancakes and fill with stuffing.
See also:
- Spinach and cottage cheese fritters
- Zucchini pancakes
- Fried potato pancakes
Berry sauce
Ingredients : 290 g of any berries (strawberries, blueberries, blueberries, cranberries, etc.), 1 tbsp. powdered sugar, 1 tbsp. lemon or orange juice.
Manual. Mix all the ingredients, grind with a blender. Serve with cereals and fruit salads.
See also:
- Coolie sauces: recipes from chefs
- Homemade sauces that won't make you fat
Lunch and Dinner
Lunch is the second main meal of the day to give your child the energy they need from noon to evening. The basis of a proper, healthy lunch is soup and a protein dish (fish, poultry or meat). “The soup should be low-fat,” says Natalya Fadeeva. - It is best if it is a vegetable vegetarian soup without meat broth, low-fat vegetable puree soup, low-fat fish soup, soup with meat on the second broth. For the second, you can serve a cutlet, meatballs, casserole, soufflé. For them, lean fish (cod, ice, haddock, pike perch, hake, blue whiting, pollock), lean skinless poultry (chicken, turkey, guinea fowl), lean meat (veal, beef, rabbit) are best suited. A necessary addition to a protein dish for lunch is a starchy side dish, such as, for example, boiled potatoes, brown rice, buckwheat, durum wheat pasta, whole grain bread. You can make vegetable casseroles. An ideal side dish is a combination of a starchy component with thermally processed vegetables or vegetable salad.
In the evening, the body prepares for sleep. “Therefore, you need to have dinner with a sparse, light, non-exciting food,” says Natalya Fadeeva. - For dinner, there must be a protein dish - all the same low-fat fish or poultry. Suitable cottage cheese (up to 5%), eggs. It is better not to give red meat to a child in the evening - it excites and is digested for a long time. As a side dish for dinner, it is best to serve thermally processed vegetables or vegetable salads; you can make casseroles from vegetable and protein components. It is better to do without starch-containing side dishes.
Fruit and vegetable salad
Ingredients: 100 g fresh pumpkin, 1 medium carrot, 1 green apple, 1 tsp. lemon juice, 3 orange slices.
Manual. Grate vegetables and apple on a coarse grater, mix. Add lemon juice and chopped orange slices.
See also:
- Best snacks for diabetics
Lentil soup
Ingredients: 1 st. red lentils, 1.5-2 liters of water, 1 medium onion, 1 medium carrot, 1 stalk of celery (or 50 g root), black peppercorns to taste (5-6 peas), 3-4 bay leaves, 1 parsley root , spices to taste, herbs (dill, parsley).
Manual. Soak the lentils for several hours (or overnight), then rinse thoroughly, cover with cold water and cook over moderate heat. Bring to a boil and add the roots. After five to ten minutes, put chopped onions and grated carrots into the soup, cook over low heat for about 10 minutes. Add bay leaf, pepper and other spices. When the lentils are completely boiled, turn off the heat and let it brew for 5-8 minutes. Salt to taste and serve with finely chopped greens.
See also:
- Turkish Lentil Kyufta
- Red lentil curry with tomatoes
Chicken or turkey breast medallions
Ingredients: 400 g chicken (turkey) fillet, 1 tbsp. lemon juice, 0.5 tsp curry and cumin, 1 tbsp. olive oil, salt to taste.
Manual . Cut the fillet across the fibers into pieces 1-1.5 cm thick. Place in a bowl and season with lemon juice, oil, sauce, curry, cumin and salt. Mix everything thoroughly and leave to marinate for 15 minutes. Put the pieces in a cold, oil-free pan with a thick bottom and cook them under the lid for 20-25 minutes. Serve with vegetables and brown rice.
Fish cutlets
Ingredients: 400 g lean fish fillet (cod, zander, haddock), 1 medium onion, 1 egg, 1 medium potato, spices, herbs to taste.
Manual. Pass the fish fillet twice through a meat grinder. Also grind in a meat grinder (or blender) onions, potatoes, herbs, add an egg, spices, salt. Mix everything thoroughly, form cutlets and cook them in a “dry pan” lightly greased with vegetable oil (you can cook in a double boiler, slow cooker or bake). Serve garnished with chopped herbs.
See also:
- Polenta balls with mushroom garnish
- Carrot cutlets with white yoghurt sauce
- Onion cutlets
Baked apples with cranberries
Ingredients: 5–6 apples (Antonovka is best), 1/2 tsp. cinnamon, 100 g cranberries, 100–150 g water, 1–2 tbsp. Sahara
Manual. For apples, cut off the top with a cone with an indentation. Put lingonberries (can be crushed) inside the fruit, add cinnamon and sugar. Place in a fireproof saucepan, add water and cook over low heat for 15 minutes. If you bake apples in the microwave or oven, you can not add water.
See also:
- 5 Healthy Foods You're Probably Eating Wrong
- Cooking with Kids: 6 Recipes for All Ages
Feeding for Cow's Milk Protein Allergies
- Nestlé Health Science
- health care
- Feeding with CMPA
Feeding and treatment of CMPA
The appearance of allergy symptoms in an infant always causes fear in parents. The first step is to consult a doctor who will conduct an examination, make the correct diagnosis and prescribe competent treatment. With the right approach, most symptoms will disappear within 2-4 weeks.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
Breastfeeding is the best nutritional option for you and your baby. Even if your baby has been diagnosed with CMPA, breastfeeding should continue. Based on the severity of the symptoms and the presence of other types of food allergies in the child, the doctor will help determine the most appropriate diet for your child to quickly resolve the symptoms of the allergy.
Continue breastfeeding
A diagnosis of CMPA should not affect breastfeeding. Breastfeeding is the best nutritional option for your baby. Breast milk contains all the nutrients your baby especially needs during the first 6 months and continues to be beneficial for a long time to come. In addition to nutritional properties, breast milk contains antibodies, leukocytes and immune complexes, which together form the baby's immunity. In rare cases where the baby's immune system reacts to cow's milk proteins in breast milk, your doctor may recommend that you start a diet eliminating cow's milk proteins entirely (remember that a dairy-free diet may not be sufficient, as all traces of cow's milk must be eliminated) .
Early start: The sooner you start breastfeeding, the better. According to doctors, starting breastfeeding within 1 hour of birth ensures that your baby receives first milk (colostrum) and the protective factors it contains as soon as possible.
Emotional Benefit: Breastfeeding is an important factor in establishing and maintaining a strong emotional bond with your baby.
Long-term health benefits: Breastfeeding will also help develop your baby's immune system and thus protect your baby's health in the long term.
Protection for you and your baby: Studies have shown that breastfeeding reduces the risk of further infections in children, digestive diseases, diabetes, obesity and even leukemia. Breastfeeding is also good for you! Mothers who breastfeed have a reduced risk of developing diabetes, as well as breast and ovarian cancer.
Importance and benefits of breastfeeding
The sooner the better
- Breastfeeding during the first hour of birth ensures that the baby receives its first milk, called colostrum
- Exclusive breastfeeding recommended for the first 6 months
Protective role for you and your child
- Breast milk is rich in protective factors that promote healthy growth and development in babies and reduce the risk of developing diseases later on.
- Mothers who breastfeed have a lower risk of developing diabetes and developing breast and ovarian cancer
Emotional Benefits
- You and your child develop and maintain a strong emotional bond.
What type of food is best for my child?
The only way to eliminate symptoms is to eliminate cow's milk proteins from the child's diet.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
If breastfeeding is not possible or supplemented with infant formula, your doctor will help you select an appropriate infant formula that does not contain cow's milk proteins. These infant formulas are formulated with children in mind and contain all the necessary nutrients to support growth and development.
These specialized infant formulas can be based on:
- cow's milk processed in a certain way so that the proteins are no longer recognized by the baby's immune system and therefore do not cause an allergic reaction
- amino acids
The table below describes the differences between the two types of infant formula.
| SOGSB | COA | |
| What is it? | WGHB stands for "Whey Protein Hydrolysate Blend". The proteins in cow's milk that cause allergic reactions in a baby are severely broken down (hydrolyzed). | COA stands for "amino acid blend". This mixture does not contain any cow's milk proteins. |
| What does it consist of? | Cow's milk proteins have been broken down into smaller particles, which means they can no longer be recognized by the baby's immune system. Mixtures contain the macro- and micronutrients necessary for the child. | For severe allergies, an amino acid mixture is used. This mixture does not contain any cow's milk proteins. The mixture is also enriched with all the necessary elements to support healthy growth and development. |
When and how to introduce complementary foods
At 6 months of age, breastfeeding (or special infant formula) is no longer sufficient to fully support a child's growth and development and supplementary foods must be introduced into the diet. But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby.
It is important to introduce complementary foods on time. The reflex responsible for moving solid foods in the mouth and swallowing them usually develops between 4 and 7 months of age. If you start solid foods too early, the baby will not be ready for it. Similarly, if you start too late, your child may not get all the nutritional support he or she needs, which increases the child's risk of developing essential vitamin and mineral deficiencies and stunting. Along with the nutritional benefits, introducing complementary foods will also provide sensory stimulation and improve your baby's motor skills.
IMPORTANT NOTE: : It is possible to continue breastfeeding if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old.