What to feed baby after stomach bug
Gastroenteritis (Stomach Flu) (for Parents)
What Is Gastroenteritis?
Gastroenteritis, often called the stomach flu, is a common illness that causes nausea, vomiting, diarrhea, and belly cramps. It usually lasts a few days and isn't serious. Most kids get better at home by resting and drinking plenty of liquids.
What Causes Gastroenteritis?
Gastroenteritis (gass-troh-en-teh-RYE-tis) happens when germs (viruses, bacteria, or parasites) infect the stomach or intestines, causing inflammation.
In kids, viruses are the most common cause of gastroenteritis. Rotavirus causes many cases of stomach flu in children, but the rotavirus vaccine can help prevent them.
Many of the germs that cause gastroenteritis spread easily. So someone can get sick if they:
- Touch something contaminated and then touch food or their mouth.
- Share food or drinks with someone who is sick.
- Live with someone who’s infected, even if that person isn’t sick.
What Are the Signs & Symptoms of Gastroenteritis?
The most common signs of gastroenteritis are vomiting and diarrhea. Many children also have a fever.
When kids have diarrhea or vomiting, they lose lots of fluid in their poop or vomit. This can lead to dehydration (not having enough water in the body). If that happens, the body can have trouble working as it should.
How Is Gastroenteritis Diagnosed?
Doctors usually can tell if someone has stomach flu by hearing about the symptoms. Usually, no tests are needed. If a child is very sick or has blood or mucus in the poop, doctors might order a stool (poop) test, urine (pee) test, or blood test to check for dehydration and to see what’s causing it.
How Is Gastroenteritis Treated?
There is no specific treatment for gastroenteritis, and most kids can be treated at home. Keep your child hydrated by offering plenty of liquids. Kids with more severe dehydration may need treatment in the ER or hospital.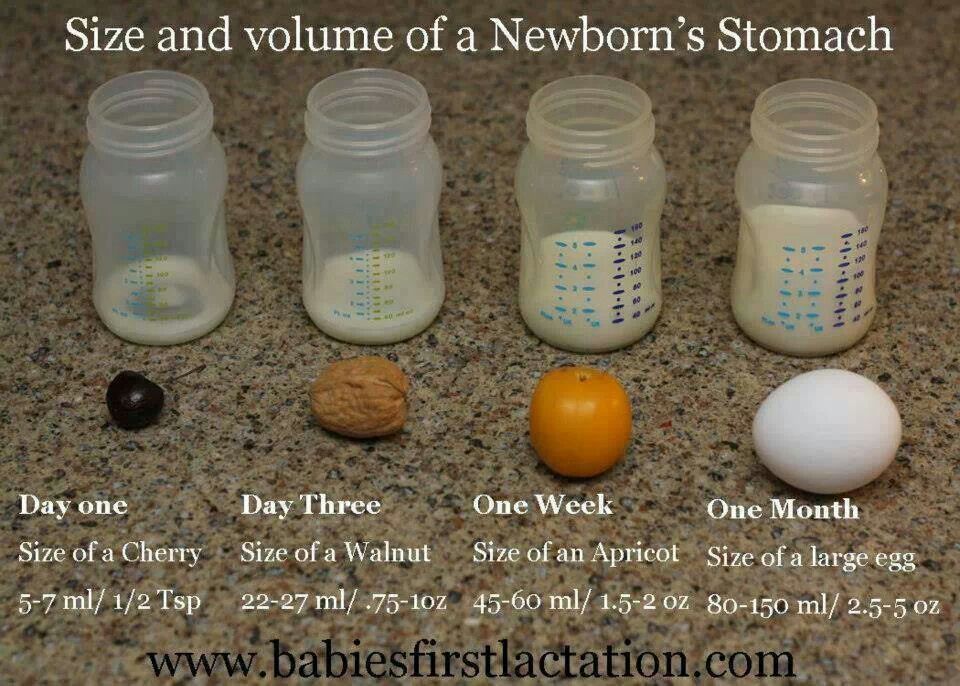
Mild dehydration is treated with oral (by mouth) rehydration. This usually includes giving oral rehydration solution (such as Pedialyte, Enfalyte, or a store brand). It has the right amounts of water, sugar, and salt to help with dehydration. You can buy it without a prescription at drugstores or supermarkets. If you can’t get oral rehydration solution, talk to your doctor.
If your child has mild dehydration and your doctor says it’s OK to start treatment at home:
- Give your child an oral electrolyte solution as often as possible. If your child throws up, start with small sips, about 1 or 2 teaspoons every few minutes.
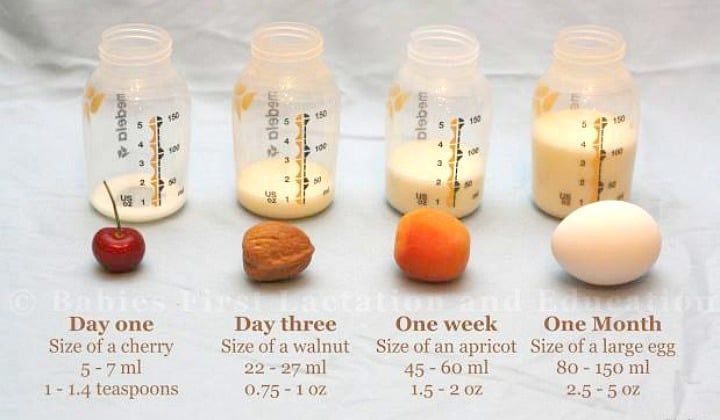
- Babies can continue to breastfeed or take formula as long as they are not throwing up repeatedly.
- Don't give babies plain water instead of oral rehydration solution. It doesn't have the right nutrients for babies with dehydration.
- Older children can have frozen electrolyte popsicles.
- Do not give your child full-strength juice (undiluted), soda, or sports drinks.
 These have a lot of sugar, which can make diarrhea worse.
These have a lot of sugar, which can make diarrhea worse.
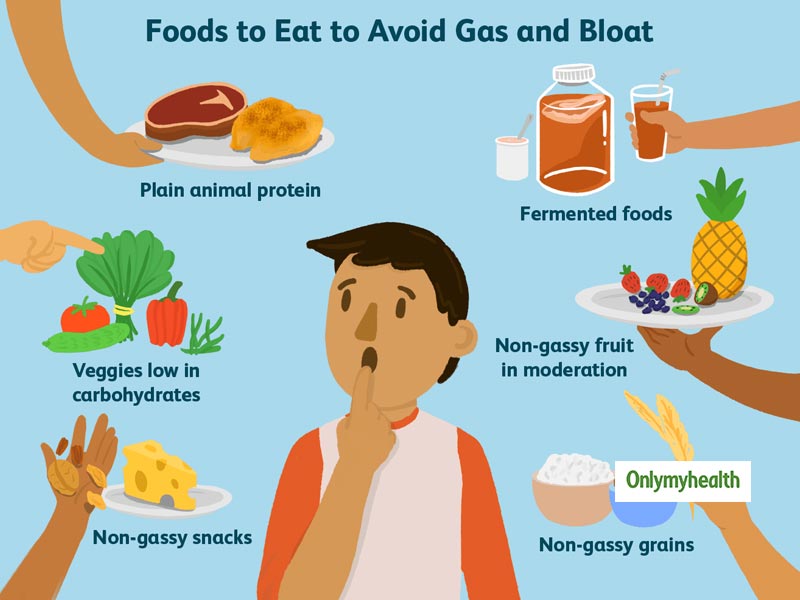
When your child stops vomiting, you can offer small amounts of solid foods, such as toast, crackers, rice, or mashed potatoes. Yogurt, fruits, vegetables, and lean meat, like chicken, are also OK.
A child who isn’t throwing up can eat a regular diet, if they feel up to it. It may take time for them to feel like eating. There's no need to avoid dairy unless it makes the vomiting or diarrhea worse. Avoid fatty foods, which can make diarrhea worse.
To help your child feel better, let your child rest as needed. You can give medicine for fever or pain, like acetaminophen or ibuprofen (do not give ibuprofen to babies under 6 months old), if your doctor says it’s OK. Follow the package directions for how much medicine to give and how often. Don't give aspirin to your child or teen. It's linked to a rare but serious illness called Reye syndrome.
Don't give medicines for diarrhea or vomiting unless your doctor tells you to.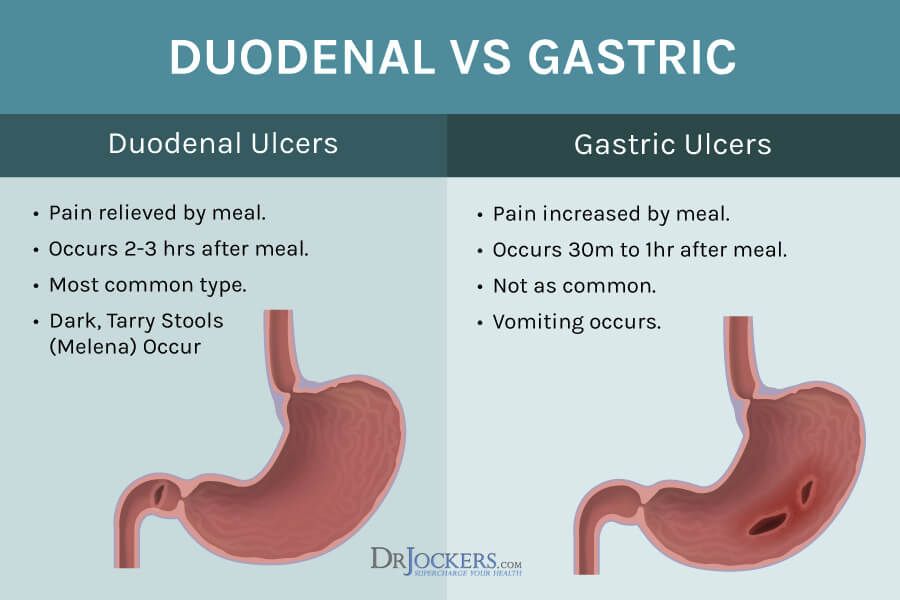
Keep your child out of school or childcare until 24 hours without vomiting or fever and diarrhea has improved. Your child also should stay out of swimming pools until all symptoms have stopped.
When Should I Call the Doctor?
Call the doctor if your child:
- can’t drink for several hours
- is peeing less often (more than 4–6 hours for babies and 6-8 hours for older children)
- has signs of dehydration, such as crying with few or no tears, having a dry mouth or cracked lips, feeling dizzy or lightheaded, acting very sleepy or less alert
- has a high fever
- has blood in their poop or vomit
- is vomiting for more than 24 hours or the diarrhea doesn’t get better after several days
Can Gastroenteritis Be Prevented?
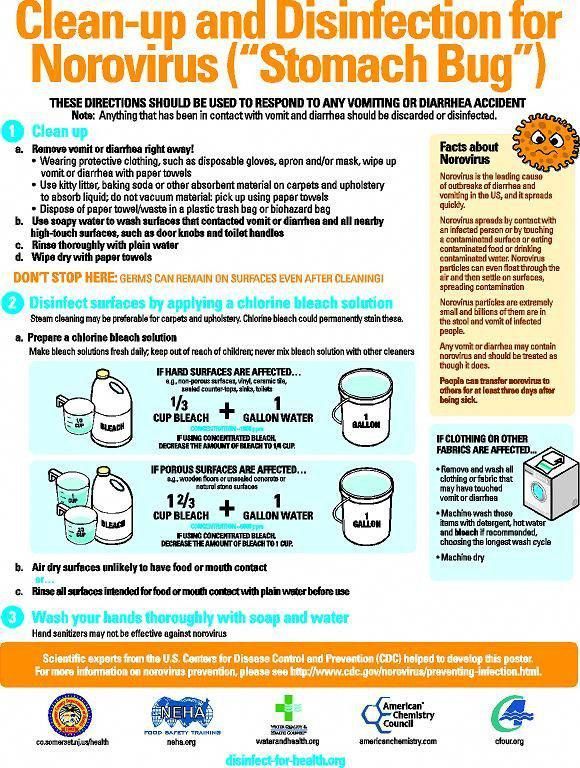
Germs that cause gastroenteritis are contagious. The best way to avoid the illness is to keep the germs from spreading:
- Teach all family members to wash their hands well and often.
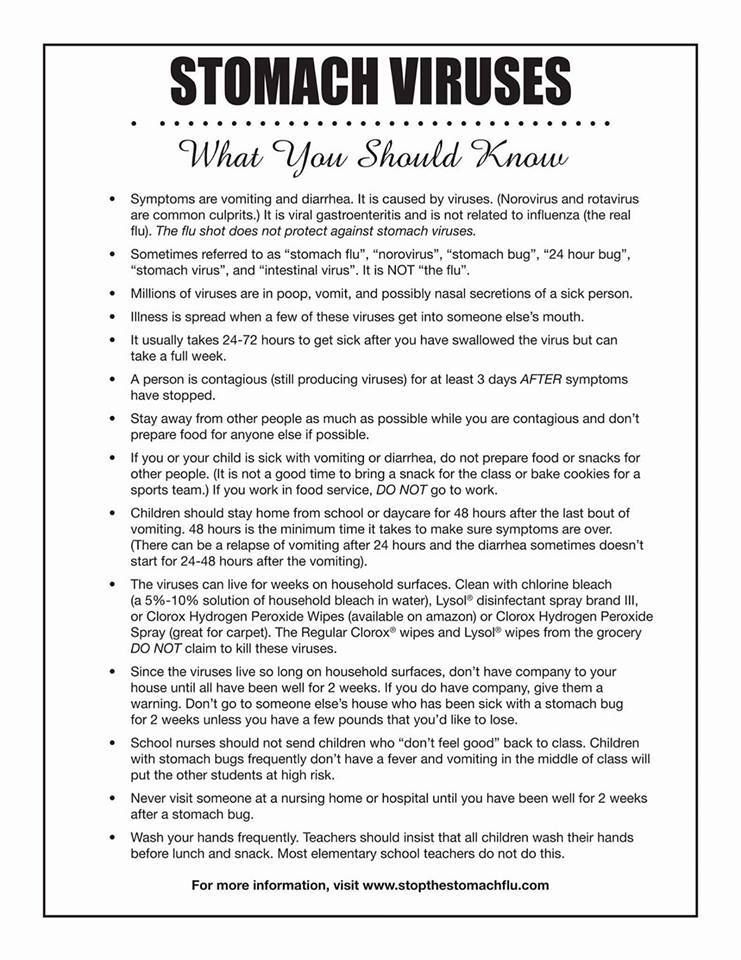 They should wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food.
They should wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food. - Clean tabletops, doorknobs, and other surfaces that get touched a lot with a cleaner that kills viruses.
- Follow food safety guidelines to prevent bacteria and viruses from getting into food and drinks (food poisoning).
- Make sure your kids get all recommended immunizations on time.
Reviewed by: Mary L. Gavin, MD
Date reviewed: September 2021
Symptoms and Treatment for Stomach Flu
What causes vomiting and diarrhea?
Vomiting (throwing up) and diarrhea (frequent, watery bowel movements) can be caused by viruses, bacteria and parasites. Foods that are hard to digest (such as too many sweets) and undercooked (still partially raw) meat or fish can also cause vomiting and diarrhea.
Can vomiting and diarrhea be dangerous for children?
Vomiting and diarrhea can be harmful because they can cause dehydration. Dehydration occurs when you lose too much fluid. Young children can become dehydrated quickly, but dehydration can occur at any age.
Dehydration occurs when you lose too much fluid. Young children can become dehydrated quickly, but dehydration can occur at any age.
Schedule a telehealth appointment
Stomach flu and dehydration
How can I prevent dehydration?
If your baby or child has had several bouts of vomiting or diarrhea, he or she will need to replace lost fluids and electrolytes.
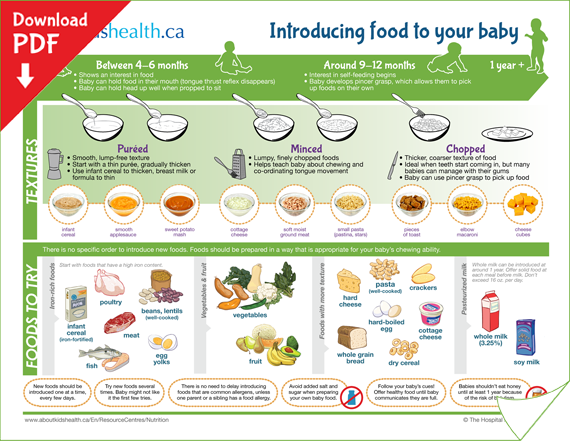
If you are breastfeeding, continue to give your baby breastmilk. Breastmilk has fluids and electrolytes needed to prevent dehydration. Your doctor may also want you to give your baby an oral rehydration solution (ORS).
If you feed your baby formula, try switching to one that is lactose free while your baby is sick. Lactose can make diarrhea worse. Your doctor may also suggest switching from formula to an ORS for 12 to 24 hours, and then switching back.
For toddlers and young children, use an ORS, which contains the right mix of salt, sugar, potassium and other nutrients to help replace lost body fluids. Children older than 1 year may also have clear soups, clear sodas or juice mixed with water to help prevent dehydration. You should avoid giving your child plain water and dark sodas. Water alone does not contain enough salt and nutrients to help with dehydration. Dark sodas are typically very high in sugar and can irritate your child’s stomach.
Children older than 1 year may also have clear soups, clear sodas or juice mixed with water to help prevent dehydration. You should avoid giving your child plain water and dark sodas. Water alone does not contain enough salt and nutrients to help with dehydration. Dark sodas are typically very high in sugar and can irritate your child’s stomach.
- Little or lack of urine, or urine that is darker than usual
- Urinating less frequently than usual (fewer than 6 wet diapers a day for infants and 8 hours or more without urinating for children)
- Thirst (babies may show thirst by crying, being irritable and eager to drink when something is offered)
- Irritability
- Not eating as well as usual
- Weight loss
- Dry mouth
- No tears when crying
- In babies who are younger than 18 months old, sunken soft spots on the top of their heads
- Skin that isn’t as springy or elastic as usual
- Sleepiness
An oral rehydration solution, or ORS, is a great way to replace fluids and nutrients lost through vomiting and diarrhea. An ORS is safe for babies and older children. An ORS can come in several forms, including a powder that you mix with water, a liquid that is already mixed and as frozen popsicle
An ORS is safe for babies and older children. An ORS can come in several forms, including a powder that you mix with water, a liquid that is already mixed and as frozen popsicle
Brands of ORS include Pedialyte, Ricelyte, Rehydralyte and the World Health Organization’s Oral Rehydration Solution (WHO-ORS). You can purchase these at most grocery stores and drugstores. If you don’t have access to store-bought ORS, you can mix 8 teaspoons of sugar and 1 teaspoon of salt in a quart (4 cups) of water. This mixture lacks potassium but is otherwise a good ORS. You can supply some potassium by adding a cup of orange juice to your homemade ORS or feeding your child some banana.
If your child is vomiting, try giving him or her small amounts of an ORS often, such as 1 teaspoonful every minute. When your child is able to keep the drink down, slowly increase how much you give.
If your child keeps vomiting, wait 30 to 60 minutes after the last time he or she vomited, and then give him or her a few sips of an ORS. Small amounts every few minutes may stay down better than a large amount all at once.
Small amounts every few minutes may stay down better than a large amount all at once.
When your child stops vomiting, you may increase how much of the ORS you give each time and add clear broths or clear sodas. Remember, small amounts are less likely to upset your child’s stomach.
If your child has diarrhea and isn’t vomiting, give him or her an ORS and other liquids. Your doctor may ask you to keep track of how much your child drinks. You can use a dropper, a spoon or a measuring cup to help you keep track.
Should I feed my child when he or she has diarrhea?Yes. Older children should begin eating within 12 to 24 hours after starting to take an ORS. Avoid foods with a lot of sugar and fat, such as ice cream, gelatin, pudding and fried foods. These may irritate your child’s stomach and digestive tract. It’s best to avoid dairy products for 3 to 7 days.
Your doctor may recommend that you give your child bland foods for the first 24 hours.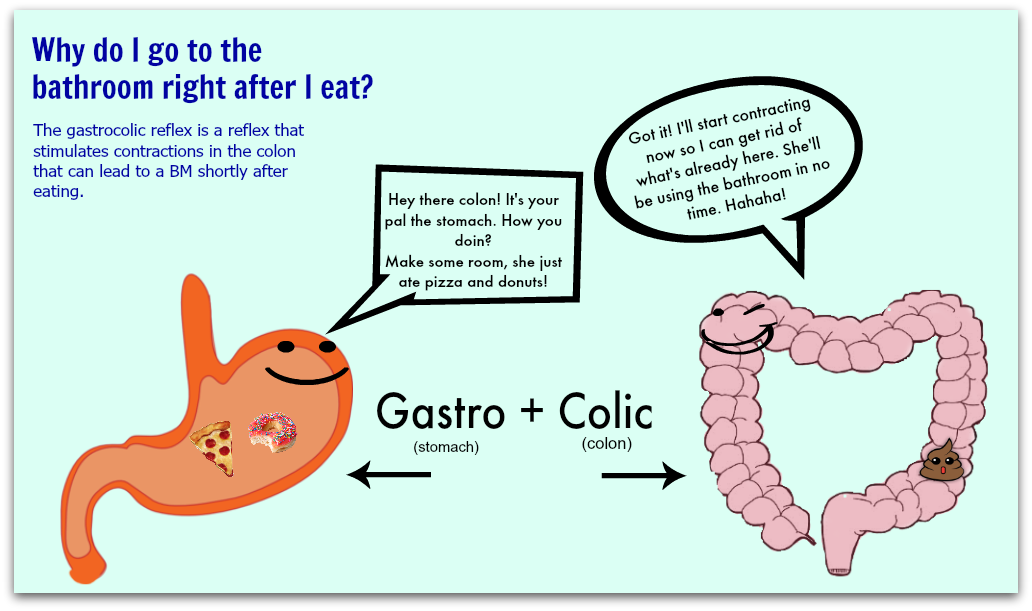 Bland foods include bananas, rice, applesauce, toast, saltine crackers and unsweetened cereals. If your child does well with these foods, you can add other foods over the next 48 hours.
Bland foods include bananas, rice, applesauce, toast, saltine crackers and unsweetened cereals. If your child does well with these foods, you can add other foods over the next 48 hours.
Most children can return to their usual diet about 3 days after the diarrhea stops. If your child has been vomiting, wait 6 hours after the last time he or she vomited before offering food. Try offering small amounts of bland foods. Do not force your child to eat. Your child may not feel very hungry for a few days after vomiting.
Should I give my child medicine to stop diarrhea?Probably not. Diarrhea usually doesn’t last long. If it’s caused by an infection, diarrhea is a way for the body to get rid of the infection. Giving medicines that stop diarrhea may actually interfere with the body’s efforts to heal. Antibiotics are usually not necessary either. Talk to your family doctor if you think your child needs medicine.
Will my child need to go to the hospital?Probably not, unless dehydration becomes severe.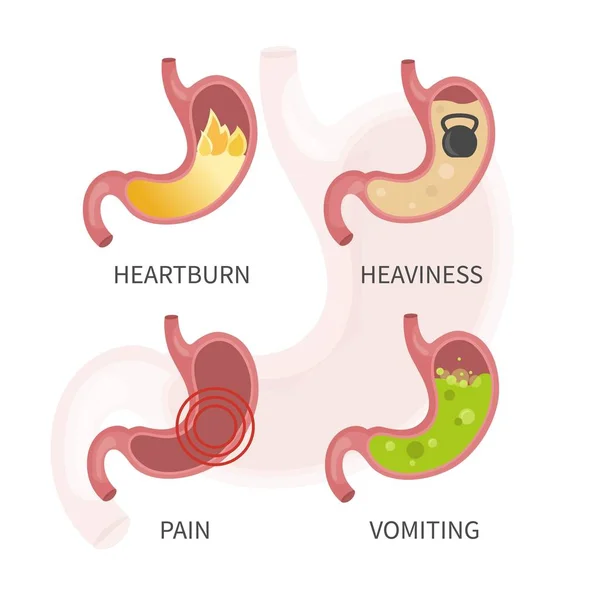 In this case, your child may need to be given fluids intravenously (through an IV) to replace fluids lost through vomiting or diarrhea. Call your doctor if you notice any of the signs in the box below.
In this case, your child may need to be given fluids intravenously (through an IV) to replace fluids lost through vomiting or diarrhea. Call your doctor if you notice any of the signs in the box below.
Call your doctor if your child is vomiting or has diarrhea and:
- Is younger than 6 months old.
- Is older than 6 months old and has a fever higher than 101.4°F.
- Has signs of dehydration (see box above).
- Has been vomiting longer than 8 hours or is vomiting with great force.
- Has blood in his or her stools.
- Has blood in his or her vomit.
- Has not urinated in 8 hours.
- Might have swallowed something that could be poisonous.
- Has a stiff neck.
- Is listless or unusually sleepy.
- Has had abdominal pain for more than 2 hours.
Vomiting and diarrhea may be caused by foods that are hard for your child to digest (such as sugar or by bacteria in undercooked meat). Make sure your child eats a healthy diet.
Make sure your child eats a healthy diet.
Most infections that cause diarrhea are caused by a virus found in feces. Help prevent infection by disposing of dirty diapers properly and by washing your hands after changing a diaper or going to the bathroom. Make sure your child washes his or her hands frequently, especially after going to the bathroom.
Schedule a telehealth appointment
Source
Written by familydoctor.org editorial staff. American Academy of Family Physicians
Diet for peptic ulcer | Sanatorium Gorny
Peptic ulcer of the stomach and duodenum is a disease in which the mucous membrane is affected with the formation of defects on it (ulcers). Treatment of gastric ulcer should be carried out in a complex way: therapeutic nutrition + drug therapy. The basic principle of nutrition in gastric ulcer is to exclude products that irritate the mucous membrane.
General rules. duration of the diet.
With an exacerbation of the disease, diet No. 1 should be followed. And when the symptoms subside, you can switch to diet number 5
1 should be followed. And when the symptoms subside, you can switch to diet number 5
Nutrition for gastric and duodenal ulcers consists of several important rules:
- A certain way of preparing food. Food can be baked without a crust, boiled, stewed.
- The number of meals should be at least 5-6 times a day. The volume of food is not more than 200 ml per 1 meal.
- Food should be warm (32-38 C), not hot or cold.
- Meals must be nutritious and balanced in nutrients.
- Drinking mode. The amount of fluid drunk per day should be at least 2 liters of fluid.
- Do not eat food that irritates the mucous membrane, as well as carbonated drinks.
- Minimize salt intake
The diet must be followed even in the case of a long remission. Any violations in nutrition can lead to an exacerbation of the disease and the development of complications.
Nutrition for an ulcer during an exacerbation:
During the period of exacerbation of the disease, it is necessary to follow a strict diet. Food should have enveloping properties. Dishes are best boiled or steamed. Food should be ground to a gruel or served in the form of mashed potatoes. The number of meals should be increased.
Food should have enveloping properties. Dishes are best boiled or steamed. Food should be ground to a gruel or served in the form of mashed potatoes. The number of meals should be increased.
Notice! An ulcer during an exacerbation is a contraindication for spa treatment: it is better to go to a hospital.
If you have a chronic form, then you should regularly carry out preventive treatment .
Nutrition for chronic peptic ulcer:
With peptic ulcer, proper nutrition is a fundamental condition for recovery and stable remission.
The diet should be selected by the attending physician, taking into account individual characteristics, concomitant diseases, stage of the disease, age and body weight of the patient.
For all patients suffering from peptic ulcer in remission, when compiling the menu, certain rules are followed:
- Complete exclusion from the diet of foods that irritate the mucous membrane.
- Fractional meals 5-6 times a day in small portions
- Last meal 2 hours before bedtime. You can drink warm milk before going to bed
- In the case of persistent and prolonged remission, it is possible to switch to a zigzag diet under the supervision of the attending physician.
Nutrition after surgery:
- A special diet must be followed in the early postoperative period. For the adaptation of the stomach, the first three days after the operation, you can not eat.
- On the 4th and 5th day, doctors allow you to drink sweetened herbal tea, berry jelly.
- In the future, the diet can be expanded. You can eat vegetable soups in the form of mashed potatoes, cereal milk porridge.
Diet types:
For stomach ulcers, table number 1 is prescribed:
- 1A - a strict diet that is prescribed during an exacerbation of the disease or in the postoperative period. Fractional nutrition 6-7 times a day with puree-like food.

- 1B - less stringent than 1A. A mushy consistency of dishes is allowed. The number of meals is 5-6 times a day.
List of approved products:
| Lean meats | Ideyka, chicken, veal, rabbit meat |
| fish | Low-fat varieties of fish, preferably river or lake fish |
| Bread and pastries | It is permissible to eat wheat bread of the day before. Unsweetened cookies, croutons without additives, biscuit. |
| Dairy | Lean cheese, low-fat cottage cheese, yogurt and fermented baked milk |
| Vegetables | Carrots, potatoes, cauliflower, zucchini, pumpkin, boiled greens |
| Fruit | Apples and pears, peeled and baked |
| Cereals in the form of porridge | Buckwheat, oatmeal, semolina, rice |
List of fully or partially restricted products:
| Foods rich in fiber | Mushrooms, legumes, wholemeal bread, fresh bread, rye bread |
| Fatty meats | Pork, lamb, duck, goose, game |
| Spreads, cooking oil, margarine | Irritate the mucous membrane |
| Spicy and salty dishes | May exacerbate disease |
| Sour and unripe fruits and berries | Oranges, tangerines, lemon, kiwi, currants, grapes |
| Dairy products | Whey, fatty dairy products and dairy products with high acidity |
Nutrition menu for peptic ulcer.
 Diet.
Diet. Proper nutrition for gastric and duodenal ulcers is a guarantee of health and the possibility of a long-term remission of the disease.
It is necessary to follow a daily diet:
- Fractional frequent meals
- Eating only warm food
- Portions should be small
- Reduce salt in meals
- Cooking is best steamed or boiled. Grind food
- Drink enough water without gas.
Diet recipes for peptic ulcer:
Breakfast: Buckwheat porridge with milk. Rosehip decoction.
Second breakfast: steam omelet. Baked pear.
Lunch: Vegetable soup with chicken meatballs. Mashed potatoes with boiled fish (perch). Herbal tea
Snack: low-fat yogurt. Galette cookies. Apple compote.
Dinner: rabbit, potato and cauliflower casserole
Before going to bed you can drink a glass (more than 200 ml) of warm milk
Dietitian comments:
Diet for peptic ulcer plays an important role in the treatment of ulcers.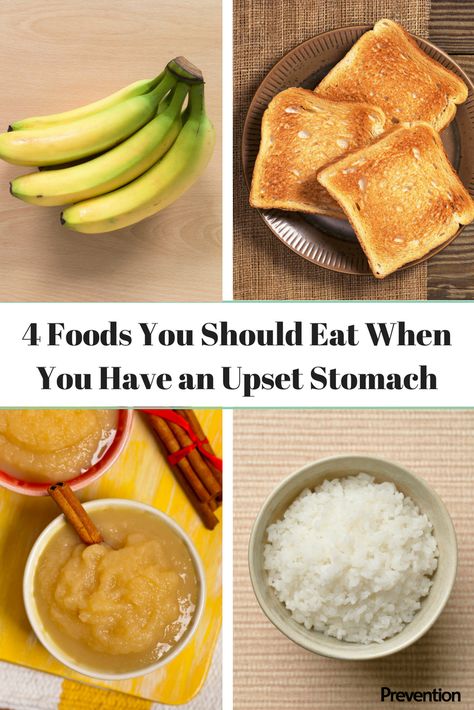 A properly composed menu makes it possible to eat tasty and healthy food, which will also be useful for the entire digestive tract.
A properly composed menu makes it possible to eat tasty and healthy food, which will also be useful for the entire digestive tract.
“The right choice of a sanatorium is a significant step towards the preservation and enhancement of health. "Gorny" is a resort complex that combines the experience and knowledge of Russian and Soviet balneology. The availability of modern medical equipment and innovative installations, the professionalism of the staff and love for their work will serve as a guarantee for extending longevity," - the head doctor of the sanatorium Karaulov Alexander Olegovich.
do's and don'ts, menu for the week
In the modern rhythm of life, we completely forget about proper nutrition. But it is of particular importance when stomach problems have already appeared. What can and what absolutely can not be eaten with a stomach ulcer? We analyze recipes for delicious dietary dishes together with an expert.
Marina Perekalina
head of the gastroenterology department of the Stavropol Regional Clinical Hospital, Candidate of Medical Sciences, chief freelance gastroenterologist of the Ministry of Health of the Stavropol Territory
What is a stomach ulcer?
Basic diet rules for stomach ulcers
What can you eat with stomach ulcers?
What can not be eaten with a stomach ulcer?
Diet menu for ulcers
Recipes for delicious and dietary meals
Main myths about the diet for ulcers
Conclusion
What is a stomach ulcer?
When several unfavorable factors add up, defects appear in the stomach wall. This is how such a chronic disease as a stomach ulcer is formed.
This is how such a chronic disease as a stomach ulcer is formed.
In the process of the disease, other organs of the digestive system can be affected: often ulcers form not only in the stomach itself, but also in the duodenum. Some studies suggest that duodenal ulcers are four times more common than gastric ulcers. The spread of a stomach ulcer can lead to life-threatening complications. As a rule, with an ulcer, periods of exacerbation alternate with periods of remission.
Gastric and duodenal ulcers are similar in many ways in terms of causes and symptoms. Therefore, experts often combine these diseases and talk about gastric and duodenal ulcers . Read more about this disease and the causes of its occurrence in the material "Stomach ulcer: causes and main symptoms " .
Diet guidelines for stomach ulcers
Of course, dietary nutrition will not solve all problems in the treatment of the disease. However, proper nutrition can greatly help when combined with medication and physical therapy. For this, a number of requirements must be taken into account.
However, proper nutrition can greatly help when combined with medication and physical therapy. For this, a number of requirements must be taken into account.
First of all, feeding the patient should be carried out in small portions, fractionally. Meals should be more frequent than usual - 6-7 times a day strictly according to the schedule , without long breaks and subsequent overfeeding.
Among food products, you need to choose those that do not affect the secretory activity , have a "quenching" effect on the acidity of the stomach. Food irritants are strictly prohibited. All foods that sharply increase acidity (containing extract substances), difficult to digest (with fiber) should be excluded from the patient's diet.
What can you eat if you have a stomach ulcer?
Cooking and cooking boiling, use of double boilers, stewing is allowed when expanding the dietary list of dishes in the remission stage.
What is allowed to eat with peptic ulcer?
Dairy products
First of all, milk, cream, kefir, non-acidic cottage cheese and sour cream are allowed for “ulcerers”. For ulcer patients, cow's milk is one of the most useful products, containing many essential substances. If you do not like milk, then try to add it to coffee or tea, or drink it in small portions.
Bread
You have to be careful here. For ulcer sufferers, any bread will not do. It must be dried or stale. It can be crackers or lean pastries.
Vegetables
Ulcer sufferers would benefit from making something out of vegetables, such as a vegetarian soup. Vegetables such as potatoes, carrots, pumpkin, zucchini, non-acidic tomatoes are allowed.
Berries and fruits
Berries and fruits without hard shells are suitable, such as strawberries, strawberries, apples (without skin) and bananas. And also various sweet fruit and berry compotes and kissels, mousses and jelly are allowed.
Sweet
For sweets, you can eat marshmallows and fruit-based marshmallows.
Beverages
Non-carbonated water, non-acidic juices diluted with water, and rosehip decoction or wheat bran decoction are allowed. Decoctions have a beneficial effect and treat the stomach.
Lean meats and fish, eggs
Chicken, beef, rabbit meat may be boiled or steamed. The same cooking methods can be applied to lean river fish. Soft-boiled chicken eggs, steamed omelet can also be added to the diet.
Porridges
For patients with ulcers, you can prepare porridges from soft cereals boiled in milk or water. Suitable cereals such as rice, oatmeal, buckwheat and semolina.
What can not be eaten with a stomach ulcer?
It must be remembered that with such a serious illness fried, smoked and pickled foods, as well as pickles are strictly prohibited.
It is necessary to exclude from the diet products that increase the release of hydrochloric acid.
Spicy foods, pickles, smoked products
Horseradish, mustard, various sauces, preserves, dressings and spicy preserves, smoked meats will have to be excluded from the menu. This also includes canned and pickled foods, including home-cooked foods
Fried foods
Fried foods are prohibited for patients with stomach ulcers in any form.
Bread
Rye bread, rich or puff pastries are forbidden in patients with ulcers. It is undesirable to use fresh bread in principle.
Vegetables
Patients with ulcers should not eat hard vegetables that contain a lot of fiber. Fresh vegetables with a rough skin will have to be excluded from your menu.
Berries, fruits and nuts
Fresh sour berries are forbidden in patients with stomach ulcers. Hard-skinned fruits and berries are prohibited. Some dried fruits should also be excluded from the diet: dried apricots, raisins, figs and dates. We'll have to give up and seeds with nuts.
Some dried fruits should also be excluded from the diet: dried apricots, raisins, figs and dates. We'll have to give up and seeds with nuts.
Sweet
Ice cream and chocolate should disappear from the menu of a patient with a stomach ulcer.
Drinks
Soda, kvass and strong coffee must be excluded from drinks. Sour juices and fruit drinks are banned. And, of course, alcohol in any form is prohibited for patients with an ulcer.
Fatty fish and meats
Fatty meats (such as pork, lamb, poultry skins, lard and layers of fat) will need to be eliminated from your diet. Under the ban and broths from them for soup, decoctions. We will have to give up sausages, sausages, sausages.
Cereals
Legumes: peas, lentils and beans should also be banned. We'll have to forget about cereals from "hard" cereals: millet, pearl barley, corn. It is undesirable to use undercooked pasta.
Diet menu for ulcers
Mechanical sparing is achieved by grinding, boiling and processing products to a liquid state. The list of dishes in the daily menu depends on the stage of the disease, which is determined by the attending physician.
The list of dishes in the daily menu depends on the stage of the disease, which is determined by the attending physician.
In accordance with the classification of dietary tables according to Pevzner, depending on the complication of the ulcer, the patient will be able to eat dietary tables No. 1A, 1B and No. 1. The differences lie in the degree of sparing of the stomach and intestines.
Diet No. 1A is prescribed for the first few days (from 7 to 10 days). It eliminates all irritating factors as much as possible.
Diet No. 1B is considered a transitional form of nutrition. It is needed to replenish the body with useful substances and energy.
Diet №1 can be eaten outside the period of complications. It is as close as possible to the common table, but retains restrictions.
As a rule, the result of the diet is relief of abdominal pain and normalization of the stomach. It is advisable to avoid hard peel on fruits, large pieces of food - it will be difficult for the stomach to digest them. It is advisable to dilute juices with water, and replace sugar with honey. Salt should be added to food as little as possible.
It is advisable to avoid hard peel on fruits, large pieces of food - it will be difficult for the stomach to digest them. It is advisable to dilute juices with water, and replace sugar with honey. Salt should be added to food as little as possible.
When dieting, food temperature is very important : foods that are too cold or too hot should not be eaten. The temperature of food should approach 38 degrees: this way it will be better absorbed.
May be moderately added to food butter and vegetable oil . Oils, like animal fats, provide faster healing of stomach and intestinal ulcers.
Recipes for tasty and healthy meals
Multi-cooker chicken with vegetables
Ingredients:
- 9001 1 chicken breast
- carrots - 1 pc.
- marrow - 1 pc.
- frozen cauliflower - 1 package (or 300 g fresh)
- vegetable oil - 2 tbsp.
- salt
- thyme
Cooking steps:
- Peel carrots and courgettes. Cut them into cubes.
- Switch on the multicooker in the "frying" or "baking" mode. Slightly fry the vegetables, avoiding the appearance of a crust.
- Add cabbage, broken into florets.
- Cut the chicken into cubes, season with salt. Add to vegetables.
- Sprinkle dried herbs over vegetables.
- Pour in a glass of water.
- Switch on the extinguishing mode.
- Simmer for approx. 1.5 hours.
Potato and pumpkin soup
Ingredients:
- potatoes - 2 pcs.
- pumpkin - 120 g.
- cream - 2 tbsp.
- greens
- salt
Cooking steps:
- Boil pumpkin and carrots in a little water.

- Pass the prepared vegetables through a sieve and mix with the remaining vegetable broth.
- Add salt and cream.
- Return to heat and bring to a boil.
- Sprinkle with herbs before use.
steam cutlets
Ingredients:
- non -fat meat - rabbit, beef, turkey or chicken) - 100 g.
- Pshenichnoye
- Pshenichnoye
- olive 1 tsp
- water or milk - 15 ml
- salt
Preparation steps:
- Pass the meat through the meat grinder several times until smooth.
- Add olive oil, salt and bread soaked in water to the minced meat.
- Place the cutlets in a water bath for 40 minutes. You can use a steamer.
- Boiled rice, mashed potatoes or mashed vegetables are a good garnish.
Mannered pudding with pears
Ingredients:
- Sunny cereal - 1 cup
- 11 Milk - 3 cups
- 1 cup of sugar - 1 cup of glass
- sweet pears - 5-6 pcs.
- vanillin
- 3-4 eggs - 3-4 pcs.
- butter - 2 tbsp.
Cooking steps:
- Boil the milk, skim off the foam.
- Pour the sifted semolina into the milk.
- Add vanilla.
- Boil the porridge until it thickens. Add oil.
- Mash egg yolks with sugar and add to hot porridge.
- Slice the pears and add to the porridge.
- Whisk the egg whites into a strong foam, add to the porridge.
- Place the pudding in a saucepan or greased dish.
- Boil in a water bath for half an hour.
We have prepared something useful for you (in every sense prepared and in every sense useful).
Together with the chef we will try to prove that tasty, easy to prepare and healthy is not always about different food.
Key Ulcer Diet Myths
Myth #1: Ulcers Cause Improper Diet
Improper diet alone cannot cause ulcers. Of course, fried, spicy and fatty foods do not harm our body. But only this factor cannot become the cause of an ulcer.
Of course, fried, spicy and fatty foods do not harm our body. But only this factor cannot become the cause of an ulcer.
Myth #2: Baking soda helps with pain
It was once common to use baking soda for pain. You can't do that. At first, soda really reduces pain. But later they become even stronger, because soda has a leavening effect. At the same time, food in general relieves pain, even if it is ordinary water. Milk will also help.
Myth #3: Diet can cure an ulcer
Alas, diet alone cannot help cure the disease. Especially if it is provoked by an infection. This requires drug therapy. But in the complex, the diet can provide an invaluable service for stomach ulcers.
Conclusion
Strictly adhering to the menu, which includes only permitted foods for ulcers, you can defeat the disease.