What to feed baby for first time
Feeding Your 4- to 7-Month-Old (for Parents)
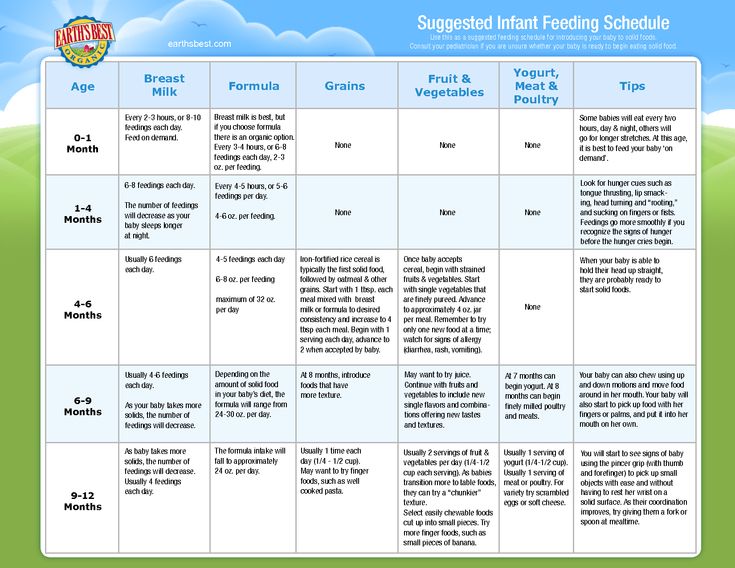
Most babies this age are ready to try solid foods. Experts recommend starting solid foods when a baby is about 6 months old, depending on the baby's readiness and nutritional needs.
Be sure to check with your doctor before giving any solid foods.
Is My Baby Ready to Eat Solid Foods?
How can you tell if your baby is ready for solids? Here are a few hints:
- Does your baby swallow food or push it out of their mouth? Babies have a natural tongue-thrust reflex that pushes food back out. Wait until this reflex disappears (typically when babies are 4–6 months old).
- Can your baby support their own head? To eat solid food, an infant needs good head and neck control and should be able to sit up.
- Is your baby interested in food? Babies who stare, reach and grab, and open their mouths for food are ready to try solid foods.
If your doctor gives the go-ahead but your baby seems frustrated or uninterested in solid foods, try waiting a few days before trying again. Breast milk and formula will still meet nutritional needs as your baby learns to eat solid foods. But after 6 months, babies need the added nutrition — like iron and zinc — that solid foods provide.
Do not add cereal or other food to your baby's bottle because it can lead to too much weight gain.
Watch for signs that your child is hungry or full. Respond to these cues and let your child stop when full. A child who is full may suck with less enthusiasm, stop, or turn away from the breast or the bottle. With solid foods, they may turn away, refuse to open their mouth, or spit the food out.
How Should I Start Feeding My Baby Solid Foods?
When your baby is ready and the doctor says it’s OK to try solid foods, pick a time of day when your baby is not tired or cranky. You want your baby to be a little hungry, but not so hungry that they’re upset. So you might want to give your baby a little breast milk or formula first.
Have your baby sit supported in your lap or in a high chair with a safety strap.
Most babies' first food is iron-fortified infant single-grain cereal mixed with breast milk or formula. Place the spoon near your baby's lips, and let the baby smell and taste it. Don't be surprised if this first spoonful is rejected. Wait a minute and try again. Most food offered to your baby at this age will end up on the baby's chin, bib, or high-chair tray. Again, this is just an introduction.
When your little one gets the hang of eating cereal off a spoon, it may be time to try single-ingredient puréed meat, vegetables, or fruit. The order in which you give them doesn't matter, but go slow. Offer foods that are high in iron and zinc — such as meat, poultry, eggs, and beans — especially if your baby is breastfeeding. Try one food at a time and wait several days before trying something else new. This will let you identify any foods that your baby may be allergic to.
Which Foods Should I Avoid?
Foods that are more likely to cause allergies can be among the foods you introduce to your baby. These include peanuts, eggs, cow’s milk, seafood, nuts, wheat, and soy. Waiting to start these foods does not prevent food allergies. Talk to your doctor if you’re concerned about food allergies, especially if any close family members have allergies, food allergies, or allergy-related conditions, like eczema or asthma.
These include peanuts, eggs, cow’s milk, seafood, nuts, wheat, and soy. Waiting to start these foods does not prevent food allergies. Talk to your doctor if you’re concerned about food allergies, especially if any close family members have allergies, food allergies, or allergy-related conditions, like eczema or asthma.
Infants with severe eczema or egg allergies are more likely to have allergies to peanuts. Talk to your doctor about how and when to introduce these foods to your child.
Possible signs of food allergy or allergic reactions include:
- rash
- bloating or an increase in gassiness
- diarrhea
- vomiting
Get medical care right away if your baby has a more severe allergic reaction, like hives, drooling, wheezing, or trouble breathing.
If your child has any type of reaction to a food, don't offer that food again until you talk with your doctor.
Babies shouldn't have:
- foods with added sugars and no-calorie sweeteners
- high-sodium foods
- honey, until after the first birthday.
 It can cause botulism in babies.
It can cause botulism in babies. - unpasteurized juice, milk, yogurt, or cheese
- regular cow's milk or soy beverages before 12 months instead of breast milk or formula. It’s OK to offer pasteurized yogurt and cheese.
- foods that may cause choking, such as hot dogs, raw carrots, grapes, popcorn, and nuts
Tips for Feeding Your Baby Solid Foods
With the hectic pace of family life, most parents try commercially prepared baby foods at first. They come in small, convenient containers, and manufacturers must meet strict safety and nutrition guidelines.
If you prepare your own baby foods at home, here are some things to keep in mind:
- Follow the rules for food safety, including washing your hands well and often.
- To preserve the nutrients in your baby's food, cook it in ways that keep the most vitamins and minerals. Try steaming or baking fruits and vegetables instead of boiling, which washes away the nutrients.
- Freeze portions that you aren't going to use right away.

- Whether you buy the baby food or make it yourself, texture and consistency are important. At first, babies should have finely puréed single-ingredient foods. (Just applesauce, for example, not apples and pears mixed together.)
- After your baby is eating individual foods, it's OK to offer a puréed mix of two foods. As babies get older, they will learn to eat a greater variety of tastes and textures.
- If you use prepared baby food in jars, spoon some of the food into a bowl to feed your baby. Do not feed your baby right from the jar — bacteria from the baby's mouth can contaminate the remaining food. If you refrigerate opened jars of baby food, it's best to throw away anything not eaten within a day or two.
- Around 6 months of age is a good time for your baby to try a cup. You might need to try a few cups to find one that works for your child. Use water at first to avoid messy clean-ups. Do not give juice to infants younger than 12 months.
Over the next few months, introduce a variety of foods from all the food groups. If your baby doesn't seem to like something, don’t give up. It can take 8 to 10 tries or more before babies learn to like new foods.
If your baby doesn't seem to like something, don’t give up. It can take 8 to 10 tries or more before babies learn to like new foods.
Sleep and Your 4- to 7-Month-Old (for Parents)
By this age, your baby should be well on the way toward having a regular sleep pattern. Some infants, particularly those who are breastfed, may still wake at night. But most no longer need a middle-of-the-night feeding.
How Long Will My Baby Sleep?
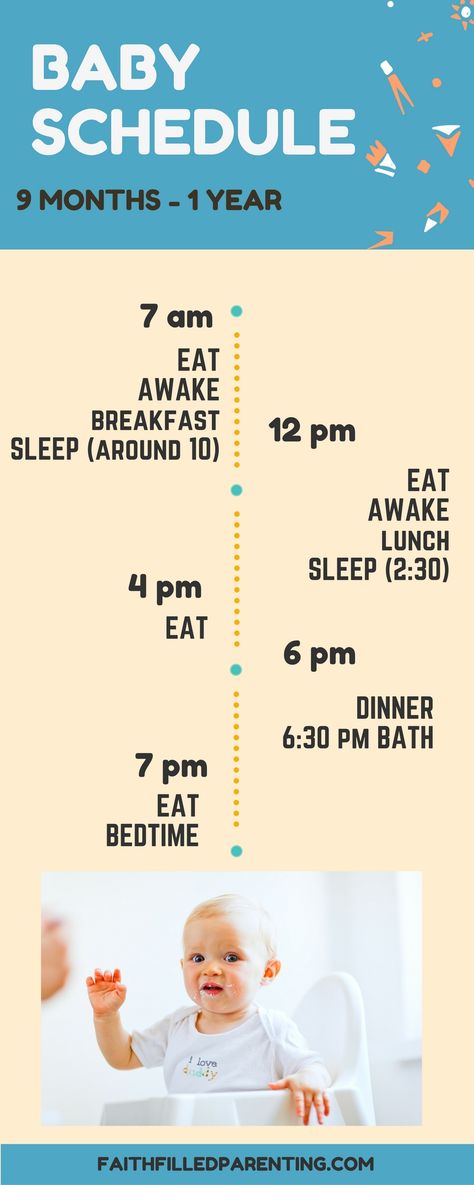
Most babies this age should sleep 12–16 hours a day, which includes a longer stretch at night and at least two naps during the day, says the National Sleep Foundation. The average amount of daytime sleep is now about 3–4 hours.
By 6 months, most babies are sleeping at night for 9 hours or longer, with brief awakenings.
How Should Babies Sleep?
The American of Academy of Pediatrics (AAP) recommends room-sharing without bed-sharing until the first birthday or for at least 6 months, when the risk of SIDs (sudden infant death syndrome) is highest.
Room-sharing is when you place your baby's crib, portable crib, play yard, or bassinet in your own bedroom instead of in a separate nursery. This keeps your baby nearby and helps with feeding, comforting, and monitoring your baby at night.
While room-sharing is safe, putting your baby to sleep in bed with you is not. Bed-sharing increases the risk of SIDS and other sleep-related deaths.
Follow these recommendations for a safe sleep environment for your little one:
- Always place your baby on their back to sleep, not on the stomach or side. The rate of SIDS has gone way down since the AAP began recommending this in 1992. When babies consistently roll over from front to back and back to front, it's fine for them to remain in the sleep position they choose.
- Use a firm, flat sleep surface. Cover the mattress with a sheet that fits snugly.
- Do not put anything else in the crib or bassinet. Keep plush toys, pillows, blankets, unfitted sheets, quilts, comforters, sheepskins, and bumper pads out of your baby's sleep area.
- To avoid overheating, dress your baby for the room temperature and don't overbundle. Don't cover your baby's head while they're sleeping. Watch for signs of overheating, such as sweating or feeling hot to the touch.
- Keep your baby away from smokers. Secondhand smoke increases the risk of SIDS.
- Offer a pacifier to your baby at sleep time, but don’t force it. If the pacifier falls out during sleep, you don’t have to replace it. If you're breastfeeding, wait until breastfeeding is firmly established.
- Watch out for other hazards, such as items with cords, ties, or ribbons that can wrap around a baby's neck, and objects with any kind of sharp edge or corner. Look around for things that your baby can touch from a seated or standing position in the crib. Hanging mobiles, wall hangings, pictures, draperies, and window blind cords could be harmful if they are within a baby's reach.
- Don’t let your baby fall asleep on a product that isn’t specifically designed for sleeping babies, such as a sitting device (like a car seat), a feeding pillow (like the Boppy pillow), or an infant lounger (like the Dock-a-Tot, Podster, and Bummzie).
- Don’t use products or devices that claim to lower the risk of SIDS, such as sleep positioners (like wedges or incliners) or monitors that can detect a baby’s heart rate and breathing pattern. No known products can actually do this.
- Don’t use weighted blankets, sleepers, or swaddles on or around your baby.
- Make sure that all sleep surfaces and products you use to help your baby sleep have been approved by the U.S. Consumer Product Safety Commission (CPSC) and meet federal safety standards.
Helping Your Baby Sleep
You may have started a bedtime routine that you're sticking to. If you haven't yet, now is a good time to start. Soothing activities that lead up to "night-night" time can help relax your baby. A warm bath followed by stories or singing will signal an end to the day, and these same activities can be used at bedtime for years to come.
You'll want your baby to fall asleep on their own. This may mean doing your nighttime routine and putting the baby into the crib while they're drowsy but still awake. If your baby cries, stay away for a few minutes. Your baby may settle down and go to sleep.
If your baby cries, stay away for a few minutes. Your baby may settle down and go to sleep.
If the crying continues, soothe your baby for a moment without picking your little one up. This may go on a few times until your baby figures out that the crying is not getting results. This can be tough for parents, since it's upsetting to hear your baby cry. If you know your baby is safe (and not hungry, wet, soiled, or feeling unwell), it's OK to give them time to settle down.
Why Does My Baby Wake at Night?
Even a baby who has been sleeping through the night will sometimes wake in the wee hours, just as adults do. Some babies may call out or cry in the middle of the night, then calm down when mom or dad enters the room. This is due to separation anxiety, a normal stage of development that happens during this time.
Give your baby a few fussy minutes before you respond. After seeing that everything is OK and reassuring your baby without taking your little one out of the crib, leave your baby alone to fall back to sleep.
Remember: Cuddling, feeding, or talking when your baby wakes up may prompt your little one to wake regularly for this attention.
When Should I Call the Doctor?
Most infants at this age will have a regular sleep routine and are able to sleep through the night. But there is a wide range of normal. If you have any questions about your baby's sleep, talk with your doctor.
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. nine0009 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ” nine0003
If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ” nine0003
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK. nine0003
nine0003
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a cesarean section or other complications during childbirth,
You can still make skin-to-skin contact with your baby and breastfeed him in the first hours after birth. nine0003
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.” nine0003
“It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.” nine0003
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy. nine0003
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop.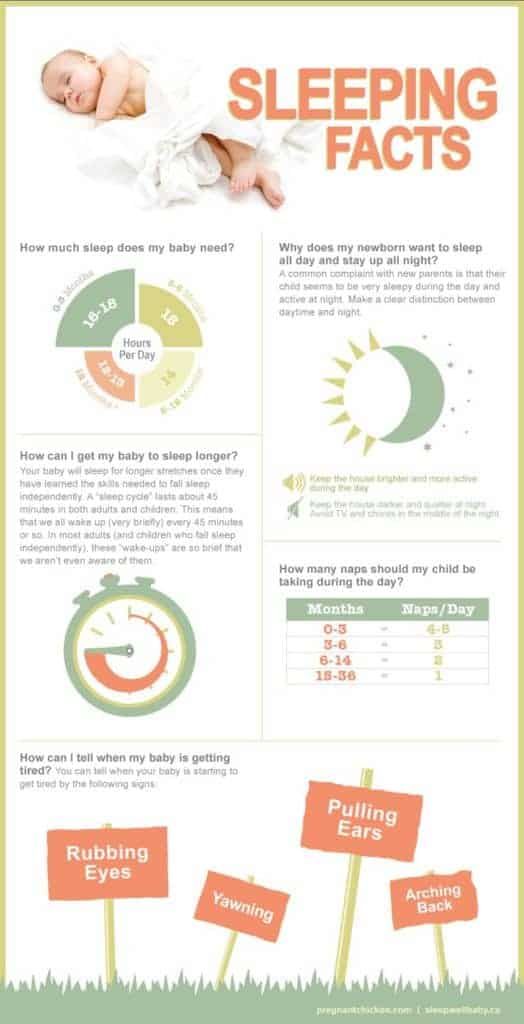 Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital. nine0003
Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital. nine0003
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth.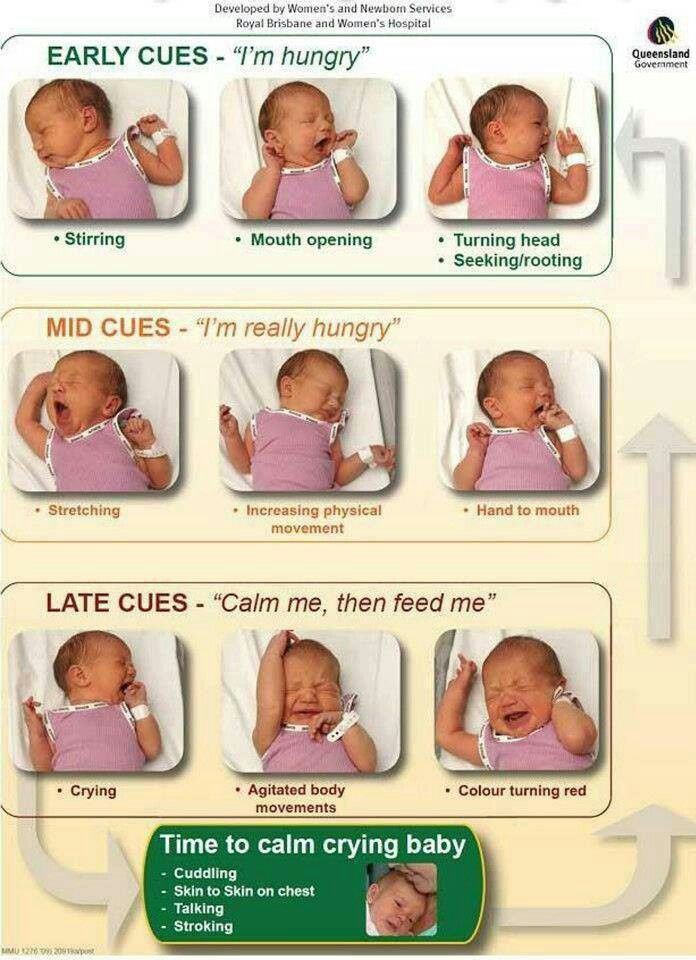 nine0009 6
nine0009 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed? nine0015
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy. nine0003
When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy. nine0003
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise." nine0003
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable. nine0003
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.” nine0003
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. nine0009 4
This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. nine0009 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black. nine0087
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often.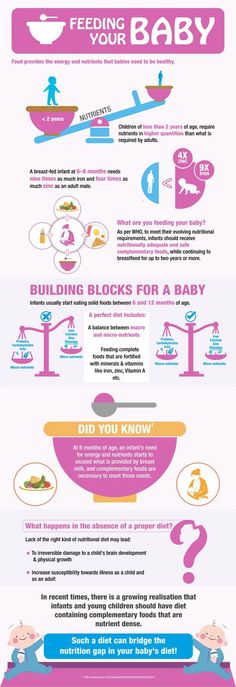 In addition, during the first few days, the weight of wet diapers increases. nine0009 11
In addition, during the first few days, the weight of wet diapers increases. nine0009 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that this is not enough for your baby. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends. nine0003
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." nine0201 Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." nine0201 G Egypt Public Health Assoc.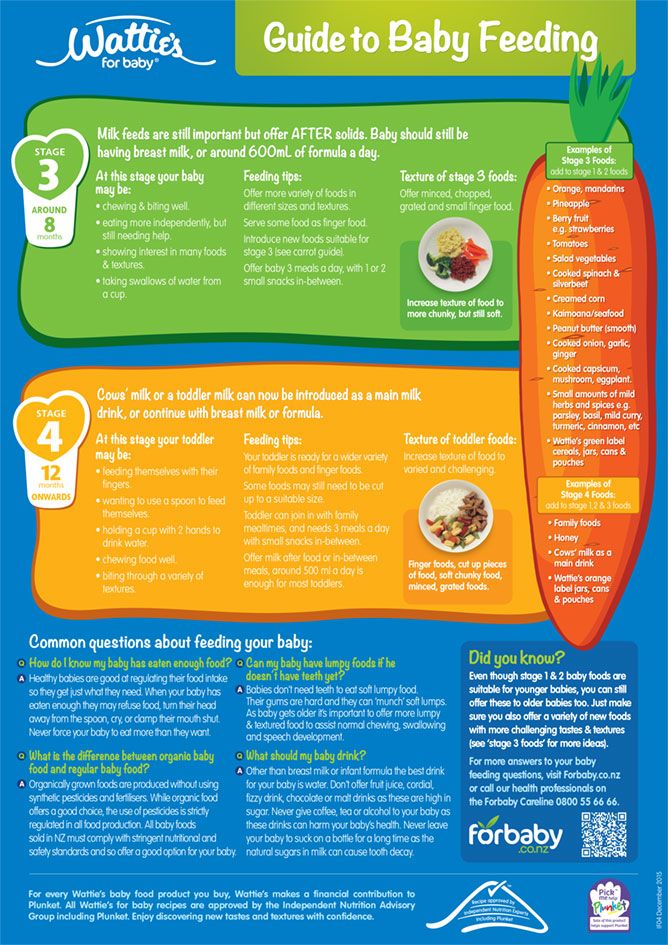 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." W Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al. , "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
, "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
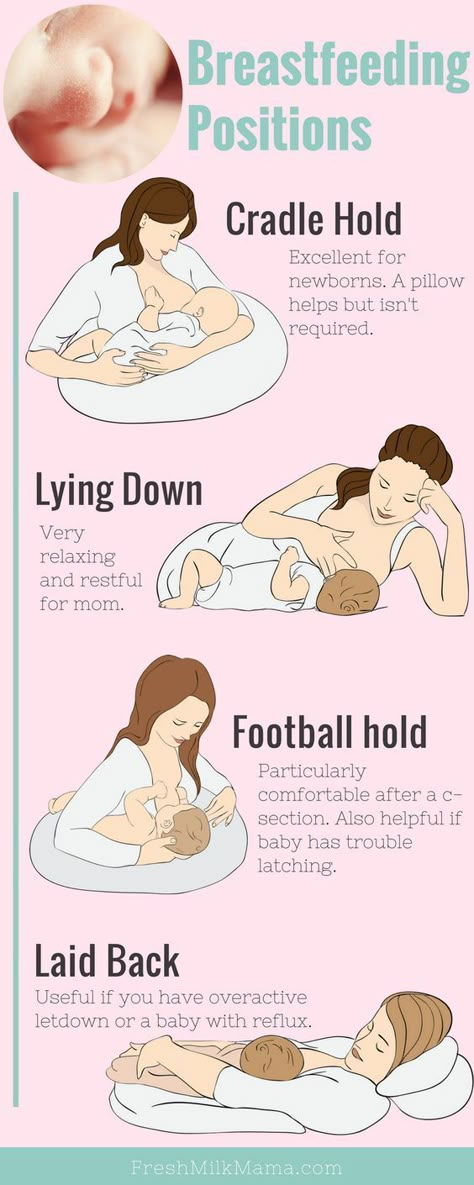
Different breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information nine0003
There is no right or wrong way to hold the baby while feeding
, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.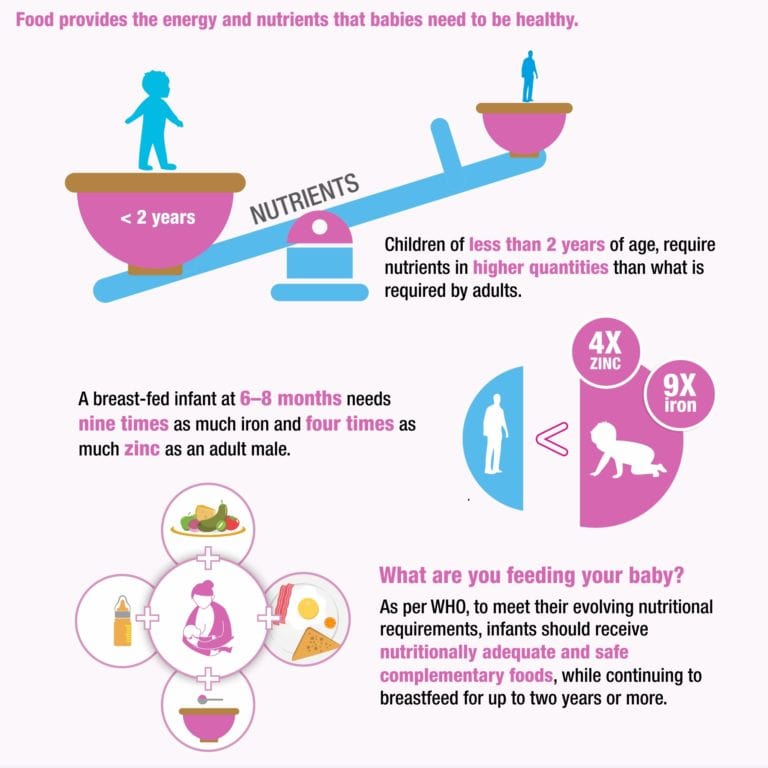
Whatever position you choose to breastfeed your baby, remember a few simple rules. nine0003
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby firm, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms. nine0087
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
Relaxed feeding position, also known as biological feeding, 1 is often the first position for most moms.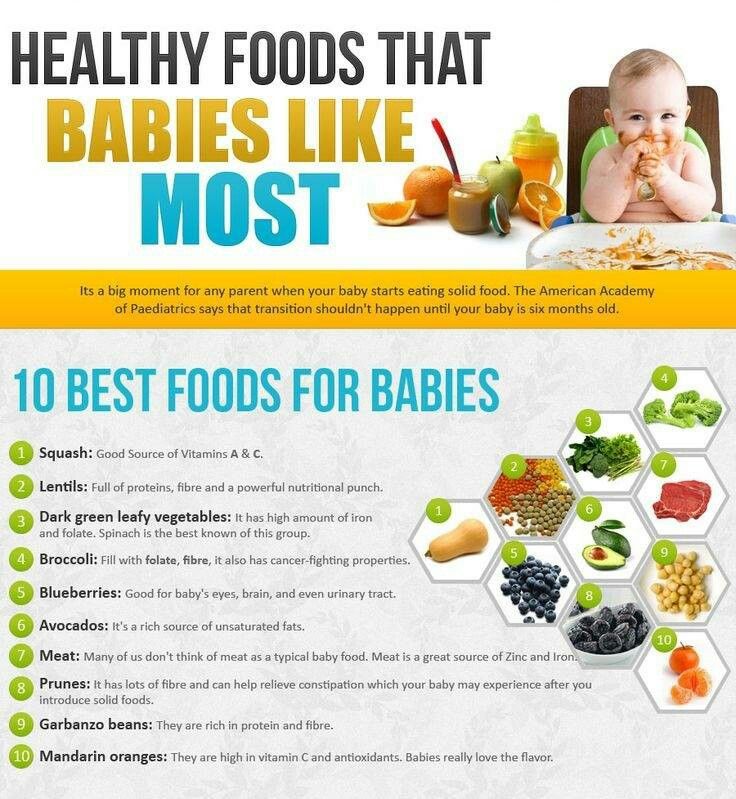 If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ” nine0003
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows.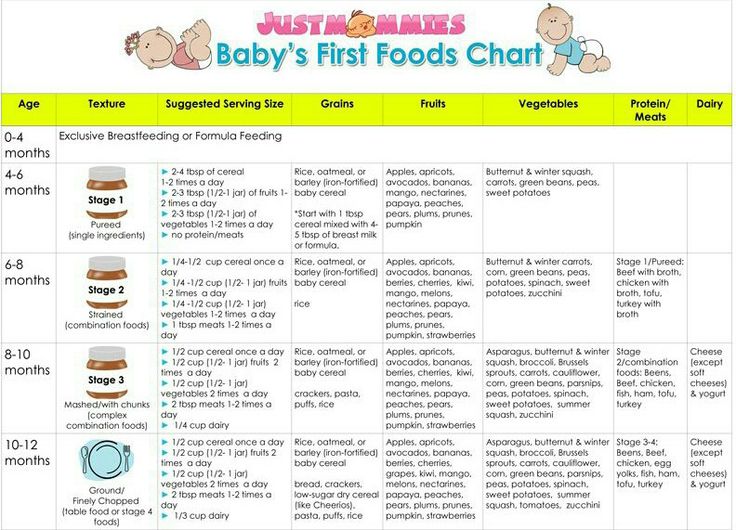 So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits
straight, and the baby lies on her side on her arm, pressing her stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided. nine0003
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost exactly like the cradle, but the baby is on the other arm. 3 This gives baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand. nine0003
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above). nine0003
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above). nine0003
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of the position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts. nine0003
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for relaxed
feedings at night in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.” nine0003
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 Try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding an older child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone. nine0003
nine0003
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 According to some mothers, this breastfeeding position is good to use from time to time for mastitis, when touching the breast is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain. nine0003
nine0003
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful. nine0003
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out of the house, look after older children, or even do a little household chores. nine0003
nine0003
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest. nine0003
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball gripping”) is great for mothers of twins—you can breastfeed both at the same time, with your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second. nine0003
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second. nine0003
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other). nine0003
11. Feeding in the “hand-supported breast” or “dancer's hand” position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time.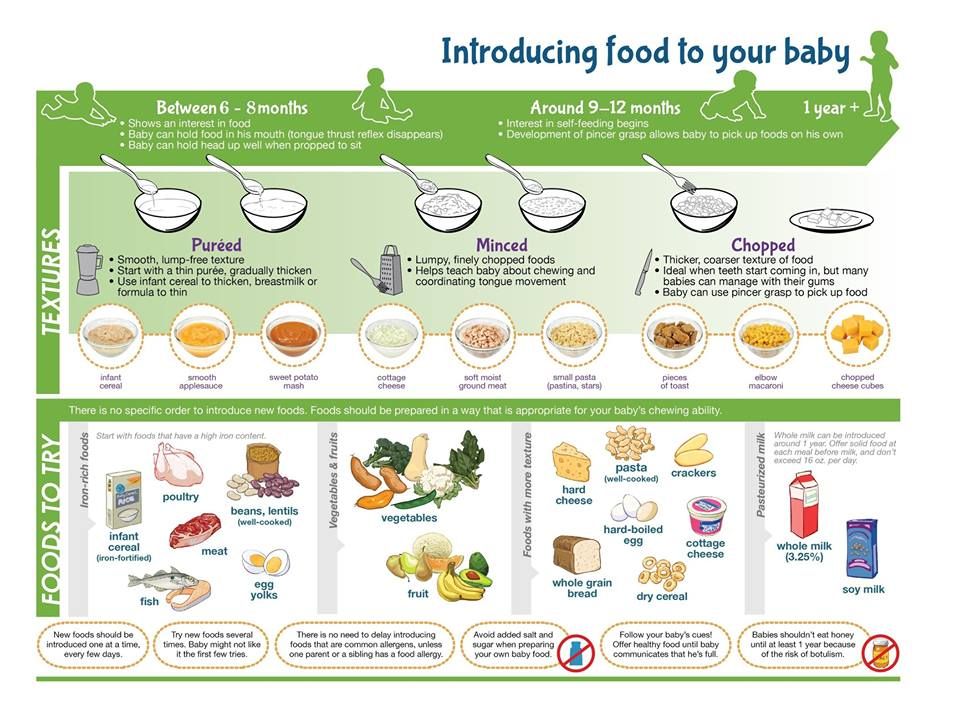 4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast. nine0003
4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast. nine0003
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ].