When to feed baby dairy
Milk FAQs for Babies & Toddlers - First Foods
Just joining? Check out our guides on Starting Solids and Toddlers at the Table.
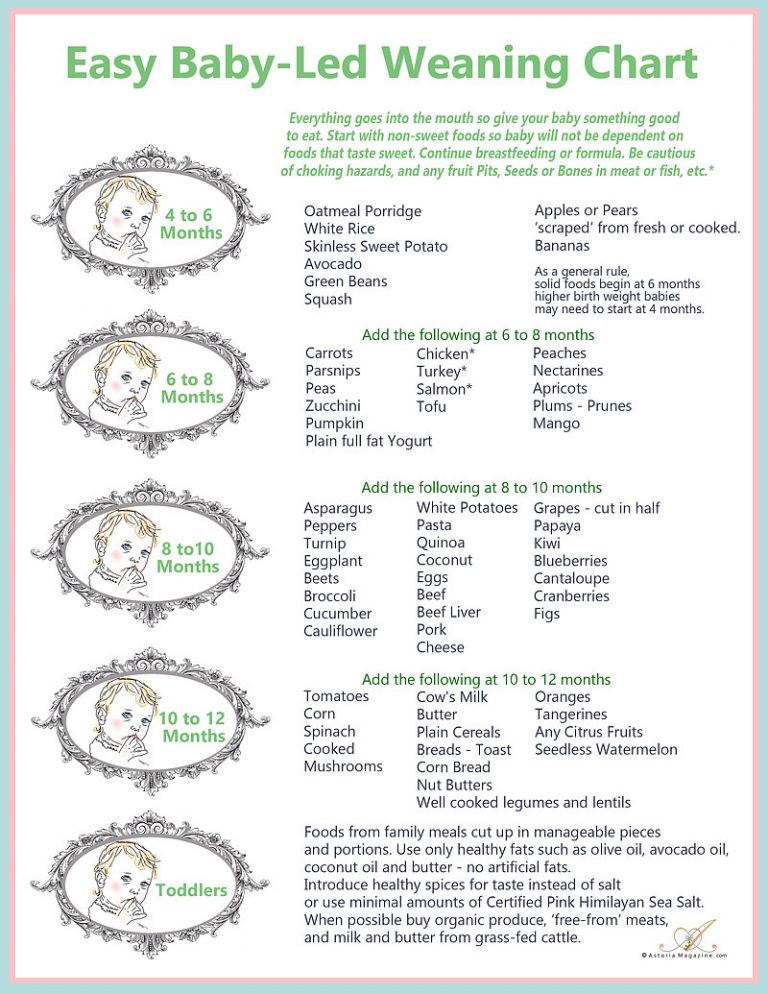
Can babies have dairy before age one?Yes. Babies can have dairy as solid foods before age one, but the type and preparation matters. Dairy products such as full fat yogurt, low-sodium cheeses, butter, and ghee, are fine to offer to your baby after 6 months of age in age-appropriate amounts after having successfully introduced iron-rich foods. Small amounts of milk can also be used in cooking, as long it doesn’t replace breastmilk or formula intake. This can be confusing since cow’s milk or other milk drinks are not usually recommended until after 12 months of age.
Because cow’s milk as a drink is consumed in much greater amounts than the other dairy foods mentioned, and often takes the place of, or can completely replace breast milk and formula intake, its introduction before 11-12 months of age can lead to issues like iron deficiency anemia and intestinal distress. This is because cow’s milk is nutritionally incomplete, low in iron, and has proteins that can be difficult to digest.1 2 Interestingly, because yogurt and cheese are fermented, the harder-to-digest proteins can become partially broken down, and may make them easier for baby to tolerate.3 4 Ghee and butter have minimal to no protein and are usually well tolerated by babies.
No, though the American Academy of Pediatrics does recommend plain cow’s milk for toddlers 12 months and older as a source of essential fat and nutrients, including calcium, vitamin D, protein, vitamin A, and zinc.5 That said, if your child is 12 months or older, meeting growth chart standards, without health concerns or allergies that may affect diet and eating a wide variety of fresh foods high in the aforementioned essential nutrients, cow’s milk (or any milk, plant-based or otherwise) may not be necessary. If you want to avoid animal milk entirely, it would be wise to work with your pediatrician and/or pediatric dietitian to ensure your child is receiving optimal nutrients.
If you want to avoid animal milk entirely, it would be wise to work with your pediatrician and/or pediatric dietitian to ensure your child is receiving optimal nutrients.
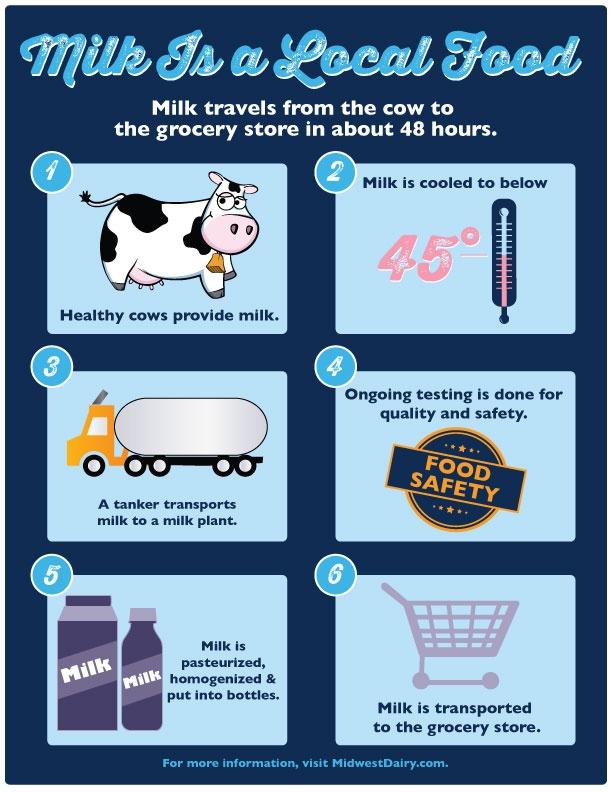
Most pediatric organizations have recommended waiting until a baby’s first birthday to introduce cow’s milk as a drink as the digestive systems of babies may not tolerate cow milk protein in large quantities well.6 Compared to breast milk or formula, cow’s milk is nutritionally incomplete, which means that it does not provide all of the healthy fats and nutrients that your baby needs to thrive.7 8 While cow’s milk forms the base for most infant formulas, it is modified in formula to make it nutritionally similar to human milk.9
Dairy products like yogurt and cheese, however, can be introduced as early as 6 months of age. You do not need to wait to introduce these nutritious foods and many dairy products like Greek yogurt are easily tolerated and digested.
Around 11 months of age, it is our opinion that it’s okay to offer small sips of cow’s milk (about 1 ounce) in an open cup to encourage your baby’s drinking skills and to acclimate your child to the new taste. Just avoid replacing breast milk or formula feeds with cow’s milk. Cow’s milk should ideally never be served in a bottle, but it can be offered in an open cup or with a straw. Babies who consume cow’s milk prior to their first birthday are more at risk of iron deficiency anemia and intestinal distress, which can also contribute to anemia.10 Why? Cow’s milk is low in iron and babies who drink cow’s milk may reduce their intake of other iron-rich foods.11
Can I give baby cow’s milk in a bottle?
As a child starts the transition to cow’s milk around 12 months old, it might feel like a natural progression to serve milk in baby bottles. We advise against this practice for a few key reasons:
- By 12 months of age, most children have become efficient with drinking from a bottle and can rapidly consume several ounces at a time from one.
 Because they are used to the bottle offering a full meal, serving cow’s milk in this way can lead to toddlers taking in too much in one sitting and throughout the day, which increases the risk for iron deficiency anemia and tends to decrease interest in solids.
Because they are used to the bottle offering a full meal, serving cow’s milk in this way can lead to toddlers taking in too much in one sitting and throughout the day, which increases the risk for iron deficiency anemia and tends to decrease interest in solids. - Unlike formula and breast/human milk during infancy, cow’s milk is not meant to be a meal for toddlers. It’s a drink to be consumed with a meal at the table. Bottles are often consumed away from the table for both nourishment and comfort, so putting cow’s milk in a bottle can create a slippery slope toward a toddler drinking cow’s milk throughout the day and away from the table.
- Cow’s milk in a bottle is associated with increased risk of cavities. The risk is highest when a toddler sips on cow’s milk from a bottle throughout the day and when they consume cow’s milk at night in bed. These practices can lead to pervasive cavities, commonly referred to as “bottle rot.”12
Is cow’s milk good or bad for babies?
Compared to breast milk and formula, cow’s milk poses many nutritional disadvantages for babies younger than 12 months of age.
Cow’s milk is low in a number of nutrients but, most importantly, it is low in iron—an essential nutrient that fuels your baby’s brain development. To complicate matters, the type of iron that is present in cow’s milk is not as well absorbed as the form of iron found in breast milk.13 While cow’s milk has more protein and minerals like calcium and phosphorous, the higher mineral content may increase the risk of dehydration in babies (though evidence is limited).14 Lastly, early consumption of cow’s milk can take the place of other, more nutritious foods that your baby would have otherwise been eating, increasing the risk of nutritional deficiencies as a result.15
Genetics, gut function, and the age at the time of introduction all influence your baby’s response to dairy. Additionally, the quality of dairy matters. Upwards of 90 percent of cows live on a diet of genetically-modified, pro-inflammatory corn, cottonseed, and soy and contain levels of toxins often exceeding government limits. 16 17 Unfortunately, the contaminants in conventional dairy can disrupt hormone function and lead to a wide range of adverse health concerns.18
16 17 Unfortunately, the contaminants in conventional dairy can disrupt hormone function and lead to a wide range of adverse health concerns.18
Because we don’t fully understand either the effects of these chemicals on the body, aim to buy organic, pasteurized dairy if possible. We do understand that organic milk isn’t an option for all families and in this case, we encourage that you do the best you can with the resources available to you and your family.
Whenever you decide to introduce dairy, be sure to watch for signs that your baby cannot digest dairy (such as stomach pain, gas, and/or diarrhea) and consult your pediatrician for advice.
How much cow’s milk can my child drink?Introduction of cow’s milk is discouraged for babies 6-12 months of age, but it’s fine to offer dairy products such as yogurt or cheese in limited amounts. Around 11 months of age it may be fine to offer small sips of whole cow’s milk (no more than 1-2oz) in an open cup to practice feeding skills and accustom baby’s palate to the new taste of cow’s milk, as long as it doesn’t displace the intake of breast/human milk, formula, or iron-rich foods. 19 20 This practice varies across countries, cultures, and health guidance. Beyond 12 months of age, whole cow’s milk is fine to offer to your now toddler, assuming that they have a well-balanced diet that has adequate iron.21
19 20 This practice varies across countries, cultures, and health guidance. Beyond 12 months of age, whole cow’s milk is fine to offer to your now toddler, assuming that they have a well-balanced diet that has adequate iron.21
Recommendations for dairy intake for 12 months and up are considered in total servings of dairy products in a day, not just from liquid milk alone. This includes servings of yogurt and cheeses, but excludes butter and ghee.22
Serving sizes of dairy include the following: 23
- 1 cup of milk or yogurt (8oz) = 1 serving of dairy
- 1-1.5oz of cheese = 1 serving of dairy
- 1 cup of a calcium-fortified milk substitute like soy or pea protein milk = 1 serving of dairy
Fear not, it’s simpler than it sounds. Let’s break it down by age!24
- 6-12 months: Stick to breast/human milk or formula as baby’s main drink. A little bit of milk mixed into foods is fine as long as it doesn’t replace breast/human milk or formula intake.
 At this age, there are no set recommendations for total servings of dairy. Aim to limit dairy to 0.5-1 daily servings as baby will be receiving plenty of calcium from breast/human milk or formula and to help prioritize iron-rich foods.
At this age, there are no set recommendations for total servings of dairy. Aim to limit dairy to 0.5-1 daily servings as baby will be receiving plenty of calcium from breast/human milk or formula and to help prioritize iron-rich foods. - 11-12 months: Closer to one year of age and with the go ahead from your doctor, it’s okay to offer small sips of whole cow’s milk (no more than 1 to 2 ounces per day) in an open cup to accustom baby’s palate to the new taste of cow’s milk. That said, it is also fine to hold off.
- 1-2 years: Limit milk consumption to no more than 16oz of cow milk per day or 2 servings total of dairy products so milk doesn’t displace valuable nutrients (such as iron) from solids.25 Opt for whole cow’s milk and whole milk dairy products. If still consuming breast/human milk, the child may not need as many servings of dairy in a day.
- 2-3 years: Toddlers can have up to 2-2.5 servings of dairy per day.
 26 You may hear of recommendations to switch to a lower fat milk, but not all kids need this so be sure to speak with your pediatric health professional for guidance.
26 You may hear of recommendations to switch to a lower fat milk, but not all kids need this so be sure to speak with your pediatric health professional for guidance.
Our recommendations slightly vary from the AAP, which recommends 16-24oz of dairy for children 12+ months and is more in line with USDA’s recommendation of up to 2 daily servings of dairy or other calcium-fortified dairy replacements, such as soy or pea protein milk.27 It is our stance that exceeding 16oz of dairy for 12-24-month-old children risk displacing valuable nutrients (especially iron) from other food sources as it can impede appetite and hunger.
Note: If your child is dairy-free, then these recommendations also apply to milk alternatives like soy and pea protein milks. Cheeses and yogurts made from alternative milks are not usually as nutritious as those made from cow’s milk and are often highly processed. Consider sticking to the dairy-free milk itself as your child’s main source of “dairy,” calcium, and vitamin D.
Does calcium in cow’s milk inhibit iron absorption?
Yes, calcium can affect how our bodies absorb iron from certain foods. Know, however, that your baby’s ability to absorb iron is affected by many factors.
At this stage in life, your baby’s iron levels are already at their lowest and lots of iron is needed for healthy growth. Iron doesn’t affect calcium absorption, but calcium does affect the absorption of iron from plants, meat, and seafood.28 29 This is one of the key reasons why cow’s milk is not recommended for babies under 12 months of age. The body is brilliant at self-regulating and studies show that iron status is not necessarily affected by calcium intake because the body will adjust iron absorption when stores are low.30 Studies also show that the effect of calcium on iron absorption is reduced when a diet consists of a wide range of foods.31
For a list of foods that offer the nutrients babies need most, see our Nutrition Cheat Sheet for babies.
What is the best milk for toddlers? Whole milk, low fat, or skim?
The verdict is still out. Whole pasteurized milk is recommended for children under two years of age, at which point many parents are guided to switch their toddler to reduced-fat cow’s milk. However, a summary of 14 studies measuring the effects of consumption of whole milk versus reduced-fat milk shows that higher fat intake correlates with lower weight as children age, and that reduced-fat milk consumption correlates with increased weight or obesity.32 Whatever fat content you choose, be sure to look for milk without any added flavors or sugars.
Adie, 18 months, asks for more milk.Hawii, 15 months, downs a cup of milk.
Can cow’s milk cause constipation?
Yes. Cow milk, specifically the protein found in cow milk, is notorious for exacerbating constipation. If your child is 12 months and older, we generally recommend trying a non dairy milk alternative such as fortified unsweetened soy or pea protein milk (and we typically advise against toddler formulas unless prescribed by a doctor for weight gain.) Aside from milk, to prevent or ease constipation, make sure your child is drinking plenty of water throughout the day, being offered a varied diet rich in whole foods, and remaining active. Constipation can be a little tricky to treat, so definitely check in with your doctor on the plan of action.
Constipated baby? See our guide How to Relieve Infant Constipation.
Constipated toddler? See our guide 10 Ways to Relieve Constipation in Toddlers.
What about raw milk?
Avoid. Babies’ immune systems are still developing, and raw milk can harbor pathogenic bacteria and other potential contaminants that can increase the risk of foodborne illnesses, which can be fatal to babies. Pasteurization—the process of heating a food to a certain temperature to kill bacteria—is fundamental to reducing the risk of foodborne illness and thus making food safer to eat.33 For these reasons and more, many medical organizations recommend that all milk for human consumption should be pasteurized.34
Pasteurization—the process of heating a food to a certain temperature to kill bacteria—is fundamental to reducing the risk of foodborne illness and thus making food safer to eat.33 For these reasons and more, many medical organizations recommend that all milk for human consumption should be pasteurized.34
Can babies be allergic to milk?
Absolutely. Cow’s milk is one of the most common food allergens for babies.35
Learn more about common food allergens in our guide Introducing Allergens to Babies.
Can a baby outgrow a milk allergy?
Yes! If your baby is allergic to dairy, be reassured that it is an allergy that often disappears with time. Research shows that the majority of children with cow’s milk allergy will outgrow it by age 6 and many babies with milder symptoms of milk protein allergy (which can show up as painless blood in stool) are able to successfully reintroduce cow’s milk as early as their first birthday, with the guidance of their doctors. 36 37
36 37
No, unfortunately if baby has CMPA, they can’t have other dairy products, including milk, yogurt, and cheese.38 Milk from other animals, such as goat and sheep, are also not recommended.39 Lastly, soy milk or soy-based formula is generally not recommended either, as babies with CMPA can also be sensitive to soy and soy-based products. Remember, research shows that the majority of children with cow’s milk allergy will outgrow it by age 6 and many babies with milder symptoms of milk protein allergy (which can show up as painless blood in the stool) are able to successfully reintroduce cow’s milk as early as their first birthday, with the guidance of their doctors.40
What is the best milk substitute for a baby with CMPA?If your baby has CMPA, then they should also avoid milk from other animals, as well as soy milk and soy products since babies with CMPA can also be sensitive to these. 41 42 The good news is that there are a number of other milk substitutes available, such as breast/human milk (from a provider who is avoiding dairy and soy in their diet) or a CMPA-appropriate formula for babies, as recommended by your healthcare provider, or fortified pea protein or oat milk for toddlers. Do note that when compared to cow’s milk, pea protein milk is generally lower in calories and oat milk is generally lower in protein and can be included as part of a generally balanced diet. Be sure to connect with your pediatric healthcare provider such as your dietitian/nutritionist, to help identify the best substitute for your child’s individual needs.
41 42 The good news is that there are a number of other milk substitutes available, such as breast/human milk (from a provider who is avoiding dairy and soy in their diet) or a CMPA-appropriate formula for babies, as recommended by your healthcare provider, or fortified pea protein or oat milk for toddlers. Do note that when compared to cow’s milk, pea protein milk is generally lower in calories and oat milk is generally lower in protein and can be included as part of a generally balanced diet. Be sure to connect with your pediatric healthcare provider such as your dietitian/nutritionist, to help identify the best substitute for your child’s individual needs.
Note: Lactose-free formula or milk would not be appropriate for a child with CMPA. In CMPA, the natural proteins in milk are triggering the allergic reaction. Lactose-free milk still contains these natural proteins but is free of a natural sugar called lactose. Lactose-free milk is appropriate for individuals with lactose intolerance, but keep in mind that lactose intolerance is uncommon in infants and toddlers and is typically not an issue in this age group. 43
43
What is the best milk alternative for children sensitive to cow’s milk?
It depends on the age:
0 to 12 months old: Breast milk. Studies show that breast milk is the most tolerated milk for babies.44
If you think your baby has sensitivities to infant formulas with dairy, reach out to your pediatrician for guidance. Cow’s milk protein allergy is thought to occur in 2-3% of infants in the US, and approximately 0.5% of breastfed babies.45 If your baby is formula fed and is having digestive difficulties, they may need to try out hypoallergenic or amino acid-based formulas.46 For breastfed babies, mom may need go on a dairy-free diet (but consult your pediatrician before self-diagnosing) and ensure she is getting adequate nutrition during this time too. As always, be sure to consult a pediatrician or pediatric gastroenterologist and/or pediatric dietitian or nutritionist when selecting an alternative, as some of these options can still pose a risk for allergic reaction. 47
47
12+ months of age: If your baby has a true cow milk protein allergy, they may need to avoid mammalian milks as well (such as buffalo, goat, and sheep milks), in addition to unmodified rice and soy milk as these milks have a risk of also triggering an allergic reaction and may not be nutritionally adequate.48 However, if your child is sensitive to cow’s milk, but not allergic, they could try alternative mammalian milk, or other plant-based milk alternatives listed below.49
What are the best plant-based milks for babies and toddlers?
Not all plant-based milks are created equal when it comes to nutritional value.50 Furthermore, plant-based milks are considered to be a nutritionally incomplete drink for babies and may promote nutrient deficiencies if they take the place of healthier foods for babies, like breast milk or formula.51 That’s why general consensus suggests waiting to serve plant-based milks as a drink until after a baby’s first birthday, though cooking foods with plant-based milks for your baby is perfectly fine.
When shopping for plant-based milks, read the labels. You want to select brands of plant-based milks that are fortified with calcium and vitamin D, free of added sugars, low in preservatives, and offer similar protein and calorie content to cow’s milk. Below are our top choices of plant-based milks ranked according to nutritional similarity to cow’s milk:
- Soy milk (fortified)
- Pea protein milk (fortified)
- Oat milk (fortified)
Our guide Best & Worst Plant-Based Foods for Babies explains the nutrients vegetarian and vegan babies need and where to find them.
The chart below shows how popular plant-based milks stack up against mammalian milks, organized by nutritional density across key nutrients babies and toddlers need:
Nutritional content of common animal and plant-based milksPer 8 oz serving
| Milk type | Calories | Fat (gm) | Protein (gm) | Calcium (mg) | Vitamin D (mcg) | Vitamin B12 (mcg) |
| Cow1 | 149 | 7. 9 9 | 7.7 | 276 | 3.2 | 1.1 |
| Cow1 (lactose-free) | 146 | 7.8 | 8 | 300 | 2.7 | 1.3 |
| Goat1 | 168 | 10.1 | 8.7 | 327 | 3.2 | 0.2 |
| Sheep1 | 265 | 17 | 15 | 473 | Unavailable | 1.7 |
| Buffalo1 | 237 | 17 | 9 | 412 | Unavailable | 0.9 |
| Camel2 | 134 | 7.7 | 7.4 | 274 | Unavailable | Unavailable |
| Soy3,9 | 105 | 3.6 | 6.3 | 300 | 2.7 | 2.1 |
| Pea4,9 | 70 | 4.5 | 8 | 465 | 6 | 2.5 |
| Oat5,9 | 160 | 9 | 3 | 350 | 3.6 | 1.2 |
| Rice9 | 113 | 2.3 | 0. 7 7 | 283 | 2.4 | 1.5 |
| Almond3,9 | 90 | 2.5 | 1 | 451 | 2.5 | 3 |
| Coconut3,9 | 76 | 5.1 | 0.5 | 459 | 2.4 | 1.5 |
| Hemp6,9 | 80 | 8 | 2 | 390 | 5 | 0.6 |
| Flax7,9 | 25 | 2.5 | 0 | 280 | 2.3 | 1.4 |
| Macadamia7,9 | 50 | 5 | 1 | 585 | 5 | 1.2 |
| Breast/human milk10 | 172 | 10.8 | 2.53 | 79 | 0.25 | 0.123 |
 9. Nutritional content will vary with different brands and preparations. 10. The nutrition of all breast milk is not the same and will vary based on various factors, including mom’s diet and health. Breast milk, animal milks, and plant-based milks are not nutritionally equivalent; as such, animal and plant-based milks should not be offered in place of breast milk in babies <12 months of age.53
9. Nutritional content will vary with different brands and preparations. 10. The nutrition of all breast milk is not the same and will vary based on various factors, including mom’s diet and health. Breast milk, animal milks, and plant-based milks are not nutritionally equivalent; as such, animal and plant-based milks should not be offered in place of breast milk in babies <12 months of age.53Using data from USDA’s FoodData Central unless otherwise specified, accessed May 14, 2020.
What are the best plant-based milks for toddlers with allergies?
Fortified, organic soymilk or pea protein milk are the most nutritious milk alternatives from the standpoint of nutrients that toddlers need. If your child is allergic to soy or legumes, oat milk is a good alternative. In detail:
- Soy, a legume, was one of the first plants to replace dairy. Compared to cow milk, it’s lower in carbohydrates, fats and proteins, and insufficient amounts of calcium and B-12.
 However, compared to other plant-based beverages, soymilk is one of the best sources of all of these nutrients, and it’s the only plant-based milk with protein levels similar to cow’s milk. Therefore, if your child can tolerate soymilk, that is the most nutritious option. Note that soy contains high levels of isoflavones (which may alter hormones, though no statistically significant data has surfaced), and still poses risk of allergic reaction.54 For these reasons, soy may not be ideal as the only plant-based beverages offered as a milk alternative.
However, compared to other plant-based beverages, soymilk is one of the best sources of all of these nutrients, and it’s the only plant-based milk with protein levels similar to cow’s milk. Therefore, if your child can tolerate soymilk, that is the most nutritious option. Note that soy contains high levels of isoflavones (which may alter hormones, though no statistically significant data has surfaced), and still poses risk of allergic reaction.54 For these reasons, soy may not be ideal as the only plant-based beverages offered as a milk alternative.
- Pea protein milk, another legume, (often sold under the brand name Ripple), offers fewer carbohydrates and fat than cow’s milk, yet is a great source of protein. It also touts higher levels of calcium, iron and vitamin D than cow’s milk, and is fortified with vitamin B12.55
- Oat, a pseudo-grain, is low in beneficial fats and proteins, yet has a better amino acid profile that other plant-based beverages.
 While the fiber in oats may benefit the gut, it’s naturally low in calcium (although it is often fortified with calcium, vitamin D, and vitamin B12) and also contains phytic acid, which may inhibit nutrient absorption.56
While the fiber in oats may benefit the gut, it’s naturally low in calcium (although it is often fortified with calcium, vitamin D, and vitamin B12) and also contains phytic acid, which may inhibit nutrient absorption.56
Also, each of these plant-based beverages has benefits and drawbacks. If using a milk alternative, opt for one that is fortified with key vitamins and minerals (be sure to read labels, as not all are fortified). Some are high on the glycemic index and come in forms that also include added sugars, preservatives, binders and other ingredients that may not benefit health when offered frequently and in large quantities.57 Lastly, most grains, nuts and legumes grown in conventional agriculture are genetically modified and/or are grown with chemicals. Therefore, consider milk alternatives as a “sometimes” beverage and/or considering rotating the types of milk alternatives you offer.
In most cases, milk alternatives are not recommended to replace cow’s milk (except for health reasons). A well-balanced diet consisting of whole plant and animal foods may offer ideal nutrient intake without cow’s milk or fortified milk alternatives. As always, work with your pediatrician, allergist, and/or pediatric dietitian or nutritionist when selecting a cow milk alternative that is best for your child.
A well-balanced diet consisting of whole plant and animal foods may offer ideal nutrient intake without cow’s milk or fortified milk alternatives. As always, work with your pediatrician, allergist, and/or pediatric dietitian or nutritionist when selecting a cow milk alternative that is best for your child.
Is almond milk good for babies and toddlers?
Unfortunately, almond milk lacks the protein, fat, and calories we like to see in plant-based milks for toddlers. More nutritious options would be fortified soy, pea, or oat milk—all of which have greater amounts of calories, fat, and protein.
What if my child won’t drink milk?In general, milk is a great source of protein, fat, carbohydrates, zinc, vitamin B12, and especially, calcium and vitamin D (if the milk if vitamin D-fortified). The good news is that you can find many of these essential nutrients from a wide variety of foods. Let’s hone in on the key nutrients found in milk, calcium and vitamin D.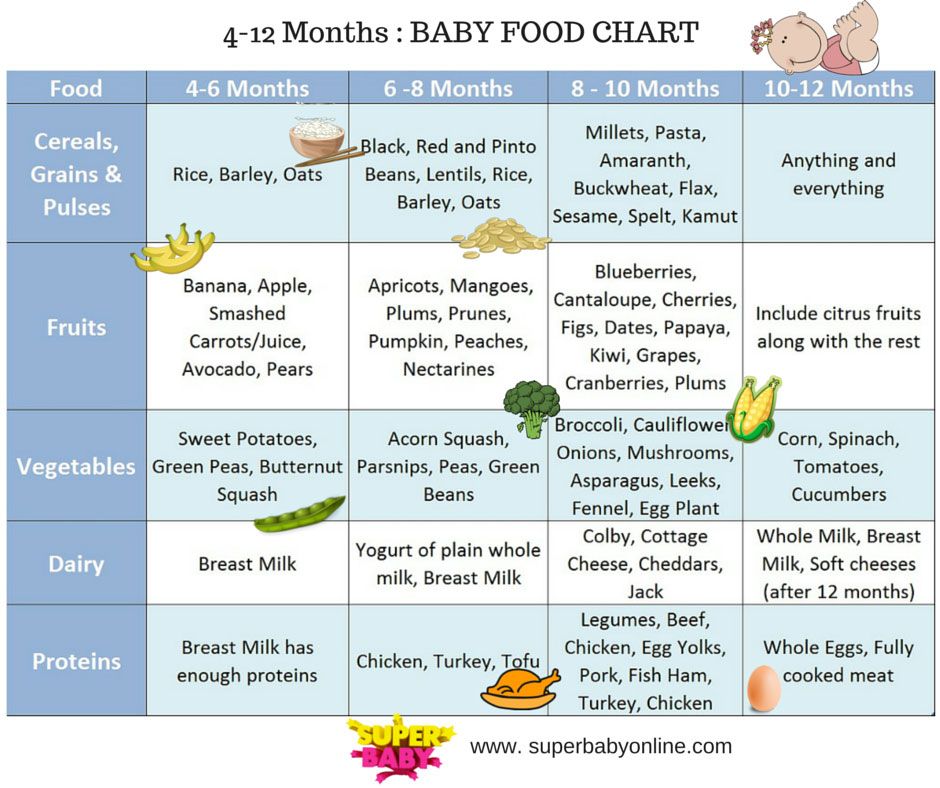 For calcium, you can offer other calcium-rich foods to your child like yogurt and cheese, as well as plant-based sources of calcium like sesame, almonds, broccoli, other dark green vegetables, and tofu or other soy products that are made with calcium. When it comes to vitamin D, there aren’t a ton of foods that are naturally rich in it. Interestingly, yogurt and cheese aren’t usually rich in vitamin D. There is a small handful of vitamin D-rich foods, such as fatty fish, egg yolks, certain mushrooms exposed sunshine/UV-light, liver, and vitamin D-fortified milk alternatives. A note: vitamin D is commonly supplemented, even for those with no dietary restrictions. If your health care provider says your child needs a supplement, don’t worry, low vitamin D levels are common for infants, kids, and adults alike.58 Bottom line: don’t sweat it if your kid isn’t drinking milk; nutritionally, there are tons of other alternatives to offer.
For calcium, you can offer other calcium-rich foods to your child like yogurt and cheese, as well as plant-based sources of calcium like sesame, almonds, broccoli, other dark green vegetables, and tofu or other soy products that are made with calcium. When it comes to vitamin D, there aren’t a ton of foods that are naturally rich in it. Interestingly, yogurt and cheese aren’t usually rich in vitamin D. There is a small handful of vitamin D-rich foods, such as fatty fish, egg yolks, certain mushrooms exposed sunshine/UV-light, liver, and vitamin D-fortified milk alternatives. A note: vitamin D is commonly supplemented, even for those with no dietary restrictions. If your health care provider says your child needs a supplement, don’t worry, low vitamin D levels are common for infants, kids, and adults alike.58 Bottom line: don’t sweat it if your kid isn’t drinking milk; nutritionally, there are tons of other alternatives to offer.
There’s no definitive cap on breast milk intake (as there is for cow’s milk, for example). However, it’s important to make sure that breast milk isn’t coming at the expense of solid food. After your baby’s first birthday, the primary source of nutrition should be solid food. A good rule of thumb is to limit breastfeeding sessions to 3 to 4 times per 24 hours after your baby’s first birthday and to make sure you are not breastfeeding too close to the solid meals. It can help to think of treating breastfeeds as you would snacks.
For example, make sure you offer solids first, and then if you want to top off with breast milk, wait at least 20 minutes after the solid meal so your child doesn’t hold out for the breast and skip the meal. A breastfeed is about the equivalent of a meal or snack, so if you are breastfeeding on demand and your child isn’t eating well at the table, it’s very possible that it’s because too much breast milk is being consumed.
A breastfeed is about the equivalent of a meal or snack, so if you are breastfeeding on demand and your child isn’t eating well at the table, it’s very possible that it’s because too much breast milk is being consumed.
For more information on this topic, check out our video on feeding schedules and weaning.
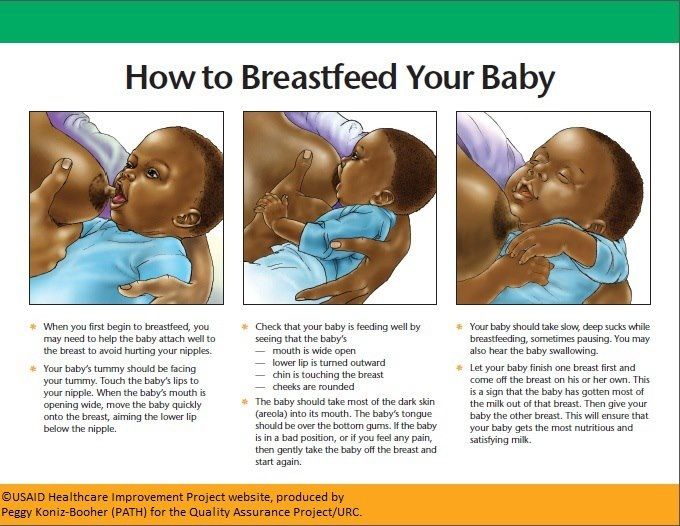
Is breast milk the same as other milks?Absolutely not. Breast milk is a very special food, because it is biologically active, meaning it contains unique components that support your baby’s growth, immunity, and gut health.59 Interestingly, its nutrient composition can also vary depending on a variety of factors, meaning its nutritional content fluctuates.60 Breast milk, or infant formula, is the ideal source of nutrition for a baby and should be a baby’s sole source of nutrition for the first 6 months of life. From 6-12 months of age, breast milk or formula should continue to be your baby’s primary beverage.
The nutritional composition of breast milk can vary based on a number of factors; some moms may produce fattier breast milk, while others may produce lighter breast milk – no breast milk is the same. What’s more, is that mom’s diet can also impact the nutrients and components found in breast milk, but more research is needed in this area.61 In general, breast milk may be lower in protein and other nutrients, but higher in fat (to provide plenty of calories to support baby’s growth), when compared to animal and plant-based milks. That said, the nutrients in breast milk are thought to be more available for absorption than other milks.62 63 In summary, no other milk, besides infant formula, can replace breast milk for an infant.
What’s more, is that mom’s diet can also impact the nutrients and components found in breast milk, but more research is needed in this area.61 In general, breast milk may be lower in protein and other nutrients, but higher in fat (to provide plenty of calories to support baby’s growth), when compared to animal and plant-based milks. That said, the nutrients in breast milk are thought to be more available for absorption than other milks.62 63 In summary, no other milk, besides infant formula, can replace breast milk for an infant.
How do you properly store breast milk?
The most important thing to keep in mind when storing breast milk is avoiding cross contamination with other foods. All containers for collection and storage of breast milk should be kept clean and sterile.
It is acceptable to store breast milk for up to 4 days in the refrigerator (preferably in the back of the refrigerator to prevent intermittent warming from the door opening).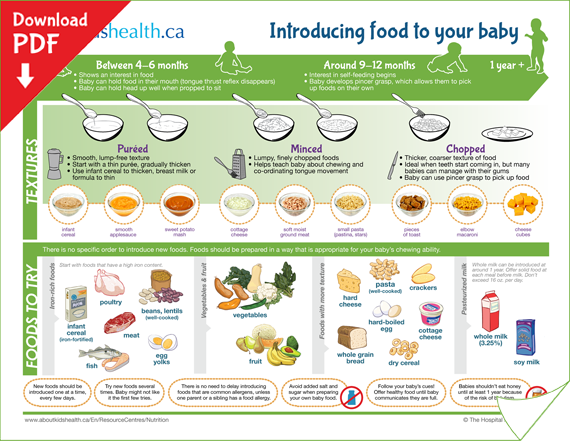 If you are going to freeze breast milk, try to freeze the fresh or refrigerated breast milk within 24 hours as the beneficial enzymes begin to change at approximately 25 hours. This doesn’t have to be a determining factor in the how quickly you freeze your refrigerated milk, but it’s worth consideration.
If you are going to freeze breast milk, try to freeze the fresh or refrigerated breast milk within 24 hours as the beneficial enzymes begin to change at approximately 25 hours. This doesn’t have to be a determining factor in the how quickly you freeze your refrigerated milk, but it’s worth consideration.
If not used within 72 hours, fresh breast milk should be transferred to the freezer in a clean, freezer-safe container and dated. While it is acceptable to store breast milk in a deep freezer with an attached refrigerator (0°F or −18°C) for up to 6 months and in a deep freezer (−4°F or −20°C) for up to 9-12 months, the sooner you use it, the better. Frozen breast milk lasts safely in the freezer for one month while preserving most of the nutrients, but after 3 months in the freezer, there is a noteworthy decline in concentrations of fats, calories and other macronutrients.
To thaw, plan ahead and defrost overnight in the refrigerator, and never on the counter. And because heating to excessive temperatures can greatly alter the nutrient quality, refrain from defrosting breast milk in the microwave or on the stove. Once breast milk is completely thawed, you have 24 hours to use it. And remember: breast milk does not have to be heated at all! Many babies will happily drink room temperature—or even cold—breast milk.
Once breast milk is completely thawed, you have 24 hours to use it. And remember: breast milk does not have to be heated at all! Many babies will happily drink room temperature—or even cold—breast milk.
Can you cook with breast milk?
Yes, though heat does alter the structure of breast milk. Some studies have suggested that when breast milk is heated to just 100.4°F (38°C)—slightly above body temperature—its proteins begin to break down. This means that even when we heat stored breast milk it can lose important immunologically “active” and digestive components that benefit babies.
While you lose some nutrients in the heating process, cooked breast milk still offers nutritional value, so if you want to cook with your breast milk, go for it. Just know it would be better just to add some fresh breast milk stirred into food after it has been cooked.
Note: If you intend to freeze the food you cook with breast milk, remember to only use fresh breast milk as it is not safe to refreeze breast milk.
My baby has gone on a nursing strike. What do I do?
A nursing strike can usually last a few days to a week, sometimes longer depending on the cause of the strike. Usually, it’s a normal part of infant development, but can also be caused by pain, teething, ear infection. Regardless of the underlying reason, it’s stressful! It’s important to note that the baby is not rejecting you or the milk, but just managing a different experience. Milk supply is fairly regulated and a few days of disruption won’t drastically impact your milk supply. Additionally, efficient breastfeeding babies will often spend less time extracting enough milk from the breast and expect a reduction in the number of nursing sessions as baby ages and increases solid food intake. Here are some ways to encourage baby back to the breast to continue your breastfeeding journey:
- If baby is distracted: nurse in a decreased stimulating environment (like a dark, quiet room), nurse while baby is drowsy or in the baby carrier, try the side lying position, and/or increase the amount of evening/night time nursing opportunities.

- If baby is congested or you suspect an ear infection/head cold: nurse in an upright position to help with nasal drainage and use breast compressions as needed to increase milk flow.
- Increase skin-to-skin or babywearing. This is particularly helpful if you suspect a pain-related reason for the nursing strike.
- If teething: try rubbing the gums with chilled breast/human milk and use teethers that reach back to the molars. Increasing skin-to-skin will also help with this.
Nursing strikes can also happen during pregnancy or menstruation/ovulation. In each of these cases, milk can take on a different flavor and supply naturally decreases.
Can you store formula in the refrigerator?
Yes. Similarly to breast milk, it is important to: avoid cross contamination with other foods, maintain clean surfaces, use sterile containers, keep the refrigerator at less than 41°F or 5°C, and preferably place the formula at the back of the refrigerator to avoid intermittent warming with door openings. 64 If formula is prepared from powder for later use, it should be covered and stored in the refrigerator immediately and is recommended to be used within 24 hours to avoid risk of foodborne illness. If using a ready-to-feed formula, once opened, it can be stored covered in the refrigerator for up to 48 hours. Formula that is left over from feeding your baby should not be stored in the refrigerator and should be thrown away as your baby’s saliva can contribute to the growth of bacteria.65
64 If formula is prepared from powder for later use, it should be covered and stored in the refrigerator immediately and is recommended to be used within 24 hours to avoid risk of foodborne illness. If using a ready-to-feed formula, once opened, it can be stored covered in the refrigerator for up to 48 hours. Formula that is left over from feeding your baby should not be stored in the refrigerator and should be thrown away as your baby’s saliva can contribute to the growth of bacteria.65
Can you cook with formula?
Yes, though similarly to breast milk, heating formula can also degrade certain nutrients and decrease the bioavailability (the usability) of certain vitamins and minerals.66 67 68
This can be avoided by adding prepared or powdered formula into foods after cooking. Up to 1 teaspoon of powdered infant formula can be sprinkled onto 4 ounces of soft or puree textured foods.69 Prepared formula can be used to thin out certain thicker consistency foods and stirred into other foods. That being said, we recognize that feeding your baby can feel overwhelming at times and we want to reassure you that it is completely fine to cook with prepared infant formula as it still provides calories, fat, protein, and other vital nutrients to help your baby thrive.
That being said, we recognize that feeding your baby can feel overwhelming at times and we want to reassure you that it is completely fine to cook with prepared infant formula as it still provides calories, fat, protein, and other vital nutrients to help your baby thrive.
When can babies drink water?
In small amounts, water may be introduced after 6 months of age. When babies consume water, it puts them at risk of inadequate intake of calories, protein, and essential nutrients. However, per the American Academy of Pediatrics, starting around 6 months of age—and as long as baby is growing and gaining appropriately—small amounts of water can be offered, although not usually required.
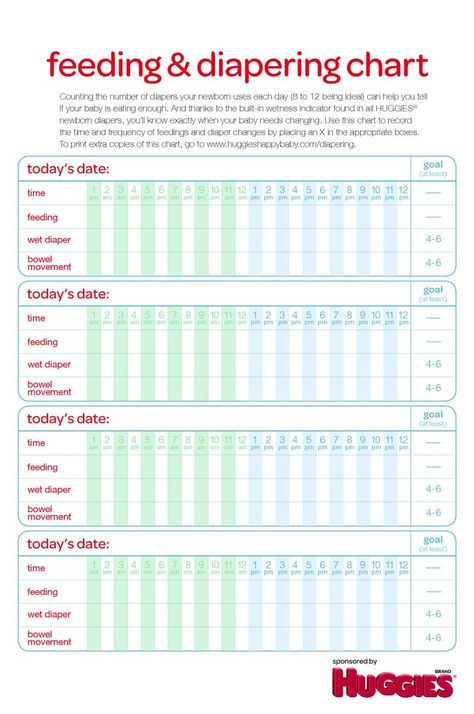
While the American Academy of Pediatrics suggests you can offer up to 8 ounces of water per day starting at 6 months old, it is our strong opinion that water should be limited to less than 2 to 4 ounces a day so it doesn’t displace valuable nutrition from breast milk or formula.70 If you’re concerned about your baby’s hydration status, you can monitor the number of wet diapers and energy levels and contact your pediatrician.
In short: no. Toddler formulas and “transition formulas” for the most part are not necessary for your child. What’s more, these toddler formulas do not face the same level of regulatory scrutiny as infant formulas.71 You can continue providing breast milk well into toddlerhood and offer cow’s milk at 12 months of age while focusing on providing a nutritious and diverse diet. Special supplemental drinks, like Pediasure, are not typically required for most toddlers unless there is a medical need. Either way, both of these options tend to have added sugars and preservatives, which are best to avoid where possible. As always, be sure to talk to your pediatric health care provider for more guidance and information on this.
Reviewed by:
V. Kalami, MNSP, RD, CSP
J. Truppi, MSN, CNS
R. Ruiz, MD, FAAP. Board Certified Pediatrician & Gastroenterologist
- Leung, A.
 K., & Sauve, R. S. (2003). Whole cow’s milk in infancy. Paediatrics & child health, 8(7), 419–421. https://doi.org/10.1093/pch/8.7.419
K., & Sauve, R. S. (2003). Whole cow’s milk in infancy. Paediatrics & child health, 8(7), 419–421. https://doi.org/10.1093/pch/8.7.419 - American Academy of Pediatrics, Cow’s Milk Alternatives.
- Mohamed H. Abd El-Salam & Safinaz El-Shibiny (2019) Reduction of Milk Protein Antigenicity by Enzymatic Hydrolysis and Fermentation. A Review, Food Reviews International, DOI: 10.1080/87559129.2019.1701010
- TZVETKOVA, I., DALGALARRONDO, M., DANOVA, S., ILIEV, I., IVANOVA, I., CHOBERT, J.‐M. and HAERTLÉ, T. (2007), HYDROLYSIS OF MAJOR DAIRY PROTEINS BY LACTIC ACID BACTERIA FROM BULGARIAN YOGURTS. Journal of Food Biochemistry, 31: 680-702.
- Healthy Children.org, Recommended Drinks for Young Children (website). Retrieved June 7, 2020
- Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- Leung AK, Sauve RS.
 Whole cow’s milk in infancy. Paediatr Child Health. 2003;8(7):419-421. doi:10.1093/pch/8.7.419
Whole cow’s milk in infancy. Paediatr Child Health. 2003;8(7):419-421. doi:10.1093/pch/8.7.419 - Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- Martin C, Ling P-R, Blackburn G. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5):279. doi:10.3390/nu8050279
- Martin C, Ling P-R, Blackburn G. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5):279. doi:10.3390/nu8050279
- Leung AK, Sauve RS. Whole cow’s milk in infancy. Paediatr Child Health. 2003;8(7):419-421. doi:10.1093/pch/8.7.419
- Samaneh, R., Pardis, A., Simin, M. Z., Mohammad K.J.(2020). Impact of Health Promotion Interventions on Early Childhood Caries Prevention in Children Aged 2–5 Years Receiving Dental Treatment Under General Anesthesia. Frontiers in Public Health.
 8, 6. DOI: 10.3389/fpubh.2020.00006. Retrieved October 25, 2021.
8, 6. DOI: 10.3389/fpubh.2020.00006. Retrieved October 25, 2021. - Leung AK, Sauve RS. Whole cow’s milk in infancy. Paediatr Child Health. 2003;8(7):419-421. doi:10.1093/pch/8.7.419
- Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- Giraldo, P. A., Shinozuka, H., Spangenberg, G. C., Cogan, N., & Smith, K. F. (2019). Safety Assessment of Genetically Modified Feed: Is There Any Difference From Food?. Frontiers in plant science, 10, 1592. https://doi.org/10.3389/fpls.2019.01592
- Welsh JA, Braun H, Brown N, et al. Production-related contaminants (pesticides, antibiotics and hormones) in organic and conventionally produced milk samples sold in the USA.
 Public Health Nutr. 2019;22(16):2972‐2980. doi:10.1017/S136898001900106X
Public Health Nutr. 2019;22(16):2972‐2980. doi:10.1017/S136898001900106X - Özen, S., & Darcan, Ş. (2011). Effects of environmental endocrine disruptors on pubertal development. Journal of clinical research in pediatric endocrinology, 3(1), 1–6. https://doi.org/10.4274/jcrpe.v3i1.01
- Making the Switch to Cow’s Milk for 1-year-olds. (2016). Retrieved from https://www.chop.edu/news/making-switch-cow-s-milk-1-year-olds
- Health Canada. (2014). Infant nutrition – Canada.ca. Retrieved from https://www.canada.ca/en/health-canada/services/infant-care/infant-nutrition.html
- Kleinman, Ronald, and Frank Greer. 2020. Pediatric Nutrition. 8th ed. American Academy of Pediatrics.
- My Plate. (n.d.). Dairy. Retrieved from https://www.myplate.gov/eat-healthy/dairy
- USDA. (2021). Dairy. MyPlate. https://www.myplate.gov/eat-healthy/dairy
- Allen, R., & Myers, A. (2006). Nutrition in Toddlers. Am Fam Physician, 1527–1532. Retrieved from https://www.
 aafp.org/afp/2006/1101/p1527.html#:~:text=A%20toddler’s%20diet%20should%20include,other%20dairy%20products%20per%20day.&text=Fat%20and%20cholesterol%20should%20not,children%20younger%20than%20two%20years
aafp.org/afp/2006/1101/p1527.html#:~:text=A%20toddler’s%20diet%20should%20include,other%20dairy%20products%20per%20day.&text=Fat%20and%20cholesterol%20should%20not,children%20younger%20than%20two%20years - Domellöf, M., Braegger, C., Campoy, C., Colomb, V., Decsi, T., Fewtrell, M., Hojsak, I., Mihatsch, W., Molgaard, C., Shamir, R., Turck, D., & van Goudoever, J. (2014). Iron Requirements of Infants and Toddlers. Journal of Pediatric Gastroenterology & Nutrition, 58(1), 119–129. https://doi.org/10.1097/mpg.0000000000000206
- Muth, N. (2019). Recommended Drinks for Young Children Ages 0-5. Retrieved from https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Recommended-Drinks-for-Young-Children-Ages-0-5.aspx
- USDA. (2020). Dietary Guidelines for Americans 2020–2025 (Ninth Edition). https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf
- Gropper, S., Smith, J.
 (2013). Advanced Nutrition and Human Metabolism, 6th ed. Independence, KS: Wadsworth Publishing, Cengage Learning.
(2013). Advanced Nutrition and Human Metabolism, 6th ed. Independence, KS: Wadsworth Publishing, Cengage Learning. - Oregon State University. Iron. (website) Retrieved June 12, 2020
- Weaver CM. Calcium. In: Erdman JJ, Macdonald I, Zeisel S, eds. Present Knowledge in Nutrition. 10th ed: John Wiley & Sons, Inc.; 2012:434-446.
- Oregon State University. Iron.(website) Retrieved June 12, 2020.
- Vanderhout, et al. American Journal of Clinical Nutrition, Whole milk compared with reduced-fat milk and childhood overweight: a systematic review and meta-analysis.(Website) Retrieved June 12, 2020.
- Bull World Health Organ, Foodborne Listeriosis. WHO Working Group. (Website) Retrieved June 12, 2020.
- Centers for Disease Control and Prevention. Raw Milk Questions and Answers. (Website) Retrieved June 12, 2020.
- GI Kids, North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Cow’s Milk Protein Allergy. (Website) Retrieved June 12, 2020.
- GiKids – Cow’s Milk Protein Allergy. (2020, February 26). GiKids. https://gikids.org/digestive-topics/cows-milk-protein-allergy/
- Wood, R. A., Sicherer, S. H., Vickery, B. P., Jones, S. M., Liu, A. H., Fleischer, D. M., Henning, A. K., Mayer, L., Burks, A. W., Grishin, A., Stablein, D., & Sampson, H. A. (2013). The natural history of milk allergy in an observational cohort. Journal of Allergy and Clinical Immunology, 131(3), 805-812.e4. https://doi.org/10.1016/j.jaci.2012.10.060
- https://gikids.org/digestive-topics/cows-milk-protein-allergy/
- https://www.kidswithfoodallergies.org/food-allergies-and-cross-reactivity.aspx
- https://gikids.org/digestive-topics/cows-milk-protein-allergy/
- https://gikids.org/digestive-topics/cows-milk-protein-allergy/
- https://www.kidswithfoodallergies.org/food-allergies-and-cross-reactivity.aspx
- https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Lactose-Intolerance-in-Children.
 aspx
aspx - Martin C, Ling P-R, Blackburn G. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5):279. doi:10.3390/nu8050279
- Lifschitz C, Szajewska H. Cow’s milk allergy: evidence-based diagnosis and management for the practitioner. Eur J Pediatr. 2015;174(2):141‐150. doi:10.1007/s00431-014-2422-3
- Martin C, Ling P-R, Blackburn G. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5):279. doi:10.3390/nu8050279
- Verduci, E., D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A., Landi, M., Trikamjee, T., & Peroni, D. G. (2019). Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739.
- Lifschitz C, Szajewska H. Cow’s milk allergy: evidence-based diagnosis and management for the practitioner. Eur J Pediatr. 2015;174(2):141‐150. doi:10.1007/s00431-014-2422-3
- Verduci, E.
 , D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A., Landi, M., Trikamjee, T., & Peroni, D. G. (2019). Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739.
, D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A., Landi, M., Trikamjee, T., & Peroni, D. G. (2019). Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739. - Verduci, E., D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A., Landi, M., Trikamjee, T., & Peroni, D. G. (2019). Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739.
- Verduci, E., D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A., Landi, M., Trikamjee, T., & Peroni, D. G. (2019). Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739.
- Medhammar E, Wijesinha-Bettoni R, Stadlmayr B, Nilsson E, Charrondiere UR, Burlingame B.
 Composition of milk from minor dairy animals and buffalo breeds: a biodiversity perspective. J Sci Food Agric. 2012;92(3):445‐474. doi:10.1002/jsfa.4690
Composition of milk from minor dairy animals and buffalo breeds: a biodiversity perspective. J Sci Food Agric. 2012;92(3):445‐474. doi:10.1002/jsfa.4690 - Bravi, F., Wiens, F., Decarli, A., Dal Pont, A., Agostoni, C., & Ferraroni, M. (2016). Impact of maternal nutrition on breast-milk composition: a systematic review. The American journal of clinical nutrition, 104(3), 646–662. https://doi.org/10.3945/ajcn.115.120881
- Oregon State University. Soy Isoflavones. (Website) Retrieved June 12, 2020.
- Ripple Products. (Website) Retrieved June 12, 2020.
- Verduci, E., D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A., Landi, M., Trikamjee, T., & Peroni, D. G. (2019). Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739.
- Verduci, E., D’Elios, S., Cerrato, L., Comberiati, P., Calvani, M., Palazzo, S., Martelli, A.
 , Landi, M., Trikamjee, T., & Peroni, D. G. (2019).Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739.
, Landi, M., Trikamjee, T., & Peroni, D. G. (2019).Cow’s Milk Substitutes for Children: Nutritional Aspects of Milk from Different Mammalian Species, Special Formula and Plant-Based Beverages. Nutrients, 11(8), 1739. - Haimi, M., & Kremer, R. (2017). Vitamin D deficiency/insufficiency from childhood to adulthood: Insights from a sunny country. World journal of clinical pediatrics, 6(1), 1–9. https://doi.org/10.5409/wjcp.v6.i1.1
- Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- Wu, X., Jackson, R. T., Khan, S. A., Ahuja, J., & Pehrsson, P. R. (2018). Human Milk Nutrient Composition in the United States: Current Knowledge, Challenges, and Research Needs. Current developments in nutrition, 2(7), nzy025. https://doi.org/10.1093/cdn/nzy025
- Bravi, F., Wiens, F., Decarli, A., Dal Pont, A., Agostoni, C.
 , & Ferraroni, M. (2016). Impact of maternal nutrition on breast-milk composition: a systematic review. The American journal of clinical nutrition, 104(3), 646–662. https://doi.org/10.3945/ajcn.115.120881
, & Ferraroni, M. (2016). Impact of maternal nutrition on breast-milk composition: a systematic review. The American journal of clinical nutrition, 104(3), 646–662. https://doi.org/10.3945/ajcn.115.120881 - Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- Saarinen, U. M., Siimes, M. A., & Dallman, P. R. (1977). Iron absorption in infants: high bioavailability of breast milk iron as indicated by the extrinsic tag method of iron absorption and by the concentration of serum ferritin. The Journal of pediatrics, 91(1), 36–39. https://doi.org/10.1016/s0022-3476(77)80439-3
- Redmond EC, Griffith CJ. The importance of hygiene in the domestic kitchen: Implications for preparation and storage of food and infant formula. Perspect Public Health. 2009;129(2):69-76. doi:10.1177/1757913908101604
- Centers for Disease Control. Infant Formula Preparation and Storage.
 Infant Formula Preparation and Storage. Published May 7, 2018. Accessed April 28, 2020.
Infant Formula Preparation and Storage. Published May 7, 2018. Accessed April 28, 2020. - Galán MG, Drago SR. Food matrix and cooking process affect mineral bioaccessibility of enteral nutrition formulas: Mineral bioaccessibility of enteral nutrition formulas. J Sci Food Agric. 2014;94(3):515-521. doi:10.1002/jsfa.6280
- García R, Alegría A, Barberá R, Farre R, Lagarda MJ. Dialyzability of iron, zinc, and copper of different types of infant formulas marketed in Spain. Biol Trace Elem Res. 1998;65(1):7-17. doi:10.1007/BF02784110
- Drago SR, Valencia ME. Influence of Components of Infant Formulas on in Vitro Iron, Zinc, and Calcium Availability. J Agric Food Chem. 2004;52(10):3202-3207. doi:10.1021/jf035191e
- University of California San Francisco Benioff Children’s Hospital. Adding Calories into Your Baby’s Food. (Website) Retrieved May 15, 2020.
- Muth N. Recommended Drinks for Young Children 0-5 years old. Published September 18, 2019. Accessed May 14, 2020.

- Pomeranz, J. L., Romo Palafox, M. J., & Harris, J. L. (2018). Toddler drinks, formulas, and milks: Labeling practices and policy implications. Preventive medicine, 109, 11–16. https://doi.org/10.1016/j.ypmed.2018.01.009
Dairy for Baby - Introducing Milk, Yogurt, Cheese for Baby. Frequently Asked Questions about giving babies Dairy
Commonly Asked Questions about Offering Dairy, like Yogurt and Cheese, to Your Baby
Many parents wonder when they can offer their babies dairy products such as yogurt and cheese. Some common questions are: “Should I give my baby full fat dairy products?” and “Can I use milk in recipes that my baby will be eating?”
On this page you will find a compiled a list of common questions and answers concerning giving your baby yogurt and cheese and dairy products in general.
If you do not see your question here, please contact us. If we cannot answer your question about offering your baby dairy products, we will point you in the direction of someone who may. We are always eager to add information to this site. The more information that we have based on your questions, the more informed our visitors will be.
We are always eager to add information to this site. The more information that we have based on your questions, the more informed our visitors will be.
Homemade Baby Food – Dairy FAQs
Why can I introduce Yogurt earlier than 12 months?
Yogurt may be introduced as early as 6 months old, (the typical age recommendation is 8 months old) depending on your baby’s pediatrician and your baby’s propensity to allergies.
Here are 2 reasons why introducing Yogurt (and cheese) is different than introducing milk:
- Unlike a Whole Cow Milk beverage, your baby is not at risk of formula/breast milk being replaced by Yogurt or Cheese. The medical community worries that if Whole Cow milk is introduced to an infant prior to 1 year old, that parents would stop formula and/or breastfeeding and use Milk as the replacement. This would be dangerous to your baby’s health.
- Lactose is already broken down with the culturing of the yogurt or cheese and milk proteins are either removed or limited thus it is typically easier to digest; people with lactose intolerance often are be able to handle cheese and/or yogurt without trouble.
 The same is true for some people with a milk protein (either to the casein or the whey) allergy.
The same is true for some people with a milk protein (either to the casein or the whey) allergy.
Yogurt is a great way for baby to get calcium and the “bacteria” in yogurt that is so good for our digestive systems. Yogurt is also a great way for baby to get the fat that is so highly needed during baby’s first year. The majority of yogurts on the market are made low fat or non fat but babies need the fat!
Can I Use Milk in Recipes?
Using milk in a baked good recipe, like offering yogurt and cheese, will not risk weaning your baby to milk from formula and/or breast milk. Milk in a baked good, or otherwise cooked recipe is considered safe for the baby who is 7-8 months of age+ and who has no familial history of dairy allergies.
When Can I Introduce Cheese to my Baby?
Cheese is very good for baby and may be introduced as early as 8 months providing there are no dairy allergies; start by offering the lighter tasting cheeses (Colby, Jack, American).
If baby cannot mash/grasp, melt cheeses over vegetables or add to veggie/meat purees. If baby can mash/grasp and has had Baby Finger Foods, cut cheeses into small bits and offer to baby as a snack.
Cheeses also may be offered via the old classic grilled cheese sandwich or mac-n-cheese – again, this will be dependant on how baby is with mashing/grasping other foods.
Learn more about Feeding Cheese to Baby
Why Should I Wait Until After 12 Months to Introduce Milk as a Drink?
One of the main reasons you should wait until after baby is 1 year old to introduce milk as a formula/breast milk replacement is that milk/dairy hinders the absorption of iron in the body. Milk is also much harder for baby to digest than breast milk or infant formula.
Milk by itself does not contain all the nutrients of breast milk or formula and should never be used as a substitute until after 1 year of age. The cooking of the food that contains the milk will aid in breaking down the milk proteins so that many babies who are 8 months+ are able to have baked goods that contain milk.
As noted on our solid food chart for the 4-6 month old baby, we indicate that dairy should not replace breast milk or formula until a baby is 12 months of age. There is a possibility of serious health risks should breast milk and/or formula be replaced with cow milk, particularly at the 4-6 month age range.
These risks include Iron Deficient Anemia. Cow milk hinders the absorption of Iron and can cause anemia. Iron is crucial for baby’s healthy development. Besides the risk of iron deficient anemia, if your baby drinks cow milk to replace breast milk and/or formula, baby will not receive enough Vitamin E or enough EFAs (essential fatty acids). These nutrients are also crucial to healthy growth and development.
Your baby would also receive levels of protein and sodium that would be too high for baby’s fragile system to handle. Cow milk protein is very difficult for an infant to digest and absorb. While formula may be cow milk based, the proteins are “pre-digested” and cultured in a way that make baby’s tummy better able to tolerate them. Believe it or not, the levels of sodium (and potassium) in cow milk are very high. Too much sodium might cause an infant’s kidneys to fail and as we know, high levels of sodium can lead to high blood pressure.
Believe it or not, the levels of sodium (and potassium) in cow milk are very high. Too much sodium might cause an infant’s kidneys to fail and as we know, high levels of sodium can lead to high blood pressure.
These are a few of the reasons why the AAP and other pediatric authorities do not want babies to drink milk as a replacement until 12 months of age. As you know, breast milk is the most perfect food for infants and babies could survive on breast milk alone for the first 12 months. Formula, while not nature’s perfect food like breast milk, has been created with the crucial and essential nutrients that an infant needs to grow healthy and maintain a proper nutritional status. Whole cow milk does not provide for the good health and growth of babies.
What About Dairy Allergies?
If you, your family members or your baby have a history of allergies to milk (to the milk protein) and/or a history of lactose intolerance; introducing dairy in any form prior to 1 year is probably not a good idea.
As most babies can outgrow these types of allergies, if you hold off until after 1 yr, the risk of developing these allergies is significantly decreased.
Also note that an infant who has a true allergy to the milk protein(s) may also have allergies to other foods – soy being one of the most common. Learn more about Dairy Allergies and other Allergy information
Delaying the introduction of cow milk or other food products may not be favorable in preventing the development of atopy. A study in 2008 (Dairy Introduction past 9 months ) showed that more delay in introduction of cow milk products was associated with a higher risk for eczema.
Are You Sure Baby Should Have Full-Fat Dairy Products?
Your baby needs fats. One of the reasons why formula and breast milk are so nutritious is due to the high fat content. Fat and fatty acids are essential for brain development to name one reason.
DO NOT GIVE baby 2%, 1% or low fat dairy products until after 2 years old unless you are otherwise instructed by your baby’s doctor.
Some doctors recommend waiting to give lower fat dairy products until after the baby has turned 3 years old.
For more information about Diary products, click below:
Yogurt & Your Baby – In depth Information about giving your baby yogurt.
Learn About Updated Lactose Intolerance Statements from the AAP
Feeding Cheese to Your Baby – Read about Cheese for Your Baby – Ideas
Remember, always consult with your pediatrician regarding introducing solid foods to your baby and specifically discuss any foods that may pose allergy risks for your baby.
This site complies with the HONcode standard for trustworthy health information:
verify here.
SHARE ON FACEBOOK SHARE ON PINTEREST
From 6 months and older - what dairy products should be given as complementary foods to young children
From the age of six months, you can gradually introduce complementary foods: cereals, mashed potatoes, vegetable mixtures, and, of course, dairy products, because this is one of the main sources of calcium, as well as many vitamins.
In this article, we will talk about dairy products that pediatricians recommend giving to young children as complementary foods.
What you need to know about baby food
Milk bought on the market can be a source of infectious diseases and a huge amount of harmful bacteria. The cow may be infected, and hygiene standards during milking and bottling may have been repeatedly violated.
· Manufacturer's baby milk products are ideally suited to the needs of young children. Raw milk, in turn, is not adapted to the needs of the child's body - for example, it contains too high levels of sodium and protein.
· In early childhood, it is not so much how much dairy products you give your child that matters, but how well these products are balanced in mineral composition and meet the needs of the child's body. For example, the absorption of calcium is directly related to the presence of other vitamins and trace elements. At the same time, if you give your baby a lot of milk or kefir, this can lead to an overload of milk protein.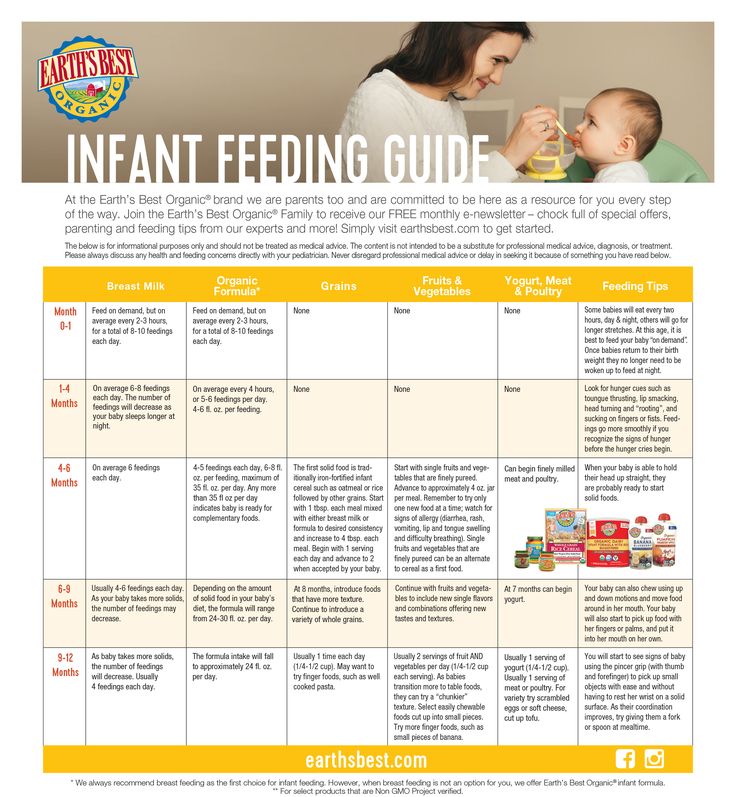
Fortunately for today's mothers and fathers, if compared with Soviet times, modern dairy products manufacturers have gone far ahead.
· First of all, modern children's cereals and curds are made in accordance with all requirements and norms. It is especially worth paying attention to manufacturers who export products to the EU countries. The fact that the company's products are approved for export to Europe indicates high quality and safety.
· Secondly, children's products are made taking into account the needs of the child's body. In the process of development, they are being researched at the Institute of Hygiene and Medical Ecology. O. M. Marzeev of the National Academy of Medical Sciences of Ukraine, and only after that are recommended for production.
· Thirdly, for young parents, baby milk nutrition is a way to save time and effort, while providing the child with everything necessary for good nutrition and development.
Baby food for different age groups
So, what dairy products can be given to babies as complementary foods? Depends on the age and preferences of the baby.
6 months
· From the age of six months, ready-made milk porridges can be introduced into the diet. The advantage of such cereals is that they do not need to be cooked - just open and give to the child. Young parents, exhausted by many months of sleep deprivation, will appreciate this advantage. When choosing cereals, keep in mind that gluten-rich cereals (oatmeal, semolina) should be given to a small child with great care, as gluten can cause intestinal problems.
· From the age of 6 months, for nutrition and complementary foods, you can start giving your baby branded sour-milk cottage cheese. It is important that children's cottage cheese (as well as other children's products) be produced on closed-cycle equipment - that is, one where human intervention is minimal.
· Also, from this age, you can give your baby curd pastes with fruit and vegetable fillings. It is desirable that fruits and vegetables are "native" to Ukraine - blueberries, raspberries, apples, peaches, carrots, watermelon, and others.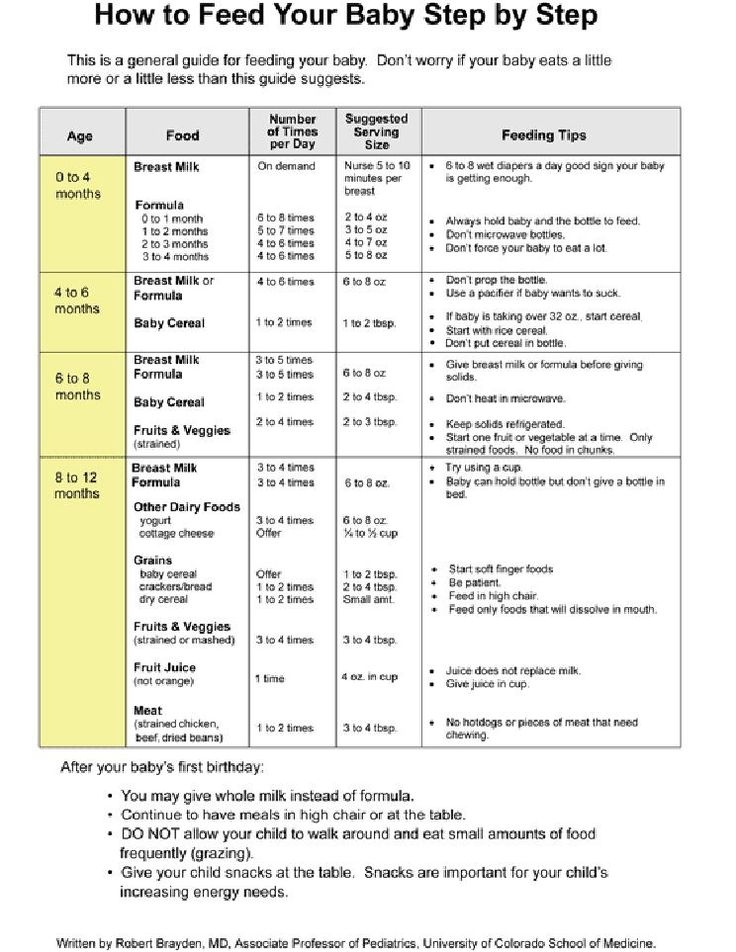 The exception is a banana - firstly, this fruit does not cause allergies, and secondly, it is great as a first feeding for babies. It is preferable that the curd paste be made on the basis of fructose (insulin is not needed for its absorption), without sucrose.
The exception is a banana - firstly, this fruit does not cause allergies, and secondly, it is great as a first feeding for babies. It is preferable that the curd paste be made on the basis of fructose (insulin is not needed for its absorption), without sucrose.
8 months
From the age of eight months, dairy products that can be given to a baby become more diverse - now kefir, yogurt, sourdough can be introduced into the diet.
· It is important to give kefir and sourdough specifically for “children”, as these are adapted products, and “adult” kefir may not be suitable for a child. Kefir and sourdough should be introduced as complementary foods after the baby has become acquainted with cereals, cottage cheese and other children's food. Ideally, these foods are fortified with vitamins (A, D, E). It is important to understand who kefir and sourdough are radically different products, with different content of lactic microorganisms and taste.
· Fruit and vegetable yoghurts for children can be introduced from 8 months. As with cottage cheese pastes, it is preferable that fruits and vegetables are “native” to Ukraine - blueberries, raspberries, apples, peaches, carrots, watermelons (banana is an exception).
As with cottage cheese pastes, it is preferable that fruits and vegetables are “native” to Ukraine - blueberries, raspberries, apples, peaches, carrots, watermelons (banana is an exception).
9 months
· From the age of nine months, children are recommended UHT milk, produced specifically for children. Such milk can be stored from 10 days (in a bottle) to 90 days in a Tetra Pak package, while retaining all useful vitamins and minerals. An interesting fact: only very high quality milk can be used for ultra-pasteurization, otherwise it simply will not go through the process of high heat treatment. Therefore, in order to produce ultra-pasteurized milk, an enterprise must be very careful in the selection of suppliers - work with reliable farm suppliers, and not with the population, whose quality of raw materials is much lower.
When introducing complementary foods, the recommendations of the paediatrician are paramount. However, it is also important to follow the manufacturer's recommendations on the label and observe the baby's reaction to each new product. The label should say "no colorants, no preservatives, no GMOs", for yoghurts and curd spreads - "does not contain sucrose". When choosing milk cereals, pay attention to the gluten content. Also keep in mind that baby food should be consumed immediately after opening, it is unacceptable to use the leftovers of the product in the next feeding.
The label should say "no colorants, no preservatives, no GMOs", for yoghurts and curd spreads - "does not contain sucrose". When choosing milk cereals, pay attention to the gluten content. Also keep in mind that baby food should be consumed immediately after opening, it is unacceptable to use the leftovers of the product in the next feeding.
TM "Yagotynske for children" has launched a new product on the market - ready-made milk porridges: milk-rice, milk-wheat and milk-buckwheat. This new product will become an indispensable assistant for parents, because milk porridges are completely ready to eat. That is why, they will allow parents to spend their time not on cooking for the baby, but on their favorite thing.
Dairy products in children's nutrition / When and what to introduce, how much to give - an article from the "Healthy habits" section on Food.ru
From birth to one year: formula milk
If a mother is breastfeeding a child, but he is not gaining weight well, the pediatrician will offer to transfer him to mixed feeding, and if lactation has stopped, to artificial.
In the reference book on children's diet, edited by I. Vorontsov and A. Mazurin ("Medicine", 1980), we read:
"... any attempt to feed a child with the milk of another biological species is, in essence, an ecological disaster for this child" .
Modern medicine and the food industry can significantly mitigate this threat to babies. We are talking about adapted, that is, as much as possible similar in composition to breast milk, milk mixtures. They are:
-
highly adapted;
-
less adapted;
-
partially adapted.
Famous pediatrician Evgeniy Komarovsky says:
“...it doesn't mean that some mixtures are better and some are worse. The composition of mother's milk changes with the age of the child, and manufacturers take this into account.
Consult your pediatrician. Having bought the mixture, let the child try it according to the scheme proposed by the doctor.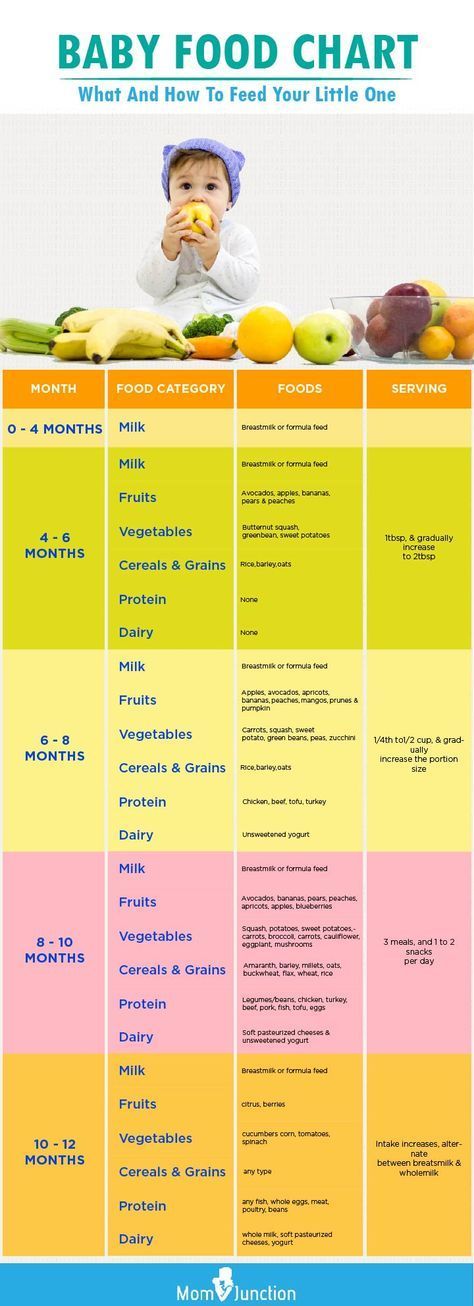 If the feeding went well, the child has no allergic reactions and the stomach does not hurt, enter the mixture according to the instructions.
If the feeding went well, the child has no allergic reactions and the stomach does not hurt, enter the mixture according to the instructions.
Many children do not tolerate the transition from one formula to another. A well-known specialist in baby nutrition, Professor Igor Kon, argued that children receiving adapted milk formulas do not need early introduction of additional complementary foods, as they receive all the necessary fats and proteins, vitamins and minerals with them.
By the way
Don't be surprised to find palm oil in infant formula. It contains a lot of palmitic acid, which is necessary for the formation of the baby's brain, which is also found in breast milk. The highest quality palm oil is used in infant formulas.
The first year of life: fermented milk products in the diet
The first introduction of kefir and other fermented milk products into the diet of infants in Russia began in 1922, when the first dairy kitchen was opened at the Institute for Maternal and Child Health.
The benefits of fermented milk products in the diet of children have long been known, they:
-
inhibit the growth of pathological intestinal microflora;
-
stimulate the immune system;
-
improve intestinal motility;
-
are suitable for children who are allergic to milk.
However, Russian pediatricians recommend introducing fermented milk products into a child's diet no earlier than at 8 months. It is believed that before this age, the child's gastrointestinal tract is not yet mature enough to digest milk proteins.
Despite the benefits of fermented milk products, there should be few of them in the diet of a child of the first year of life: no more than 200 g of baby kefir or yogurt and no more than 50 g of baby curd per day.
It is worth paying attention to one of the new functional products for baby food - biolact. According to the recipe, lactic acid bacteria are used for its preparation, and not fungi, as is the case with kefir.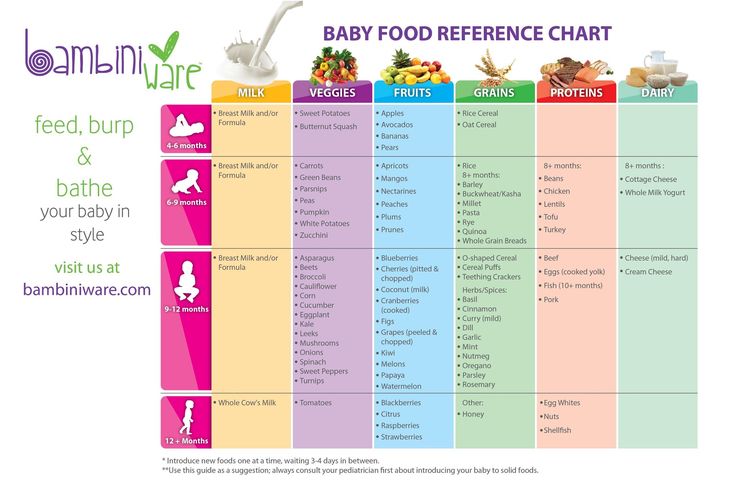 It contains all the essential amino acids and is rich in easily digestible calcium, which is necessary for the formation of the skeleton and teeth.
It contains all the essential amino acids and is rich in easily digestible calcium, which is necessary for the formation of the skeleton and teeth.
A common question asked by parents in the first year of a baby's life is whether adult dairy products can be included in the children's diet?
As practice shows, many too early transfer the child to "adult" milk for reasons of economy. But this cannot be done.
It has been proven that the consumption of milk from farm animals in children under 1-2 years of age leads to iron deficiency anemia. The fact is that the main protein in cow's milk, casein, damages the intestinal mucosa. This leads to subtle bleeding, but gradually the baby's body is deprived of iron. The child becomes lethargic, weak, often gets sick, develops more slowly, he is drawn to eat inedible objects like sand. That is why it is better to give a child up to a year of iron-fortified mixtures.
Early introduction of cow's milk can also lead to an allergy to it, which develops in 25% of children who received cow's milk before the age of one.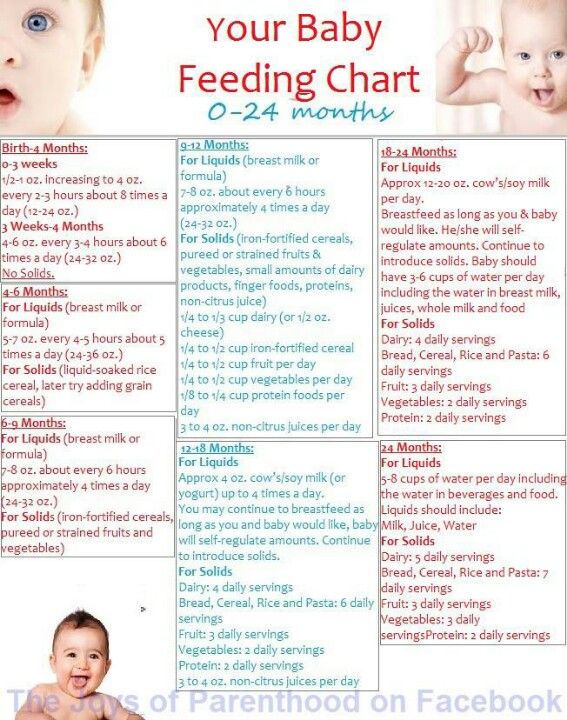
Cow's milk is high in sodium, which increases the burden on the child's kidneys. Also, too early introduction of "adult" dairy products into the children's diet contributes to obesity and insulin resistance.
From one to three years: "adult" dairy products in the diet of a child
Cow's milk can appear in the diet of a child only when he reaches 1-3 years, in an amount of not more than half a liter per day. As the baby grows, more milk and dairy products should be introduced.
Milk is an important source of calcium that a child needs to strengthen bones and teeth. According to the Nutrilife study, which is devoted to the study of the nutrition of Russian children aged 1-3 years, 60% of them have a calcium deficiency.
The Union of Pediatricians of Russia believes that the diet of a 1-3 year old child should include at least three servings of milk and dairy products.
Scientific evidence shows that if a child does not form sufficient bone mass by puberty, in adulthood he will suffer from osteoporosis. A serving of yogurt or cheese covers 30% of the daily calcium requirement, while a serving of salmon - 18%, broccoli - only 2%.
A serving of yogurt or cheese covers 30% of the daily calcium requirement, while a serving of salmon - 18%, broccoli - only 2%.
Milk and dairy products are an important source of vitamin D, which is deficient in most children. So, when employees of the Laboratory of Vitamins and Minerals of the Federal State Budgetary Institution "Federal Research Center for Nutrition and Biotechnology" in Moscow examined 360 children aged 10 to 17 years. It turned out that vitamin D deficiency was detected in more than 92% of children.
From five to seven: cow's milk instead of soy milk
Milk and dairy products help children achieve their genetic growth potential. A Canadian study published in The American Journal of Clinical Nutrition found that children whose parents gave them soy milk instead of cow's milk were lower than children who received all the essential amino acids from cow's milk.
Since 2005, the School Milk international program has been operating in Russia, in which schoolchildren of grades 1-4, and in some regions, all grades participate.