Why is it so hard to feed my baby
Why Your Baby Won't Eat
Reviewed by Dan Brennan, MD on November 23, 2022
It's just a fact of life: "Children come equipped to reject new foods," says Elizabeth Ward, MS, RD, author of The Complete Idiot's Guide to Feeding Your Baby and Toddler. To help your baby accept new foods, start with tiny portions. Also try to make new food look similar to a familiar favorite. If they like pureed carrots, try pureed sweet potato.
Cereal on the floor and peas in baby's hair? Congratulations, your little one is showing signs of independence. At about 9 months, many babies start wanting to control feeding time and where they put their food. While it may be hard to sit back and watch the mess grow, take heart, this is an important step for your baby's learning, growth, and self-reliance.
It's normal for babies to spit up a little, especially newborns. Babies' digestive systems are still developing. Babies can also get reflux, which is when food in the stomach backs up into the esophagus. To help manage reflux, try feeding your baby more slowly or feed them less at each sitting, loosening their diaper, and keeping them upright after they eat. Reflux almost always resolves without treatment by 12-14 months of age.
You offer your little one a bit of food and they turn their head, swat at the spoon, or clamp their mouth shut. Babies refuse to eat every now and then for lots of reasons: They're tired, sick, distracted, or just full. Don't force-feed your baby, but do talk to your child's doctor if you're worried.
While picky eating may linger for weeks, even months, it rarely lasts. Your baby can become a picky eater for lots of reasons, says Ward. When babies aren’t feeling their best -- like when teething -- familiar foods provide comfort. Or maybe your baby just isn't ready to try a new food. Make sure you don't give the baby junk food just because that's all they want. Offer healthy foods, and a hungry baby will eventually eat them.
Up to 8% of children have food allergies. Symptoms such as rash, diarrhea, vomiting, or stomach pain can show up suddenly. Though kids can be allergic to any food, milk, nuts, eggs, soy, wheat, and shellfish are the most problem foods. Food intolerances are more common than allergies and may cause gas, bloating, and belly pain. If you suspect a food allergy, work with your child's doctor to find safe foods.
Symptoms such as rash, diarrhea, vomiting, or stomach pain can show up suddenly. Though kids can be allergic to any food, milk, nuts, eggs, soy, wheat, and shellfish are the most problem foods. Food intolerances are more common than allergies and may cause gas, bloating, and belly pain. If you suspect a food allergy, work with your child's doctor to find safe foods.
As many as 2 out of 5 babies cope with colic -- crying for hours at a time. Colic can start when a baby is 3 weeks old and usually goes away by their 3rd month. While colic won't affect your baby’s appetite or ability to suck, a colicky baby may need time to calm down before they eat. And they may be inclined to spit up a little once they do. However, call their doctor about vomiting, diarrhea, fever, weight loss, or blood or mucus in their stool. These are not symptoms of colic.
Diarrhea can quickly lead to dangerous dehydration. Signs include dry mouth, decrease in urination or wet diapers, no tears with crying, weight loss, lethargy, or sunken eyes. All are worth a call to baby’s doctor.
All are worth a call to baby’s doctor.
Babies are rarely constipated. And it can be hard to tell if they are because how often babies have bowel movements can vary. For example, babies who only breastfeed may have a firm stool just once a day. Signs of constipation include hard stools that can be large and painful, and blood around the stool. Before trying home remedies, talk to your baby's doctor.
Is jarred baby food the cause of your baby's digestive issues? It could be if you feed them directly from the food jar and save the leftovers for another meal. Doing that can introduce bacteria from your baby's mouth into the food where it waits until the next time your baby eats it. When baby eats the leftover food it can lead to tummy trouble such as vomiting, diarrhea, and other symptoms.
Sometimes mom and dad may be the source of baby's feeding problem. "There's a temptation to give older infants the same foods you're eating," says Ward. But that's never a good idea if what you're eating is junk. Start giving baby sweet, salty, or fatty foods now and it'll be hard to keep break your child's unhealthy eating habits when they are a toddler.
Start giving baby sweet, salty, or fatty foods now and it'll be hard to keep break your child's unhealthy eating habits when they are a toddler.
A baby's undeveloped gastrointestinal system can't deal with some foods that an adult's body can. Honey, for example, may lead to infant botulism, which can be fatal. Always steer clear of chunky foods that pose choking hazards such as popcorn, hot dogs, raw fruits and veggies, raisins, and meat or cheese chunks.
Because so many things could be causing your baby's feeding problems, it's a good idea to talk to your doctor if you're worried. Always call your child's pediatrician right away if your baby is losing weight; if they gag or vomit when they have certain foods; if you suspect diarrhea, dehydration, or constipation; or if you think they have reflux. You shouldn't feel shy about talking with your child's doctor if you have any questions or concerns.
IMAGES PROVIDED BY:
1) Pixtal Images / Photolibrary
2) Christoph Ermel / iStock
3) Julian Winslow / Ableimages
4) Harald Eisenberger / LOOK
5) Ryan McVay / Stone
6) Kevin RL Hanson / DK Stock
7) Terry Vine / Blend Images
8) SimplyMui Photography / Getty
9) Betsy Van Der Meer / Taxi
10) Peter Cade / Iconica
11) Jason Edwards / National Geographic
12) Purestock / Getty
REFERENCES:
Elizabeth Ward, MS, RD, registered dietitian; author, The Complete Idiot's Guide to Feeding Your Baby and Toddler.
Piette, L. Just Two More Bites: Helping Picky Eaters Say Yes to Food, Three Rivers Press, 2006.
American Academy of Pediatrics. Caring for Your Baby and Young Child: Birth to Age 5, Bantam Books, 2009.
Children's Hospital Boston: "Newborn Gastrointestinal Problems."
National Digestive Diseases Information Clearinghouse, National Institutes of Health: "Gastroesophageal Reflux in Infants."
National Society for Pediatric Gastroenterology, Hepatology, and Nutrition: “Pediatric Gastroesophageal Reflux Clinical Practice Guidelines.”
Mackonochie, A. The Practical Encyclopedia of Pregnancy, Babycare and Nutrition for Babies and Toddlers, Lorenz Books, 2006.
National Institutes of Health: "Food Allergy."
American Academy of Family Physicians: "Feeding Problems in Infants and Children."
KidsHealth.org: "Your Colicky Baby."
ADD American Academy of Pediatrics, healthychildren.org: "Diarrhea" and "Constipation"
Children's Hospital Boston: "Newborn Gastrointestinal Problems. "
"
American Dietetic Association: "Don't Feed Baby from the Jar," "Introducing Solid Foods."
Dr. Greene.com: "Honey and Infant Botulism."
The New York Times: "Labels Urged for Foods That Can Choke."
Children's Physician Network: "Picky Eaters."
© 2022 WebMD, LLC. All rights reserved. View privacy policy and trust info
Causes, Emergency Care, and Treatments
“Poor feeding in infants” is a term used to describe an infant with little interest in feeding. It can also refer to an infant who is not feeding enough to receive the necessary nutrition required for adequate growth.
Poor growth associated with lack of feeding can lead to a separate condition called failure to thrive.
Poor feeding is caused by a variety of factors. It differs from picky eating, in which a baby may reject one form of milk for another or a toddler may refuse certain foods.
No matter the precise cause of poor feeding, undernutrition is a top concern. In fact, the World Health Organization (WHO) estimates that 45 percent of child deaths are related to undernutrition.
It is important not to dismiss poor feeding as something that will improve over time. This is a critical point in your child’s life, and missing key nutrients can lead to physical and cognitive concerns.
One of the most common causes of poor feeding is premature birth. Premature babies are typically poor feeders because they often have not yet developed the skills needed to suck and swallow milk.
Still, feeding usually increases as baby grows. If your little one was born prematurely and still has feeding trouble after leaving the hospital, it’s important to continue following up closely with your pediatrician, particularly if feeding concerns worsen or do not improve.
Other causes include congenital conditions such as jaundice and infections such as viral gastroenteritis. Once these conditions are treated, poor feeding usually subsides.
Serious conditions
Poor feeding can also be caused by serious conditions, such as Beckwith-Wiedemann syndrome. This is an overgrowth syndrome that causes infants to be particularly large and grow at a considerably fast pace. It affects an estimated 1 in 13,700 newborns worldwide.
It affects an estimated 1 in 13,700 newborns worldwide.
Other serious conditions include:
- congenital hypothyroidism, which occurs when the thyroid fails to develop or function properly
- other genetic conditions, including Down syndrome
- hypoplastic left heart, a rare condition that occurs when the left side of the heart fails to develop properly and is unable to pump blood to the body
- other heart defects
Less serious conditions
Other causes of poor feeding aren’t related to a congenital condition at all. Temporary illnesses can make feeding uncomfortable (and even painful) for infants.
Common ailments that get in the way of feeding include:
- diarrhea
- ear infections
- coughs and colds
- teething
When in doubt, it’s always best to double-check with a pediatrician. You don’t want to assume a minor illness when in fact there could be a serious underlying condition.
Feeding difficulty is a serious matter. When accompanied by other symptoms, emergency care may be required. Seek immediate medical attention if your baby is showing any of the following signs:
When accompanied by other symptoms, emergency care may be required. Seek immediate medical attention if your baby is showing any of the following signs:
- has a fever of over 100°F (37.8°C), an emergency in babies 3 months old and younger
- is vomiting after every feeding
- is vomiting blood
- has a cough with breathing difficulties
- is crying constantly
- has bloody stool
- is wheezing
- is becoming unresponsive to touch
Poor feeding that is caused by an infection will usually stop when the infection is resolved.
Treatment of poor feeding depends on the cause. This can involve changing the feeding schedule to consist of smaller, more frequent meals. If a milk-based intolerance is suspected, your doctor will work closely with you to find a formula and feeding plan that suits your baby.
While serious cases of poor feeding require prompt medical care, other causes can be resolved at home with the advice of a pediatrician.
If your baby is breastfeeding or chestfeeding, try to avoid:
- certain medications that can enter breast milk
- applying lotions and other skin products to your breasts
- high levels of stress — this may also make your milk taste differently
Other considerations may concern formula feeding as well as infants who have started solid foods.
Formula feeding
While breastfeeding is the method of feeding for infants recommended by health agencies such as WHO, it is a fact that not all babies are successful with this method — and not all nursing parents may want or be able to breastfeed.
If your baby doesn’t seem to latch on despite repeated attempts, you may consider talking with your doctor about formula feeding. You may still be able to try breastfeeding or chestfeeding, even when supplementing with formula, if you’d like.
The key is that your baby gets adequate nutrition. A lactation consultant may be helpful, if available to you.
“Picky eating”
After baby reaches 6 months of age, your pediatrician may encourage you to introduce solids to their diet. While solids shouldn’t replace breast milk at this phase of your child’s life, most infants require additional nutrients around the 6-month mark.
Examples include:
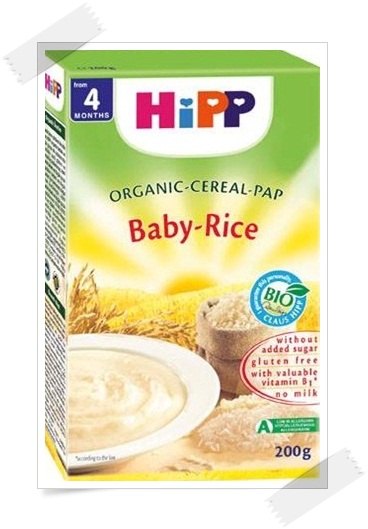
- rice cereal
- pureed fruits and vegetables
- pureed or soft meats
Introducing solid foods can be exciting for both caregiver and child. However, some infants don’t take to solids as readily as other babies.
This can be alarming, but the issue may be solved by:
- mixing cereal with solid foods
- offering solids in small increments
- only giving solids two to three times per day
- starting with one food at a time, then introducing others as your baby gets used to solids
When an infant doesn’t like solids, it’s easy to jump to the conclusion that they are a “picky eater.” However, this phase doesn’t usually start until your baby becomes a toddler.
Stress management
When your baby is eating poorly, it’s easy to get stressed out. This is especially true for new parents who may not yet know the distinctions between serious conditions and minor feeding concerns.
Remember that stress can worsen feeding concerns. It may interfere with attempts at feeding if your infant senses something is wrong.
Managing your stress won’t treat all causes of poor feeding, but it can help in many cases.
It’s difficult to find time for yourself during this busy stage of your life — even a few minutes a day can help. When you feel stress coming on during feedings, take a moment for some deep breathing.
Poor feeding in infants can lead to serious issues, such as malnutrition and stunted growth. It is essential that babies consume and digest the necessary nutrients to thrive and develop.
Any infant who is feeding poorly should be taken to a pediatrician for evaluation. After a proper diagnosis, treatment may be necessary.
In other cases, poor feeding can be resolved through refined techniques and perseverance at home. If you suspect feeding difficulties may be causing other concerns, call a doctor right away.
Breastfeeding and postpartum depression: stories of mothers with unsuccessful breastfeeding experiences
What could be more natural than breastfeeding? But sometimes there are problems with this. We collected the stories of mothers who went wrong and analyzed them together with the lactation consultant, obstetrician-gynecologist Anastasia Markova.
“I thought I’d rather give birth again than put her to my breast”
Ksenia Zheglaya, producer of the Normal Songs for Children project:
After giving birth, my daughter and I were in different wards — accordingly, she was brought to me strictly on time. Thoroughly fed, well-fed and satisfied. She showed no interest in mother's milk. Plus, each nanny had her own signature joke. One of us scolded us all the time: “Mommies, you work very poorly, you don’t try hard. ” The second shoved her breast into the child’s mouth and shouted: “Yes, it hurts! And what did you think, gave birth - and that's it? You are a woman, be patient." And all this against the background of nerves, a wild fever due to the arrival of milk and messages from a friend who insisted that I go to the clinic management to complain about the staff.
” The second shoved her breast into the child’s mouth and shouted: “Yes, it hurts! And what did you think, gave birth - and that's it? You are a woman, be patient." And all this against the background of nerves, a wild fever due to the arrival of milk and messages from a friend who insisted that I go to the clinic management to complain about the staff.
The pediatrician reassured me that when we returned home, everything would be fine. Already on the second day, I had to invite a lactation consultant, but nothing improved. When mastitis loomed on the horizon, I could not get through to a single pediatrician, and I was helped by the hotline of LaLecheLeague, a non-profit organization to support breastfeeding.
It was insanely painful for me - I ran away from my daughter and seriously thought that I would rather give birth again than put her to my chest. I knew that discomfort might appear during feeding, but I was categorically not ready for the fact that it would be so painful.
One night I realized that I was screaming from pain, I practically threw the baby to the floor - it was a reflex
And then I gave up - a breast pump appeared, and for two months I fed my daughter with expressed milk with interruptions for a series of lactostasis with the threat of surgery . Once I was sitting in the car and pumping milk through a breast pump that was connected to the transmission line through a shield.
And, of course, it was a separate pleasure to go for checkups and stumble upon posters with happy women a la "Breastfeed - you will be a good mother." GV propaganda is great and important, but no one says or writes that it can be so painful and difficult. Nobody says you always have a choice. This develops a fantastic inferiority complex.
My daughter was two months old when the breast pump disappeared and we finally found a common language. By the year, she had warmed up, and everything went as it should.
Anastasia Markova comments:
Unfortunately, both experienced mothers and experienced breastfeeding consultants experience breastfeeding pain. Since the problem can be not only in the mother, but also in the child. And this requires an integrated approach and the help of specialists (in addition to a breastfeeding consultant). Ordinary doctors in a maternity hospital or a local pediatrician may simply not guess about the cause of pain during feeding. And they blame the “armless mother” for everything or say something like “You have to endure it, but how did you want to?”.
Since the problem can be not only in the mother, but also in the child. And this requires an integrated approach and the help of specialists (in addition to a breastfeeding consultant). Ordinary doctors in a maternity hospital or a local pediatrician may simply not guess about the cause of pain during feeding. And they blame the “armless mother” for everything or say something like “You have to endure it, but how did you want to?”.
I myself know this repulsion reflex of a child, when you just want to howl in pain. At the same time, I considered myself an experienced mother, and happy women advised me to each other as a cool consultant who saved everyone!
I bow to such mothers: I did not give up, I did everything to keep the baby fed with milk. And it was not in vain.
“They let me sleep, and I get up and pump. For what?"
Ekaterina Stepanenko, editor-in-chief of the publishing house "Walk into History":
There was so little milk in the maternity hospital that I immediately started formula feeding. Just a few weeks after being discharged, Petya stopped waking up at night - he ate around midnight, and the next time at 5-6 in the morning. The pediatrician advised me to get up at night and pump so that the milk would not go away completely.
Just a few weeks after being discharged, Petya stopped waking up at night - he ate around midnight, and the next time at 5-6 in the morning. The pediatrician advised me to get up at night and pump so that the milk would not go away completely.
I got up a couple of times, and then I thought, what the hell? The child gives me a unique opportunity to sleep, and instead of gaining strength, I myself get up at night. In short, I let go of the situation rather quickly.
Ekaterina Stepanenko with her son PetyaNow, looking back at this situation, I understand that, most likely, I had postpartum depression. Petya was a very calm baby, and at the same time I was all broken, everything fell out of my hands. I didn't know what to take. I cried that I couldn't go where I wanted to. Perhaps this also affected lactation and my indifference to this issue.
Anastasia Markova comments:
As a specialist, I often encounter various manifestations and severity of postpartum depression. And here sometimes you just have to not establish lactation, but help complete it. In the interests of mother. After all, her mental and physical health is always a priority. When there is no resource for anything, the child does not please, expectations do not coincide with reality, or there is simply no strength, then breastfeeding will not bring happiness, but will only aggravate the mother's condition. A specialist should not impose his opinion or want something for a woman.
And here sometimes you just have to not establish lactation, but help complete it. In the interests of mother. After all, her mental and physical health is always a priority. When there is no resource for anything, the child does not please, expectations do not coincide with reality, or there is simply no strength, then breastfeeding will not bring happiness, but will only aggravate the mother's condition. A specialist should not impose his opinion or want something for a woman.
A mother is always the main expert in caring for her child, she knows best, even purely intuitively. The main thing here is that mom found a way out for herself, which at that time was optimal. This will preserve the remnants of her resource without serious consequences.
“In general, I think that everyone is obsessed with GV, and this is a personal matter for everyone”
Anna Borodina:
It was all some kind of sheer torment. Because of the stitches, I couldn't sit. The chest is small. It hurts to sit, it is uncomfortable to lie, standing - the hands fall off. And my son could not grasp the chest. And then the pediatrician came and said: “How thin he is! Are you not feeding him?" And the other said that there was no milk and that it was necessary to supplement the formula. And after the very first bottle, he, happy and contented, fell asleep. And slept. And he didn't yell. The bottle was a great option for me: any person from the family could easily feed their son without my participation.
The chest is small. It hurts to sit, it is uncomfortable to lie, standing - the hands fall off. And my son could not grasp the chest. And then the pediatrician came and said: “How thin he is! Are you not feeding him?" And the other said that there was no milk and that it was necessary to supplement the formula. And after the very first bottle, he, happy and contented, fell asleep. And slept. And he didn't yell. The bottle was a great option for me: any person from the family could easily feed their son without my participation.
When my youngest daughter was born, I decided not to bother, especially since I had a cesarean and antibiotics, and she was in intensive care for a week because she swallowed amniotic fluid. When they finally let me see her, I gave her a breast for show, while there was still at least something in it.
But I'm not particularly dairy, on one of the ultrasounds they told me that the mammary gland itself is very small and there is nowhere for milk to come from. So I chose convenience and have no regrets. In general, I think that everyone is obsessed with GW, and this is a personal matter and everyone's personal choice. For children, it’s okay, if the mixture is normal and mom is happy.
So I chose convenience and have no regrets. In general, I think that everyone is obsessed with GW, and this is a personal matter and everyone's personal choice. For children, it’s okay, if the mixture is normal and mom is happy.
Anastasia Markova comments:
A classic example of the lack of support, psychological and informational, at the beginning of GV. A woman already in pain after childbirth receives strange comments from doctors instead of support, from whom she did not hear anything sensible. And there was no one to provide practical assistance. Having given birth to the second, such women often do not even try to fix something with GV. After all, then a solution was found that brought relief and saved my mother's nervous system.
The key phrase here is "happy mother". I always tell women that even if breastfeeding does not work out, then you will not become worse as a mother from this. And indeed it is. Love and care can be given in many ways, regardless of the type of feeding.
“I failed twice…”
Daria Nashchekina, founder of the Allergomoms community:
I honestly tried to breastfeed both of my sons. And with both I didn't succeed. I was sure that everything would work out for me. But there was simply not enough milk. I followed all the rules, lay skin to skin in a quiet room for hours, applied every half an hour. But everything was pointless. I hated myself for having to supplement my children with formula.
Every time I had to answer the pediatrician what kind of feeding the child was on, I broke out in a sweat. After one doctor at the father of the children told me that "only those who had their breasts cut off do not breastfeed," I sobbed for two days.
I did not enjoy the child and motherhood, but constantly tormented myself with guilt
With the second child, I was sure that I would improve. I worked with a consultant even before giving birth. I chose natural childbirth without stimulation and anesthesia. But in the end, the son refused to breastfeed. Or rather, he took it, but did not suck like a vacuum cleaner, as the elder did. It was hard for me to understand that something was wrong. Basically, I didn't feed him. And with my obsession with breastfeeding due to constant propaganda that this is how a good mother should do, I almost brought the child to a dangerous state. He lost a lot of weight, almost did not write. But it turned out that he had a birth injury and he simply could not suckle. And I do not have enough tissue in the mammary gland to ensure lactation.
But in the end, the son refused to breastfeed. Or rather, he took it, but did not suck like a vacuum cleaner, as the elder did. It was hard for me to understand that something was wrong. Basically, I didn't feed him. And with my obsession with breastfeeding due to constant propaganda that this is how a good mother should do, I almost brought the child to a dangerous state. He lost a lot of weight, almost did not write. But it turned out that he had a birth injury and he simply could not suckle. And I do not have enough tissue in the mammary gland to ensure lactation.
But why are pregnant women and those who have given birth not examined by a mammologist? They don't do ultrasound? How many problems could have been avoided. How many mothers would sleep peacefully and not torment themselves for years. We have those in "Allergomoms" who blame themselves for the fact that the child has hay fever. Because they didn't breastfeed. But this is only one brick out of a hundred. Yes, some people manage to feed, and some don't. But this does not make mom worse or better. This is her personal business and her choice. The situation when the first question from an unfamiliar mother on the playground is "Are you on GW?" - not the norm.
Yes, some people manage to feed, and some don't. But this does not make mom worse or better. This is her personal business and her choice. The situation when the first question from an unfamiliar mother on the playground is "Are you on GW?" - not the norm.
Anastasia Markova comments:
It is very difficult for an excellent mother to survive situations when not everything is perfect. Moreover, such women really try and honestly follow the recommendations. Competent advice on a problem is often half the battle. It is more important to try to understand whether the mother is comfortable with what she feels
Torturing yourself for something that was not exclusively breastfeeding, that not everything worked out according to the norms and rules of WHO, is fundamentally wrong. After all, in fact, it has developed, it’s just different for everyone. Any mother is the best for her child. And breastfeeding is not the same as being a good mother. To give birth, to take care, to give warmth to a child - this is what is really important. And there are a lot of ways and means for this.
And there are a lot of ways and means for this.
“She won’t fit in his mouth”
Natalya Knyazeva:
The child was born, he didn’t take a breast, sobbed, didn’t gain weight. My attempts to get advice on how to stick his chest in were unsuccessful. It seems that they helped to apply, but in the end they came to the conclusion that "you have to try, but the chest is big, the mouth is small ...".
Milk came to me at home. In the second week after giving birth, I didn’t pump enough, lactostasis began, which I tried to resolve on my own for three days, and as a result I got a breast abscess.
I was contacted by a good mammologist, who pumped out the pus from my chest with a syringe, lamenting for a long time that such an abscess is an indication for hospitalization and ten days in the hospital.
However, there were literally two drops of milk in this breast. I saw this, because the child still did not take the breast. I bought an expensive breast pump, they fed me with expressed milk from a bottle. He was constantly lacking, they were supplemented with a mixture. The same mammologist gave me a lesson on application, it became better. Before that, I was constantly uncomfortable, and in general I am clumsy in life, but here it was just a climax.
He was constantly lacking, they were supplemented with a mixture. The same mammologist gave me a lesson on application, it became better. Before that, I was constantly uncomfortable, and in general I am clumsy in life, but here it was just a climax.
No matter how you sit, no matter how you lie down, your breasts don't get into your mouth normally. I constantly fell asleep on my chest, so it lasted for hours. After that, he still “caught up” with the mixture. I felt that I was not coping - but how to wash the floor, how to walk for four hours, how to cook dinner? I was alone with the child almost all the time.
Fuel was added to the fire by a pediatrician from the clinic, who recommended not to keep at the breast during the first month. “You should spend half an hour feeding. This is to feed, then hold, so that he burps ... ”- her phrase is almost verbatim. For some reason, I began to count how much milk I had, kept a diary - how much I expressed, how much formula, this made me even more nervous.
In the process, I tried to read something on the Internet, but it turned out badly: lack of sleep, the child screams, my chest hurts - I worked until I was 30 years old, and life did not prepare me for this. Until 4.5 months, we were still delaying, and then it became clear that there was nothing to save. The child left with no problems, the milk disappeared in just three days. To be honest, I breathed a sigh of relief: I finally felt normal in motherhood.
Having already stopped feeding, I found out that the breast is not a mug, but rather a water tap, and milk is produced in it on demand.
Anastasia Markova comments:
Unfortunately, specialists in the maternity hospital are novice volunteers or medical workers with a minimum set of knowledge in this area. Yes, the badge says “HV consultant”, but he is not always able to help the mother due to his own inexperience
Ideally, the mother takes care of the child, and everyone else takes care of the mother. In real life, after discharge, a woman is faced with the fact that she has to simultaneously rake in the hardships of motherhood and everyday issues that cannot be avoided. Many really cannot quickly change their mindset, drop everything and rest. No one died from dirt, and my husband, probably, is able to cook food for himself. But the woman who became a mother for the first time (she herself was one) tries to embrace the immensity, not even thinking that it is possible in a different way.
In real life, after discharge, a woman is faced with the fact that she has to simultaneously rake in the hardships of motherhood and everyday issues that cannot be avoided. Many really cannot quickly change their mindset, drop everything and rest. No one died from dirt, and my husband, probably, is able to cook food for himself. But the woman who became a mother for the first time (she herself was one) tries to embrace the immensity, not even thinking that it is possible in a different way.
Preparing for GV in theory helps to avoid at least part of the difficulties. And very often even the most experienced breastfeeding consultants with their far from the first children have problems.
“To be ashamed and ashamed that you don’t have milk is stupid”
Ksenia Zhukova, writer:
I have two children. While waiting for the first one, I went to natural childbirth courses. According to the contract, in case of problems with breastfeeding, I was entitled to one home visit of a specialist and one correspondence consultation. I was told that I have large breasts, so there should be a lot of milk. During the courses, they explained to us that it is necessary to feed with our own milk for at least a year.
I was told that I have large breasts, so there should be a lot of milk. During the courses, they explained to us that it is necessary to feed with our own milk for at least a year.
I had milk, but very little. No lactation teas, cabbage leaves, consultations (which ate a lot of money), massages did not help. Milk did not disappear, but it was not added either. The husband, having read and heard enough at lectures about the exceptional benefits of breastfeeding, did not allow me to supplement with anything else. The whole apartment was covered in milk stains, the baby was always on the chest.
With my second child (now she is two years old), I bought a breast pump and a bottle of milk formula in advance and decided not to torture myself. And if there is not enough milk, supplement with formula. Everyone around told how convenient it is to breastfeed: you can travel everywhere, and the child’s immunity is strengthened.
There is even less milk. Ten years ago, at the maternity hospital, they told me not to torment a screaming baby, who immediately competently grabbed an empty breast, and they quietly slipped the horns with the mixture.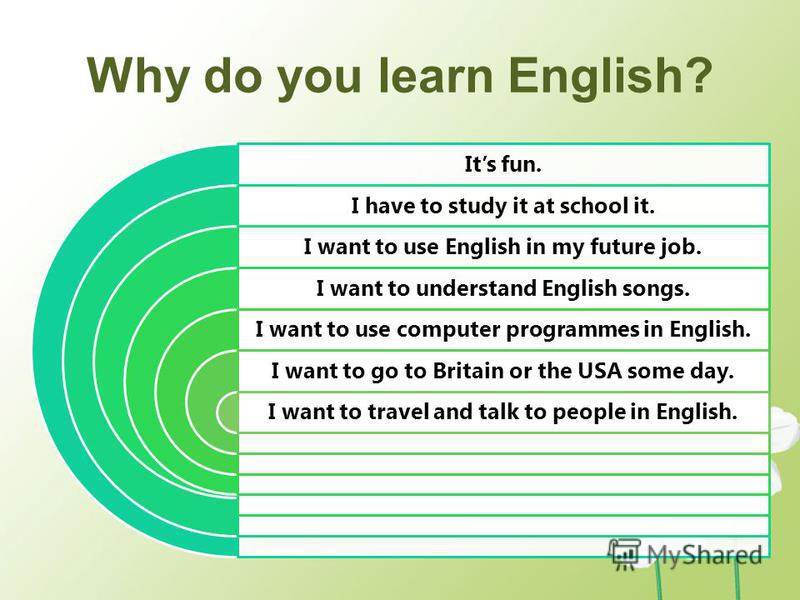 And I rejected them, because mother's milk is our everything.
And I rejected them, because mother's milk is our everything.
But at home after being discharged, a pre-prepared jar of formula was waiting for me
I honestly brought the baby to my chest. But here an unexpected problem arose, about which no one warned me. Every feeding made me feel very bad, sometimes it came to panic attacks. I looked incomprehensibly at photographs of smiling mothers with babies. What smile when you start to feel sick during feeding?
It's good that we had a competent nurse who, thanks to her, straightened my brain by talking about herself. How she didn't produce milk. From the word "in general". And that there are many of them - as she put it, "non-dairy". And so that I don’t think to consider myself some kind of not such a mother or something. And most importantly, that the children feel good, satisfying, calm. And my mother is also calm nearby. Being ashamed and ashamed that you don't have milk is stupid.
Anastasia Markova comments:
There are situations when, due to various physiological reasons or health conditions, a mother really has a lack of milk. Here you can’t blame yourself or consider yourself “not such a mother.” And mixed feeding is much better than completely artificial, and even 10 ml of milk per day makes a difference to the health of the child.
Here you can’t blame yourself or consider yourself “not such a mother.” And mixed feeding is much better than completely artificial, and even 10 ml of milk per day makes a difference to the health of the child.
Therefore, mothers who try to save milk in every way deserve only praise and support.
After the second birth, mother acted as her previous experience and intuition prompted her. And I have to say a special thank you to the nurse. Yes, she could not help her mother increase the amount of milk, but her words hit the target and saved her mother from an inferiority complex and guilt for not being able to feed her child exclusively with breast milk. Mom found a solution that made her calm. The child was full, adequately developed and grew. And what is not on breast milk is not a shame at all.
Where to go for help with problems with breastfeeding:
- LaLecheLiga is an organization that provides free consultations, conducts online and offline meetings for breastfeeding mothers, organizes support groups and conducts educational activities.

- AKEV (Association of Lactation Consultants): You can find a lactation consultant in your city.
- Hotline of the Department of Health of the Government of Moscow on breastfeeding problems - tel. 495 772-09-32
- Breastfeeding hotline: +7 495 926-63-23 from 07:00 to 23:00 daily
- Medela hotline 24/7 free of charge throughout Russia: +7 (800-20) 0-68-08
On the cover: Ksenia Zheglaya with her daughter. Photo: Anya Stepanova
Prejudices related to breastfeeding
Instead of an introduction, I would like to say that the ideas of modern women about breastfeeding are a collection of prejudices. They are so common that in many books for expectant mothers and in magazines for parents, it is actions based on prejudice that are described as correct and necessary.
“Breastfeeding is something incredibly difficult, almost no one is able to feed for a long time, everyone always has a lot of problems and one continuous inconvenience”
There is nothing easier, more convenient, more pleasant for mother and child, and, by the way, cheaper, than proper breastfeeding. But for that to be the case, breastfeeding needs to be learned. The best teacher in this matter may not be a book or a magazine for parents, but a woman who has been breastfeeding her child for a long time, more than a year, and receiving positive emotions from this. There are women who breastfeed for a long time and perceived it as a punishment. For example, one mother fed a child for 1.5 years and for all these 1.5 years she pumped after each feeding, and when she decided that she was enough and decided to wean the child, she had mastitis due to wrong actions. Now she tells everyone that breastfeeding is hell. She didn't feed her baby properly for a single day.
But for that to be the case, breastfeeding needs to be learned. The best teacher in this matter may not be a book or a magazine for parents, but a woman who has been breastfeeding her child for a long time, more than a year, and receiving positive emotions from this. There are women who breastfeed for a long time and perceived it as a punishment. For example, one mother fed a child for 1.5 years and for all these 1.5 years she pumped after each feeding, and when she decided that she was enough and decided to wean the child, she had mastitis due to wrong actions. Now she tells everyone that breastfeeding is hell. She didn't feed her baby properly for a single day.
"Breastfeeding spoils the shape of the breast"
It is true that breastfeeding does not improve the shape of the breast, but the breast changes during pregnancy. It is then that it increases and becomes heavier, and, if its shape contributes to this, it “sags”.
Breast changes during lactation. Approximately 1-1. 5 months after birth, with stable lactation, it becomes soft, produces milk almost only when the baby suckles. After the end of breastfeeding, 1.5-3 or more years after the birth of the baby, involution of the mammary gland occurs, lactation stops. Iron "falls asleep" until the next time. Under natural conditions, the end of breastfeeding always coincides with a decrease in the baby's need for breastfeeding. The chest remains soft, inelastic. The shape of the breast largely depends on the presence of adipose tissue in it, the amount of which decreases during prolonged breastfeeding. After the end of breastfeeding, adipose tissue is gradually restored. If a woman does not feed a child, the involution of the mammary gland occurs within the first month after childbirth. The shape of the breast still does not return to its pre-pregnancy state. And if you think about it and figure out why a woman has breasts at all? It's for breastfeeding.
5 months after birth, with stable lactation, it becomes soft, produces milk almost only when the baby suckles. After the end of breastfeeding, 1.5-3 or more years after the birth of the baby, involution of the mammary gland occurs, lactation stops. Iron "falls asleep" until the next time. Under natural conditions, the end of breastfeeding always coincides with a decrease in the baby's need for breastfeeding. The chest remains soft, inelastic. The shape of the breast largely depends on the presence of adipose tissue in it, the amount of which decreases during prolonged breastfeeding. After the end of breastfeeding, adipose tissue is gradually restored. If a woman does not feed a child, the involution of the mammary gland occurs within the first month after childbirth. The shape of the breast still does not return to its pre-pregnancy state. And if you think about it and figure out why a woman has breasts at all? It's for breastfeeding.
"Breastfeeding spoils the figure"
Many women are afraid to gain weight while breastfeeding. But usually a woman gains weight mainly during pregnancy, and not when she is nursing. Moreover, if before pregnancy she tried to meet certain fashionable standards, for example, 90-60-90, during pregnancy she returns to her weight, her genetically incorporated physiological norm (and it may be far from fashionable standards) + the well-known 7-10kg per uterus, fetus, amniotic fluid, increased volume of circulating blood and a little bit more for various little things. Weight gain during pregnancy can be significant. Many women begin to lose weight after 6-8 months of feeding, and gradually, in the second, third year of feeding, she “drops” everything that she has accumulated. It turns out that the figure from breastfeeding often just improves.
But usually a woman gains weight mainly during pregnancy, and not when she is nursing. Moreover, if before pregnancy she tried to meet certain fashionable standards, for example, 90-60-90, during pregnancy she returns to her weight, her genetically incorporated physiological norm (and it may be far from fashionable standards) + the well-known 7-10kg per uterus, fetus, amniotic fluid, increased volume of circulating blood and a little bit more for various little things. Weight gain during pregnancy can be significant. Many women begin to lose weight after 6-8 months of feeding, and gradually, in the second, third year of feeding, she “drops” everything that she has accumulated. It turns out that the figure from breastfeeding often just improves.
Very often it turns out that a woman, having stopped breastfeeding 1.5-2 months after giving birth, begins to gain weight. Perhaps this is due to the resulting hormonal imbalance, tk. no woman is designed for such a rapid cessation of lactation.
"You have to prepare the breast for feeding." And then various recommendations follow, from sewing hard rags into the bra to advice to the husband at the end of pregnancy to “dissolve the ducts” of his wife
There is no need to prepare the breast for feeding, it is so arranged by nature that by the time of birth it is quite ready to feed the child. Cloths, for example, can cause skin irritation. Any manipulation of the nipple at the end of pregnancy can lead to very undesirable consequences due to the stimulation of the oxytocin reflex: stimulation of the nipple - release of oxytocin - contraction of the muscles of the uterus under the influence of oxytocin - the uterus is "in good shape" - and, as the worst option, stimulation of premature labor. And in general, has anyone seen a cat with a rag in a bra, or a monkey doing a hardening shower massage?
“With a flat, let alone inverted nipple, breastfeeding is impossible”
Strange as it may seem to people who have never breastfed, a baby's nipple is just a point from which milk flows. If the child sucks in the correct position, then the nipple is located at the level of the soft palate and does not participate in the actual sucking. The child sucks not the nipple, but the areola, massaging, decanting it with the tongue. A breast with a flat or inverted nipple is difficult for a baby to hold in his mouth while suckling and it is more difficult for him to suck on it. Mom should show patience and perseverance in the first days after the birth of a child. Any child is perfectly trained to suck even the most uncomfortable, from our point of view, breast.
If the child sucks in the correct position, then the nipple is located at the level of the soft palate and does not participate in the actual sucking. The child sucks not the nipple, but the areola, massaging, decanting it with the tongue. A breast with a flat or inverted nipple is difficult for a baby to hold in his mouth while suckling and it is more difficult for him to suck on it. Mom should show patience and perseverance in the first days after the birth of a child. Any child is perfectly trained to suck even the most uncomfortable, from our point of view, breast.
The nipple changes shape during sucking, stretches and takes on a more comfortable shape for the baby, usually in 3-4 weeks. There are also various devices called "nipple formers". They are put on immediately after feeding, when the nipple is slightly extended by the efforts of the child and worn until the next application. The nipple formers hold the nipple in an extended position. But even without these things it is quite possible to do.
It is very important for a mother with flat or inverted nipples to ensure that her baby never suckles anything but her mother's breast after birth. The child of such a mother, having sucked on a bottle or a pacifier, quickly realizes that this is a more convenient object for sucking and begins to refuse the breast. In this situation, mom will need even more patience and perseverance.
"You can't keep a newborn at the breast for more than 5 minutes, otherwise there will be cracks"
The child should be kept at the breast for as long as he needs. Feeding ends when the baby himself releases the breast.
If we talk about cracks, then there are only three groups of causes that lead to their formation
- Mother washes her breasts before each feeding. If she does this (and even with soap, and even anoints with brilliant green after feeding - a favorite pastime in Russian maternity hospitals, for example) - she constantly washes off the protective layer from the areola, which is produced by special glands located around the nipple, and dries the skin.
 This protective lubricant exists just to prevent the loss of moisture in the delicate skin of the nipple, it has bactericidal properties and inhibits the growth of pathogenic microorganisms and, which is especially important for the child, smells about the same as amniotic fluid. The sensitive skin of some women cannot tolerate such exposure for a long time and begins to crack, even with proper attachment of the baby.
This protective lubricant exists just to prevent the loss of moisture in the delicate skin of the nipple, it has bactericidal properties and inhibits the growth of pathogenic microorganisms and, which is especially important for the child, smells about the same as amniotic fluid. The sensitive skin of some women cannot tolerate such exposure for a long time and begins to crack, even with proper attachment of the baby. -
Causes related to the incorrect position and behavior of the baby at the breast: the baby is not properly attached and sucks in the wrong position. And if this is true, then 5 minutes after 3 hours is enough for the formation of abrasions, and then cracks. The baby may latch on correctly, but in the process of suckling, he may perform various actions that can lead to cracking if the mother does not know that these actions need to be corrected and not allowed to behave like this. It must be remembered that the child has not suckled before, and does not know how to do it (he knows only the general principle of sucking).
 Unfortunately, most mothers also do not know how a baby should behave at the breast; they have never, or almost never seen it. What shouldn't a child be allowed to do? "Move out" to the tip of the nipple. This happens especially often if, during sucking, the child does not stick his nose into his mother's breast. If the mother feels that the grip is changing, she should try to press the baby with her nose to her chest. Very often this is enough for the child to “put on” correctly.
Unfortunately, most mothers also do not know how a baby should behave at the breast; they have never, or almost never seen it. What shouldn't a child be allowed to do? "Move out" to the tip of the nipple. This happens especially often if, during sucking, the child does not stick his nose into his mother's breast. If the mother feels that the grip is changing, she should try to press the baby with her nose to her chest. Very often this is enough for the child to “put on” correctly.
If this does not help, the nipple must be removed and re-inserted correctly. The baby should not suckle the breast incorrectly for a single minute. He doesn’t care how to suck, he doesn’t know that he hurts his mother, he doesn’t know that the wrong position does not allow him to suck out enough milk, he doesn’t know that with the wrong position there is not enough stimulation of his mother’s breast and there will not be enough milk production. You can not let the child play with the nipple. A child who has learned to slide down on the tip of the nipple sometimes begins to pass the nipple back and forth through the parted jaws. Mom, of course, it hurts or is unpleasant, but in most cases, mothers allow this to be done “If only he sucked ...” they say ... Why? It often happens that children who do not feel the touch of the breast with their nose during sucking, or do not feel it very well, begin to make search movements with the nipple in their mouth. Here you need to gently press the baby to your chest so that he understands that he is already in place and there is nothing more to look for. Sometimes, especially if the mother has long and large nipples, the baby grabs the breast in several steps, “climbing” up in several movements. This also happens in cases where the child has already sucked on the pacifier and does not open his mouth well. The nipple is injured so very quickly. To avoid this, it is necessary to properly insert the nipple into the wide-open mouth, bringing the nipple itself past the jaws, as deep as possible.
A child who has learned to slide down on the tip of the nipple sometimes begins to pass the nipple back and forth through the parted jaws. Mom, of course, it hurts or is unpleasant, but in most cases, mothers allow this to be done “If only he sucked ...” they say ... Why? It often happens that children who do not feel the touch of the breast with their nose during sucking, or do not feel it very well, begin to make search movements with the nipple in their mouth. Here you need to gently press the baby to your chest so that he understands that he is already in place and there is nothing more to look for. Sometimes, especially if the mother has long and large nipples, the baby grabs the breast in several steps, “climbing” up in several movements. This also happens in cases where the child has already sucked on the pacifier and does not open his mouth well. The nipple is injured so very quickly. To avoid this, it is necessary to properly insert the nipple into the wide-open mouth, bringing the nipple itself past the jaws, as deep as possible. Moms don't know how to breastfeed properly.
Moms don't know how to breastfeed properly.
A typical picture for maternity hospitals with separate stay is as follows: a baby was brought to the mother for 30 minutes, the baby held everything correctly and sucked well for these 30 minutes, he would still suck, but they came to pick him up and the mother pulls (slowly or quickly) his nipple from mouth. Six such pulls per day is enough for the development of abrasions. You can take the nipple only after opening the jaw with the little finger (quickly insert the tip of the finger into the corner of the mouth and turn it - it does not hurt at all and no one suffers).
Diseases of the skin of the nipples. Most often, mothers are faced with a fungal infection of the skin of the nipples - "thrush". In this situation, the skin most often looks "irritated", it can peel off, itch, cracks may appear, even despite proper application, there may be pain during and after sucking, piercing pains along the milk ducts. This problem is usually solved with the use of specific treatment and also has nothing to do with the topic of preparing the breast for feeding or the time the baby is at the breast.
“While there is no milk, it is necessary to drink more water”
The first day after childbirth, liquid colostrum forms in the breast of a woman, on the second day it becomes thick, on 3-4 days transitional milk may appear, 7-10-18 days - milk become mature. Colostrum is scarce and thicker than milk. This is the main argument in most Russian maternity hospitals in favor of supplementing and feeding the child (otherwise he allegedly suffers from hunger and thirst).
If a child needed large volumes of liquid immediately after birth, then nature would arrange the woman in such a way that she would be flooded with colostrum immediately after childbirth. But the child does not need extra water at all. All he needs he gets from colostrum and milk! The water that is given to the child while the mother has colostrum literally “washes away” the colostrum from the gastrointestinal tract, depriving the baby of the action of colostrum necessary for him. Water is given from a bottle, which leads to "tangled nipples" in the baby and may lead to refusal of the breast. Water causes a false feeling of fullness and reduces the need for suckling in a child. If we give a child 100 g of water per day, he sucks 100 g less milk (this applies not only to a newborn). The kidneys of a newborn are not ready for a large load of water and begin to work with overload. The list of arguments against can be continued, but these are enough.
Water causes a false feeling of fullness and reduces the need for suckling in a child. If we give a child 100 g of water per day, he sucks 100 g less milk (this applies not only to a newborn). The kidneys of a newborn are not ready for a large load of water and begin to work with overload. The list of arguments against can be continued, but these are enough.
“While there is no milk, it is necessary to supplement the child with formula, otherwise he will lose weight, starve”
The child is not designed to receive anything other than colostrum and milk. In the first days after birth, one colostrum is enough for him. Weight loss in the first day of life is a physiological norm. Newborns lose up to 6-8% of their birth weight in the first two days of their lives. Most children regain their weight or begin to put on weight by 5-7 days of life. Supplementary feeding with a mixture in the first days of a child's life is nothing more than a gross interference in the functioning of the baby's body. You can call this intervention a metabolic catastrophe. But in most Russian maternity hospitals, this is completely ignored!
You can call this intervention a metabolic catastrophe. But in most Russian maternity hospitals, this is completely ignored!
In addition, the introduction of supplementary feeding is carried out through a bottle, which very quickly leads to "tangled nipples" and the baby refuses the breast. Sometimes one or two bottle feedings are enough to stop a baby from breastfeeding! The mixture causes a feeling of fullness, lingers in the stomach for a long time, the child has a reduced need to suckle the breast, which leads to a decrease in breast stimulation and a decrease in milk production.
“I feed my baby on demand! He demands from me in 3.5 hours!”
Feeding on demand means putting the baby to the breast for every disturbance or search. The baby needs breastfeeding around every sleep, he falls asleep at the breast and when he wakes up, he is given the breast. A newborn child in the first week of his life can indeed be applied relatively rarely - 7-8 times a day, but in the second week of life, the intervals between applications are always reduced. During wakefulness, the child can ask for a breast up to 4 times per hour, i.e. every 15 minutes! Usually a child fed on demand is applied in the first month of life 12 or more times a day, usually 16-20 times. If a child in the first months of life is applied less than 12 times, then the mother either does not notice his modest requests, or ignores them (meaning a healthy, physiologically mature child).
During wakefulness, the child can ask for a breast up to 4 times per hour, i.e. every 15 minutes! Usually a child fed on demand is applied in the first month of life 12 or more times a day, usually 16-20 times. If a child in the first months of life is applied less than 12 times, then the mother either does not notice his modest requests, or ignores them (meaning a healthy, physiologically mature child).
In the overwhelming majority of cases, at the moment when the child begins to ask for a breast more often, the mother decides that the child is starving and introduces supplementary feeding. And the child asks for breasts not at all because he is hungry. He constantly needs a sense of confirmation of physical contact with his mother. During his life in his mother's belly, he is very used to the following: warm, crowded, I hear my heart beating, my lungs breathe, my intestines growl, I smell and taste amniotic fluid (filling the baby's nose and mouth), almost all the time I suck a fist (studies suck). Only in these conditions the baby feels comfortable and safe. After childbirth, he can get into such conditions only if his mother takes him in her arms, puts him on her breast, and then he will again feel cramped, warm, he will hear familiar rhythms, start sucking and feel the familiar smell and taste (the smell and taste of milk are similar to the taste and smell of amniotic fluid). And a newborn child wants to get into such conditions as often as possible. And a modern mother is waiting, she can’t wait, when the intervals between feedings will increase, when will the child start eating in 3.5-4 hours, when will he stop waking up at night ??? Hurry!!! And, usually, to the timid attempts of the child to ask for a breast, he answers with a pacifier, a rattle, gives some water, talks, entertains. The child is most often applied to the breast only when he wakes up. And he quickly agrees with this position. The child always takes the mother's position. But here a “pitfall” awaits mother and baby - insufficient breast stimulation and, as a result, a decrease in the amount of milk.
Only in these conditions the baby feels comfortable and safe. After childbirth, he can get into such conditions only if his mother takes him in her arms, puts him on her breast, and then he will again feel cramped, warm, he will hear familiar rhythms, start sucking and feel the familiar smell and taste (the smell and taste of milk are similar to the taste and smell of amniotic fluid). And a newborn child wants to get into such conditions as often as possible. And a modern mother is waiting, she can’t wait, when the intervals between feedings will increase, when will the child start eating in 3.5-4 hours, when will he stop waking up at night ??? Hurry!!! And, usually, to the timid attempts of the child to ask for a breast, he answers with a pacifier, a rattle, gives some water, talks, entertains. The child is most often applied to the breast only when he wakes up. And he quickly agrees with this position. The child always takes the mother's position. But here a “pitfall” awaits mother and baby - insufficient breast stimulation and, as a result, a decrease in the amount of milk.
“Feeding on demand is a nightmare! It is impossible to sit and feed the child for days!”
That's what mothers who can't breastfeed say. With properly organized feeding, mom is resting! She lies, relaxed, hugs the baby, the baby sucks. What could be better? Most women cannot find a comfortable position, they sit, they hold the child awkwardly, their back or arm numbs, if they feed lying down, it usually “hangs” over the child on the elbow, the elbow and back become numb. Moreover, if the child does not take the breast well, it hurts the mother ... What kind of pleasure can we talk about here? In the first month - one and a half after childbirth, when the child is applied chaotically, without a pronounced regimen, sucks often and for a long time, the mother can feel good only if breastfeeding is organized correctly, it is convenient for the mother to feed, she knows how to do it standing, lying down and sitting, and even moving.
“After each feeding, you must express the rest of the milk, otherwise the milk will be wasted”
No, you do not need to express after each feeding if breastfeeding is properly organized. If you feed your baby 6 times a day and do not express, indeed, milk can disappear very quickly. If you express after each feeding, then you can support lactation for some time. The terms are different, but rarely it is more than six months, cases of feeding on such behavior for more than a year are rare.
If you feed your baby 6 times a day and do not express, indeed, milk can disappear very quickly. If you express after each feeding, then you can support lactation for some time. The terms are different, but rarely it is more than six months, cases of feeding on such behavior for more than a year are rare.
When feeding a baby on demand, the mother always has as much milk as the baby needs and there is no need to pump after each application. In order for the newborn to completely suck out the breast, it is applied to one breast for 2-3 hours, and to the other for the next 2-3 hours. Somewhere after 3 months, when the child is already applied relatively rarely, he may need a second breast in one attachment, then the next time he is applied to the one that was last.
There is one unpleasant “pitfall” in regular pumping after feeding, which even most doctors are not aware of. It's called lactase deficiency. When a mother expresses after a feed, she expresses just the “hind” fatty milk, which is relatively poor in milk sugar, lactose. She feeds the child mainly with the anterior portion, which accumulates in the breast between rare feedings. There is a lot of lactose in the anterior portion. The child is fed "only lactose", the gastrointestinal tract of the child after some time ceases to cope with such volumes of lactose. Lactase deficiency develops (Lactase is an enzyme that breaks down lactose - milk sugar, it begins to be missed). This is one of the reasons for the development of lactase deficiency; the second, for example, is this: the mother gives the child two breasts in one feeding. But about this separately.
She feeds the child mainly with the anterior portion, which accumulates in the breast between rare feedings. There is a lot of lactose in the anterior portion. The child is fed "only lactose", the gastrointestinal tract of the child after some time ceases to cope with such volumes of lactose. Lactase deficiency develops (Lactase is an enzyme that breaks down lactose - milk sugar, it begins to be missed). This is one of the reasons for the development of lactase deficiency; the second, for example, is this: the mother gives the child two breasts in one feeding. But about this separately.
“You should give your baby two breasts at one feeding.”
No, it is not necessary to give two breasts. A newborn baby can be applied for 1.5-3 hours to one breast. Then 1.5-3 hours to another (for example, the baby woke up, sucked a little and didn’t want to anymore, but after 30 minutes he wanted to suck a little more. After 20 minutes, he sucked longer and fell asleep; all these attachments were from one breast; when the baby wakes up, you can offer him another breast). We need this so that the baby sucks the breast to the end, and receives "front" and "hind" milk in a balanced amount. If the baby is transferred to the other breast in the middle of feeding, he will receive less fat-rich hind milk. He will suck mainly the front portion from one breast and add the same from the other. Foremilk is rich in lactose, and after a while the baby can no longer cope with the load of lactose. Lactose intolerance develops.
We need this so that the baby sucks the breast to the end, and receives "front" and "hind" milk in a balanced amount. If the baby is transferred to the other breast in the middle of feeding, he will receive less fat-rich hind milk. He will suck mainly the front portion from one breast and add the same from the other. Foremilk is rich in lactose, and after a while the baby can no longer cope with the load of lactose. Lactose intolerance develops.
Transferring a baby from one breast to another can cause hyperlactation in some women, and if the mother also expresses both breasts after each feeding ... There are such mothers. Curtailing excess milk is sometimes more difficult than adding missing ... In some cases, feeding at one feeding from two breasts is necessary to stimulate lactation when there is a shortage of milk. A growing baby, most often after 3-4 months, may need two breasts in one feeding. Then the next application begins with the breast that was last.
“The more liquid you drink, the more milk”
There are mothers who try to drink as much as possible, sometimes up to 5 liters of liquid per day. And a nursing mother should drink only as much as she wants. By thirst. Mom shouldn't be thirsty. And if water is drunk on purpose, and even more than 3-3.5 liters per day, lactation can begin to be suppressed.
And a nursing mother should drink only as much as she wants. By thirst. Mom shouldn't be thirsty. And if water is drunk on purpose, and even more than 3-3.5 liters per day, lactation can begin to be suppressed.
“Sucking the fist is very harmful”
The whole end of pregnancy the child sucked the fist, so he learned to suck. Fist sucking is one of the inborn habits of a newborn. After childbirth, the baby begins to suck on the fist as soon as it enters his mouth. At 3-4 months, the fist is the first thing that the baby can put into his mouth on his own. He can do things on his own!!! This is amazing! And at this age, many babies begin to actively suck their fingers and fists. There is nothing wrong with that. Mom only needs to watch the baby a little. If a baby plays with a fist, then he sucks, then he stops, he can not be distracted from this activity. If the baby begins to actively suck the fist, then the baby wants to suck for real, offer him a breast. If the need to suckle the baby is fully satisfied by the breast, then the baby stops sucking the fist by 5-6 months. (Then, at 6-7 months, he begins to “look for teeth”, but this is a completely different behavior). The cam baby sucks almost the same as the breast, opening its mouth wide. Some babies have a very funny behavior when, having stuck to the chest, the baby tries to put his fist in his mouth ...
(Then, at 6-7 months, he begins to “look for teeth”, but this is a completely different behavior). The cam baby sucks almost the same as the breast, opening its mouth wide. Some babies have a very funny behavior when, having stuck to the chest, the baby tries to put his fist in his mouth ...
"My baby needs a pacifier"
The baby is not designed by nature to suckle anything other than the breast (and the fist, in a pinch). A child is always taught to use a pacifier. There are children who immediately push out the pacifier with their tongue. And there are those who begin to suck it. There are mothers who hold the pacifier with their finger so that her child does not push it out. Usually, the first time a baby gets a dummy is when he showed concern and the mother does not know how to calm him down. To calm down, the child needs to suck on the breast, well, they didn’t give him a breast, they gave him something else, he will have to suck what they give ...
“A child often asks for breasts, which means that he is hungry, there is not enough milk for him”
As mentioned above, a newborn child asks to be breastfed often, not at all because he is hungry. He wants to suck, he wants to mom. He constantly needs confirmation of psycho-emotional and physical contact with his mother.
He wants to suck, he wants to mom. He constantly needs confirmation of psycho-emotional and physical contact with his mother.
“Sufficient milk or not, we will find out on control feeding”
We will not learn anything on control feeding (the child is weighed before and after feeding, the difference is calculated and find out how much he sucked for feeding). Because:
- A baby who feeds on demand constantly sucks different portions of milk. In one application 5 ml, in another - 50, in the third - 150. You can get 5 ml. (I once weighed my daughter after 30 minutes of suckling. She gained 14 g. In the first month of her life, she gained 1200 g - and what would the local pediatrician tell me if this was control feeding in the clinic?)
- The newborn is designed to receive small portions of milk, but often. The vast majority of newborns in the conditions of feeding 6-7 times a day still suck out small portions of milk, and not 6 times 120 ml. And of course they don't eat.
 They start gaining poorly or stop gaining weight, or lose weight altogether.
They start gaining poorly or stop gaining weight, or lose weight altogether.
Sufficient or not enough milk can be determined in two ways:
Wet diaper test. (This is a test for wet diapers, not for used diapers, because you need to know exactly the number of urination). If a child older than 7 days pees more than 6-8 times a day, his urine is light, transparent, odorless, then he receives a sufficient amount of milk. Usually the child pees during wakefulness every 15-30 minutes. If a mother uses diapers, but wants to find out if there is enough milk or not, she needs to remove the diapers from the child for three hours. If the baby pees 3-4 times or more in three hours, then you can not count further. If you peed 3 times or less, we count for 6 hours. If in six hours he peed 4-5 times or more, you can not count further, if less than 4, we count further. And so on… Weekly weight gain (for a child older than 7 days) should be between 125 and 500 g.
“If applied frequently, the baby will suck everything out quickly, the breast is soft all the time – there is no milk. It is necessary to “save” milk for feeding”
When feeding a child on demand, the breast becomes soft about a month after the start of feeding, when lactation becomes stable. Milk begins to be produced only when the baby suckles. The breast is never “empty”, in response to the sucking of the child, milk is constantly produced in it. If the mother is trying to fill her breasts for feeding, waiting for the breasts to “fill up”, she gradually reduces the amount of milk by such actions. The more mother attaches the child, the more milk, and not vice versa.
“The stomach needs to rest”
But the child's stomach doesn't work very well. Milk there only curdles and is quickly evacuated to the intestines, where the actual digestion and absorption takes place. This is the prejudice from the old song about feeding according to the schedule after 3 hours. The newborn does not have a clock. No mammal makes even intervals in feeding its newborns. The body of the child is adapted to the continuous flow of mother's milk, and he does not need to rest at all.
“After each feeding, keep the baby upright for 20 minutes”
Do not hold the baby upright after each feeding, especially if the baby has fallen asleep. Most of the time the baby lies on its side. If he burps a little, then the diaper just changes under his cheek. It is necessary to hold the artificial man vertically so that he does not spill the 120g poured into him. And we are talking about babies who are fed on demand and receive small portions of mother's milk. In addition, the cardiac sphincter of the stomach needs training, which it can only receive if the child is lying down.
“You need to sleep at night”
At night, you need to not only sleep, but suck your breast. Most newborn children are so arranged that they sleep from 10-11 pm to 3-4 am, then they begin to wake up and ask for breasts. In a child of the first month of life, applications in the morning hours (from 3 to 8) are usually 4-6. Night feedings with properly organized breastfeeding look something like this: the baby got worried, the mother put it to the breast, the baby sleeps sucking and the mother also sleeps, after a while he lets go of the breast and sleeps more soundly. And such episodes happen in a night 4-6. All this is easy to organize if the mother sleeps with her child, and for this she needs to be able to feed lying down in a comfortable position.
If the baby sleeps separately from the mother, in his own bed, then he stops waking up for morning feedings, sometimes already a week after birth, sometimes by 1.5-2 months. Most modern mothers take this with relief, because. for them, finally, the night running back and forth, nodding while sitting in a chair or on a bed over a sucking child, and some also pumped at night ... And here they are waiting for a pitfall called insufficient stimulation of prolactin and, as a result, a decrease in the amount of milk . A mother and her child are a wonderful self-regulating system. While the baby has a need to suck in the morning, his mother produces the maximum amount of prolactin, just from about 3 to 8 in the morning.
Prolactin is always present in the female body in small amounts, its concentration in the blood increases significantly after the baby begins to breastfeed, most of all it is obtained in the morning hours from 3 to 8 in the morning. Prolactin, which appeared in the morning, is engaged in the production of milk during the day. It turns out who sucks at night, stimulates his mother's prolactin and provides himself with a decent amount of milk during the day. And whoever fails to suckle at night, he can quite quickly be left without milk during the day. No mammal takes a nightly break from feeding its young.
“I lost my milk because of my “nerves””
Milk production depends on the hormone prolactin, the amount of which depends on the number of times the baby is latched on and nothing else. The experiences of the mother on any occasion do not affect him. But the release of milk from the breast depends on the hormone oxytocin, which is engaged in the fact that it contributes to the contraction of muscle cells around the lobules of the gland and thereby contributes to the flow of milk. The amount of this hormone is very dependent on the psychological state of the woman. If she is frightened, tired, in pain or in any other discomfort during feeding, oxytocin stops working and milk stops flowing from the breast. A child cannot suck it out, a breast pump does not express it, and it cannot come out with its hands ...
The manifestation of the “oxytocin reflex” was observed by every breastfeeding woman: when a mother hears the crying of a child (and not necessarily her own), her milk begins to leak. The body tells the mother that it is time to apply the baby. In a situation of stress or fear, nothing like this is observed. (Relationship to the ancient instinct of self-preservation: if a woman runs from a tiger and she smells of leaking milk, the tiger will find and eat her faster, so while she runs in fear through the jungle with a child under her arm, the milk will not leak when she gets to the safety of the cave - and calmly settle down to feed the child, the milk will come again.)
Modern stressful situations work like those tigers. In order for milk to flow out again, you must try to relax during feeding, think only about the child. You can drink soothing herbs, shoulder massage, calm conversation helps well. Anything to help you relax. And most modern mothers are not able to relax during feeding, it is uncomfortable for them to sit or lie down, it can be painful to feed - all this prevents the manifestation of the oxytocin reflex - milk remains in the breast, which leads to a decrease in lactation.
"The baby is too fat, it is necessary to limit the number of feedings and give water"
A breastfed child gains 125 to 500 g per week, or 500 to 2000 g per month. Usually, by 6 months, a child born with a weight of 3-3.5 kg weighs about 8 kg. The rate of gain is very individual, there is never any talk of "overfeeding", children who are actively gaining weight grow rapidly in length and look proportionate. Children who gain 1.5-2 kg per month in the first half of life, usually sharply reduce weight gain in the second half of the year and can weigh 12-14 kg by the year. There is never a need to limit the number of feedings, much less to give water.
“Baby lacks nutrients, needs complementary foods from the age of 4 months”
The need for other food manifests itself in a child of about 6 months of age, when he begins to actively wonder what everyone is eating there. And if a mother takes a baby to the table with her, he begins to actively take an interest in the contents of his plate. This behavior is called active food interest, and it indicates that the child is ready to get acquainted with new food and can begin it. Nevertheless, breast milk remains the main food of the child in the first year of life, and in many cases even at the beginning of the second, contains absolutely all the nutrients the child needs and much more.
"A nursing mother should have a strict diet"
Food should be habitual. It is preferable not to use exotic foods in the diet that are not characteristic of the "native" climatic zone. A breastfeeding mother may have interesting nutritional needs, and they must be met in the same way as the desires of a pregnant woman. A woman should eat according to her appetite, and not stick food for two into herself. And, of course, you need to try to eat healthy food. Do not use products containing preservatives, dyes and other unhealthy substances.