35 week premature baby feeding
Feeding late preterm babies - La Leche League GB
What is a “late preterm” baby?Late preterm babies are usually defined as those born between 34 and 36 weeks gestation. Because these babies are often well – most don’t need to spend time in Special Care – and because they look like full-term babies (just a bit smaller), it’s often assumed that they will breastfeed easily from the start.
Babies born before 37 weeks gestation are treated as premature. Most late preterm babies do very well when they are born and, if they don’t need extra support with breathing, will usually stay with you. Your baby’s doctor will want your baby monitored closely over the next few days to ensure his temperature is fine, his blood sugars are in the normal range, he doesn’t need treatment for jaundice and that he is feeding well.
The following information may also be helpful if your baby was born at “early term” (37-39 weeks) but was small for gestational age, especially if under 2500g. It may also be helpful if your baby was born earlier than 34 weeks but is now at or after term age and still needs help with feeding.
Small babies – those born early and/or small for their gestational age – can be tricky to feed at first, and it’s helpful to be aware of this. They are sometimes known as “the Great Pretenders”, because they may spend a lot of time looking like they are feeding, but are not actually taking much milk! This is because, even when well positioned and deeply attached at the breast, and encouraged to feed as often and long as they want, they often just don’t have enough energy yet to take what they need from the breast. If they could, they would!
Giving birth earlyGiving birth to your baby early, especially if you weren’t expecting it, can be a shock. You might feel worried about looking after a small, early baby, and confused about what to expect, even if you’ve had a baby before. Doctors may be more involved in your baby’s care than if they had been born at term, and you might feel as if others are making decisions about your baby’s care which can be difficult to understand. Knowing about the special challenges of feeding these babies can help you to make sense of what is going on. Staff may be important partners in your baby’s care, but you, as the parents, are the most important people to your baby, so don’t be afraid to ask questions and make your wishes and feelings known.
Doctors may be more involved in your baby’s care than if they had been born at term, and you might feel as if others are making decisions about your baby’s care which can be difficult to understand. Knowing about the special challenges of feeding these babies can help you to make sense of what is going on. Staff may be important partners in your baby’s care, but you, as the parents, are the most important people to your baby, so don’t be afraid to ask questions and make your wishes and feelings known.
Some families know their baby or babies will be born early. You may have a condition which means it will be safer to give birth earlier, and have opted for an early induction of labour or a caesarean birth. Sometimes a placental problem is identified or the baby isn’t growing well and an early delivery may be the best option.
Antenatal expression of colostrumIncreasingly, mothers who know in advance that their babies will be born early are choosing to hand express colostrum (first milk) before their baby is born. Your body makes colostrum from as early as 16 weeks of pregnancy and with a little practice, you can learn to express (gently squeeze out) some of it, to keep until your baby needs it. It is usually recommended to start doing this at 36 weeks, but if you know that your baby is going to be born before this, you can discuss with your healthcare team whether it might be helpful in your situation, and if so, when to start.
Your body makes colostrum from as early as 16 weeks of pregnancy and with a little practice, you can learn to express (gently squeeze out) some of it, to keep until your baby needs it. It is usually recommended to start doing this at 36 weeks, but if you know that your baby is going to be born before this, you can discuss with your healthcare team whether it might be helpful in your situation, and if so, when to start.
Colostrum is usually yellow or orange in colour and known as “liquid gold” because it is so valuable for protecting your baby from infection and kick-starting their immature immune system. Any farmer will tell you that baby animals who get their mother’s colostrum do better than those who don’t! Expressed drops of colostrum can be frozen at home and brought into hospital at the time of birth. As well as having colostrum on hand should your baby need it, expressing before birth helps you get to know your breasts and to practise hand expression, so if you are separated from your baby, or they are slow to get going with breastfeeding, you will have a head start on expressing colostrum after birth.
You can find more information about expressing antenatally here: https://www.laleche.org.uk/antenatal-expression-of-colostrum/ and https://www.laleche.org.uk/hand-expression-of-breastmilk/
Skin to skin contactHolding your baby “skin to skin” (dressed just in a nappy, against your bare skin) has many benefits for all babies, but even more for late preterm babies. Ask hospital staff to help you and your baby enjoy skin to skin contact as soon as possible after birth; you will soon become confident about how to get yourself and your baby comfortable. The warmth of your body will help your baby stay warm and they will be calm and relaxed, saving their energy for feeding. Late premature babies are usually sleepy and you may only get a short “window” of alertness before they fall asleep again. While your baby is held against your chest you will get to know them and notice their subtle feeding cues as they move about, bobbing their head, licking their lips. You can gently help them move towards your breast and perhaps express some drops of colostrum onto your nipples for them to lick off. They may latch on and have a little suckle. Exploring your body and your breasts is an important part of your baby’s learning to breastfeed. If they aren’t quite ready to begin breastfeeding yet, there’s no rush to make them start. If your baby can breastfeed at all, even if they aren’t getting many calories from feeding yet, it can still be comforting and provide pain relief. You may be able to feed them through medical procedures such as having a cannula put in – your medical team may be surprised how little your baby cries, if you work with them to find ways of doing this!
You can gently help them move towards your breast and perhaps express some drops of colostrum onto your nipples for them to lick off. They may latch on and have a little suckle. Exploring your body and your breasts is an important part of your baby’s learning to breastfeed. If they aren’t quite ready to begin breastfeeding yet, there’s no rush to make them start. If your baby can breastfeed at all, even if they aren’t getting many calories from feeding yet, it can still be comforting and provide pain relief. You may be able to feed them through medical procedures such as having a cannula put in – your medical team may be surprised how little your baby cries, if you work with them to find ways of doing this!
Encouraging your baby to feed
Having a late preterm baby can be frustrating at times. Although they might look like a slightly smaller version of a full-term baby, you can see that their prematurity affects the way they breastfeed. Because they are immature, it is normal for their feeds to be sleepy and short, and for you to need to encourage them to wake and feed.
In the early months, most babies need to feed at least 8-12 times in 24 hours, with at least 5-20 minutes of active sucking per breast (deep sucks, with swallows after every 1-2 sucks for most of the feed). If your baby is too sleepy to do this much feeding yet, or if there are any signs that your baby might not be getting enough milk (fewer dirty nappies, more weight loss or slower weight gain than expected), it’s important to act quickly to keep your baby safely fed and to protect your milk supply. You can read more about how to tell if your baby is getting enough milk at https://www.laleche.org.uk/is-my-baby-getting-enough-milk/ and https://www.laleche.org.uk/whats-in-a-nappy/
Some babies need extra milk at firstIn the very early days, before your milk supply increases rapidly, and if they aren’t feeding vigorously yet, they may need more milk than the small quantities of colostrum you can express at this time. Depending on the hospital, there may be donor milk available or your baby’s doctor may suggest infant formula for a short time until your milk supply increases. In the early days and weeks after birth it is important to remove as much milk from your breasts as possible, as often as you can, to give your body a strong signal to make plenty of milk later. Staff will support you to hand express at first (usually for about 3-4 days) and then to use a breast pump. Make sure you know where and how you can rent or buy a breast pump for when you get home.
Depending on the hospital, there may be donor milk available or your baby’s doctor may suggest infant formula for a short time until your milk supply increases. In the early days and weeks after birth it is important to remove as much milk from your breasts as possible, as often as you can, to give your body a strong signal to make plenty of milk later. Staff will support you to hand express at first (usually for about 3-4 days) and then to use a breast pump. Make sure you know where and how you can rent or buy a breast pump for when you get home.
You can read more about how to use extra milk (expressed milk, donor milk or formula) to support breastfeeding here: https://www.laleche.org.uk/formula-supplements/
Growing into breastfeedingAs the days go by and they get closer to their due date, you will notice your baby getting better at breastfeeding. Their feeds are longer, their sucking feels stronger, they wake by themselves and tells you when they are hungry. You will start to find that they don’t want so much extra milk (and you may be able to express less), because they are taking more milk at the breast now. Keep closely in touch with your midwife or health visitor to ensure that as they take less extra milk, they continue to grow well. It’s really tempting to stop expressing as soon as your baby is feeding better, but it’s wise to be cautious at this stage, and to reduce expressing and extra milk feeds gradually, while keeping a close eye on your baby’s nappies and growth.
You will start to find that they don’t want so much extra milk (and you may be able to express less), because they are taking more milk at the breast now. Keep closely in touch with your midwife or health visitor to ensure that as they take less extra milk, they continue to grow well. It’s really tempting to stop expressing as soon as your baby is feeding better, but it’s wise to be cautious at this stage, and to reduce expressing and extra milk feeds gradually, while keeping a close eye on your baby’s nappies and growth.
Recent research has suggested that some late preterm babies drink more milk when using a silicone nipple shield. The firm shield seems to help the baby with a weak suck to grasp and remove milk more effectively from the breast. Not all late preterm babies will need a nipple shield, but they may be worth considering after day 4 or 5 if your baby is still very sleepy at the breast and their suck seems weak. You can find more information here: https://www.laleche.org.uk/nipple-shields/. You can talk to your midwife, health visitor or breastfeeding supporter about whether this is a suitable option for you and your baby.
You can find more information here: https://www.laleche.org.uk/nipple-shields/. You can talk to your midwife, health visitor or breastfeeding supporter about whether this is a suitable option for you and your baby.
Parents sometimes worry that if their baby isn’t breastfeeding at all yet, or is breastfeeding but needs to use tools such as shields or bottles as well, that they will forget how to breastfeed. You can be reassured that babies are strongly “hard-wired” to breastfeed, and will keep on trying for at least 8-12 weeks after birth. You will notice that when your awake baby is placed face-down on your body, they start to move themselves around, as if they are looking for something. If anything touches their head, they will turn towards it. They may smack their lips and suck their hands. These are all feeding behaviours which are going to be useful to them in the months to come, and they won’t disappear for many weeks. Getting breastfeeding going matters but is it also very important to get your milk supply going! In the meantime, spending lots of time holding your baby skin to skin gives them lots of time to practise their feeding behaviours and to enjoy being near the breast.
Getting breastfeeding going matters but is it also very important to get your milk supply going! In the meantime, spending lots of time holding your baby skin to skin gives them lots of time to practise their feeding behaviours and to enjoy being near the breast.
If your early baby is spending a lot of time at the breast, it can feel as if there aren’t enough hours in the day to express milk. Babies who aren’t feeding efficiently may spend most of their at-breast time sucking lightly (short, “fluttery” sucks, all the same length, with little or no swallowing) and complain when they are taken off the breast. Despite a lot of time spent “breastfeeding”, they don’t do as many dirty nappies as expected, or grow normally. When this happens, it’s important to know what needs to be done first, so you can spend your time effectively. Removing milk efficiently from your breasts, to feed your baby and build your milk supply, is the first priority. If your baby isn’t yet strong enough to do this themselves, you may need to limit their time at the breast for now, to free up enough time to express milk. Once you have a good milk supply, your baby has plenty of time to learn to breastfeed well when he is ready.
If your baby isn’t yet strong enough to do this themselves, you may need to limit their time at the breast for now, to free up enough time to express milk. Once you have a good milk supply, your baby has plenty of time to learn to breastfeed well when he is ready.
How milk supply works
Milk supply usually reaches its peak level within the first month after birth, with most of this increase occurring in the first couple of weeks. After this time, it tends to become more difficult to increase supply, and many mothers find it hard or even impossible to get more milk after about 4-6 weeks, however hard they work at it. This is why it’s so important to start expressing early and often, if your goal is for your baby to be fully breastfed when he is ready.
Some women do manage to get a significant supply increase later than this, though – you never know what you can do until you try! If you’ve had a slow start with your milk supply, and are wondering if you can increase it, find good local breastfeeding support as soon as possible.
Our article on how milk production works has more information you may find helpful.
Here are some tips on maximising your milk supply. For more information, please also see our article on increasing your milk supply.
- Use your breasts as much as you can. More milk out = more milk made. This is the main “rule” of milk supply, and much more important than any other factors, such as your diet, fluid intake, health or how unwell or tired you are (though of course you will feel better if you take good care of these things too!) Milk removal doesn’t have to be done regularly (with equal time gaps between), just as often as you can. While your baby is still small and tires quickly, it is likely that a breast pump is more effective than your baby at removing milk, so if you want to maximise your supply, it makes sense to prioritise expressing. Aim to express at least 8-12 times in 24 hours.
 Expressing doesn’t need to be regular; do it whenever is convenient for you, even if this means expressing several times close together (babies often feed like this too!) Try not to allow more than about 6 hours to go by without removing milk, though, since this causes your hormone levels to fall. The number of times per day you express is more important than the total time you express for, so if you only have a few minutes, it’s still worth it. You can of course use any time left over for breastfeeding as much as you like! Some mothers find that lining up 8-12 treats (e.g. chocolates or biscuits) each morning, and eating one each time they express, helps them to track how many times they are expressing, as well as rewarding them for doing it! If you have a competitive streak, you might enjoy aiming each day to beat how much milk you expressed yesterday!
Expressing doesn’t need to be regular; do it whenever is convenient for you, even if this means expressing several times close together (babies often feed like this too!) Try not to allow more than about 6 hours to go by without removing milk, though, since this causes your hormone levels to fall. The number of times per day you express is more important than the total time you express for, so if you only have a few minutes, it’s still worth it. You can of course use any time left over for breastfeeding as much as you like! Some mothers find that lining up 8-12 treats (e.g. chocolates or biscuits) each morning, and eating one each time they express, helps them to track how many times they are expressing, as well as rewarding them for doing it! If you have a competitive streak, you might enjoy aiming each day to beat how much milk you expressed yesterday! - Maximise efficiency at the breast. If there is any question about your baby’s effectiveness at the breast, skilled face to face breastfeeding support can help a lot.
 Often, a bit of adjustment to how your baby comes to the breast can help to make the most of the time that he is feeding. A slightly deeper attachment can make a big difference (and to your comfort as well, if you’ve had any pain or nipple damage). However, even with comfortable, deep attachment, a small or early baby tends not to have enough energy to remove all the milk they need, so just waiting until he grows a bit is likely to help a lot with their efficiency! In the meantime, switch nursing and breast compressions, both described here: https://www.laleche.org.uk/my-baby-needs-more-milk/ during feeds can help them to get more milk out in a shorter time. Switching sides keeps the baby interested – flow is faster on the “new” side – and compressions do some of the work for them. As your milk supply increases, breastfeeding is going to become easier for your baby – he won’t have to work so hard to get milk out – another great reason to invest effort in milk expression at this stage!
Often, a bit of adjustment to how your baby comes to the breast can help to make the most of the time that he is feeding. A slightly deeper attachment can make a big difference (and to your comfort as well, if you’ve had any pain or nipple damage). However, even with comfortable, deep attachment, a small or early baby tends not to have enough energy to remove all the milk they need, so just waiting until he grows a bit is likely to help a lot with their efficiency! In the meantime, switch nursing and breast compressions, both described here: https://www.laleche.org.uk/my-baby-needs-more-milk/ during feeds can help them to get more milk out in a shorter time. Switching sides keeps the baby interested – flow is faster on the “new” side – and compressions do some of the work for them. As your milk supply increases, breastfeeding is going to become easier for your baby – he won’t have to work so hard to get milk out – another great reason to invest effort in milk expression at this stage! - Use the most effective pump.
 For most women, this is a double electric “hospital grade” pump of the kind used in Special Care units, or the next size down. Smaller (single electrics, or manual) pumps are designed for casual use, perhaps once or twice a day, rather than the big job of establishing a milk supply for a baby who can’t yet feed effectively. Hospital grade pumps can be hired; your local LLL Leader may know of any pump agents in your area, or you can arrange hire online.
For most women, this is a double electric “hospital grade” pump of the kind used in Special Care units, or the next size down. Smaller (single electrics, or manual) pumps are designed for casual use, perhaps once or twice a day, rather than the big job of establishing a milk supply for a baby who can’t yet feed effectively. Hospital grade pumps can be hired; your local LLL Leader may know of any pump agents in your area, or you can arrange hire online. - Use “hands on pumping”. This is the most efficient technique that we know of, for getting the most milk in the shortest time. How much you use your hands is probably even more important than what kind of pump you use, and whether you pump one or both breasts at a time. “Double pumping” (both breasts at once) can be faster and more efficient, but some women find that it feels “too much” and prefer to express one breast at a time, using their hands to massage while they express. You can find some great pumping ideas to try here: https://med.
 stanford.edu/newborns/professional-education/breastfeeding/maximizing-milk-production.html. Hand expressing as much as you can after pumping is probably the most important tip – the better you can drain the breast, the faster it will make milk. A full hands-on expression session takes around 15-20 minutes, but it’s still worth expressing even if you don’t have more than a few minutes.
stanford.edu/newborns/professional-education/breastfeeding/maximizing-milk-production.html. Hand expressing as much as you can after pumping is probably the most important tip – the better you can drain the breast, the faster it will make milk. A full hands-on expression session takes around 15-20 minutes, but it’s still worth expressing even if you don’t have more than a few minutes. - Finish at the breast. Breastfeeding experts differ about exactly how to time formula or expressed milk supplements, but some say that the least helpful way to give them is always to offer them after breastfeeding. This encourages dissatisfaction at the breast, and tends to undermine your confidence. Supplements can either be given as a completely separate feed (not offering the breast at all), or in the middle of a breastfeed. As long as the baby gets the right amount of milk in each 24 hour period, it really doesn’t matter exactly how it’s timed! The goal is to finish on the breast as often as possible.
 It’s much nicer for your baby to feed off to sleep on the breast rather than the bottle, and for you to see them rolling off the breast looking full and happy! Even if he isn’t breastfeeding at all yet, you can let them end their feed of expressed milk or formula milk with their cheek pillowed on your breast as they fall asleep. A baby who enjoys being at the breast, and associates it with feeling satisfied, comfortable and happy, will be eager to breastfeed as soon as they are ready.
It’s much nicer for your baby to feed off to sleep on the breast rather than the bottle, and for you to see them rolling off the breast looking full and happy! Even if he isn’t breastfeeding at all yet, you can let them end their feed of expressed milk or formula milk with their cheek pillowed on your breast as they fall asleep. A baby who enjoys being at the breast, and associates it with feeling satisfied, comfortable and happy, will be eager to breastfeed as soon as they are ready. - Use feeding tools in ways that support breastfeeding. There are lots of ways to give your baby extra milk, if they need it. Hospital staff may suggest that you feed extra milk by cup, or by nasogastric (NG) tube. Sometimes, bottles are the most convenient way of giving extra milk. Babies are hardwired to breastfeed, and once the underlying feeding issues have been addressed (or they have matured a bit more), they will usually happily begin or continue breastfeeding, whether or not they’ve needed alternative feeding methods.
 Having said that, there are ways of using feeding tools that are more, and less, supportive of breastfeeding. However you choose to give extra milk, feed carefully and slowly, paying attention to your baby’s signals, to keep feeding calm for your baby and encourage behaviours that are useful at the breast. You can read more about cup-feeding, “paced” bottle feeding, side-lying bottle-feeding and other ways of giving extra milk here: https://www.laleche.org.uk/bottles-and-other-tools/
Having said that, there are ways of using feeding tools that are more, and less, supportive of breastfeeding. However you choose to give extra milk, feed carefully and slowly, paying attention to your baby’s signals, to keep feeding calm for your baby and encourage behaviours that are useful at the breast. You can read more about cup-feeding, “paced” bottle feeding, side-lying bottle-feeding and other ways of giving extra milk here: https://www.laleche.org.uk/bottles-and-other-tools/ - Consider domperidone. This is a prescription-only drug which has a side effect of increasing the levels of the hormone prolactin in your bloodstream. It isn’t magic, but there is good evidence that for some women domperidone can help to boost milk supply, when combined with intensive milk removal as described above. If your GP is not familiar with its use for this purpose (and it isn’t licensed for this use, so your GP needs to be willing to take responsibility for prescribing it), these are useful resources to share: Breastfeeding Network – domperidone factsheet and UKMi – “Drug Treatment of Inadequate Lactation”.

- Get support from other mothers who value what you are trying to do. Any LLL group will welcome a mother who is working on her milk supply, and the other mothers will highly value the effort you are putting in. We warmly welcome anyone who is interested in breastfeeding or providing their own milk for their baby, whether or not they are currently breastfeeding – please don’t feel awkward about giving extra milk at a LLL meeting. Many LLL groups are on Facebook too – it can be a great way to connect with other mothers whose babies have been born early, and who have overcome their early feeding challenges.
See also: www.laleche.org.uk/how-to-increase-your-milk-supply/
How much milk do I need to make?It might help to know that a week-old full-term baby takes about 500ml in 24 hours, rising to an average of 750ml in 24 hours by 2-4 weeks after birth and staying at this level until the baby starts eating other foods, around 6 months. Although every baby is different, with some babies needing more and some less milk than this, it can be helpful to have a rough idea in mind of how much milk to aim for when you’re expressing. Even if your small baby doesn’t need this much milk yet, if your goal is to feed them only on your milk, it makes sense to aim for a full supply, so that you will have plenty of milk for them as they grow.
Although every baby is different, with some babies needing more and some less milk than this, it can be helpful to have a rough idea in mind of how much milk to aim for when you’re expressing. Even if your small baby doesn’t need this much milk yet, if your goal is to feed them only on your milk, it makes sense to aim for a full supply, so that you will have plenty of milk for them as they grow.
Although formula instructions suggest increasing the amount in line with the baby’s weight (feeding a certain number of ml per kg of baby weight), human milk supply doesn’t work like this – the daily amount stays the same from about 1-6 months, and this is probably a better guide. If you can get to a full milk supply by the end of the first month, you’ll be making as much milk as your baby will ever need!
Babies often go through a “catch up” phase of drinking large volumes of milk and growing fast, until they catch up with their natural size. You can tell when this happens, because their growth curve settles on one of the “centile lines” on the chart in the red book. It is important to work closely with your health visiting team during this stage. You will probably want to weigh your baby at least once a week until you and your healthcare team are confident that your baby is feeding well.
It is important to work closely with your health visiting team during this stage. You will probably want to weigh your baby at least once a week until you and your healthcare team are confident that your baby is feeding well.
If your baby has needed some formula supplements, you can find information on how to use and perhaps reduce them here: https://www.laleche.org.uk/formula-supplements/ This is an art rather than a science, and it’s important to work with your local healthcare team and local feeding supporters with the skills and experience to work with late preterm babies.
Early/small babies just need a little more time and support
With time, and patience, this special group of babies can breastfeed beautifully – they just need some extra help at first, when they aren’t yet able to do all the work of feeding by themselves. Knowing what to expect, being prepared for the extra investment of effort, and finding good breastfeeding support will help you to reach your breastfeeding goals.
Key points
- If you know your baby will be born early, consider expressing colostrum antenatally. This gives you a headstart with feeding your baby and learning how to express milk by hand.
- Keep your baby close. Holding your baby against your skin will keep them calm and happy, encourage them to feed, save their energy for feeding and help you to notice the small signs that he wants to feed (like smacking their lips and sucking their hands). It’s the best way to get to know and enjoy each other.
- Keep your baby fed. Early/small babies might not ask to feed as often as they need to, and often tire quickly when feeding. Your baby needs to be fed at least 8-12 times in 24 hours. Short, frequent feeds usually work best. Encourage them to feed whenever they show interest. Watch your baby’s nappies and growth carefully to make sure he is getting enough milk. Some babies may need extra milk (expressed mother’s milk, donor breastmilk or formula milk) at first.

- Keep your milk flowing. Milk supply usually reaches its peak level (around 750ml in 24 hours on average) within 4 weeks of birth. Removing milk frequently in the early days and weeks gives your body a strong signal to make more milk. If your baby can’t take all they needs at the breast yet, express your milk with a pump and/or your hands, as often as you can, to keep your baby fed and ensure a good milk supply for when they are ready to breastfeed.
- Keep your goal in mind. Early/small babies will grow into breastfeeding, with time and patience. Their path might be more complicated, and involve more people, tools and time than a full-term baby. Get the support you need while you do some of the work of feeding for your baby, until they can do it all for themselves!
Further reading
www.laleche.org.uk/is-my-baby-getting-enough-milk
www.laleche.org.uk/how-to-increase-your-milk-supply
www. laleche.org.uk/hand-expression-of-breastmilk/
laleche.org.uk/hand-expression-of-breastmilk/
www.laleche.org.uk/how-milk-production-works
www.laleche.org.uk/bottles-and-other-tools
www.laleche.org.uk/formula-supplements/
www.laleche.org.uk/my-baby-needs-more-milk/
Written by Jayne Joyce, Ann Davison & Emily Tammam
Photos courtesy of Naomi Cotton, Becca Map, Roisin Keenan and Laura Loasby
Breastfeeding your premature baby - NHS
Your breast milk is important to your baby at any age. Giving your premature baby your breast milk benefits their health as well as yours.
Breast milk:
- helps protect your baby from infections, particularly of their gut – premature babies are more likely to get infections
- contains hormones, nutrients and growth factors that help your baby to grow and develop
- is easier for your baby to digest than formula milk, because it's human milk specially designed by your body for your baby
See other benefits of breastfeeding.
If your baby is very small or sick, they may not be able to breastfeed from your breast at first. But, you can start regularly collecting your breast milk (called expressing) as soon as possible after your baby's born. This will help get your milk supply going and the milk you express can be frozen so you can give it to your baby later. Then you can start breastfeeding from the breast once you and your baby are ready.
Even if you were not planning to breastfeed, you could express your breast milk for a while to help boost your baby's immune system in the early weeks after birth.
Spending lots of time close together with your baby can help boost your breast milk supply and establish breastfeeding.
Skin-to-skin contact with your premature baby
If your baby is well enough, you'll usually be encouraged to spend time holding them against your skin as soon as possible. This is sometimes called kangaroo care.
Your baby will usually be dressed just in a nappy, hat and socks and then placed inside your top, under a blanket, or in a soft sling so they can be held securely against your skin. If it's cold outside you can also put them in a sleeveless vest with an open neck.
If it's cold outside you can also put them in a sleeveless vest with an open neck.
This skin-to-skin contact helps you feel close to your baby. Your partner can enjoy this kind of contact as well.
For your premature baby, skin-to-skin contact:
- reduces stress and/or pain
- promotes healthy weight gain
- helps to establish breastfeeding
- helps them sleep better
- helps to regulate and support their heart rate and breathing
For mums, skin-to-skin contact:
- helps reduce your chance of developing postnatal depression
- increases your confidence as a new parent
- can help make breastfeeding easier and increase the amount of milk you make
For dads and partners, holding your baby skin to skin:
- helps you bond with your baby – babies can hear both parents' voices in the womb and will be calmed by the sound of your voice as well as their mum's
- helps you feel more confident as a parent
Expressing milk if your baby is premature
It's recommended you express often, ideally at least 8 times a day to begin with – including at least once at night – to keep your milk supply up.
In the early days, it's often easier to express your milk by hand. Your midwife or a breastfeeding supporter can show you how.
You'll probably only express a few drops to begin with but, if you hand express often, this will increase. Even if you are only expressing a small amount it will still help your baby.
In the early days you can collect your breast milk in a small, sterile cup and store it in a syringe.
Once you are producing more milk, you could try using a breast pump. If your baby is in a neonatal unit, the hospital will usually be able to lend you an electric breast pump for expressing your milk. If they cannot lend you one, you can hire one.
Read more about breastfeeding help and support to find out about hiring a pump, or phone the National Breastfeeding Helpline on 0300 100 0212.
The staff, your midwife or a breastfeeding supporter can give you advice about how to increase your milk supply. They can also show you how to encourage your milk to flow and how to use a breast pump.
Always ask for help early if you have any worries or questions.
Tube feeding your baby
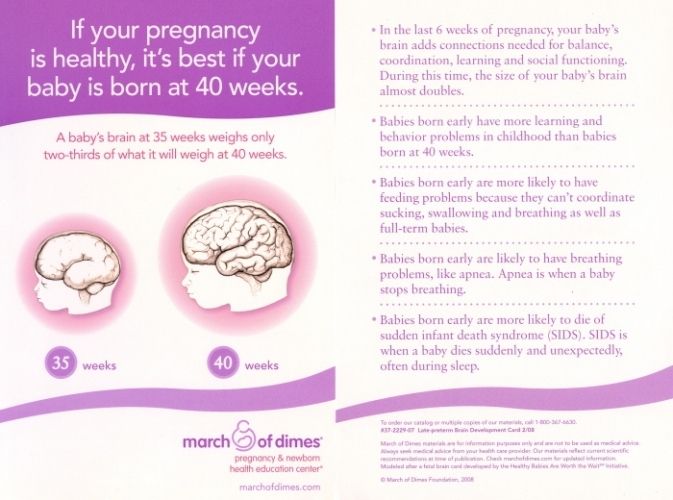
Babies do not normally learn to co-ordinate the sucking, swallowing and breathing needed for feeding until about 34 to 36 weeks of pregnancy.
If your baby is born before this time, they may need to have breast milk via a feeding tube to begin with. This goes through their nose or mouth into their stomach. The staff in the neonatal unit can show you how to feed your baby this way.
Babies who are very premature or sick may need to be fed via an intravenous (IV) line to begin with. A fluid containing nutrients is fed straight into your baby's vein.
Visit the Bliss website to read more about tube feeding.
Using donor breast milk
Some hospitals can provide donated breast milk for your baby to have until your own supply is established.
See the United Kingdom Association for Milk Banking (UKAMB) website for more about donor breast milk.
If donor breast milk is not available, your baby can have formula milk until you're producing enough breast milk.
It's recommended you do not buy donor milk over the internet. This is because the source cannot be confirmed and you cannot be sure whether the donor or the milk has been screened for infections.
Moving on to breastfeeding your premature baby
While holding your baby, you may notice them try to move towards your breast. Gradually, as they develop and get stronger, they will be able to breastfeed directly.
The first time you try it, the hospital staff may ask you to express first, then put your baby to your breast. This is so your baby is not overwhelmed when your milk lets down.
At first, your baby may only lick the breast, then next time take a few sucks until they gradually become happy and confident feeders.
You can combine tube feeding with breastfeeding until your baby is getting everything they need from the breast only.
Using a lactation aid (supplementer)
You could also consider using a lactation aid. This is a way of supplementing your baby's breastfeeds with either expressed breast milk or formula.
A tiny tube is taped next to your nipple so your baby can get milk via the tube as well as from your breast while attached to your breast. This helps to support your baby as they get used to attaching to the breast.
Visit healthtalk.org to see mums talking about feeding their sick or premature babies.
Got a breastfeeding question?
Sign into Facebook, or use an Amazon Alexa or Google Home and use the Start4Life Breastfeeding Friend chatbot for fast, friendly, trusted NHS advice anytime, day or night.
Feeding premature babies | Breastfeeding premature babies
Premature babies have a special need for breast milk, but it can be difficult to breastfeed them directly. Our expert advice will help you provide your premature baby with healthy breast milk.
Share this information
Professor Katsumi Mizuno, Department of Pediatrics, Showa University Koto Toyosu Hospital:
Katsumi is a Certified Breastfeeding Consultant, Professor of Pediatrics at Showa Medical University, and one of Japan's leading pediatric neonatologists. His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
Babies born before the 37th week of pregnancy are considered premature. 1 The causes of preterm birth are not always obvious, but certain factors increase the likelihood of such an event. These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth.
Because premature babies spend less time in the womb, they are not mature enough and may be more susceptible to infection and disease. They often require hospitalization in the neonatal intensive care unit.
Why is breast milk so important for premature babies?
Breast milk is essential for optimal growth and development of term babies, but it is even more important for premature babies.
During pregnancy, the fetus receives important substances from the mother through the placenta, such as DHA (a fatty acid essential for brain and eye development) and immunoglobulin G (an antibody). 2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. 4
In addition, premature babies have an underdeveloped gastrointestinal tract, which can make digestion and absorption of nutrients difficult, so they need food that their sensitive stomach and intestines can easily digest. Breast milk contains enzymes that make it easier for the baby to digest, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Breast milk is so important for premature babies that if the baby's mother does not produce enough breast milk at first for any reason, it is recommended that the deficiency be replenished with donor milk rather than formula.
Does breast milk improve the condition of premature babies?
Breast milk contains protective substances that can prevent serious diseases that preterm infants are susceptible to, 8 such as severe infections, 9 retinopathy of prematurity (which can cause vision loss) 10 and bronchopulmonary dysplasia (chronic lung disease). 11
The more milk your baby gets, the lower the risk of developing diseases. 12 Every additional 10 ml of milk per kilogram of body weight per day reduces the risk of sepsis by 19%. 9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
Most importantly, premature infants who are breastfed are typically discharged an average of two weeks earlier than formula-fed infants. 14 They also have a 6% lower risk of readmission in the first year of life. 15
Breast milk has been proven to have a beneficial effect on mental and physical development in the long term. Studies show that low-birth-weight babies who are breastfed in the neonatal intensive care unit have an average IQ of up to five points higher than those who are not breastfed. 15 In addition, their cardiovascular system works better during their lifetime. 17
Will milk be produced if the baby is born prematurely?
Yes, the mother's body is ready to produce milk by the middle of pregnancy. After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first.
After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first.
To replicate the sensations that trigger milk production, you can manually stimulate the breasts and nipples, or use a breast pump to express nutrient-rich colostrum for your baby. 18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
Breast milk usually comes in two to four days after birth, but if it was premature, the milk supply may be delayed. However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. 19 This is why it is important to start expressing breast milk as early as possible.
How to prepare if the baby is expected prematurely?
Visit the neonatal intensive care unit to see how it works and how premature babies are cared for. In addition, it will be useful to learn how breast milk is produced and secreted and why it is not only a healthy food, but also an important medicine for premature babies. Read more about this in our free e-book Surprising Breast Milk Facts .
What if a premature baby cannot breastfeed?
Many babies born before 34 weeks have difficulty coordinating sucking, swallowing and breathing. Until the baby masters these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
If your baby is too weak to latch on and suckle milk, you can use a breast pump* available at the hospital or maternity hospital to “do the job for the baby”. Breast stimulation with research-based technology, 20 mimics the rhythm of the baby's suckling, plays an important role in starting and maintaining milk production in the first hours after birth 21 .
Milk should be expressed at the same frequency as term infants are usually fed every two to three hours, i.e. 8 to 12 times a day.
You can try putting a small amount of expressed breast milk into the baby's mouth with a syringe, or putting milk-soaked cotton swabs in the baby's mouth. 22 This is how your baby learns the taste of your milk, which will facilitate the transition to breastfeeding in the future. In addition, the protective substances that make up breast milk will help strengthen the local immunity of the baby's oral cavity. You can be involved in the care of your premature baby in a variety of ways - check with your healthcare provider for details.
Very low birth weight babies - less than 1.5 kg - usually need extra protein, calcium and phosphorus, so they are given fortified breast milk. In some countries, such additives are made on human milk, and, for example, in Japan, on cow's milk.
Recommendations for pumping milk
If the baby will be in the neonatal intensive care unit for a long time, neonatologists recommend using a double breast pump for pumping. I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
In addition, I advise you to create the most comfortable conditions for pumping. It is generally agreed that it is best to express milk during or after prolonged skin-to-skin contact with the baby (more on this "kangaroo method" below). Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.
What is kangaroo care for premature babies?
The so-called kangaroo method involves prolonged skin-to-skin contact between parents and infant. This is extremely beneficial for you and your baby, as well as for milk production. Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
What if the neonatal intensive care unit offers formula feeding?
Feel free to state that you want to breastfeed your baby instead of formula. If you don't have enough breast milk to feed your baby, ask the ward for help to increase your milk supply.
It is natural for mothers whose babies are in the neonatal intensive care unit to experience anxiety and stress. Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
How to switch from pumping to breastfeeding?
At whatever gestational age a baby is born, if the baby is stable enough for skin-to-skin contact, it can seek the breast for sedative suckling. This is the perfect way for your baby to learn sucking skills before they learn to coordinate sucking, swallowing and breathing.
Babies love the smell of breastmilk, so you can put some milk on the nipple before putting your baby to the breast to make him want to suckle. He might even be able to suck some milk. Don't worry if your baby seems to suck very little - he learns every time. He can start with one or two sips and gradually move on to full breastfeeding. Until then, the baby can be fed through a tube, pressed to the breast, so that the taste of milk and touching the breast is associated with a feeling of satiety.
You can put your baby to the breast for sedative suckling as soon as you are ready for kangaroo care, unless your baby is suffering from bradycardia (slow heartbeat) or low oxygen levels in the blood. You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
Literature
1 World Health Organization. Geneva, Switzerland; 2018. Media Centre: Preterm birth fact sheet; November 2017 [03/26/2018]. Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - World Health Organization. Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article at: http://www.who.int/mediacentre/factsheets/fs363/en/
2 Duttaroy AK. Transport of fatty acids across the human placenta: a review. Prog Lipid Res . 2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
3 Palmeira P et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G through the placenta with healthy and pathological pregnancy. " Klin Virgo Immunol. 2012: 985646.
IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G through the placenta with healthy and pathological pregnancy. " Klin Virgo Immunol. 2012: 985646.
4 Underwood Ma. Human Milk Formature North Am . 2013;60(1):189-207. - Underwood, M.A., "Breast milk for the premature baby." 1):189-207.
5 Pamblanco M et al. Bile salt - stimulated lipase activity in human colostrum from mothers of infants of different gestational age and birthweight. Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al., "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights. " Akta Pediatr. 1987;76(2):328-331.
" Akta Pediatr. 1987;76(2):328-331.
6 Dvorak B. Milk epidermal growth factor and gut protection. J Pediatr. 2010;156(2): S 31-35. - Dvorak B., "Epidermal growth factor in milk and gut protection". F Pediatrician (Journal of Pediatrics). 2010;156(2):S31-35.
7 Taylor SN et al. Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
8 Newburg DS. Innate immunity and human milk. J Nutr . 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312.
9 Patel AL et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol . 2013;33(7):514-519.- Patel A.L. et al., "Impact of early breast milk on sepsis and health care costs in extremely low birth weight infants". Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
10 Zhou J et al . Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis." Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
11 Patel AL et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. 12 MEIER PP ET AL AL AL AL . Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." Perinatol wedge. (Clinical perinatology). 2010;37(1):217-245. 13 Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 14 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406. 15 Vohr BR et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. 16 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490. 17 Lewandowski AJ et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood. Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." Pediatrix (Pediatrics). 2016;138(1):pii:e20160050. 18 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36(7):493-499. 19 Parker LA et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." J Perinatol (Journal of Perinatology). 2012;32(3):205-209. 20 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants. 21 Parker LA et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91. 22 Lee J et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2): e 357-366. - Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. 23 Prime PK et al. 24 Uvn ä s Moberg K Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206. 25 Boundy EO et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2015;137(1): e 20152238. - Boundi I.O. and co-authors, "The Kangaroo Method and Its Impact on Newborns: A Meta-Analysis". 26 Acuña-Muga J et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. J Hum Lact . 2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." F Hum Lakt. 2014;30(1):41-46 27 Nyqvist KH et al. Towards universal kangaroo mother care: recommendations and report from the first European conference and seventh international workshop on kangaroo mother care. Acta Paediatr . 2010;99(6):820-826.- Nukvist K.H. et al., "On the Universality of the Kangaroo Method: Recommendations and Report from the First European Conference and the Seventh International Kangaroo Method Workshop". 28 American Academy of Pediatrics - Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics . 2012;129(3): e 827-841.- American Academy of Pediatrics - Section "Breastfeeding", "Breastfeeding and the use of breast milk". Pediatrix (Pediatrics). 2012;129(3): e 827-841. *RU No. ФСЗ 2010/06525 dated 03/17/2021 Premature babies If your baby is born too soon, the joy of having a baby can be overshadowed by health concerns and thinking about the possible consequences. Instead of returning home with the baby, holding him and caressing him, you will have to stay in the department, learn to cope with the fear of touching the baby, realize the need for treatment and various manipulations, get used to the complex equipment that surrounds him. In this situation, not only your baby needs help, you need it too! The best assistants are your loved ones, their love and care, as well as professional advice and recommendations from doctors and psychologists. This section of articles will help you improve your knowledge of preterm infant care, development and nutrition. Your help for the baby Previously, parents were often not allowed into the neonatal unit and, especially, into the intensive care unit because of the fear of infection of the baby, but now the contact of the parent with the child is recognized as desirable and is prohibited only in exceptional cases (for example, if parents have acute infections) Close communication between you and your baby is very important from the first days of his life. Even very immature premature babies recognize the voices and feel the touch of their parents. The newborn needs this contact. Studies have shown that it greatly contributes to the faster adaptation of an immature child to new conditions and the stabilization of his condition. By constantly and attentively observing the baby, parents can notice the smallest changes in his condition before others. In addition, communication in the hospital is a good practice that will undoubtedly come in handy after discharge. For parents, early physical contact with the baby is very valuable, because it allows them to feel him, despite the incubator and other obstacles, and show him their love. Treatment in the neonatal intensive care unit requires parents to have full confidence in all medical staff. Care of premature babies in the hospital Many premature babies cannot breathe, suckle and regulate their body temperature sufficiently after birth. Constant attention requires fluid loss due to the immaturity of the skin of premature babies and the insufficiency of thermoregulation processes. Modern approaches focused on nursing premature babies help to cope with these problems. Heat regulation incubator Premature babies are very susceptible to temperature fluctuations. At the same time, clothing can interfere with the monitoring of the baby's condition and its treatment. That is why an incubator is used to provide the conditions necessary for premature babies. It maintains a certain temperature and humidity, which change as the child grows. When the body weight of a premature infant reaches 1500-1700 g, he can be transferred to a heated bed, and after reaching a weight of 2000, most premature babies can do without this support. In incubators, very young premature babies are placed in special "nests" - soft hemispheres in which the baby feels comfortable and assumes a position close to intrauterine. It must be protected from bright lights and loud noises. For this purpose, special screens and coatings are used. Critical treatments during the first days of life of preterm infants with low and very low birth weight: Use of an incubator or heated bed. Oxygen supply for respiratory support. If necessary, artificial ventilation of the lungs or breathing using the CPAP system. Intravenous administration of various drugs and fluids. Carrying out parenteral nutrition with solutions of amino acids, glucose and fat emulsions. Don't worry: not all premature babies need such extensive treatment! Mechanical ventilation and CPAP for respiratory support When it comes to nursing, the provision of oxygen is of the utmost importance for premature babies. This new method made it possible to dispense with the majority of even very immature children without mechanical ventilation. The need for intubation of children has disappeared: during treatment with CPAP, oxygen is supplied through short tubes - cannulas that are inserted into the nasal passages. CPAP or mechanical ventilation is continued until the lungs can function at full capacity on their own. In order for the lungs to expand and remain in this state in the future, a surfactant is needed - a substance that lines the alveoli from the inside and reduces surface tension. Surfactant is produced in sufficient quantities starting from the 34-35th week of pregnancy. Basically, it is by this time that the formation of the lungs is completed. Parenteral nutrition - giving nutrient solutions by vein Premature babies, especially those born weighing less than 1500 g, are not able to get and absorb enough nutrients, even when fed through a tube. For the rapid growth of the baby, a large amount of nutrition is needed, and the size of the stomach is still very small, and the activity of digestive enzymes is also reduced. Therefore, such children are given parenteral nutrition. Special nutrients are injected into a vein using infusion pumps that deliver solutions slowly at a predetermined rate. In this case, amino acids necessary for building proteins, fat emulsions and glucose, which are sources of energy, are used. These substances are also used for the synthesis of a number of hormones, enzymes and other biologically active substances. Gradually, the volume of enteral nutrition increases, and parenteral nutrition decreases until it is completely canceled. Premature infants with gastrointestinal disease require parenteral nutrition for a longer period of time. By the time your grown baby is discharged from the hospital, everything should be well prepared at home. And this applies not only to the environment, clothes and means of caring for the child. All family members must be ready to receive the baby. Of course, the main care will fall on the shoulders of the parents. Although you have already gained some experience in the hospital, it is important to feel the support of others, especially in the early days. Older children can also help. The discharge of your baby is a great joy that you want to share with all your relatives. While you are getting used to your new role, it is important that nothing distracts you from communicating with your child. Preparing for discharge from the hospital Before discharge, you must make sure that: When can a child go home This question is very difficult to answer because all children are different. The stay in the hospital can last from 6 days to 6 months, depending on the degree of prematurity of the child, the severity of his condition, as well as the presence of certain complications. Of course, all parents look forward to the moment when the baby can be brought home. Long-term nursing of a premature baby is often a difficult test for you. But we must not forget that safety comes first, and the baby can be discharged home only when the doctors are confident in the stability of his condition. It is certainly in your interest as well. The rate of increase in body weight and length Weight gain is the main indicator of the growth of the baby and the adequacy of the treatment. The weight of the child, especially in the first days and weeks of life, is influenced by a number of factors: the presence of milk in the stomach (immediately after feeding), the time of bowel movement, the degree of filling of the bladder, the presence of edema. Therefore, if an edematous child does not gain weight for several days, and perhaps even loses it, do not worry. It should be remembered that children grow unevenly and periods of high weight gain alternate with lower ones. It is currently accepted that in the interval corresponding to 28-34 weeks of pregnancy, the normal weight gain of the child is 16-20 g/kg per day. Then it is reduced to 15 g/kg. It is also important to take into account the rate of increase in body length. With malnutrition, at first the child gains less weight (or even loses it), and with a more pronounced deficiency of nutrients, his growth is also disturbed. The weight must not only increase at a certain rate, but must also correspond to the length of the baby. An important parameter characterizing the development of the baby is an increase in the circumference of the head. The brain most actively increases in size during the first 12–18 months of life. But an excessively rapid increase in head circumference, as well as a slowdown in its increase, indicate neurological disorders. A premature baby can be discharged from the hospital if: The decision to discharge home is made for each patient individually. In addition to the state of health of the baby, the degree of preparedness of parents, their ability to provide high-level care for a premature baby is also taken into account. Feeding a premature baby after discharge Breastfeeding is the ideal way to feed premature babies. However, if the baby was born much premature and his birth weight did not exceed 1800-2000 g, his high nutritional requirements cannot be met by breastfeeding. The growth rate will be insufficient. Moreover, over time, the content of many nutrients, including protein, in milk decreases. And it is the main material for building organs, and primarily brain tissue. Therefore, proteins must be supplied to the body of a premature infant in the optimal amount. In addition, premature babies have a significantly increased need for calcium and phosphorus, which are essential for bone formation. In order for the baby's nutrition to be complete even after being discharged from the hospital, special additives - "enrichers" are introduced into breast milk in a certain amount, already less than in the hospital. They make up for the lack of protein in it, as well as some vitamins and minerals. As a result, the child receives them in the optimal amount. The duration of their use will be determined by your doctor. If there is not enough milk or it does not exist at all, children born prematurely should be transferred to artificial feeding. Complementary feeding of premature babies is carried out with special children's dairy products designed for children with low birth weight. This baby milk is ideally suited to both the ability of immature children to digest and assimilate nutrients, and their needs. Premature infant milk contains more protein, fat and carbohydrates than term infant milk, resulting in a higher calorie content. In specialized baby milk, the concentration of many minerals is higher, especially iron, zinc, calcium, phosphorus, as well as vitamins, including vitamin D. At present, specialized children's dairy products have been developed and used to feed premature babies after discharge from the hospital. In its composition, it occupies an intermediate position between a specialized product for premature babies and regular baby milk. Your baby will be transferred to such baby milk while still in the hospital. Feeding needs for premature babies Higher caloric intake because they need to gain weight faster than term babies. More protein as premature babies grow faster. More calcium and phosphorus for bone building. More trace elements and vitamins for growth and development. A premature baby grows faster than a term baby. Nutrition for such children is calculated taking into account body weight at birth, the age of the baby and its growth rate. As a rule, the calorie content of the daily diet is about 120-130 calories per 1 kg of body weight. Arch DIS Child Neonat ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261.
Arch DIS Child Neonat ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261.  1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523.
1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523.  Pediatrix (Pediatrics). 2006;118(1):e115-123.
Pediatrix (Pediatrics). 2006;118(1):e115-123.  - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
- Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.  " J Perinatol (Journal of Perinatology). 2012;32(2):103-110.
" J Perinatol (Journal of Perinatology). 2012;32(2):103-110.  Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.  Pediatrix (Pediatrics). 2015;137(1): e20152238.
Pediatrix (Pediatrics). 2015;137(1): e20152238.  Akta Pediatr. 2010;99(6):820-826.
Akta Pediatr. 2010;99(6):820-826. Read instructions before use. Consult a specialist about possible contraindications.
Your child was born prematurely | Regional perinatal center

 The baby's resistance to therapy increases, he absorbs large amounts of food and quickly begins to suck on his own. Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.
The baby's resistance to therapy increases, he absorbs large amounts of food and quickly begins to suck on his own. Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.  Only in the last weeks of pregnancy is the maturation of the lungs, gastrointestinal tract, kidneys, brain, which regulates and coordinates the work of all organs and systems.
Only in the last weeks of pregnancy is the maturation of the lungs, gastrointestinal tract, kidneys, brain, which regulates and coordinates the work of all organs and systems.  There are no strict rules here: when nursing children with low body weight, doctors are guided by the severity of the condition of each premature baby and its degree of maturity.
There are no strict rules here: when nursing children with low body weight, doctors are guided by the severity of the condition of each premature baby and its degree of maturity.  In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.  If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.
If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.  Additionally, minerals and vitamins are introduced.
Additionally, minerals and vitamins are introduced.  Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.
Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.


 It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.

 Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.  You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is not gaining weight well, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is not gaining weight well, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies. 











