4 month baby bottle feeding
Formula Feeding FAQs: How Much and How Often (for Parents)
Whether you plan to formula feed your baby from the start, want to supplement your breast milk with formula, or are switching from breast milk to formula, you probably have questions.
Here are answers to some common questions about formula feeding.
How Often Should I Feed My Baby?
Newborns and young babies should be fed whenever they seem hungry. This is called on-demand feeding.
After the first few days of life, most healthy formula-fed newborns feed about every 2–3 hours. As they get bigger and their tummies can hold more milk, they usually eat about every 3–4 hours. As babies get older, they’ll settle into a more predictable feeding routine and go longer stretches at night without needing a bottle.
Talk to your doctor if you have concerns about feeding your baby, especially if your baby is very small, is not gaining weight, or was born early (prematurely).
How Can I Tell When My Baby Is Hungry?
Signs that babies are hungry include:
- moving their heads from side to side
- opening their mouths
- sticking out their tongues
- placing their hands, fingers, and fists to their mouths
- puckering their lips as if to suck
- nuzzling again their mothers' breasts
- showing the rooting reflex (when a baby moves its mouth in the direction of something that's stroking or touching its cheek)
Babies should be fed before they get upset and cry. Crying is a late sign of hunger. But every time your baby cries is not because of hunger. Sometimes babies just need to be cuddled or changed. Or they could be sick, tired, too hot or too cold, in pain, or have colic.
How Much Should My Baby Drink?
In the first few weeks, give 2- to 3-ounce (60- to 90-milliliter) bottles to your newborn. Give more or less depending on your baby’s hunger cues.
Here's a general look at how much your baby may be eating at different ages:
- On average, a newborn drinks about 1.5–3 ounces (45–90 milliliters) every 2–3 hours. This amount increases as your baby grows and can take more at each feeding.
- At about 2 months, your baby may drink about 4–5 ounces (120–150 milliliters) every 3–4 hours.
- At 4 months, your baby may drink about 4–6 ounces (120-180 milliliters) at each feeding, depending on how often they eat.
- By 6 months, your baby may drink 6–8 ounces (180–230 milliliters) about 4–5 times a day.

Watch for signs that your baby is hungry or full. Respond to these cues and let your baby stop when full. A baby who is full may suck with less enthusiasm, stop, or turn away from the bottle.
Why Does My Baby Seem Hungrier Than Usual?
As babies grow, they begin to eat more at each feeding and can go longer between feedings. Still, there may be times when your little one seems hungrier than usual.
Your baby may be going through a period of rapid growth (called a growth spurt). These can happen at any time, but in the early months are common at around:
- 7–14 days old
- between 3–6 weeks
- 4 months
- 6 months
During these times and whenever your baby seems especially hungry, follow their hunger cues and continue to feed on demand, increasing the amount of formula you give as needed.
Is My Baby Eating Enough?
At times, you may wonder whether your baby is getting enough nutrients for healthy growth and development. Babies who get enough to eat seem satisfied after eating and are regularly peeing and pooping.
Babies who get enough to eat seem satisfied after eating and are regularly peeing and pooping.
At your baby’s checkups, the doctor will review your baby’s growth chart, track your little one’s development, and answer any questions. Talk to your doctor if you have any concerns about your baby’s feeding and nutrition.
Reviewed by: Mary L. Gavin, MD
Date reviewed: November 2021
Bottle-Feeding (Formula) Questions
Is this your child's symptom?
- Formula and bottle-feeding questions
Topics Covered for Formula Feeding
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice:
- Types of formulas
- Switching formulas and milk allergies
- Powdered versus liquid formulas
- Whole cow's milk, 2%, 1% and skim milk
- Vitamins and iron
- Water to mix with the formula
- Extra water
- Amounts: how much per feeding?
- Schedules or frequency of feedings
- Length of feedings
- Night feedings: how to eliminate?
- Formula temperature
- Formula storage
- Cereals and other solids
- Burping
- Baby bottle tooth decay
- Traveling
- Nipples and bottles
- Normal stools
- Breast discomfort
When to Call for Bottle-Feeding (Formula) Questions
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Dehydration suspected.
 No urine in more than 8 hours, dark urine, very dry mouth and no tears.
No urine in more than 8 hours, dark urine, very dry mouth and no tears. - Will not drink or drinks very little for more than 8 hours
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Does not seem to be gaining enough weight
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bottle-feeding question about a healthy baby
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Bottle (Formula) Feeding
- Types of Formulas:
- Milk-protein formulas, soy-protein formulas, and hydrolysate formulas
- Soy formulas don't contain lactose or cow's milk protein.
 Currently, 20% of infants in the U.S. are fed soy formula. Often, switching to soy is not done with a valid reason.
Currently, 20% of infants in the U.S. are fed soy formula. Often, switching to soy is not done with a valid reason. - Hydrolysate formulas mean the protein is broken down. These are advised when children are sensitive to both soy and milk protein.
- Switching Formulas and Milk Allergies:
- Switching from one milk-based formula to another is not helpful for any symptom. It is also not harmful.
- Switching from milk formula to soy formula is sometimes helpful for severe diarrhea. This may occur from temporary low lactase levels. It may also be used for those families who are vegetarian.
- Switching from milk formula to soy is sometimes helpful for cow's milk allergy. A cow's milk allergy occurs in 1-2% of infants. Most often, protein hydrolysate formulas (such as Alimentum) are advised. This is because 15% of these infants are also allergic to soy protein.
- Switching formulas for frequent crying, spitting up or gas is rarely helpful.

- Don't switch formulas without talking with your child's doctor.
- Powdered versus Liquid Formulas:
- Formulas come in 3 forms: powder, concentrated liquid and ready-to-feed liquid.
- Concentrated formulas are mixed 1:1 with water.
- Ready-to-feed formulas do not need any added water.
- Powdered formulas are mixed 2 ounces (60 mL) of water per each level scoop of powder. Never add extra water because dilute formula can cause a seizure.
- Powdered formula costs the least. Ready-to-feed formula costs the most.
- Powdered formula is the easiest to use to supplement breastfeeding.
- Ready-to-feed formula is the easiest to use for traveling.
- Whole Cow's Milk, 1%, 2% and Skim Milk:
- Cow's milk should not be given to babies before 12 months of age. Reason: raises risk of iron deficiency anemia.
- Skim milk (fat free milk), 1% low fat milk or 2% milk should not be used before 2 years.
 Reason: the fat content of whole cow's milk (3.5%) is required. It is needed for rapid brain growth.
Reason: the fat content of whole cow's milk (3.5%) is required. It is needed for rapid brain growth.
- Vitamins and Iron:
- For all infants, use a formula that has iron in it. This helps to prevent iron deficiency anemia.
- The iron amount in iron-fortified formulas is too small to cause any symptoms. Iron in formulas does not cause constipation or diarrhea.
- Iron-fortified formulas contain all the vitamins and minerals needed.
- Extra vitamins are therefore not needed for infants taking formula.
- Fluoride. Babies no longer need to take fluoride drops. Reason: the fluoride in toothpaste works very well. For children at high risk for tooth decay, your dentist may use fluoride varnish.
- Water to Mix With the Formula:
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. Reason: to avoid potential lead exposure.
 Heat cold water to desired temperature. Add this to powder or formula concentrate.
Heat cold water to desired temperature. Add this to powder or formula concentrate. - Exceptions:
- Untested well water or
- City water with recent contamination or
- Developing countries with unsafe water supply or
- Your child has decreased immunity.
- For these conditions, use distilled water, bottled water, or filtered tap water.
- Another option is to use city water or well water that has been boiled. Boil for 10 minutes. Add 1 extra minute per each 1,000 feet (305 meters) of elevation.
- Bottled water costs more than distilled water.
- If making a batch of formula, distilled, bottled or boiled water is needed.
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. Reason: to avoid potential lead exposure.
- Extra Water:
- Babies less than 6 months of age should not be given any extra water. Reason: regular formula is 85% water. Also, water can cause harm at this age.
- Infants older than 6 months of age can have some extra water. Reason: water may be needed after starting solid foods or if weather is very hot.
 Safe at this age.
Safe at this age. - Limit water for infants age 6 to 12 months: don't give more than 4 ounces (120 mL) of extra water per day. On hot days, can give up to 8 ounces (240 mL) per day (AAP).
- Amounts - How Much Per Feeding: Newborn to 6 Months Old
- The average amount of formula that babies take per feeding is:
- Newborn: 1-2 ounces (30-60 mL) per feeding
- 1 month old: 3-4 ounces (90-120 mL) per feeding
- 2 months old: 5 ounces (150 mL) per feeding
- 4 months old: 6 ounces (180 mL) per feeding
- 6 months old: 7-8 ounces (210-240 mL) per feeding
- The amount can vary depending on the baby's weight and if the baby is going through a growth spurt.
- A baby's appetite varies throughout the day. If the infant stops feeding or loses interest, the feeding should be stopped.
- If healthy babies are not hungry at several feedings, increase the feeding interval.
- The most amount of formula advised per day is 32 ounces (1 liter).

- Over-feeding can cause vomiting, diarrhea or too much weight gain.
- If your baby needs over 32 ounces (1 liter), talk to your doctor about starting solids.
- Get rid of any formula left in bottle at end of each feeding. Do not reuse this leftover formula. Reason: contains germs that can grow.
- Frequency of Feedings (Schedules): Babies mainly need to be fed when they are hungry. If your baby is fussy and it's been more than 2 hours, feed him. Some guidelines are listed below:
- From birth to 3 months of age, feed every 2 to 3 hours.
- From 3 to 9 months of age, feed every 3 to 4 hours.
- Infants often set their own schedule by 1 to 2 months of age.
- Length of Feedings:
- Feedings shouldn't take more than 20 minutes.
- If the feeding is prolonged, check the nipple to be sure it isn't clogged.
- A clean nipple should drip about 1 drop per second. Check this when the bottle of formula is turned upside down.

- Night Feedings - How to Get Rid of Them:
- Most newborns need to be fed at least twice each night.
- Most formula-fed babies give up night feedings by 4 months of age. The tips below can help your baby sleep for longer stretches during the night:
- Keep daytime feeding intervals to at least 2 hours. Slowly stretch them to 3 hours.
- During daytime, your baby shouldn't sleep for more than 3 hours at a time. If your baby naps longer than that, wake him for a feeding.
- Place your baby in the crib drowsy but awake. Don't bottle-feed or rock until asleep.
- Make middle-of-the-night feedings brief and boring compared to daytime feedings. Don't turn on the lights or talk to your child. Feed him rather quickly.
- Formula Temperature:
- Most babies like formula at body temperature.
- In the summertime, some infants prefer formula that's cooler.
- In the wintertime, some prefer warm formula.

- The best temperature is the one your infant prefers. Either way, there's no health risk involved.
- Just make sure the formula is not too hot. Reason: it can burn your baby's mouth.
- Formula Storage:
- If you can, make your child's formula fresh for each feed. However, if formula needs to be made ahead of time:
- Prepared formula should be stored in the refrigerator. It must be used within 24 hours.
- Open cans of formula should also be kept in the refrigerator. They should be covered and used within 24 hours.
- Prepared formula left at room temperature for more than 1 hour should be discarded.
- Leftover used formula should always be tossed. Reason: contains germs that can grow.
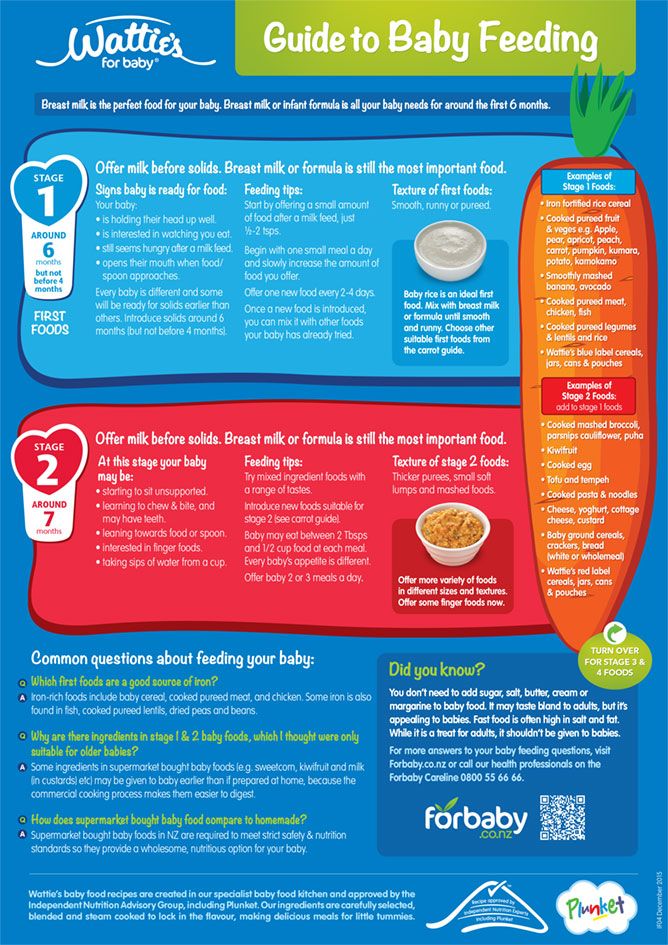
- Cereals and Other Solids:
- Bottle-fed infants should be started on baby foods around 6 months of age. First baby foods can be cereals and/or fruit.
- Starting before 6 months is not needed.
 Starting before 6 months makes feedings messier and longer. Early use of solids can also cause gagging.
Starting before 6 months makes feedings messier and longer. Early use of solids can also cause gagging. - Solids don't increase sleeping through the night for bottle-fed infants.
- Delaying solids past 9 months of age is not advised. The delay runs the risk that your infant will refuse solids.
- Burping:
- It is not harmful if a baby doesn't burp.
- Burping is an option, but not required.
- It can decrease spitting up, but it doesn't lessen crying.
- Burping can be done twice per feeding, once midway and once at the end.
- If your baby does not burp after 1 minute of patting, it can be stopped.
- Baby Bottle Tooth Decay:
- Some older infants and toddlers are used to a bottle before sleeping.
- Falling asleep with a bottle of milk or juice can cause severe tooth decay.
- Prevent this bad habit by not using the bottle as a pacifier. Also, do not use the bottle as a security object.

- If you cannot stop the bottles, fill it with water. Use water instead of formula or milk at bedtime.
- Traveling:
- Use bottles of ready-to-feed formula (most expensive).
- Or mix formula ahead of travel and carry in a cold insulated container.
- Or use powered formula. Put the required number of scoops in a bottle. Carry clean water in a separate bottle. Mix before each feeding.
- Nipples and Bottles:
- Any nipple/bottle products are fine.
- It is not necessary to sterilize bottles or nipples. Wash them with soap and water. Rinse them thoroughly.
- It is also safe to wash bottles and nipples in the dishwasher.
- Formula-fed Stools, Normal:
- Meconium Stools are dark greenish-black, thick and sticky. They normally are passed during the first 3 days of life.
- Transitional Stools are a mix of meconium and milk stools.
 They are greenish-brown and looser. They are passed day 4 to 5 of life.
They are greenish-brown and looser. They are passed day 4 to 5 of life. - Normal Milk Stools without any meconium are seen from day 6 on.
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter. Green stools are also normal (usually caused by bile).
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They are soft and solid.
- Breast Discomfort in Bottle-feeding Mothers:
- Even though you chose not to breastfeed, your breasts will make milk. Breast milk comes in on day 2 or 3. Swollen breasts can be painful for a few days. Here is what to do:
- Ibuprofen. Take 400 mg of ibuprofen (such as Advil) 3 times per day. This will help to lessen pain and swelling. There's no special prescription medicine for this.

- Cold Pack. Use a cold pack or ice bag wrapped in a wet cloth. Put it on your breasts for 20 minutes. Do this as often as needed. This will decrease milk production. Do not use heat. Heat will increase milk production.
- Pumping. For moderate pain, hand express or pump off a little breast milk. This will help to reduce your pain. Pumping breast milk can increase milk production. But, doing this to take the edge off your discomfort is not harmful.
- Bra. Wear a bra that offers good breast support or a sports bra. Wear it 24 hours a day.
- Binding. Binding the breasts by wearing a tight bra is no longer advised. Binding by using an elastic wrap is also not advised. Binding can increase the risk of breast infections (mastitis).
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/06/2022
Last Revised: 09/18/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Bottle feeding
When breastfeeding is not possible, or there is not enough breast milk and supplementary feeding is required, the use of infant milk formulas allows you to establish good nutrition for the baby.
The mixtures contain all the necessary nutrients, vitamins and trace elements. As a rule, they are well tolerated and digested, especially if the feeding process is properly established.
If you plan to bottle feed or supplement your baby with formula, our article will help you navigate the basic rules and intricacies of artificial feeding.
How to choose a teat (nozzle) for a bottle
Teats differ in composition (silicone, latex), shape and flow rate. While the shape of the nipple and the material are often chosen according to the preferences and needs of a particular baby, the flow rate is strictly determined by the age category.
Babies are fed from birth using the slowest flow nipple (these are usually labeled from 0 and one drop). Next, the teat flow rate in most bottle manufacturers increases at 3 months, 6 months, 12 months.
In order not to be mistaken, pay attention to the labeling and the age group for which the nipple to the bottle of the selected manufacturer is intended.
Whether such a nipple is right for you, you will also probably be able to understand during feeding.
- The baby should be able to comfortably grip the nipple and drink formula confidently (without too much effort).
- He should not choke/choke frequently.
- The mixture should flow well. If the mixture does not flow until you shake the bottle, the hole may be clogged with powder.
- If the mixture flows too much, check if the nipple is not torn.
How to treat the bottle
For newborn babies in the first months of life, it is recommended to sterilize the bottles before each feeding. Sterilization is the immersion of all feeding accessories (bottles, nipples, other parts) in boiling water for about 5 minutes to destroy pathogenic microflora.
Sterilization is the immersion of all feeding accessories (bottles, nipples, other parts) in boiling water for about 5 minutes to destroy pathogenic microflora.
You can choose any convenient method of sterilization: using a special device (sterilizer), in a microwave oven, dishwasher, ordinary boiling. Read more about how to properly sterilize bottles in our other article.
It is important to ensure that the baby bottle you use is made of safe plastic that can be heated. Some types of plastic release harmful chemicals when heated. As a rule, information about the possibility of sterilization and heating is indicated on the packaging. If there is no such information, it is not worth the risk. Use special baby bottles from well-known manufacturers. For example, a Dino Reno feeding bottle with nipple can be sterilized completely by any of the listed methods.
How to prepare formula and feed your baby
- Wash your hands with soap and water and dry with a dry towel.

- Remove the bottle and nipple from the sterilizer using the special holder (tweezers), assemble the bottle with the nipple, being careful not to touch the part that will go into the baby's mouth with your hands.
- Take boiled or special baby water heated to body temperature, dilute the mixture in the proportion indicated on the package.
- Use the special measuring spoon for preparation (it is included in each box with the mixture).
- Dilute the mixture strictly in the proportion indicated by the manufacturer. A thicker or thinner formula can harm your baby and cause stomach problems.
- Shake the bottle thoroughly to mix the contents evenly. Make sure that there are no lumps and clots left in the liquid and on the walls of the bottle.
- Check the temperature of the prepared mixture by dropping a little liquid on your wrist, it should not burn.
- Hold the bottle at the right angle. So that the tip of the nipple is always filled with milk and not with air.
- After feeding, hold the baby upright, let him burp the excess air.
- Feed your baby only fresh formula. According to the recommendations of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) of 2004, the reconstituted dry formula can be stored in a sealed bottle at a cool temperature for no more than 4 hours.
- If the mixture has cooled down, it can be warmed up with a special heater or in a water bath.
- If you are going on a long trip or outing, do not prepare the formula ahead of time. Better just pour the required amount of water into the bottle, and pour the right amount of the mixture into a separate container. Mix before feeding.
You will also find recommendations on the amount of formula to eat at a time, taking into account the age of the child, on the package. But some features of the baby's behavior can tell you whether he is full or not.
- If the baby pushes the nipple out of the bottle with his tongue and spit out the formula, he is probably already full and the feeding should be stopped.

- If the baby drank the contents of the bottle quickly and is crying, he may not have eaten enough and it is time to increase the portion.
- When your baby grows up, a feeding bottle with handles will come to your rescue. The child will be able to hold it himself and regulate the amount eaten.
Baby won't take bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ Top
In most cases, switching a baby from breastfeeding to bottle feeding does not cause any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing the bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full.
 So the child can eat at his own pace.
So the child can eat at his own pace. - Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple is weak or too fast for the baby, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses a bottle
If you've followed the steps above and your baby still refuses a bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain body contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast. Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast.
 Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Give preference to nipples with an anti-colic valve that vents air out of the bottle. Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
Refs:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", Russian Federation, 02.10.2012
1 . 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website.