Baby aspirated food
Aspiration in Babies and Children
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is aspiration in babies and children?
Aspiration is when something enters the airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen when a person has trouble swallowing normally. This is known as dysphagia. It can also happen if a child has gastroesophageal reflux disease (GERD). This is when the contents of the stomach come back up into the throat.
When your child swallows food, it passes from the mouth down into the throat. This is called the pharynx. From there, the food moves down through a long tube (esophagus) and into the stomach. This journey is made possible by a series of actions from the muscles in these areas. If your child has dysphagia, the muscles don’t work normally. They cause problems with the swallowing process.
The pharynx is also part of the system that brings air into the lungs. When a person breathes, air enters the mouth and moves into the pharynx. The air then goes down into the main airway (trachea) and into the lungs. A flap of tissue called the epiglottis sits over the top of the trachea. This flap blocks food and drink from going down into the trachea when your child swallows. But in some cases, food or drink can enter the trachea. It may go down as your child swallows. Or it may come back up from the stomach. A child with dysphagia is much more likely to aspirate. A child with a developmental or health problem is more likely to have dysphagia.
Aspiration can happen during a feeding or meal. And it can happen after a feeding or meal. This is common in babies and children with certain health conditions. Aspiration can also happen at any time when your child swallows saliva.
If your child aspirates a small amount of material, it may not cause much harm. This can happen in children who don’t have a health problem. It can happen when eating, sleeping, or talking. But aspiration that happens often or in a large amount can be serious.
What causes aspiration in babies and children?
Aspiration is often caused by dysphagia. This is when the muscles don’t work normally in the throat and lead to swallowing problems. Different medical conditions can lead to this, such as:
- Abnormal anatomy, such as a cleft palate or a problem in the esophagus
- Delayed growth, from premature birth or a condition such as Down syndrome
- Brain damage or other problems, such as from cerebral palsy or infection
- Problems with the cranial nerves that control the muscles of swallowing
- Neuromuscular disease, such as spinal muscular atrophy
- Medical procedures, such as a nasogastric tube or a tracheostomy
Gastroesophageal reflux disease (GERD) can also cause aspiration. This is when the contents of the stomach come back up into the throat.
This is when the contents of the stomach come back up into the throat.
What are the symptoms of aspiration in babies and children?
Aspiration can cause signs and symptoms in a baby such as:
- Weak sucking
- Choking or coughing while feeding
- Other signs of feeding trouble, like a red face, watery eyes, or facial grimaces
- Stopping breathing while feeding
- Faster breathing while feeding
- Voice or breathing that sounds wet after feeding
- Slight fever after feedings
- Wheezing and other breathing problems
- Repeated lung or airway infections
And aspiration can cause signs and symptoms in an older child such as:
- Choking or coughing while eating
- Voice that sounds wet after eating
- Slight fever after meals
- Complaints of food feeling stuck or coming back up
- Wheezing and other breathing problems
- Repeated lung or airway infections
Signs and symptoms can happen right after eating. Or they may happen over time. Your child may not have all of these signs and symptoms. The signs and symptoms may depend on the age of your child, and how often and how much your child aspirates.
Or they may happen over time. Your child may not have all of these signs and symptoms. The signs and symptoms may depend on the age of your child, and how often and how much your child aspirates.
Some children who aspirate do not have any signs or symptoms. This is called silent aspiration.
How is aspiration in babies and children diagnosed?
Your child will need to be checked for aspiration if he or she has:
- Any signs or symptoms of aspiration
- Health problem that can cause trouble swallowing
- GERD
The healthcare provider will ask about your child’s medical history and symptoms. This may be done by a speech-language pathologist (SLP). The SLP may ask about what foods or drink cause problems, and when your child’s symptoms happen. He or she may want to watch your child during a feeding.
Your child may also need tests. These can check for problems and show if food and fluid is going into your child’s lungs. The tests may include:
The tests may include:
- Chest X-ray or CT scan
- Modified barium swallow test (MBS)
- Fiber optic endoscopic evaluation of swallowing (FEES)
How is aspiration in babies and children treated?
Treatment for aspiration may vary depending on the cause and severity. Treatments for your child may include:
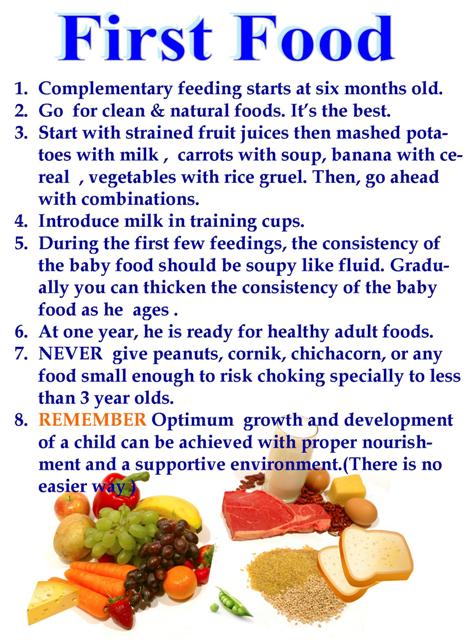
- Making changes in position and posture during meals
- Changing the thickness of liquids
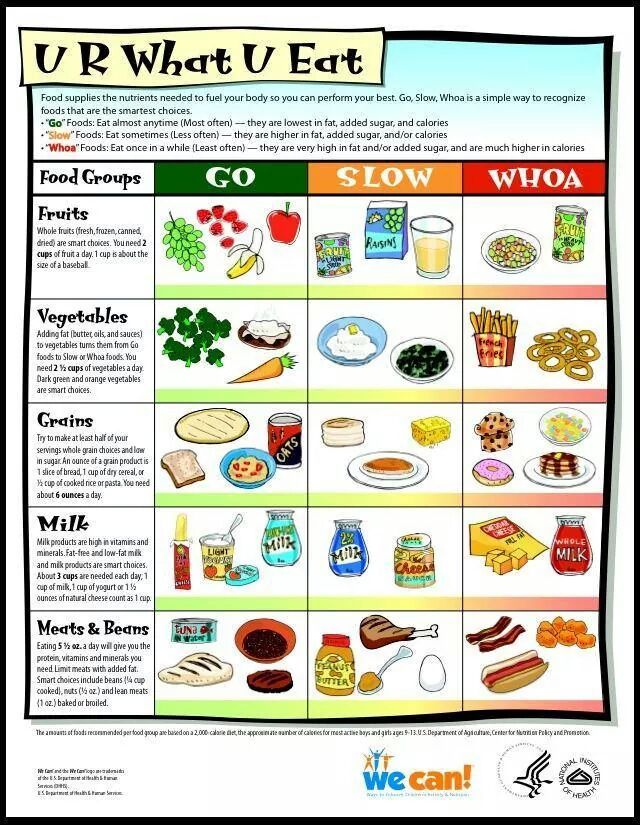
- Changing the types of foods in your child’s diet
- Doing exercises to help with swallowing (for an older child)
- Medicines for GERD
- Medicines or Botox injection for children who make excess saliva
- Surgery to reduce reflux
- Surgery to correct a problem such as a cleft palate
If your child still has a high risk of aspiration despite these methods, he or she may need a special tube to help with eating for a while. The feeding tube will help your child get good nutrition until his or her risk of aspiration improves. Your child will not eat or drink normally until the tube is removed. A thin tube may be put through the nose down into the stomach. This is called a nasogastric tube. This may be used for a short time while other treatment is considered. Or a tube may be put directly into your child’s stomach during a surgery. This is called a gastrostomy tube.
The feeding tube will help your child get good nutrition until his or her risk of aspiration improves. Your child will not eat or drink normally until the tube is removed. A thin tube may be put through the nose down into the stomach. This is called a nasogastric tube. This may be used for a short time while other treatment is considered. Or a tube may be put directly into your child’s stomach during a surgery. This is called a gastrostomy tube.
In some children, aspiration lessens over time. In other cases, a child may need more treatment to address the cause. Your child’s healthcare providers will carefully watch your child so that he or she can return to normal eating as soon as possible.
Talk with your child’s healthcare provider if your child has a tracheostomy tube. You may need to suction food or liquid from the tube.
What are possible complications of aspiration in babies and children?
A major complication of aspiration is harm to the lungs. When food, drink, or stomach contents make its way into your child’s lungs, it can damage the tissues there. The damage can sometimes be severe. Aspiration also increases the risk of pneumonia. This is an infection of the lungs that causes fluid to build up in the lungs. Pneumonia needs to be treated with antibiotics. In some cases, it may cause death.
When food, drink, or stomach contents make its way into your child’s lungs, it can damage the tissues there. The damage can sometimes be severe. Aspiration also increases the risk of pneumonia. This is an infection of the lungs that causes fluid to build up in the lungs. Pneumonia needs to be treated with antibiotics. In some cases, it may cause death.
Other possible complications from aspiration include:
- Dehydration
- Malnutrition
- Weight loss
- Increased risk of other illness
When should I call my child's healthcare provider?
Let your child’s healthcare provider know right away if your child has any signs or symptoms of aspiration. It needs to be treated as soon as possible.
Key points about aspiration in babies and children
Aspiration is when something enters the airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen when a child has trouble swallowing normally. This is known as dysphagia.
Aspiration can happen when a child has trouble swallowing normally. This is known as dysphagia.
- Your child might have aspiration caused by problems with growth, development, or certain health conditions.
- Your child may have a signs such as breathing problems and a wet-sounding voice after meals.
- Some children with aspiration don’t have any signs or symptoms. This is known as silent aspiration.
- If your child has any symptoms of aspiration, he or she needs to be checked and treated right away.
- Aspiration may be treated by addressing the cause of dysphagia. It can also be managed with methods to help your child feed better.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.

- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
What is Aspiration? - Stanford Medicine Children's Health
What is aspiration?Aspiration occurs when food, liquid, or saliva that’s intended to be swallowed enters the trachea, or airway, and in some circumstances the lungs, instead of going down the esophagus to the stomach. It also can occur when a child inhales a foreign body or when gastric reflux comes up from the stomach and enters the airway.
It also can occur when a child inhales a foreign body or when gastric reflux comes up from the stomach and enters the airway.
The classic symptoms of aspiration are a cough, wet or congested breathing, and watery eyes after swallowing during drinking or eating, or when introducing solid foods (such as with baby-led weaning). In babies, aspiration might also produce a wet or gurgling noise during or after breastfeeding. Although aspiration can occur with any food or liquid, thin liquids (such as water, juice, formula, or milk) are most frequently aspirated.
What children are at risk for aspiration?Aspiration is more common in infancy, particularly in babies who are premature, but it can occur at any time in childhood. Premature babies are at a higher risk for aspiration because their ability to swallow is not completely developed, and they may not be able to produce a coordinated and timely swallow. An uncoordinated pattern during sucking, swallowing, and breathing may lead to mistimed swallowing, and liquid may enter the airway as a result. In older children, aspiration may be more likely to occur alongside neurological or neuromuscular disorders, such as during seizures or when anatomical (physical) or structural abnormalities are present. Often, aspiration has more than one cause.
An uncoordinated pattern during sucking, swallowing, and breathing may lead to mistimed swallowing, and liquid may enter the airway as a result. In older children, aspiration may be more likely to occur alongside neurological or neuromuscular disorders, such as during seizures or when anatomical (physical) or structural abnormalities are present. Often, aspiration has more than one cause.
Many young children outgrow swallowing problems that lead to aspiration. Our job is to keep them safe while they grow and to rule out chronic (ongoing) aspiration. This includes identifying any anatomical problems that may be causing aspiration and identifying silent aspiration (which occurs without any obvious signs or symptoms). When we catch aspiration early and treat it, your child will likely do very well.
How common is aspiration?The prevalence of aspiration is largely unknown, and pathological (disease related) aspiration is likely underdiagnosed. Everyone has the ability to aspirate a little bit, such as swallowing small amounts of saliva that enters the airway during sleep. Our bodies can handle minor aspiration events like this every now and then. At times, children may choke on water when they drink too fast or have a coughing or choking event when they eat a certain food that’s not appropriate for their age. But if your child aspirates regularly, such as with every few swallows of a drink, then there is likely an underlying cause that needs to be identified. We call this chronic, pathological (disease related) aspiration, and it is important to recognize and treat.
Everyone has the ability to aspirate a little bit, such as swallowing small amounts of saliva that enters the airway during sleep. Our bodies can handle minor aspiration events like this every now and then. At times, children may choke on water when they drink too fast or have a coughing or choking event when they eat a certain food that’s not appropriate for their age. But if your child aspirates regularly, such as with every few swallows of a drink, then there is likely an underlying cause that needs to be identified. We call this chronic, pathological (disease related) aspiration, and it is important to recognize and treat.
Swallowing is a complex series of movements and neurological responses, so children with any type of coordination problem with that process are at risk for the chance of the swallowing and breathing sequence to be mistimed. Children who have anatomical abnormalities in the throat or airway (such as a cleft in the larynx or a hole or fistula in the esophagus) may also be at a higher risk for aspiration, even if the motor function used to swallow is otherwise normal. Occasionally, part of a child’s airway does not function properly during swallowing, as can be seen with vocal cord motion disorders such as vocal cord paralysis.
Occasionally, part of a child’s airway does not function properly during swallowing, as can be seen with vocal cord motion disorders such as vocal cord paralysis.
In patients who have signs or symptoms of aspiration with each meal, such as coughing, congestion, or difficulty breathing during breastfeeding or bottle feeding, aspiration should be considered. On occasion, aspiration is silent, meaning it occurs without any cough response or abnormal reaction from your child. As a result, chronic aspiration may disguise itself as other conditions. For example, if your child has frequent or prolonged upper respiratory problems (such as repeated, long bouts of colds) or unexplained lung disease (such as recurring pneumonia) that cannot be attributed to another condition, he or she may have aspiration. Under these circumstances, your child may have symptoms that are similar to asthma but do not respond well to medication. If this sounds like your child, aspiration should be considered.
If your child frequently aspirates, he or she needs to be investigated by a pediatric otolaryngologist, otherwise known as an ear, nose, and throat (ENT) specialist. Ideally, your child should be seen at a center that specializes in airway and swallowing problems, such as our Aerodigestive and Airway Reconstruction Center or our Center for Pediatric Voice and Swallowing Disorders. That way, many experts from different specialties with specific training in feeding and swallowing disorders can weigh in, ensuring that your child gets an accurate diagnosis and comprehensive care.
How do you diagnose aspiration?Aspiration is not always obvious or easy to diagnose. That’s why we offer a full gamut of testing options to identify aspiration and, when possible, the exact cause. Because we see a large volume of children with aspiration, and we work with a team of multidisciplinary experts, we are able to identify even subtle signs of aspiration.
Generally, we start by observing your child in the clinic while he or she eats and drinks, looking for any signs or symptoms of aspiration. This is performed with a speech-language pathologist and otolaryngologist, who simultaneously observe feeding and swallowing and perform a physical exam. We also assess for anatomical differences that may lead to aspiration. To get more information, we frequently perform a swallow study. The studies complement each other and provide different information, so your child might require more than one:
- Videofluoroscopic swallow study (VFSS), also called a modified barium swallow (MBS) study. In this study, a moving x-ray shows the workings of your child’s mouth and throat muscles while he or she swallows a liquid dye called barium. We observe the path that the dye takes as it travels from the mouth into the esophagus (feeding tube to the stomach). This study is performed by a speech-language pathologist and a radiologist.

- Fiberoptic endoscopic evaluation of swallowing (FEES). In this study, which is a modified form of laryngoscopy, we place a flexible laryngoscope (a thin flexible camera) through the nose to visualize the throat, tongue, and airway as your child eats or drinks. We are able to view the larynx (voice box) to see if there are any visible anatomical defects, determine if it is functioning normally, and test for sensation. While your child eats and drinks, we watch to see if the liquid or food being swallowed follows the usual path to the esophagus. We can see if it deviates from the normal pathway and instead enters the airway above the vocal cords (penetration) or through the vocal cords (aspiration) into the trachea (windpipe) and lungs. It’s performed in our ear, nose, and throat clinic with a pediatric otolaryngologist and speech-language pathologist. Radiation is not required.
- Advanced swallowing diagnostics. If further evaluation is needed, your child can be seen in our advanced Motility Program, where multiple specialists will evaluate for aspiration.
 When we suspect a problem with the GI tract or lungs, we partner with pediatric gastroenterologists and/or pulmonologists within our Aerodigestive and Airway Reconstruction Center. The gastroenterologist assesses the GI tract for reflux, allergic problems, or motility issues; the pulmonologist views and evaluates the lungs for evidence of inflammation or infection; and the otolaryngologist evaluates the larynx (voice box) and central airway for the presence of inflammation and/or anatomical differences. This multidisciplinary approach ensures that your child only has to undergo one procedure, and receives anesthesia just once, to investigate a range of possible causes.
When we suspect a problem with the GI tract or lungs, we partner with pediatric gastroenterologists and/or pulmonologists within our Aerodigestive and Airway Reconstruction Center. The gastroenterologist assesses the GI tract for reflux, allergic problems, or motility issues; the pulmonologist views and evaluates the lungs for evidence of inflammation or infection; and the otolaryngologist evaluates the larynx (voice box) and central airway for the presence of inflammation and/or anatomical differences. This multidisciplinary approach ensures that your child only has to undergo one procedure, and receives anesthesia just once, to investigate a range of possible causes.
Our multidisciplinary Center for Pediatric Voice and Swallowing Disorders is one of the most advanced clinics in California, where otolaryngologists, speech-language pathologists, occupational therapists, and nutritionists provide care for simple to complex voice and swallowing disorders. Our speech-language pathologists (SLP) are all members of the American Speech-Language-Hearing Association (ASHA) and dedicated to the management of aspiration. We treat aspiration in a number of different ways, depending on your child’s needs. Feeding and/or swallowing therapy improves how your child eats and drinks, and it is often an important component of treatment. For example, we can improve an infant’s aspiration by changing breastfeeding positions, altering the flow rate of milk from a bottle, or thickening liquids. Sometimes we combine feeding therapy with surgical intervention if aspiration is caused by an anatomical abnormality.
Our speech-language pathologists (SLP) are all members of the American Speech-Language-Hearing Association (ASHA) and dedicated to the management of aspiration. We treat aspiration in a number of different ways, depending on your child’s needs. Feeding and/or swallowing therapy improves how your child eats and drinks, and it is often an important component of treatment. For example, we can improve an infant’s aspiration by changing breastfeeding positions, altering the flow rate of milk from a bottle, or thickening liquids. Sometimes we combine feeding therapy with surgical intervention if aspiration is caused by an anatomical abnormality.
If your child’s anatomy is not normal or is not functioning correctly, we may consider surgery. The majority of our surgeries are minimally invasive, and we are able to perform them through the mouth without making any incisions in the skin. For example, your child might have vocal cord immobility, where one of the vocal cords is not closing properly to protect the airway during swallowing, or a short laryngeal cleft, where the larynx does not separate completely from the pharynx or esophagus.
If your child has a more complex anatomical condition, such as a tracheoesophageal fistula, where there’s a hole between the trachea (tube to lungs) and esophagus (tube to stomach), or a severe or long laryngeal cleft, he or she might need a more extensive surgery. For rare and severe cases of aspiration, we have a multidisciplinary team that performs advanced operations. The team includes pediatric general surgeons, our airway reconstruction team, and our pediatric cardiothoracic surgeons. We are one of a few children’s hospitals in the Western United States to offer the entire spectrum of these complex operations and procedures.
For more information, listen to our PedsTalks discussion on aspiration or contact our Aerodigestive and Airway Reconstruction Center or our Center for Pediatric Voice and Swallowing Disorders.
Tuberculosis | MBUZ Clinical Diagnostic Center "Health"
Information / Information for patients / Tuberculosis
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis (synonyms: Koch's bacillus, Koch's bacillus).
Mycobacterium tuberculosis is a rod-shaped bacterium that possesses a capsule of fatty acid molecules whose structure and function are not fully understood. This shell allows mycobacteria to withstand very harsh environmental conditions and survive inside the cells of the human immune system (macrophages), where all other microbes die, being dissolved by enzymes. In addition, the capsule of mycobacteria is acid-resistant and does not pass common antibiotics. It can die only under prolonged exposure to direct sunlight, high temperatures and disinfectants.
Reservoir and exciter sources . The main source of the pathogen is a person with a pulmonary form of tuberculosis and secreting mycobacteria from the respiratory tract. Sick animals (cattle, pigs, etc.) and birds, as well as sick people excreting mycobacteria with urine and feces, are of secondary epidemiological significance.
The period of contagiousness of the source is equal to the entire period of the disease, which can last for years and even decades. The intensity of mycobacterium excretion by a sick person increases during the period of clinical exacerbations (more often in spring and autumn), animals - during lactation.
The intensity of mycobacterium excretion by a sick person increases during the period of clinical exacerbations (more often in spring and autumn), animals - during lactation.
Exciter Transfer Mechanism . The greatest epidemiological significance is the aspiration mechanism with airborne (sputum particles released into the air when coughing, sneezing, talking, etc.) and airborne (airborne dust contaminated with mycobacteria) transmission routes.
Infection from animals and birds usually occurs through food, when milk and dairy products, meat, and eggs serve as transmission factors. It is possible to transmit the pathogen through various household items and household items.
The natural susceptibility of people to the disease is high. Children under the age of 3 are most susceptible to the disease. The disease is promoted by various types of immunodeficiency, in particular HIV infection.
Main epidemiological signs . The disease is ubiquitous. The conditions favorable for the spread of tuberculosis are the low socio-economic standard of living, crowding at home and at work, the low level of sanitary culture, and the lack of affordable and qualified medical care.
The disease is ubiquitous. The conditions favorable for the spread of tuberculosis are the low socio-economic standard of living, crowding at home and at work, the low level of sanitary culture, and the lack of affordable and qualified medical care.
Children of the first two years of life, adolescents, elderly people over the age of 60 are more likely to get sick. There is no pronounced seasonality, but relapses and exacerbations are usually observed in early spring. Men get sick more often than women. The incidence of zoonotic tuberculosis prevails among rural residents, in whom it is often of a professional nature (livestock breeders, poultry workers, etc.).
Incubation period is 3-12 weeks . The main clinical signs: with primary tuberculosis in most patients (more than 90%), a specific focus of broncho-lobular pneumonia is formed, from which mycobacteria are excreted through the respiratory tract. With bronchoadenitis, this process is intensified in the case of caseous degeneration of the lymph nodes and a breakthrough of pathological material into the bronchi. With hematogenous disseminated forms, a number of clinical options are possible: with miliary tuberculosis, mycobacteria appear in sputum in the event of cavities; they are also intensively released during softening and cavernization of tuberculoma, i.e. with cavernous and fibrinous-cavernous forms. Isolation of mycobacteria also occurs in tuberculosis of the bronchi, trachea, larynx, silico-tuberculosis. In cases of extrapulmonary tuberculosis, mycobacteria are isolated in case of damage to the intestines, urogenital organs, eyes, oral mucosa, mammary glands, skin, and cold abscesses of tuberculosis etiology. With osteoarticular tuberculosis, mycobacteria are not released into the external environment.
With hematogenous disseminated forms, a number of clinical options are possible: with miliary tuberculosis, mycobacteria appear in sputum in the event of cavities; they are also intensively released during softening and cavernization of tuberculoma, i.e. with cavernous and fibrinous-cavernous forms. Isolation of mycobacteria also occurs in tuberculosis of the bronchi, trachea, larynx, silico-tuberculosis. In cases of extrapulmonary tuberculosis, mycobacteria are isolated in case of damage to the intestines, urogenital organs, eyes, oral mucosa, mammary glands, skin, and cold abscesses of tuberculosis etiology. With osteoarticular tuberculosis, mycobacteria are not released into the external environment.
The main symptoms of pulmonary tuberculosis include fever (in the form of prolonged subfebrile condition), cough (dry or with easily separated sputum), hemoptysis, shortness of breath, etc.
Laboratory diagnostics is based on bacteriological examination of various materials (sputum, pus, discharge from fistulas, urine, pleural and cerebrospinal fluid, washings from the bronchi or stomach, etc. ). Direct bacterioscopy of smears is used.
). Direct bacterioscopy of smears is used.
Preventive measures include nationwide and special medical.
The former include: improvement of living conditions, provision of isolated apartments for patients with tuberculosis, improvement of working conditions, improvement of populated areas, greening of cities, etc.
The latter are carried out by medical and preventive and sanitary and epidemiological institutions under the guidance and with the participation of specialized anti-tuberculosis research institutes (dispensaries) and include early detection and treatment of patients with initial forms of tuberculosis.
Mandatory examination of employees of children's institutions (nurseries, kindergartens, orphanages, orphanages, boarding schools, forest schools, children's health institutions), children's medical and preventive and sanatorium institutions (children's hospitals and sanatoriums, maternity hospitals) related to the service and nutrition of children: teachers and educators of schools, educational institutions for children and adolescents.
When applying for a job (hereinafter once a year), public catering workers and persons equated to them are subject to examination; employees of medical and preventive institutions for adults, sanatoriums, rest homes associated with food and service to patients and vacationers, dentists, public service workers (bath attendants, pedicurists, manicurists, shower workers, hairdressers and barbershop auxiliary staff, laundries, linen workers, maids , cleaners, dormitory workers, swimming pool workers, passenger transport workers, etc.). Patients with tuberculosis are not allowed to work in these institutions (they are sent to an anti-tuberculosis dispensary or tuberculosis rooms in a polyclinic).
Of great importance in the prevention of tuberculosis are the observance of the sanitary and anti-epidemic regime at industrial enterprises, in preschool institutions, schools, catering, trade, consumer services and sanitary - educational work among the population.
The planned mass specific immunization of the population with a live BCG vaccine, which children and adults not infected with mycobacteria are subject to, plays an important role in increasing the body's resistance to tuberculosis.
Scheduled mass immunization against tuberculosis of the child population is carried out in accordance with the national calendar of preventive vaccinations and the calendar of preventive vaccinations according to epidemic indications. Newborns receive the vaccine once on the 5-7th day after birth.
Revaccination against tuberculosis is carried out only for children with a negative Mantoux test at strictly decreed ages (7 and 14 years).
Preventive vaccinations against tuberculosis is carried out with medical immunobiological preparations registered in the territory of the Russian Federation in accordance with the instructions for their use.
An epidemiological examination is aimed at identifying persons infected with mycobacteria in the environment of the patient and the sanitary and epidemiological assessment of the outbreak, taking into account the intensity of the pathogen excreted by the patients, the presence of children and adolescents, housing conditions, compliance with sanitary and hygienic rules, the presence of animals suffering from tuberculosis in the outbreak. As a result of the survey, an action plan is formulated to improve the focus.
As a result of the survey, an action plan is formulated to improve the focus.
Patients with an active form of tuberculosis (isolation of the pathogen) are subject to hospitalization in specialized hospitals and aftercare in anti-tuberculosis sanatoriums.
The main means aimed at breaking the transmission mechanism of the pathogen is disinfection.
Disinfection in the outbreak is divided into current and final. Current disinfection in the focus is carried out in the environment of an infectious patient from the moment of its detection. The final disinfection is carried out after each departure of the patient from the outbreak for a long time, but at least once a year.
Nutrition after a stroke: how to create a menu
Nutrition after a stroke: how to make the right menu
If a person has retained the ability to swallow, as well as move and talk, then he should carefully follow all the instructions of the attending physician and follow a certain diet. This is necessary to reduce the risk of a second stroke. Be sure to consult with a specialist about what kind of food you should cook for your loved one. But there are also general recommendations that can be followed.
This is necessary to reduce the risk of a second stroke. Be sure to consult with a specialist about what kind of food you should cook for your loved one. But there are also general recommendations that can be followed.
Nutrition is an important part of your treatment program. It is in your power to make sure that each meal is not only enjoyable, but also a small step towards recovery.
Make sure the person's diet includes:
- High-fiber whole grain cereals. It will lower cholesterol levels and help cleanse the body of toxins.
— Vegetables and fruits. By collecting the whole rainbow of colors on one plate, you will be sure that you are providing your body with the necessary set of nutrients. Red apples or cabbages, orange oranges, carrots or pumpkins, yellow peppers, green cucumbers, asparagus or broccoli, blue plums, dark blue grapes, purple eggplants. They can be fresh, frozen or dried.
- Fish: salmon and herring.
- Protein found in lean meat and poultry, nuts, beans, peas.
Limit your intake of:
- Salt and salt-containing foods.
- Refined sugar. Excessive sugar intake is directly linked to hypertension, type 2 diabetes and obesity, and these are the risks of recurrent stroke.
- Prepared and processed canned foods that also contain too much sodium (salt) and unhealthy additives.
— Alcohol, of course.
- Saturated fats: egg yolks, butter and margarine, ice cream, palm and coconut oils, mayonnaise.
- Trans fats: fried foods, cookies, cakes.
Let's take a look at common nutritional problems after a stroke.
Lack of appetite. And, as a consequence, malnutrition. What to do? Cook what the person likes or give foods that cause appetite, with a pronounced pleasant smell. For example, citrus fruits or baked fish. Serve food attractively and choose food that looks appetizing.
Difficulty grasping objects. With partial immobility of the hands, “spill-proof” cups with comfortable handles and drinking straws will come to the rescue. Such little things can make the process of feeding easier and not laborious.
Such little things can make the process of feeding easier and not laborious.
Problems with swallowing. If a person has trouble swallowing or is at risk of developing aspiration pneumonia, food may be chopped. Aspiration pneumonia can occur in a person if he constantly lies down, eats in the supine position, often chokes and cannot cough. But remember that the blender replaces the process of chewing food, and this is not always a good thing. When a person chews, saliva and gastric juice are produced.
It happens that people who have had a stroke complain about digestion. Do not forget that any food accumulates in the intestines, even the lightest. Your loved one is using less energy now, so there is no need to overfeed. You also need to make sure that the chair was regular.
Remember that simple, healthy eating habits can help reduce the three risk factors for stroke: high cholesterol, high blood pressure, and being overweight. Introduce them gradually into your life and the lives of your loved ones.