My baby is in pain after feeding
Why Is Baby Crying After Feeding?
The question of “why does my baby cry after feeding” is a question that can typically drive mothers and parents crazy.
Oftentimes, it can be hard to know why your baby is crying after feedings. Not knowing how to identify the problem and not having a solution can have a significant effect on the physical and mental health of both your baby and the entire family. This can include increased stress, lower quality sleep, and the physical health of your baby. However, if you identify the cause and solve the problem, you will be able to significantly improve the parenting and breastfeeding experience for you and your child.
That’s why we decided to write an article on this topic – Why does my baby cry after feeding? This is an important topic and should be known by all mothers so that you can get the best results when feeding your baby.
This article will cover the following topics:
- Why Babies Cry After Feeding
- Should You Breastfeed Every Time Your Baby Cries?
- How Do I Comfort A Newborn?
Without further ado, let’s get into it.
Why Your Baby Cries After Feeding
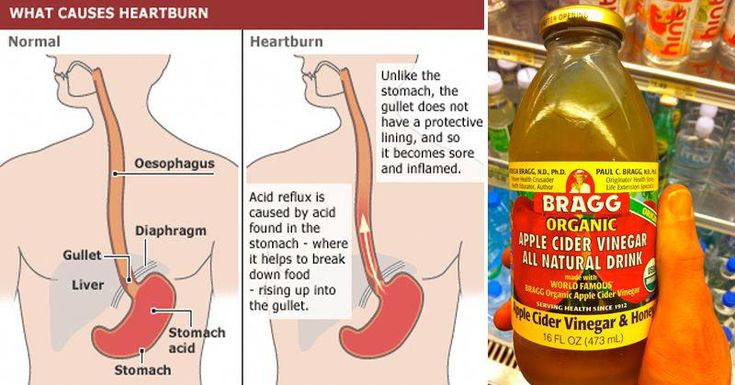
Acid Reflux
The first major reason babies cry after feeding is known as acid reflux. Acid reflux happens when the content in the stomach gets pushed back into the esophagus.
It’s estimated that more than half of infants experience acid reflux at some point. The condition usually peaks at 4 months and goes away on its own between 12 and 18 months of age.
Some symptoms of acid reflux include:
- Spitting up and/or Vomiting
- Refusal to eat and difficulty eating or swallowing
- Irritability during feeding
- Wet burp / hiccups
- Failure to gain weight
- Abnormal arching
- Frequent coughing
- Gagging or choking
- Chest pain or heartburn
- Disturbed sleep
If acid reflux symptoms persist past 24 months, it may be a sign of gastroesophageal reflux disease (GERD) when combined with weight gain.
Food Sensitivity / Allergies
In addition to acid reflux, some breastfed babies may be allergic to certain food particles that their mothers are eating. According to the Academy of Breastfeeding Medicine, some of the most common foods that lead to food sensitivities and allergies in babies is cow’s milk protein in the mother’s milk, egg, corn, and soy.
Some symptoms of food sensitivities in your baby include the following:
- Extreme irritability after feedings
- Bloody stools (poop)
If your baby has the following symptoms, you should speak with your healthcare provider about getting them tested for allergies.
Additionally, you can also follow a restricted diet that removes common allergen foods such as eggs, dairy, corn, caffeine, and seeded fruit. Be sure to speak with your doctor before changing your diet significantly.
Start by eliminating one food at a time and analyze the effects of removing certain foods on your baby’s behavior. That way you can really see what effect each individual food has so you can isolate the diet problem.
That way you can really see what effect each individual food has so you can isolate the diet problem.
Gas
The next reason your baby may be crying is gas. Gas can also be known as a buildup of air swallowed while eating. In particular, bottle feeding can lead to your baby swallowing a lot of air during feeding. This will cause gas to be trapped in the stomach and will potentially lead to baby hiccups and discomfort for the baby.
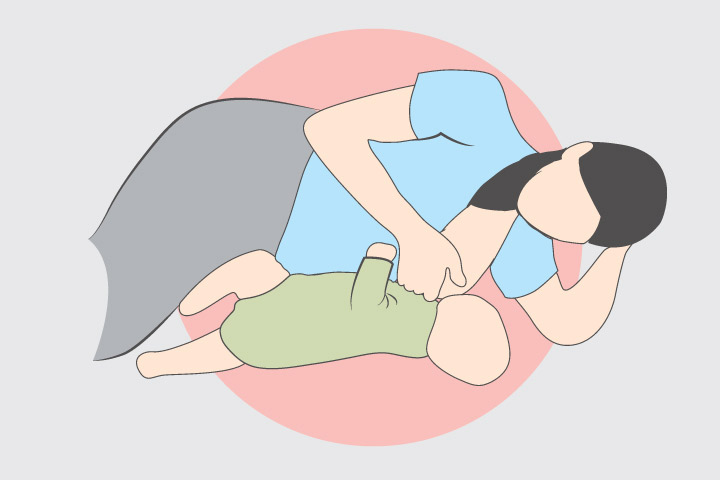
In order to help prevent gassing in your baby, you may try to change or improve your breastfeeding position. Try to keep your baby upright after feeding. Also, allow your baby to burp gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out of the body. Burping your baby can significantly reduce the chances of gassiness.
Formula
Not every baby gets fed directly from breast milk. For formula-fed babies, a change or switch of the formula you use may be your solution to your baby crying after feeding.
Every formula brand may affect each child differently, so trying a different formula for your baby may be a good solution to solving your babies crying problem. It is important to talk to your own baby’s pediatrician about whether some other formula options can be better for your child.
If you see no change or improvement by switching your baby’s formula, it is unlikely to help for any other brands.
Colic
Colic is also another reason why babies cry after feeding. Essentially, colic means persistent and excessive crying for a baby under 3 months old. More specifically, your baby is doing the following:
- Is crying a lot, for at least three hours a day
- The baby is crying at least three days per week or more
- Is under 3 months old
If all 3 of those boxes are checked, then your baby is likely colic.
Should You Breastfeed Every Time Your Baby Cries?
This is a question that is very popular among moms in regards to their baby and crying.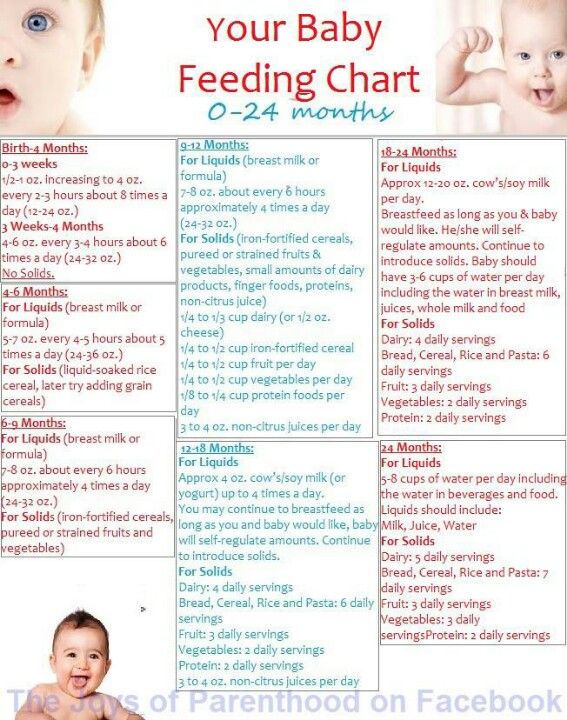 For that reason, we wanted to address this directly because it seems to be a topic that is debated out there.
For that reason, we wanted to address this directly because it seems to be a topic that is debated out there.
In short, no. You do not want to breastfeed your baby every time he or she cries. Contrary to some beliefs out there, some babies cry because of a bloated stomach, gas, or some of the other reasons we talked about already in this article.
Ultimately, the best solution is to let your baby decide when she’s had enough milk. When your baby has had enough milk, it will give you signs to let you know it will be done feeding. Including stopping feeding or turning your head away.
How Do I Comfort a Crying Newborn?
Now that you know that you shouldn’t breastfeed every time your baby cries after feeding, I’m sure you’re also wondering how to comfort your crying newborn. With that being said, there are multiple ways to comfort a crying newborn when he or she cries.
Some of these ways include:
- Offer a pacifier for sucking – this can help your baby relieve stress without crying.
- Try gently rocking your baby – this can calm your baby down and relax them.
- Quietly singing to your baby – like rocking, singing may calm your baby and get them to stop crying. You can also put on a rhythmic song or music to have the same effect.
- Cuddle and hold your baby close – Touching, holding, and cuddling your baby makes your baby feel safe and secure. You can also put your baby in a blanket to get a similar effect.
- Try walking or taking your child out for a walk – this can result in a positive change in your child’s mood.
These are some of the main ways that you can comfort your baby when crying. As mentioned above, breastfeeding is not always the answer when your baby is crying. If your baby is crying and it has had enough feeding, try the things that we’ve listed above and see if it helps and improves your baby’s mood.
Why does My Baby Cry After Feeding – Key TakeawaysIf you’re thinking, “Why does my baby cry after feeding?” hopefully this article is helpful for you. Knowing why your baby cries after feeding is extremely important for the health of your child. Some reasons why your fed baby cries after feeding can include acid reflux, food sensitivity/allergy, gas, formula, or colic.
Knowing why your baby cries after feeding is extremely important for the health of your child. Some reasons why your fed baby cries after feeding can include acid reflux, food sensitivity/allergy, gas, formula, or colic.
You should not breastfeed every time your baby cries. Instead, it’s best to let the baby tell you when it’s had enough flow of milk.
It’s also important to comfort your crying newborn when he/she cries.
Knowing how to answer the question “why does my baby cry after feeding” can help your breastfeeding experience and the health of your baby. Whether it is with bottle feeding, direct breastfed babies, your baby will be better off if you understand these basics.
If you’re looking to get the best high-quality breast pump, you can order our breast pump here. We offer a wide range of pumps with a ton of different insurances. Some insurances we cover include UPMC, Tricare, Aetna, and many others.
Baby Cries After Feeding: What Should I Do?
Medically reviewed by Karen Gill, M. D. — By Chaunie Brusie on October 3, 2018
D. — By Chaunie Brusie on October 3, 2018
My daughter, the “crier”
My second daughter was what my oldest fondly referred to as a “crier.” Or, in other words, she cried. A lot. The crying with my baby girl seemed to intensify after every single feeding and particularly at night.
It was those hellish hours between darkness and dawn when my husband and I would take turns walking around the house with her in our arms, praying and, mostly in my case, sobbing because we couldn’t console our baby.
I didn’t know it then in my sleep-deprived state, but my daughter’s crying after feedings wasn’t that uncommon. In combination with her frequent spitting up, it was pretty much a classic textbook case of colic.
Colic
Colic, in technical terms, simply means a “crying, fussy baby that doctors can’t figure out.”
OK, so that’s not really the definition, but in essence, that’s what it boils down to. The British Medical Journal (BMJ) lists one criterion for colic: A baby that cries for at least three hours a day, three or more days a week, and is under 3 months old. Check, check, and check.
Check, check, and check.
There isn’t one single known cause of colic. Even the actual clinical incidence of colic, estimated by BMJ to be around 20 percent of all babies, can be tricky.
Acid reflux
One of those causes of crying after feeding and spitting up in babies is actually acid reflux. This condition is known as gastroesophageal reflux disease (GERD) if it also causes significant symptoms such as poor weight gain.
When my “crier” daughter was 5, she frequently complained of her stomach hurting and as a result, had to undergo a series of testing with a gastroenterologist, a doctor that specializes in the GI system.
At our first appointment, the very first question he asked me was if she had colic as a baby and if she spit up a lot, to both of which I practically shouted, “Yes! How did you know?!”
He explained that acid reflux or GERD can manifest as symptoms similar to colic in babies, stomach pain in school-aged children, and later as actual heartburn pain in adolescents.
While many infants spit up, fewer have actual GERD, which can be caused by an underdeveloped flap between the esophagus and stomach or a higher-than-normal production of stomach acid.
In most cases, a diagnosis of infant reflux is simply based on your baby’s symptoms. If your doctor suspects a severe case however, there are several different tests that actually diagnose infant reflux.
Testing can involve taking a biopsy of your baby’s intestine or using a special type of X-ray to visualize any affected areas of obstruction.
Food sensitivities and allergies
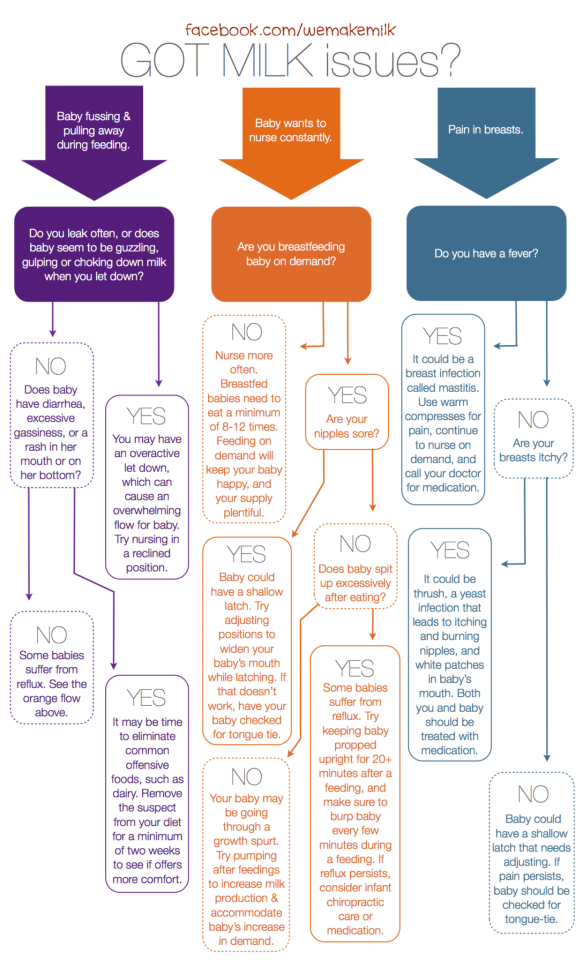
Some babies, especially breastfed babies, may be allergic to certain food particles that their mothers are eating.
The Academy of Breastfeeding Medicine notes that the most common offender is cow’s milk protein in the mother’s milk, but even a true allergy is very rare. Only about 0.5 to 1 percent of exclusively breastfed babies are thought to be allergic to cow’s milk protein.
The other most common culprits, according to the ABM, are egg, corn, and soy, in that order.
If your baby is displaying symptoms of extreme irritability after feedings and has other symptoms, such as bloody stools (poop), you should speak with your healthcare provider about getting them tested for allergies.
Aside from a true allergy, there’s also been some evidence that following a low allergen diet while breastfeeding (essentially avoiding those top allergy foods, such as dairy, eggs, and corn) may be beneficial for infants with colic.
Strict elimination diets can have their own risks, so speak with your doctor before significantly changing your diet.
In our situation, I found that dairy, caffeine, and certain seeded fruit exacerbated my daughter’s crying and spitting up. By eliminating those foods and substances from my diet, I was able to help lessen her discomfort.
If you have a baby with colic, you might want to try anything at all to help ease your baby’s crying. If you’re curious to see if your diet has any effect, you can start by logging your food in a food journal and writing down your baby’s reactions after each meal.
Next, you can eliminate one food at a time and see if reducing your intake of certain foods seems to make a difference in your baby’s behavior. If you hit on one you feel helps your baby to cry less, this does not mean they will not be able to eat that food in the future.
Just be sure to keep in mind that a true allergy is rare. Also, be sure to monitor for any additional symptoms, such as blood in your baby’s poop.
Gas
If your baby is crying a lot after every feeding, it may simply be a buildup of air swallowed while eating. It’s thought that bottle-fed babes in particular may be more prone to swallowing a lot of air during a feeding. This can trap gas in their stomachs and be uncomfortable.
In general, breastfed babies swallow less air while eating simply due to the way they eat. But every baby is different and even breastfed babies may need to be burped after a feeding.
Trying keeping your baby upright after a feeding and burping gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out. Also check out this illustrated guide to burping a sleeping baby.
Also check out this illustrated guide to burping a sleeping baby.
Formula
If your baby is formula-fed, swapping out the formula you use may be a simple solution to a crying baby after feedings. Every formula is a little bit different and certain brands make formulas for more sensitive baby tummies.
If you decide to try this, talk to your baby’s pediatrician about whether an elemental formula would be a good choice to try for a week. If you try one different brand and you see no change in your baby’s fussiness, continuing to try different brands is unlikely to help.
Takeaway
Colic, along with a few other common conditions, might be the culprit if you too have a “crier” on your hands.
If your baby doesn’t find relief after dietary changes or additional burping, then make an appointment to see their doctor.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on October 3, 2018
- Parenthood
- Baby
- 06 Months
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ABM clinical protocol #24: Allergic proctocolitis in the exclusively breastfed infant. (2011). DOI:
10.1089/bfm.2011.9977 - Harrel MC, et al. (2015). Is there a correlation between maternal diet in breastfeeding mothers and infantile colic? DOI:
10.1097/01.EBP.0000541032.94135.ca - Mayo Clinic Staff. (2018). Infant reflux.
mayoclinic. org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412
org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412 - Rosen LD, et al. (2007). Complementary, holistic, and integrative medicine.
pedsinreview.aappublications.org/content/28/10/381 - Saavedra MA, et al. (2003). Infantile colic incidence and associated risk factors: A cohort study. .
ncbi.nlm.nih.gov/pubmed/14502331 - Sung V, et al. (2014). Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. DOI:
10.1136/bmj.g2107 - Symptoms & causes of GER and GERD in infants. (2015).
niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-infants/symptoms-causes
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Solving nine breastfeeding problems in the first month
Expert advice on solving major breastfeeding problems in the first month.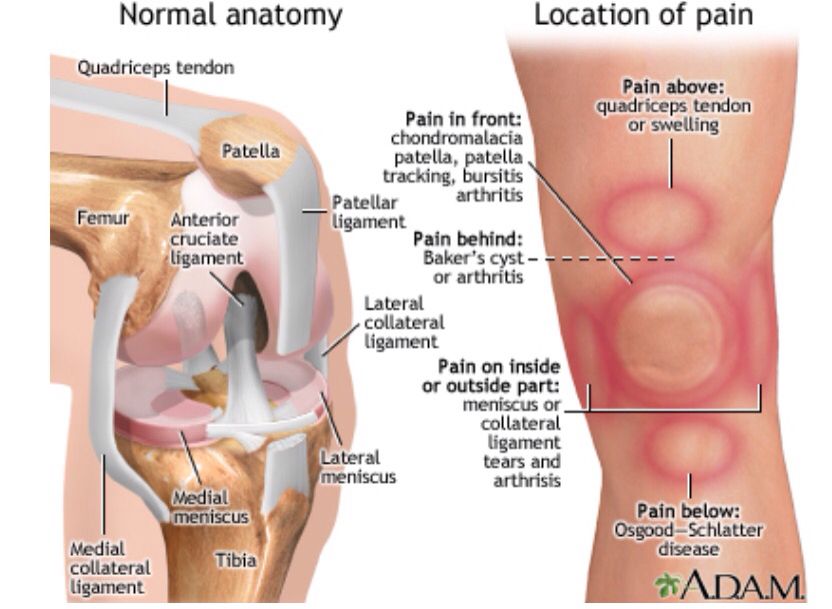
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding problems that mothers often face from the end of the first week to the end of the first month after giving birth.
Problem #1. A painful lump appeared in the breast
Lumps and lumps in the breast of a nursing woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1-3
- Massage the inflamed area, especially while breastfeeding or expressing, to clear the blockage.
- Gently apply warm flannel to your breast or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you.
- Try ultrasound therapy.
 If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist. - Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache) or if you think the lump is not related to breastfeeding .
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria entering the breast through cracked and damaged nipples,
- incorrect attachment of the child to the breast,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.
Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk.
- Give the child the inflamed breast first. This way the child can empty it completely.
 If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one. - Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before feeding or pumping.
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water.
 Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it.
Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it. - Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding. When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
Problem #4. How can I increase breast milk production?
It's easy to question whether you're making enough breast milk, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are worried about weight gain or fluid loss. Continue breastfeeding your baby. This will help naturally increase breast milk production.
- Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs.
- Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).
- Use towel or pad to soak up excess milk, or place the Milk Collection Pad** on the other breast while you breastfeed first.
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.

- Contact a lactation consultant or health care professional who will monitor you and suggest single-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply.
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby has a preference for one breast, or that one breast produces more milk than the other, and as a result the breasts have taken on different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
Solutions
- Offer less demanded breasts first during feeding as babies usually suckle more vigorously at the beginning of a feed.
- Use the breast pump to increase breast milk production in the smaller breast.

- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid clogged ducts and mastitis.
- See a doctor. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Problem #7. A blister has appeared on the nipple
With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. 7
Solutions
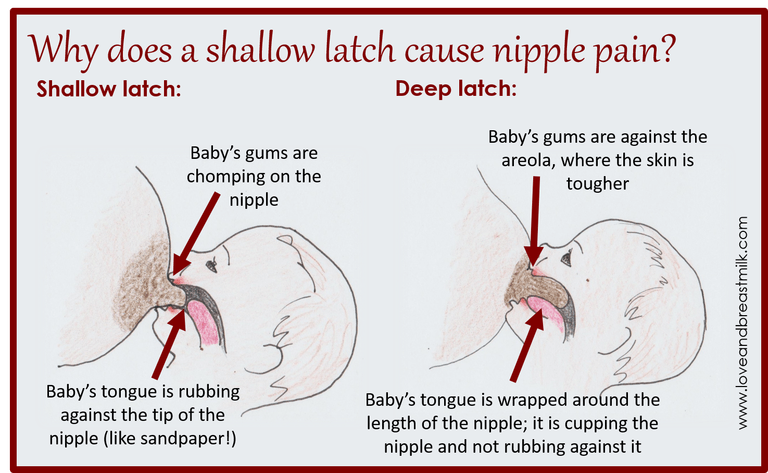
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medicine you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area.

- Lubricate inflammation with pure lanolin.
- Use Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation. Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel.
- Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Problem #8. Painful white spot on nipple
When the orifice of the milk duct becomes blocked with milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping.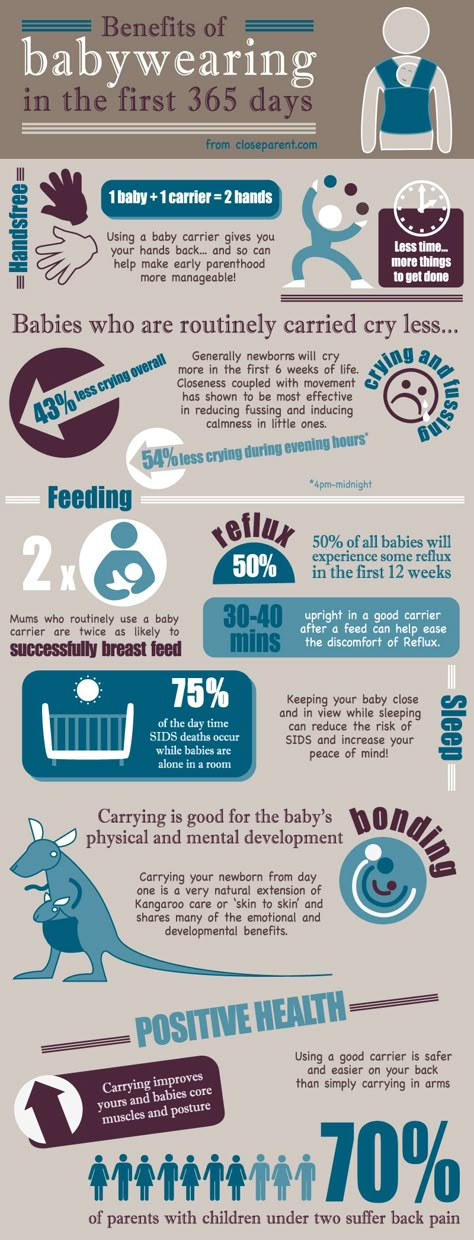 Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge. Try to squeeze it out very gently with clean nails.
- Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way.
- Apply hot wet flannel to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Manually express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.

- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.
Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. 2.7
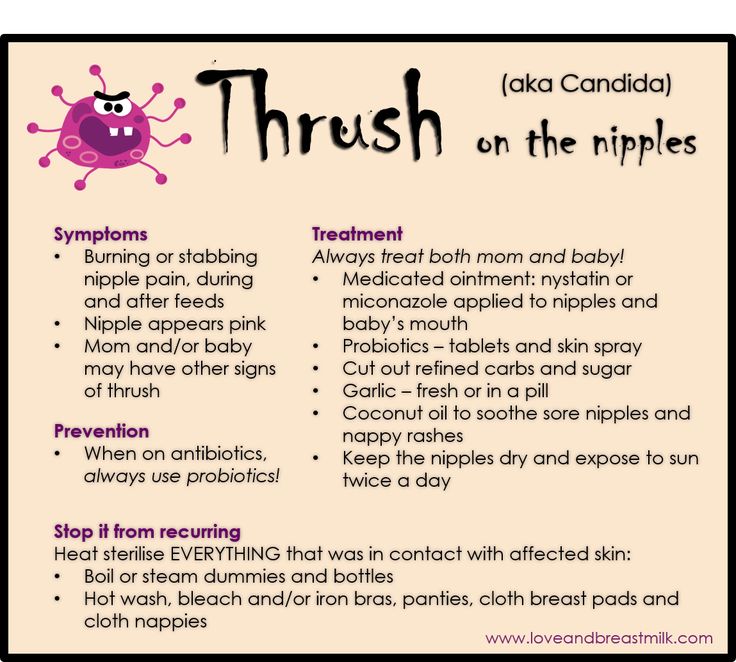
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- pain in nipples aggravated by contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch,
- stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink, darkening, dryness or peeling),
- white rash on chest or areola.
Also check if your child has the following symptoms and signs:
- hard white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis.
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.

- Let the nipples dry after feeding, as all infections love a warm and humid environment.
- See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Related materials. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
1 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". G Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - - Amir L., "Breastfeeding: problems of 'supply'. Aust fam physis. 2006;35(9):686.
6 Trimeloni L, Spencer J. Diagnosis and management of breast milk oversupply Journal Am Board Fam Med . 2016;29(1):139-142. - Trimeloni L., Spencer J., "Diagnosis and correction of excess breast milk production.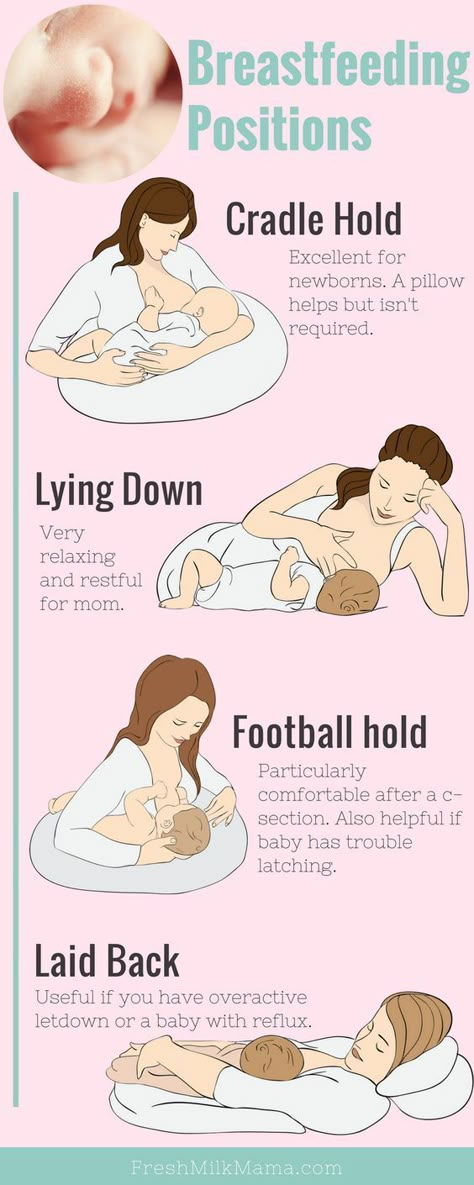 " Journal Am Bord Fam Med. 2016;29(1):139-142.
" Journal Am Bord Fam Med. 2016;29(1):139-142.
7 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol# 26: Persistent pain with breastfeeding. Breastfeed Med. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
8 Australian Breastfeeding Association [Internet] White spot nipple; March 2015 [Accessed 02/08/2018]. - Australian Breastfeeding Association [Internet], "White spots on the nipples", March 2015 [visited 02/08/2018].
Read instructions before use. Consult a specialist about possible contraindications.
* RU № ФСЗ 2010/06525 dated 03/17/2021
** RU ФСЗ 2010/07352 dated 07/19/10
Why does the chest hurt after feeding
Breastfeeding is very important, because through mother's milk the baby receives all the substances necessary for its growth and development.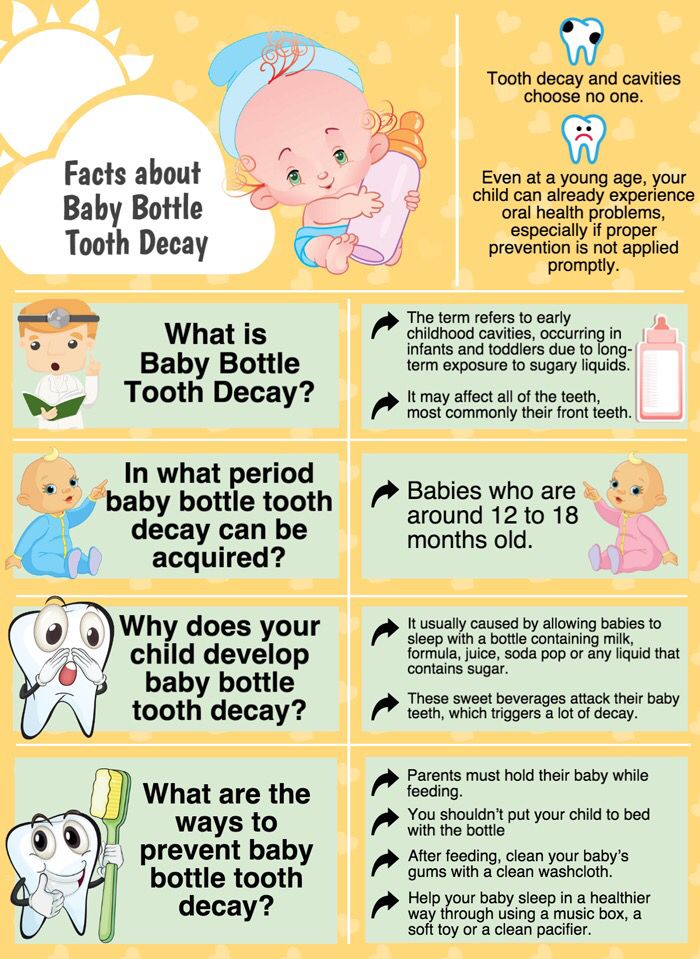 In addition, this is one of the most beautiful natural processes, because during it the mother and newborn are able to feel the maximum closeness and strengthen the emotional connection with each other. However, very often young mothers are faced with the problem of breast pain after feeding. This can be a wake-up call, so you should figure out what exactly can cause such discomfort and how to deal with it.
In addition, this is one of the most beautiful natural processes, because during it the mother and newborn are able to feel the maximum closeness and strengthen the emotional connection with each other. However, very often young mothers are faced with the problem of breast pain after feeding. This can be a wake-up call, so you should figure out what exactly can cause such discomfort and how to deal with it.
One of the reasons may be cracked nipples. They are specific linear lesions running from the center of the nipple to the areola. Cracks can be single or numerous, on the nipples of both breasts or only one. Such injuries can bring pain to a woman not only during breastfeeding, but even with simple tactile contact. Accordingly, the deeper the crack is, the more discomfort it will bring. There are situations when ichor, a clear liquid, is released from the cracks. And in case of infection or certain complications, pus can be released from the wounds.
Prerequisites for the appearance of cracks can be:
If the cracks don't go away, but rather get deeper and more painful, then going to the doctor should be high on your to-do list.
Pain during breastfeeding may occur in the first time after childbirth, after the start of lactation. So in the mammary glands of a young mother there is a strong influx of milk, discomfort in the chest may appear in the form of tingling or compression. The process of “making” milk by the body is tuned and regulated during the first few months. Accordingly, a woman also gets used to new sensations in her body and pain decreases or disappears altogether.
Breast pain in case of shv: when to see a doctor and disorders in the body of a woman. The most common pathology is lactostasis - stagnation of milk in the ducts of the mammary glands. It occurs when the glands produce more milk than the baby requires; when the breasts are damaged when expressing milk or when carelessly squeezing during feeding; when mom suddenly interrupts Guards.
Women who experience this describe the pain of lactostasis as a kind of tingling or shooting in one or both nipples. The nipples themselves can also change color: become pale or, conversely, turn blue due to the outflow of blood. If at least a few symptoms similar to this are noticed, you should definitely contact a mammologist.
Chest pain, accompanied by a burning sensation or a whitish coating, may indicate that a woman has thrush. Thrush harms both mother and baby, because the body of the newborn is not yet ready to fight such an infection. Thrush can cause inflammation of the oral cavity in a child, which, in turn, can have complications. In such situations, you simply cannot do without the help of a doctor. The pediatrician will be able to prescribe effective antifungal drugs to the child, which will help prevent the spread of the disease and its recurrence in the future.
When the pain in the nipples stops when breastfeeding
Ideally, breastfeeding should be enjoyable for both parties. Here are some tips to improve this process and minimize the pain of feeding your baby:
Here are some tips to improve this process and minimize the pain of feeding your baby:
- Change your baby's feeding technique.
- Alternate breasts for feeding.
- Express milk carefully, either manually or with a breast pump.
- Wear comfortable underwear.
- Have regular breast hygiene, but not too often.
- Avoid stress and hypothermia.
- Conduct preventive examinations at the gynecologist and mammologist.
To prevent blockages in the mammary glands, experts recommend doing the following:
- When breastfeeding or expressing milk, massage the area around the nipple with light, gentle movements.
- Before eating, a newborn should take a warm shower or apply a warm flannel to the chest.
- Continue to breastfeed as usual, do not suddenly stop this process.
- After breastfeeding with inflamed breasts, it is necessary to completely express milk from it so that blockages do not form and the patency of the milk ducts can be restored.

- Perform ultrasound therapy, this will help restore the process of milk flow.
I Love Mommy Offer
We won't be able to offer you anything that will relieve breast pain while feeding your baby. However, we can create for you the ideal conditions for online shopping, which will be a great way to recover from a difficult period and forget about any discomfort!
On our website there are many products that will make your life and the life of your baby more comfortable and cozy. I Love Mommy has been collaborating with such brands as Carter`s, Oshkosh Bgosh, H&M, George, Next, Marks&Spencer, Adidas, Barbie, Andriana Fashion Collection, Battat and several others for many years. And this means that there is no doubt about the quality and safety of our products!
We sincerely care about each of our adult and small clients, therefore we offer convenient payment methods and delivery of goods, pleasant discount offers, gift cards, as well as qualified service assistance online and by phone.