Baby aspirating while bottle feeding
Aspiration in Babies and Children
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is aspiration in babies and children?
Aspiration is when something enters the airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen when a person has trouble swallowing normally. This is known as dysphagia. It can also happen if a child has gastroesophageal reflux disease (GERD). This is when the contents of the stomach come back up into the throat.
When your child swallows food, it passes from the mouth down into the throat. This is called the pharynx. From there, the food moves down through a long tube (esophagus) and into the stomach. This journey is made possible by a series of actions from the muscles in these areas. If your child has dysphagia, the muscles don’t work normally. They cause problems with the swallowing process.
The pharynx is also part of the system that brings air into the lungs. When a person breathes, air enters the mouth and moves into the pharynx. The air then goes down into the main airway (trachea) and into the lungs. A flap of tissue called the epiglottis sits over the top of the trachea. This flap blocks food and drink from going down into the trachea when your child swallows. But in some cases, food or drink can enter the trachea. It may go down as your child swallows. Or it may come back up from the stomach. A child with dysphagia is much more likely to aspirate. A child with a developmental or health problem is more likely to have dysphagia.
Aspiration can happen during a feeding or meal. And it can happen after a feeding or meal. This is common in babies and children with certain health conditions. Aspiration can also happen at any time when your child swallows saliva.
If your child aspirates a small amount of material, it may not cause much harm. This can happen in children who don’t have a health problem. It can happen when eating, sleeping, or talking. But aspiration that happens often or in a large amount can be serious.
What causes aspiration in babies and children?
Aspiration is often caused by dysphagia. This is when the muscles don’t work normally in the throat and lead to swallowing problems. Different medical conditions can lead to this, such as:
- Abnormal anatomy, such as a cleft palate or a problem in the esophagus
- Delayed growth, from premature birth or a condition such as Down syndrome
- Brain damage or other problems, such as from cerebral palsy or infection
- Problems with the cranial nerves that control the muscles of swallowing
- Neuromuscular disease, such as spinal muscular atrophy
- Medical procedures, such as a nasogastric tube or a tracheostomy
Gastroesophageal reflux disease (GERD) can also cause aspiration. This is when the contents of the stomach come back up into the throat.
This is when the contents of the stomach come back up into the throat.
What are the symptoms of aspiration in babies and children?
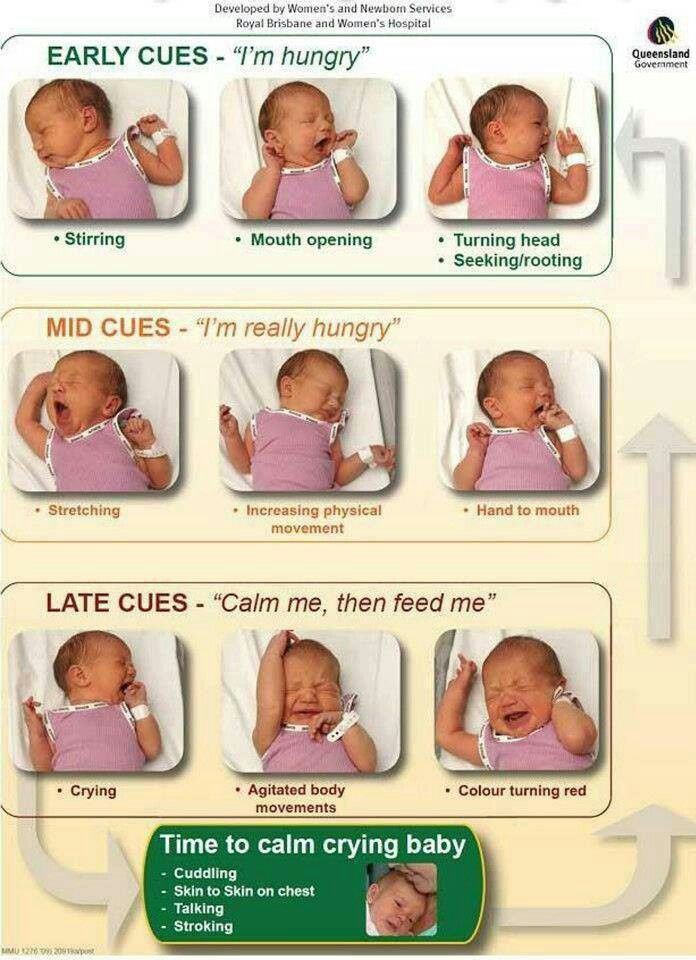
Aspiration can cause signs and symptoms in a baby such as:
- Weak sucking
- Choking or coughing while feeding
- Other signs of feeding trouble, like a red face, watery eyes, or facial grimaces
- Stopping breathing while feeding
- Faster breathing while feeding
- Voice or breathing that sounds wet after feeding
- Slight fever after feedings
- Wheezing and other breathing problems
- Repeated lung or airway infections
And aspiration can cause signs and symptoms in an older child such as:
- Choking or coughing while eating
- Voice that sounds wet after eating
- Slight fever after meals
- Complaints of food feeling stuck or coming back up
- Wheezing and other breathing problems
- Repeated lung or airway infections
Signs and symptoms can happen right after eating. Or they may happen over time. Your child may not have all of these signs and symptoms. The signs and symptoms may depend on the age of your child, and how often and how much your child aspirates.
Or they may happen over time. Your child may not have all of these signs and symptoms. The signs and symptoms may depend on the age of your child, and how often and how much your child aspirates.
Some children who aspirate do not have any signs or symptoms. This is called silent aspiration.
How is aspiration in babies and children diagnosed?
Your child will need to be checked for aspiration if he or she has:
- Any signs or symptoms of aspiration
- Health problem that can cause trouble swallowing
- GERD
The healthcare provider will ask about your child’s medical history and symptoms. This may be done by a speech-language pathologist (SLP). The SLP may ask about what foods or drink cause problems, and when your child’s symptoms happen. He or she may want to watch your child during a feeding.
Your child may also need tests. These can check for problems and show if food and fluid is going into your child’s lungs. The tests may include:
The tests may include:
- Chest X-ray or CT scan
- Modified barium swallow test (MBS)
- Fiber optic endoscopic evaluation of swallowing (FEES)
How is aspiration in babies and children treated?
Treatment for aspiration may vary depending on the cause and severity. Treatments for your child may include:
- Making changes in position and posture during meals
- Changing the thickness of liquids
- Changing the types of foods in your child’s diet
- Doing exercises to help with swallowing (for an older child)
- Medicines for GERD
- Medicines or Botox injection for children who make excess saliva
- Surgery to reduce reflux
- Surgery to correct a problem such as a cleft palate
If your child still has a high risk of aspiration despite these methods, he or she may need a special tube to help with eating for a while. The feeding tube will help your child get good nutrition until his or her risk of aspiration improves. Your child will not eat or drink normally until the tube is removed. A thin tube may be put through the nose down into the stomach. This is called a nasogastric tube. This may be used for a short time while other treatment is considered. Or a tube may be put directly into your child’s stomach during a surgery. This is called a gastrostomy tube.
The feeding tube will help your child get good nutrition until his or her risk of aspiration improves. Your child will not eat or drink normally until the tube is removed. A thin tube may be put through the nose down into the stomach. This is called a nasogastric tube. This may be used for a short time while other treatment is considered. Or a tube may be put directly into your child’s stomach during a surgery. This is called a gastrostomy tube.
In some children, aspiration lessens over time. In other cases, a child may need more treatment to address the cause. Your child’s healthcare providers will carefully watch your child so that he or she can return to normal eating as soon as possible.
Talk with your child’s healthcare provider if your child has a tracheostomy tube. You may need to suction food or liquid from the tube.
What are possible complications of aspiration in babies and children?
A major complication of aspiration is harm to the lungs.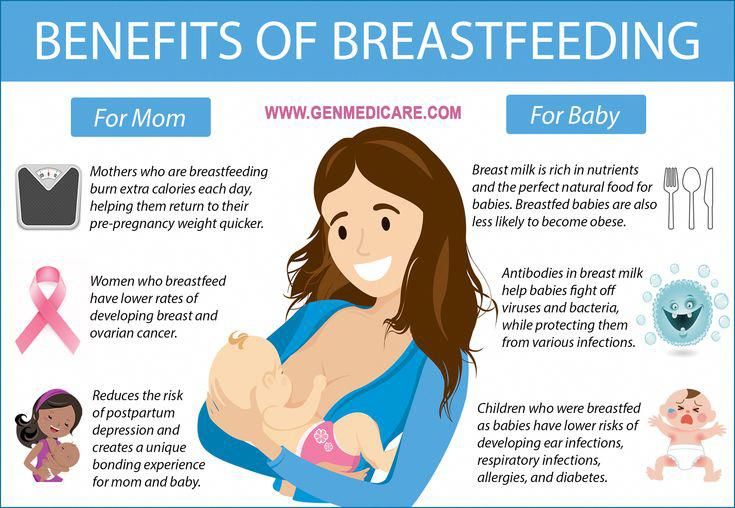 When food, drink, or stomach contents make its way into your child’s lungs, it can damage the tissues there. The damage can sometimes be severe. Aspiration also increases the risk of pneumonia. This is an infection of the lungs that causes fluid to build up in the lungs. Pneumonia needs to be treated with antibiotics. In some cases, it may cause death.
When food, drink, or stomach contents make its way into your child’s lungs, it can damage the tissues there. The damage can sometimes be severe. Aspiration also increases the risk of pneumonia. This is an infection of the lungs that causes fluid to build up in the lungs. Pneumonia needs to be treated with antibiotics. In some cases, it may cause death.
Other possible complications from aspiration include:
- Dehydration
- Malnutrition
- Weight loss
- Increased risk of other illness
When should I call my child's healthcare provider?
Let your child’s healthcare provider know right away if your child has any signs or symptoms of aspiration. It needs to be treated as soon as possible.
Key points about aspiration in babies and children
Aspiration is when something enters the airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen when a child has trouble swallowing normally. This is known as dysphagia.
Aspiration can happen when a child has trouble swallowing normally. This is known as dysphagia.
- Your child might have aspiration caused by problems with growth, development, or certain health conditions.
- Your child may have a signs such as breathing problems and a wet-sounding voice after meals.
- Some children with aspiration don’t have any signs or symptoms. This is known as silent aspiration.
- If your child has any symptoms of aspiration, he or she needs to be checked and treated right away.
- Aspiration may be treated by addressing the cause of dysphagia. It can also be managed with methods to help your child feed better.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
What is Aspiration? - Stanford Medicine Children's Health
What is aspiration?Aspiration occurs when food, liquid, or saliva that’s intended to be swallowed enters the trachea, or airway, and in some circumstances the lungs, instead of going down the esophagus to the stomach. It also can occur when a child inhales a foreign body or when gastric reflux comes up from the stomach and enters the airway.
It also can occur when a child inhales a foreign body or when gastric reflux comes up from the stomach and enters the airway.
The classic symptoms of aspiration are a cough, wet or congested breathing, and watery eyes after swallowing during drinking or eating, or when introducing solid foods (such as with baby-led weaning). In babies, aspiration might also produce a wet or gurgling noise during or after breastfeeding. Although aspiration can occur with any food or liquid, thin liquids (such as water, juice, formula, or milk) are most frequently aspirated.
What children are at risk for aspiration?Aspiration is more common in infancy, particularly in babies who are premature, but it can occur at any time in childhood. Premature babies are at a higher risk for aspiration because their ability to swallow is not completely developed, and they may not be able to produce a coordinated and timely swallow. An uncoordinated pattern during sucking, swallowing, and breathing may lead to mistimed swallowing, and liquid may enter the airway as a result. In older children, aspiration may be more likely to occur alongside neurological or neuromuscular disorders, such as during seizures or when anatomical (physical) or structural abnormalities are present. Often, aspiration has more than one cause.
An uncoordinated pattern during sucking, swallowing, and breathing may lead to mistimed swallowing, and liquid may enter the airway as a result. In older children, aspiration may be more likely to occur alongside neurological or neuromuscular disorders, such as during seizures or when anatomical (physical) or structural abnormalities are present. Often, aspiration has more than one cause.
Many young children outgrow swallowing problems that lead to aspiration. Our job is to keep them safe while they grow and to rule out chronic (ongoing) aspiration. This includes identifying any anatomical problems that may be causing aspiration and identifying silent aspiration (which occurs without any obvious signs or symptoms). When we catch aspiration early and treat it, your child will likely do very well.
How common is aspiration?The prevalence of aspiration is largely unknown, and pathological (disease related) aspiration is likely underdiagnosed. Everyone has the ability to aspirate a little bit, such as swallowing small amounts of saliva that enters the airway during sleep. Our bodies can handle minor aspiration events like this every now and then. At times, children may choke on water when they drink too fast or have a coughing or choking event when they eat a certain food that’s not appropriate for their age. But if your child aspirates regularly, such as with every few swallows of a drink, then there is likely an underlying cause that needs to be identified. We call this chronic, pathological (disease related) aspiration, and it is important to recognize and treat.
Everyone has the ability to aspirate a little bit, such as swallowing small amounts of saliva that enters the airway during sleep. Our bodies can handle minor aspiration events like this every now and then. At times, children may choke on water when they drink too fast or have a coughing or choking event when they eat a certain food that’s not appropriate for their age. But if your child aspirates regularly, such as with every few swallows of a drink, then there is likely an underlying cause that needs to be identified. We call this chronic, pathological (disease related) aspiration, and it is important to recognize and treat.
Swallowing is a complex series of movements and neurological responses, so children with any type of coordination problem with that process are at risk for the chance of the swallowing and breathing sequence to be mistimed. Children who have anatomical abnormalities in the throat or airway (such as a cleft in the larynx or a hole or fistula in the esophagus) may also be at a higher risk for aspiration, even if the motor function used to swallow is otherwise normal. Occasionally, part of a child’s airway does not function properly during swallowing, as can be seen with vocal cord motion disorders such as vocal cord paralysis.
Occasionally, part of a child’s airway does not function properly during swallowing, as can be seen with vocal cord motion disorders such as vocal cord paralysis.
In patients who have signs or symptoms of aspiration with each meal, such as coughing, congestion, or difficulty breathing during breastfeeding or bottle feeding, aspiration should be considered. On occasion, aspiration is silent, meaning it occurs without any cough response or abnormal reaction from your child. As a result, chronic aspiration may disguise itself as other conditions. For example, if your child has frequent or prolonged upper respiratory problems (such as repeated, long bouts of colds) or unexplained lung disease (such as recurring pneumonia) that cannot be attributed to another condition, he or she may have aspiration. Under these circumstances, your child may have symptoms that are similar to asthma but do not respond well to medication. If this sounds like your child, aspiration should be considered.
If your child frequently aspirates, he or she needs to be investigated by a pediatric otolaryngologist, otherwise known as an ear, nose, and throat (ENT) specialist. Ideally, your child should be seen at a center that specializes in airway and swallowing problems, such as our Aerodigestive and Airway Reconstruction Center or our Center for Pediatric Voice and Swallowing Disorders. That way, many experts from different specialties with specific training in feeding and swallowing disorders can weigh in, ensuring that your child gets an accurate diagnosis and comprehensive care.
How do you diagnose aspiration?Aspiration is not always obvious or easy to diagnose. That’s why we offer a full gamut of testing options to identify aspiration and, when possible, the exact cause. Because we see a large volume of children with aspiration, and we work with a team of multidisciplinary experts, we are able to identify even subtle signs of aspiration.
Generally, we start by observing your child in the clinic while he or she eats and drinks, looking for any signs or symptoms of aspiration. This is performed with a speech-language pathologist and otolaryngologist, who simultaneously observe feeding and swallowing and perform a physical exam. We also assess for anatomical differences that may lead to aspiration. To get more information, we frequently perform a swallow study. The studies complement each other and provide different information, so your child might require more than one:
- Videofluoroscopic swallow study (VFSS), also called a modified barium swallow (MBS) study. In this study, a moving x-ray shows the workings of your child’s mouth and throat muscles while he or she swallows a liquid dye called barium. We observe the path that the dye takes as it travels from the mouth into the esophagus (feeding tube to the stomach). This study is performed by a speech-language pathologist and a radiologist.

- Fiberoptic endoscopic evaluation of swallowing (FEES). In this study, which is a modified form of laryngoscopy, we place a flexible laryngoscope (a thin flexible camera) through the nose to visualize the throat, tongue, and airway as your child eats or drinks. We are able to view the larynx (voice box) to see if there are any visible anatomical defects, determine if it is functioning normally, and test for sensation. While your child eats and drinks, we watch to see if the liquid or food being swallowed follows the usual path to the esophagus. We can see if it deviates from the normal pathway and instead enters the airway above the vocal cords (penetration) or through the vocal cords (aspiration) into the trachea (windpipe) and lungs. It’s performed in our ear, nose, and throat clinic with a pediatric otolaryngologist and speech-language pathologist. Radiation is not required.
- Advanced swallowing diagnostics. If further evaluation is needed, your child can be seen in our advanced Motility Program, where multiple specialists will evaluate for aspiration.
 When we suspect a problem with the GI tract or lungs, we partner with pediatric gastroenterologists and/or pulmonologists within our Aerodigestive and Airway Reconstruction Center. The gastroenterologist assesses the GI tract for reflux, allergic problems, or motility issues; the pulmonologist views and evaluates the lungs for evidence of inflammation or infection; and the otolaryngologist evaluates the larynx (voice box) and central airway for the presence of inflammation and/or anatomical differences. This multidisciplinary approach ensures that your child only has to undergo one procedure, and receives anesthesia just once, to investigate a range of possible causes.
When we suspect a problem with the GI tract or lungs, we partner with pediatric gastroenterologists and/or pulmonologists within our Aerodigestive and Airway Reconstruction Center. The gastroenterologist assesses the GI tract for reflux, allergic problems, or motility issues; the pulmonologist views and evaluates the lungs for evidence of inflammation or infection; and the otolaryngologist evaluates the larynx (voice box) and central airway for the presence of inflammation and/or anatomical differences. This multidisciplinary approach ensures that your child only has to undergo one procedure, and receives anesthesia just once, to investigate a range of possible causes.
Our multidisciplinary Center for Pediatric Voice and Swallowing Disorders is one of the most advanced clinics in California, where otolaryngologists, speech-language pathologists, occupational therapists, and nutritionists provide care for simple to complex voice and swallowing disorders. Our speech-language pathologists (SLP) are all members of the American Speech-Language-Hearing Association (ASHA) and dedicated to the management of aspiration. We treat aspiration in a number of different ways, depending on your child’s needs. Feeding and/or swallowing therapy improves how your child eats and drinks, and it is often an important component of treatment. For example, we can improve an infant’s aspiration by changing breastfeeding positions, altering the flow rate of milk from a bottle, or thickening liquids. Sometimes we combine feeding therapy with surgical intervention if aspiration is caused by an anatomical abnormality.
Our speech-language pathologists (SLP) are all members of the American Speech-Language-Hearing Association (ASHA) and dedicated to the management of aspiration. We treat aspiration in a number of different ways, depending on your child’s needs. Feeding and/or swallowing therapy improves how your child eats and drinks, and it is often an important component of treatment. For example, we can improve an infant’s aspiration by changing breastfeeding positions, altering the flow rate of milk from a bottle, or thickening liquids. Sometimes we combine feeding therapy with surgical intervention if aspiration is caused by an anatomical abnormality.
If your child’s anatomy is not normal or is not functioning correctly, we may consider surgery. The majority of our surgeries are minimally invasive, and we are able to perform them through the mouth without making any incisions in the skin. For example, your child might have vocal cord immobility, where one of the vocal cords is not closing properly to protect the airway during swallowing, or a short laryngeal cleft, where the larynx does not separate completely from the pharynx or esophagus.
If your child has a more complex anatomical condition, such as a tracheoesophageal fistula, where there’s a hole between the trachea (tube to lungs) and esophagus (tube to stomach), or a severe or long laryngeal cleft, he or she might need a more extensive surgery. For rare and severe cases of aspiration, we have a multidisciplinary team that performs advanced operations. The team includes pediatric general surgeons, our airway reconstruction team, and our pediatric cardiothoracic surgeons. We are one of a few children’s hospitals in the Western United States to offer the entire spectrum of these complex operations and procedures.
For more information, listen to our PedsTalks discussion on aspiration or contact our Aerodigestive and Airway Reconstruction Center or our Center for Pediatric Voice and Swallowing Disorders.
EVERY PARENT SHOULD KNOW THIS: BEWARE OF ASPHIX AND ASPIRATION!
Articles / EVERY PARENT SHOULD KNOW THIS: BEWARE OF ASPHIX AND ASPIRATION!
MINISTRY OF HEALTH OF THE ROSTOV REGION GBU RO "MEDICAL INFORMATION AND ANALYTICAL CENTER"
RUN THE LIFE OF CHILDREN! DO NOT LEAVE THEM UNATTENDED!
(memo for parents)
External causes (not related to the state of health) cause the death of children under one year old not often, but they account for up to 30-35% of all causes of child mortality. Especially high risk of sudden death in the crib in children aged 2-4 months.
Especially high risk of sudden death in the crib in children aged 2-4 months.
Suffocation of a child often occurs when the child is in the same bed with the mother.
Accidental pressure on a child during sleep occurs when closing the openings of the nose and mouth with a soft object. More often it is in the first months of his life, when he does not have the strength to turn his head to the side to breathe. As a result of blocking the airways and stopping the supply of oxygen, the level of carbon dioxide rises and asphyxia occurs - suffocation of the child. Parental smoking is also an additional factor contributing to the child's inhalation of exhaust air with a high content of carbon dioxide.
Aspiration in children - inhalation of a foreign body (milk, milk formula, pieces of food, stomach contents) into the respiratory tract is another cause of death in children under one year old. This happens when the child is in the wrong position during feeding and profuse regurgitation, when the child’s head is thrown back, swallowing is difficult, and also, if the nasal passages during feeding are blocked by the mammary gland, the child tries to inhale through the mouth and milk enters the respiratory tract, all this can lead to aspiration.
REMEMBER! SAFETY OF CHILDREN IS CARE OF ADULTS!
Tips for new moms: Keep your baby safe and avoid risk factors!
- hold the baby at the breast for no more than 20 minutes;
- do not block the mother's nasal passages while breastfeeding;
- breastfeed and continue breastfeeding as long as possible, especially in the first 6 months of life, which strengthens the immune system and reduces the risk of sudden death of the child;
- hold the child after feeding in a "column", pressing vertically to himself for 2-3 minutes, which will facilitate the discharge of air that has entered the stomach during feeding;
- to lay the child of the first months of life on his side, so that in case of regurgitation, gastric contents do not enter the respiratory tract;
- when feeding from a bottle, make sure that the neck of the bottle and the nipple are constantly filled with formula and do not contain air during feeding;
- formula should be warm, but not cold or hot, so as not to cause cramping.

- children should not be overfed;
- do not put the baby on his stomach for sleep until he begins to actively roll over;
- prevent the child from being put into bed to sleep with you;
- do not put the baby to bed with soft blankets, feather bed soft toys; the pillow should be flat, no more than 3 cm thick;
- get rid of nicotine addiction: passive inhalation of tobacco smoke leads to the sudden death of a child in a dream;
- prevent overheating or hypothermia of the child, which may have an adverse effect on respiratory and cardiac activity;
- do not practice tight swaddling, which can cause the baby to overheat and limit his physical activity;
- to ensure a constant optimal (23-24 ° C) temperature in the room for the child to stay;
- it is strictly forbidden to shake the newborn while playing, pumping, etc., so as not to damage the delicate vessels of the brain;
- do not shy away from vaccination: it protects the baby from many serious problems, in the absence of medical contraindications, the child must be vaccinated.

In case of critical situations that threaten the life of the child, seek medical help immediately!
Reminders for parents - GBUZ JSC "City Polyclinic No. 10"
M EMERGENCY FOR THE PREVENTION OF ACCIDENTS
Rules for feeding and sleeping a child
- Breastfeeding rules
1.1. Get into a comfortable sitting or lying position. Bring the baby to your chest so that his head and body are in the same plane. The baby should be facing the breast: its nose is located opposite the nipple.
1.2. If desired, you can support the chest from below with your whole hand or put four fingers under the chest, and the fifth (large) on top.
1.3. Touch the nipple to the baby's lips, and when the baby opens his mouth wide, press his body tightly to you. If the baby is properly attached to the breast, he captures with his mouth not only the nipple, but also most of the halo with the tissue located under it.
In this case: the child's chin touches the chest; his mouth is wide open; his lower lip is turned outward; you can see most of the halos above the upper lip and not under the lower. You do not experience any discomfort in the chest.
1.4. As a rule, the child himself releases the chest satisfied and sleepy.
1.5. The baby's nasal passages should not be blocked by the mother's breast during feeding.
1.6. Hold the baby at the sternum for more than 20 minutes. The baby sucks out most of the required volume of feeding in 5-10 minutes, the rest of the time it mainly satisfies the sucking reflex.
- Artificial feeding
2.1. In bottle feeding, adequate selection of the opening in the nipple is of great importance.
2.2. The hole should be such that when the milk bottle is tipped over, the milk will flow out only in drops through the hole in the nipple.
2.3. When feeding from a bottle, make sure that the neck of the bottle and the nipple are constantly filled with formula and do not contain air during feeding. Air entering the neck causes air to be sucked in by the baby. In this case, the child does not eat up, and he easily has regurgitation and vomiting.
Air entering the neck causes air to be sucked in by the baby. In this case, the child does not eat up, and he easily has regurgitation and vomiting.
2.4. The nutrient mixture should be warm. A cold or hot mixture can cause a reflex spasm of the muscles of the esophagus and stomach.
2.5. After feeding, it is necessary to hold the child in an upright position for 2-3 minutes, which will facilitate the discharge of air that has entered the stomach during feeding.
2.6. As a rule, the child himself releases the breast (or bottle) satisfied and sleepy.
- Sleep rules
3.1. The best place for sleeping a child of the first year of life is a crib in the parents' bedroom, for children over 1 year old - a crib in the nursery. Sleeping in the same bed with parents is prohibited.
- Prevention of aspiration in children
Aspiration in children is the ingestion of a foreign body (milk, formula, pieces of food, stomach contents) into the respiratory tract.
4.1. In newborns, aspiration may be caused by regurgitation of breast milk or formula. Follow the rules for feeding children. After feeding, the newborn baby should be laid on the barrel, turning the head to the side.
4.2. During feeding, the nasal passages of the child should not be closed by the mother's breast.
4.3. During breastfeeding, it is necessary to refrain from alcohol - alcohol dulls the vigilance of the mother. A woman who has drunk can take the child with her to bed so that she can feed him at night without waking up. The child may choke, suffocate, or get other injuries.
4.4. During a meal, the act of swallowing can be affected by various psycho-emotional states. Sudden laughter, screaming, fright, or crying can cause a food bolus to back up from the pharynx into the upper respiratory tract.
4.5. Be careful with a small child. Don't leave him alone! Do not allow small objects (coins, balls, buttons and other small objects) to be played with. Pay attention to small fragments of toys, even if the child is in front of your eyes, because inhaling them is a matter of a few seconds!
Pay attention to small fragments of toys, even if the child is in front of your eyes, because inhaling them is a matter of a few seconds!
4.6. You do not need to feed your baby nuts, seeds, peas, dense whole berries, small sweets, because babies often inhale these foods. Don't risk your own children's lives!!
- Burn prevention
5.1. Children should not be left unattended.
5.2. Make sure that there are no hot objects in the reach of children ( hot food or liquids, sockets, switched on iron, etc. ).
5.3. Items that can cause burns ( matches, hot objects, chemicals and other ) should be kept out of the reach of children.
5.4. Don't let a small child turn on the taps in the bathroom and kitchen until he or she knows how to mix hot and cold water. Even water at 60 degrees can cause a serious burn in just half a minute of contact with it. You should carefully check the water before bathing and in the process of bathing the child.
5.5. Do not carry hot liquids and food over areas where the child plays.
5.6. Do not open the oven if there is a small child in the kitchen.
5.7. Avoid using open coil heaters (boilers).
5.8. When cooking on the stove, turn on the back burners and turn the pots and pans with their handles inward. This will prevent children and you yourself from accidentally turning over a hot pot or pan.
5.9. Do not delay repairing faulty electrical outlets and plugs. Do not use appliances with faulty wiring.
5.10. A high danger is fraught with an electric kettle, especially one that has just boiled. Therefore, even if you are sure that the device itself is located out of the reach of the child, still check the location of its cord as well - whether the child can pull it and tip the kettle over.
5.11. Cover accessible sockets with special devices so that your baby cannot put anything into them. Electrical cords from appliances should be out of reach of the child - the baby can take the cord in his roti and try to bite it.
Prevention of burns
Prevention of burns in young children is primarily the care and responsibility of adults who are nearby.
Dear parents, be careful!
Every fifth injury in children is a burn. Sometimes a few seconds are enough for the irreparable to happen, so the child must be under the PERMANENT supervision of adults.
- Prevention of children falling out of windows
To avoid an accident involving a child falling out of a window, the following rules must be followed:
6.1. When opening windows in the apartment and ventilating the room, make sure that the child is under supervision.
6.2. During ventilation, open transoms and vents. If you do open a window, then do not open it more than 10 cm, set limiters for this purpose.
6.3. Do not allow a child to go to the balcony without adult supervision.
6.4. Never leave a sleeping child alone in the apartment. The baby can wake up and climb to the open window.
The baby can wake up and climb to the open window.
6.5. Move all furniture, including beds, away from windows. This will help prevent your baby from accidentally getting on the windowsill.
6.6. Do not show your child how the window opens. The later he learns to open the window on his own, the safer his stay in the apartment will be.
6.7. Do not teach your child to place a chair or other device under their feet in order to look out the window or look into the street from the balcony. Subsequently, acting in this way, he may lean out too much and fall out of the window (from the balcony).
6.8. Mosquito nets pose a great danger: the child sees some obstacle in front, confidently leans on it, and as a result, the child can fall out along with the net, which is not designed for the weight of even the smallest one-year-old baby.
6.9. If a child of 5-7 years old is afraid to be alone in the apartment, do not leave him even for a short time. Often, feeling fear, children look out the window or from the balcony, hoping to see their parents, which may cause them to fall from the balcony.
Today we will talk about some aspects of the prevention of respiratory infections in children.
Acute respiratory infections in children are the most common reason for seeking medical help from a pediatrician, pulmonologist, ENT doctor.
As a rule, the incidence increases sharply from the moment the child visits preschool institutions.
Respiratory pathogens (viruses, bacteria) are characterized by damage to the mucous membranes of the respiratory tract and weakening of local protective factors.
Most infectious agents enter through the nasal mucosa.
In order to strengthen this natural barrier, various agents are often used that are injected directly into the nasal passages, i.e. intranasally.
The first thing we usually start with is saline solutions.
In outpatient and inpatient practice, we most often use isotonic saline or 0.9% sodium chloride solution, as well as various preparations based on sterile sea water, which can be isotonic and hypertonic.
These products can be used both for the purpose of daily hygiene of the nasal cavity, and for the prevention and treatment of ARI.
Salt solutions, being quite safe, help to remove mucus and normalize the protective function of the ciliated epithelium of the nasal mucosa. Hypertonic solutions help reduce mucosal edema.
Recombinant interferons are currently popular in the form of drops, spray, ointment, gel, and oxolinic ointment.
However, these drugs do not have very high activity.
Apricot oil, lanolin, vaseline, which are part of the ointments, also prevent the penetration of viruses into the cells of the nasal mucosa.
Also have barrier properties agents that are powdered cellulose of vegetable origin.
These preparations contribute to the protection of the nasal mucosa from contact with viruses (also with allergens), thanks to the formation of a special film.
The next group of drugs is bacterial lysates in the form of an intranasal spray, which include antigens from almost all major pathogens of upper respiratory tract infections.
Bacterial lysates stimulate local defense factors, which leads to both preventive and curative effects.
And in conclusion, I would like to say that
- All of the listed drugs should be used as prescribed by a doctor in accordance with the instructions.
- Storage conditions must be observed.
- When choosing an intranasal preparation, individual tolerance must be taken into account.
- The most effective way to prevent respiratory infections is vaccination.
First aid procedure
Subfebrile temperature (up to 38°C)
- Undress the child.
- Wipe with a damp cloth (slightly above room temperature).
- Do not use antipyretics.
Febrile temperature (above 38°C)
- Keep calm, put to bed.
- Drink plenty of sweet tea, fruit drink.
- Keep the child warm in case of chills (warm blanket, hot tea).
- Give antipyretics.
- At a temperature of 39.
 5-40°C, the child should not be wrapped.
5-40°C, the child should not be wrapped. - If the temperature is above 40.4°C, call for emergency help and give an antipyretic.
Specialist comment (pediatrician, candidate of medical sciences Gavrilova T. A.)
The normal temperature is not 36.6°C, as is often believed, but 36.0–37.0°C, in the evening it is slightly higher, than in the morning. Body temperature rises with many diseases. The benefits of elevated temperature are a signal of illness, a way to fight pathogens (many bacteria and viruses stop multiplying at temperatures above 37-38 ° C), this is a stimulus for the immune response, since a number of protective factors (including interferon) are released only at temperatures above 38°C.
By lowering the fever, we do not affect the cause of the disease, but we can improve the child's well-being. Subfebrile temperature (up to 38 ° C) may appear when overheating, with a viral or bacterial infection. Taking antipyretics in such cases is not worth it if the child's well-being does not suffer.
At "febrile" temperature (above 38°C) there is vasoconstriction, increased muscle contractions (hence - chills, trembling), in young children - convulsions (the so-called "febrile" convulsions).
When the temperature rises to 39.5–40.0°C, the skin vessels dilate (the skin turns red), such a child should not be wrapped up.
Fever is dangerous in spasm of skin vessels - this is malignant hyperthermia.
Symptoms:
- temperature above 40.4°C;
- mottled, marbled skin;
- limbs cold to the touch;
It is necessary to call an emergency and be sure to give an antipyretic, preferably in a solution inside.
Antipyretics Children should be given antipyretics at temperatures above 38.0°C, but if the child does not tolerate high temperatures, is anxious, cries, or has seizures at elevated temperatures, antipyretics are given at temperatures above 37.5°C. After giving an antipyretic, you can not calm down: be sure to consult a doctor (for recovery, you will need to take other drugs).