Baby breathless when feeding
Laryngomalacia (for Parents) - Nemours KidsHealth
What Is Laryngomalacia?
Laryngomalacia is a common cause of noisy breathing in infants. It happens when a baby's larynx (or voice box) is soft and floppy. When the baby takes a breath, the part of the larynx above the vocal cords falls in and temporarily blocks the baby's airway.
Laryngomalacia (luh-ring-oh-muh-LAY-shuh) usually gets better on its own by the time a baby is 1 year old.
What Are the Signs & Symptoms of Laryngomalacia?
Babies with laryngomalacia make a harsh, squeaky sound when breathing in. This sound, called stridor, can start as soon as the baby is born or, more often, in the first few weeks after birth. Symptoms usually get worse over several months.
Most babies with laryngomalacia do not have trouble breathing or feeding, even though their breathing is noisy. Breathing usually gets noisier when the baby is crying, feeding, sleeping, lying down, or has an upper respiratory infection.
Most babies with the condition have mild symptoms. A baby whose symptoms are more serious might have:
- trouble breathing (look for tugging in at neck or stomach)
- feeding problems
- poor weight gain
- breathing pauses (apnea)
- blue skin or lip color (cyanosis)
Call the doctor right away if your baby has these symptoms or breathing suddenly gets worse.
Babies with laryngomalacia often have gastroesophageal reflux (GER). This happens when food and acid go back up into the esophagus. If stomach acid reaches the voice box, symptoms may get worse. Formulas or medicines to help with reflux may help with breathing symptoms.
What Causes Laryngomalacia?
Doctors don't know what causes laryngomalacia, but it may have something to do with how the voice box formed before the baby was born. The muscles supporting the voice box may be weak or don't coordinate well with breathing. Gastroesophageal reflux may also play a role.
How Is Laryngomalacia Diagnosed?
Doctors often suspect laryngomalacia at birth or soon after based on the baby's symptoms and an exam. To confirm the diagnosis, a pediatric ear, nose, and throat (ENT) specialist will do a procedure called flexible laryngoscopy. To do this, the doctor passes a thin tube through the baby's nose or mouth to look at the airway and vocal cords in the voice box.
The doctor may check oxygen levels and order other tests to check for swallowing problems or GER. The baby's good weight gain and growth are very important.
How Is Laryngomalacia Treated?
Most of the time, laryngomalacia gets better on its own, usually by a baby's first birthday. Doctors will do regular exams to check the baby's breathing and weight. Because most babies also have GER, doctors usually prescribe anti-reflux medicine.
A baby who has severe breathing problems or poor growth may need a surgery called supraglottoplasty (soo-pruh-GLOT-oh-plass-tee). Doctors do this procedure through the baby's mouth to tighten the floppy tissue above the voice box. This will improve the baby's feeding and breathing.
This will improve the baby's feeding and breathing.
What Else Should I Know?
Noisy breathing and other laryngomalacia symptoms usually get worse over several months, then start to improve after 3–6 months. Symptoms clear up completely in most kids. Occasionally, an older child with a history of laryngomalacia may have noisy breathing while exercising, during a viral infection, or when sleeping.
Reviewed by: Steven M. Andreoli, MD
Date reviewed: October 2019
Hertfordshire and West Essex Healthier Together
For wear and tear, minor trips and everything in between.
Self-care
You can treat your child's very minor illnesses and injuries at home.
Some illnesses can be treated in your own home with support and advice from the services listed when required, using the recommended medicines and getting plenty of rest.
Sound advice
Children can recover from illness quickly but also can become more poorly quickly; it is important to seek further advice if a child's condition gets worse.
For information on common childhood illnesses go to What is wrong with my child?
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP.
- Remember that if your child's condition gets worse, you should seek further medical advice immediately.
- Help your child to understand - watch this video with them about going to the pharmacy.
For information on common childhood illnesses go to What is wrong with my child?
Health visitors are nurses or midwives who are passionate about promoting healthy lifestyles and preventing illness through the delivery of the Healthy Child Programme. They work with you through your pregnancy up until your child is ready to start school.
They work with you through your pregnancy up until your child is ready to start school.
Health Visitors can also make referrals for you to other health professionals for example hearing or vision concerns or to the Community Paediatricians or to the child and adolescent mental health services.
Contact them by phoning your Health Visitor Team or local Children’s Centre.
Sound advice
Health visitors also provide advice, support and guidance in caring for your child, including:
- Breastfeeding, weaning and healthy eating
- Exercise, hygiene and safety
- Your child’s growth and development
- Emotional health and wellbeing, including postnatal depression
- Safety in the home
- Stopping smoking
- Contraception and sexual health
- Sleep and behaviour management (including temper tantrums!)
- Toilet training
- Minor illnesses
For more information watch the video: What does a health visitor do?
School nurses care for children and young people, aged 5-19, and their families, to ensure their health needs are supported within their school and community. They work closely with education staff and other agencies to support parents, carers and the children and young people, with physical and/or emotional health needs.
They work closely with education staff and other agencies to support parents, carers and the children and young people, with physical and/or emotional health needs.
Contacting the School Nurse
Primary and secondary schools have an allocated school nurse – telephone your child’s school to ask for the contact details of your named school nurse.
There is also a specialist nurse who works with families who choose to educate their children at home.
Sound Advice
Before your child starts school your health visitor will meet with the school nursing team to transfer their care to the school nursing service. The school nursing team consists of a school nursing lead, specialist public health practitioners and school health staff nurses.
They all have a role in preventing disease and promoting health and wellbeing, by:-
- encouraging healthier lifestyles
- offering immunisations
- giving information, advice and support to children, young people and their families
- supporting children with complex health needs
Each member of the team has links with many other professionals who also work with children including community paediatricians, child and adolescent mental health teams, health visitors and speech and language therapists. The school health nursing service also forms part of the multi-agency services for children, young people and families where there are child protection or safeguarding issues.
The school health nursing service also forms part of the multi-agency services for children, young people and families where there are child protection or safeguarding issues.
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors/GPs can treat many illnesses that do not warrant a visit to A&E.
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, call 111. An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.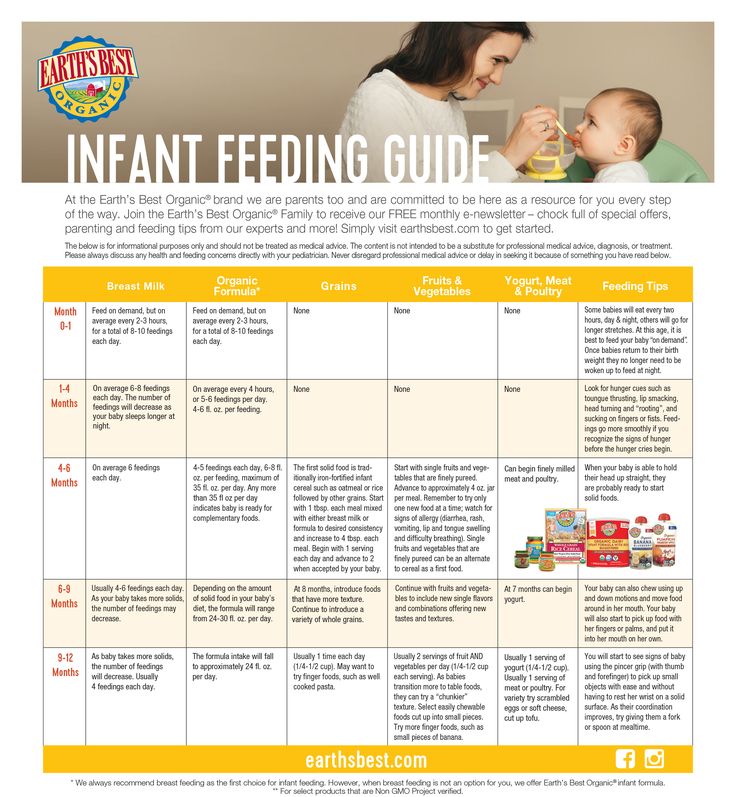
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services.
For information on common childhood illnesses go to What is wrong with my child?
A&E departments provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.
Sound advice
- Many visits to A&E and calls to 999 could be resolved by any other NHS services.
- If your child's condition is not critical, choose another service to get them the best possible treatment.
- Help your child to understand – watch this video with them about going to A&E or riding in an ambulance
The child chokes when feeding: what to do?
Nikulina Anastasia Anatolyevna
pediatrician
A newborn chokes when feeding for various reasons. Some of them the mother can eliminate, while others depend on the health of the baby. The pediatrician Anastasia Anatolyevna Nikulina will explain the causes and solutions to this problem.
Some of them the mother can eliminate, while others depend on the health of the baby. The pediatrician Anastasia Anatolyevna Nikulina will explain the causes and solutions to this problem.
— Anastasia Anatolyevna, at what age do children most often choke while feeding?
— In the first weeks of life, when the swallowing reflex is still very weak, it is difficult to dose milk supply from the breast. From the bottle, the flow of formula is controlled by the opening in the nipple and the tilt. If the hole in the nipple is not age appropriate, it is tight, then the newborn swallows air. Excess air with the mixture will enter the intestines, causing discomfort to the baby.
Why does the baby choke while breastfeeding or bottle feeding
- Baby position or bottle angle not optimal. in the optimal position. In the right position, the hand of the woman who holds the child lies on the support. Hold the baby by the back and shoulders, directing the head to the chest.
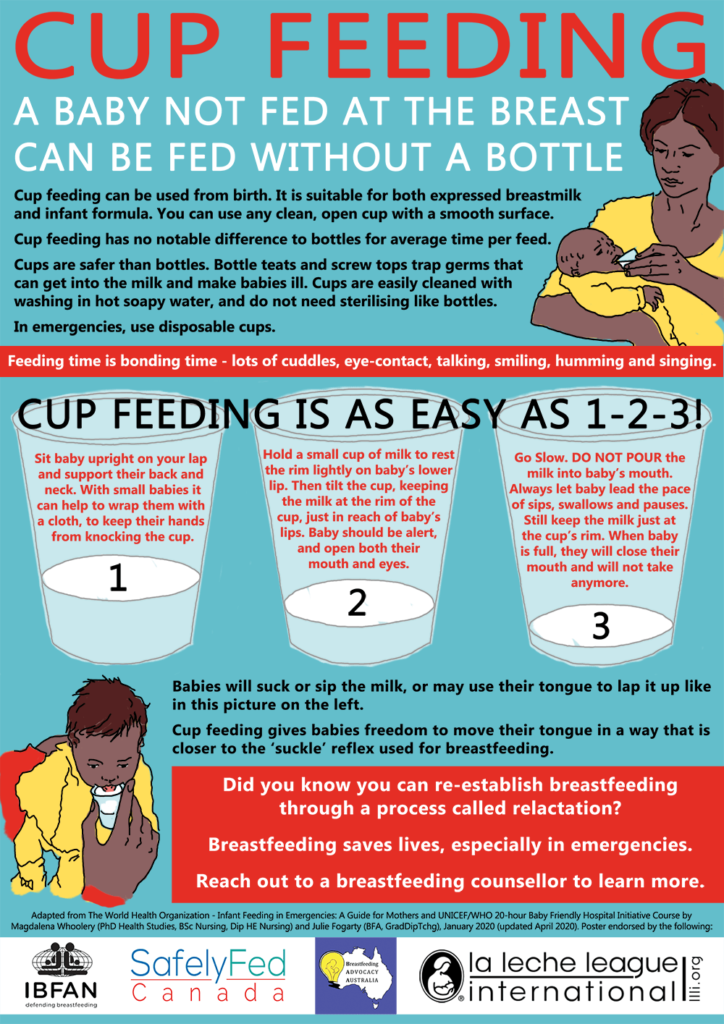 You can’t press hard on the head - the baby will recline it back reflexively.
You can’t press hard on the head - the baby will recline it back reflexively. - Anatomical features of the mother's breast, in which a woman produces enough breast milk, but it is difficult for a child to suck it out, to eat. Before feeding, the mother needs to express some of the milk or massage the breast: it will become soft, and it will be easier for the baby to suck.
- Large nipples are difficult for a baby to grab - to solve the problem, there are special nipple covers through which newborns are fed. You can feed your baby with expressed milk through a bottle and a nipple that is correctly selected for age.
- Hyperlactation. Pressurized breast milk squirts into the baby's mouth. Before feeding, some of the foremilk is expressed, and the following, more fatty, does not form a strong flow. Breaks in the sucking process also help.
- Frequent breastfeeding. The absence of long breaks between attachments to the breast prevents children from hunger and, with it, the rush to feed.

- Incorrect bottle delivery method. The neck of the bottle must be completely filled with milk: this way there will be no air in the milk. The nipple is selected taking into account the age of the baby.
- Disease. Nasal obstruction or cough interferes with feeding. Relief of the symptoms of the disease will improve nutrition. For some children, problems can be caused by improper swallowing or reflux.
- To understand why the baby is having difficulty swallowing, you need to gradually eliminate each of the possible causes. Even the environment matters. During feeding hours, it is desirable for a woman to be alone with the child, nothing should distract him from the process. If the mother finds it difficult to identify the cause, a pediatrician will help her.
— What should I do if my child chokes on milk or formula?
- Spontaneous cough is the main symptom that appears when the act of sucking and swallowing is disturbed. The baby is crying and refuses to eat.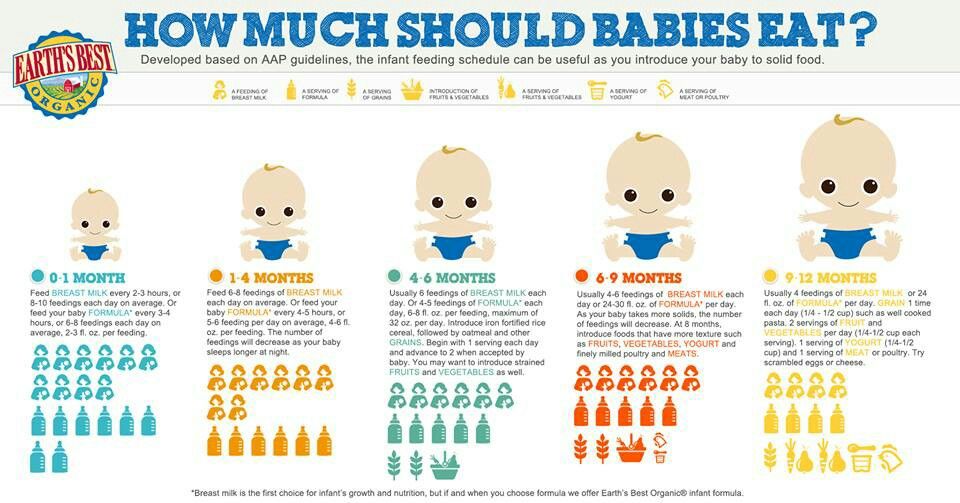
First aid for choking children
If you can’t cough up excess milk on your own or the baby chokes on saliva and starts to choke, you need to do the following, dosing the force of your actions:
- Place the baby on one hand with the belly down, with your free hand apply pressure on the area above the navel (on the area of the baby's stomach), supporting the chin.
- Tilt the child slightly forward, lightly pat on the back. This will increase the cough and help restore breathing.
- Can I continue feeding after the baby clears his throat, or should I take a break?
- Feeding can be continued after the baby clears his throat. It is advisable to vilify it with a column for two to three minutes, so that excess air comes out, and then resume feeding.
- Does increasing the interval between feedings help with the problem?
- On the contrary, the prevention of flooding will be frequent feeding.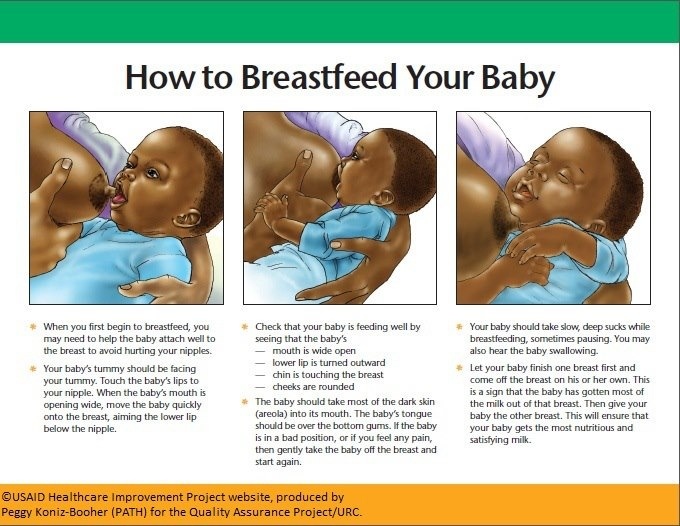 With numerous attachments, less milk accumulates in the woman’s breast, it becomes easier for the mother to feed.
With numerous attachments, less milk accumulates in the woman’s breast, it becomes easier for the mother to feed.
If the child is choking, feeding should be interrupted. The baby will cough, rest and continue to suck. If the situation recurs frequently, be sure to consult your pediatrician. Your doctor can help you find the best breastfeeding or formula-feeding method for you.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
#Tips for Mom #regurgitation 7-12 #regurgitation 12 plus
See also
Neurologist for a child under one year old: first examination
#Tips for Mom #Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Goat's milk in children's nutrition: for or against
#Food #Tips for mom #Baby digestion #breastfeeding
Javier Diaz Castro
professor, lecturer
Digestion in newborns and infants and its features
#Baby Digestion #breast-feeding #baby formula #Lure #Tips for mom #Baby development
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
First tests and vaccinations: how to prepare yourself and your child
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Omicron in children: how dangerous it is and how babies get sick up to a year
#Advice for Mom
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
How to tell if a baby has a food allergy
#allergy #Tips for mom #breast-feeding #baby formula #lure
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Calendar of doctor visits during the first year of a child's life
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Principles of successful lactation: checklist for mom
#Advice to mom #breastfeeding
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
How to properly rock a baby to sleep
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Why DHA, ARA and lutein are added to infant formula
#baby formulas #Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
See all
View all
Goat's milk in children's nutrition: for or against
# Lure # Tips for Mom # Baby's digestion # breastfeeding
Javier Diaz Castro
professor, lecturer
Digestion in newborns and infants and its features
# Baby digestion # breast-feeding # infant formula # Lure # Tips for Mom # Baby development
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Neurologist for a child under one year old: first examination
# Tips for mom # Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Calendar of doctor visits during the first year of a child's life
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Principles of successful lactation: checklist for mom
# Tips for mom # breastfeeding
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
How to properly rock a baby to sleep
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Why DHA, ARA and lutein are added to infant formula
# infant formula # Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Omicron in children: how dangerous it is and how babies get sick up to a year
# Tips for mom
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
First tests and vaccinations: how to prepare yourself and your child
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
How to tell if a baby has a food allergy
# allergy # Tips for Mom # breast-feeding # infant formula # lure
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
View all
View all
The baby gets tired quickly when feeding and breathes often: symptoms, diagnosis
With the advent of the baby, all the mother's attention is focused on feeding the baby.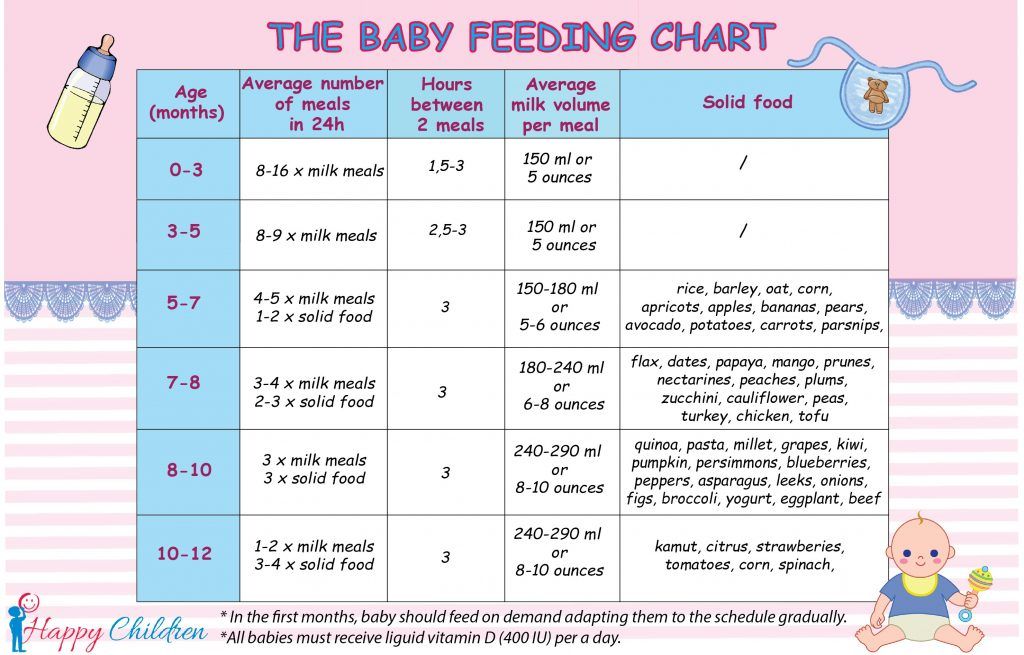 After all, I really want the baby to gain weight well. But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
After all, I really want the baby to gain weight well. But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
In pediatric cardiology, there are several important signs that indicate heart problems in a young patient. The children's cardiologist of the multidisciplinary center "Edkarik" will be able to figure out what caused the difficulties in feeding. At the first negative symptoms in the baby, parents should contact us to exclude the presence of a serious heart pathology in the crumbs.
Features of breathing in infants
It should be noted right away that difficulty breathing during feeding is not always an indicator of an existing heart pathology. Such a symptom is typical for respiratory diseases, breathing difficulties may be associated with structural features of the nasal septum. This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm.
This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm.
The breathing of children in the first months of life has its own characteristics. Babies need twice the amount of oxygen, but their respiratory system is not yet completely formed. Certain difficulties in the respiratory function are imposed by narrow nasal passages and weakness of the pectoral muscles. Therefore, breathing in children up to a year is uneven. The child often takes quick breaths, so his breathing is shallow and intermittent.
The norm of respiratory movements in babies of the first month of life is 40-60, from the end of the fourth week and up to 3 months - up to 45, in the period of 4-6 months - 35-40. By the year, the baby is already taking about 30-35 breaths per minute, which is considered the norm.
Mom can determine the respiratory rate on her own.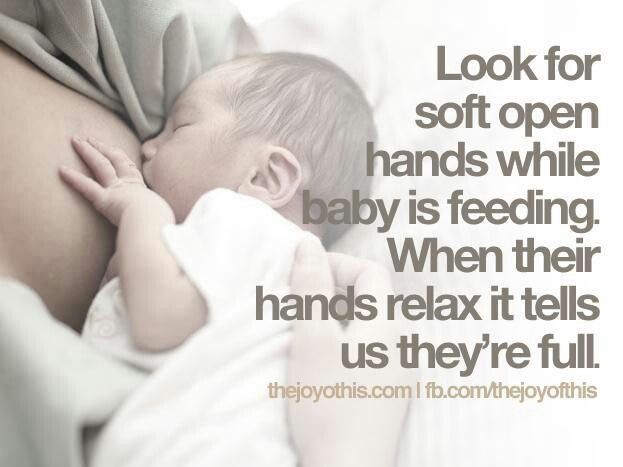 To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
When there is no reason to worry
The nervous system of young children is still imperfect, so they cannot control their breathing. During active games and crying, the frequency of respiratory movements increases, and in a dream they often sniffle. If such features are observed sporadically, you should not worry. The sniffing nose can be washed with boiled water, and then carefully remove the dried mucus.
What should cause alarm
You need to see a doctor if the baby:
- holds his breath for a long time;
- exhales noisily;
- if breathing is accompanied by wheezing and wheezing.
Typically, such symptoms can be traced against the background of an acute period of respiratory diseases.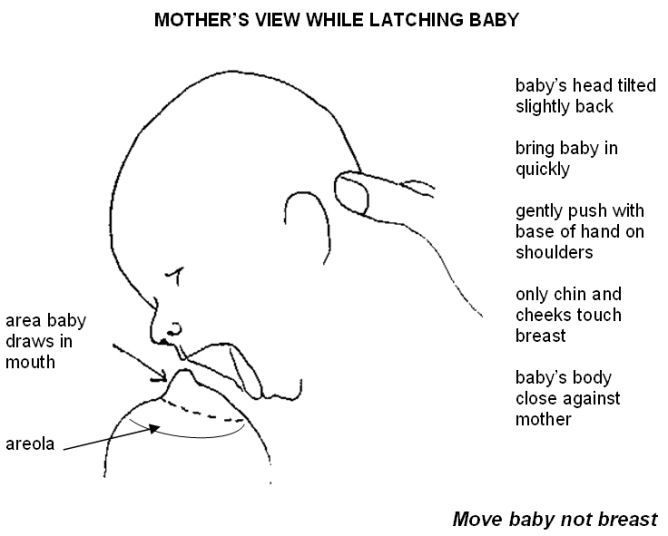 Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Which symptoms require special attention
We have listed physiological breathing problems. But sometimes the situation is much more serious than the usual runny nose. We list the signs that should be a strong argument for parents to urgently visit a pediatric cardiologist.
- Cyanosis
If holding the breath during feeding is accompanied by a blue nasolabial triangle, this sign indicates a lack of oxygen. In severe forms of cardiac pathologies, the chin and fingers of the baby turn blue. This symptom is characteristic of congenital malformations of both the heart and vascular anomalies.
- Shortness of breath
This symptom also indicates a lack of oxygen. Since the child has to expend more energy during sucking, this symptom is more pronounced than at rest. A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
- Fatigue
Infants with congenital heart defects are much less active than healthy children. They are not able to suck out the norm during feeding, so they lose weight. The problem is aggravated by frequent breathing. The child simply suffocates under tension.
- Chest pain
Infants may not complain of such a symptom, but an observant mother will notice under what circumstances and how often the child begins to worry.
If all the described signs are repeated from the baby during feeding regularly, it is urgent to consult a pediatric cardiologist. A full-scale examination will determine the cause of the problem, and an experienced pediatric cardiologist will prescribe adequate therapy for the child.
Peculiarities of diagnosing infants
Babies under one year old cannot describe the symptoms that prevent them from developing normally. Therefore, all hope for an objective examination. During the initial examination of the infant, a pediatric cardiologist:
- evaluates the general condition;
- notes the color of the skin;
- listens to the baby's heart;
- performs heart rate monitoring and saturation level measurement.
The doctor pays special attention to taking an anamnesis, since such information can indicate the cause of the problem. For example, an infection transmitted by a woman during her mother's pregnancy can provoke the development of congenital heart defects. An important factor is heredity, especially if there were cases of premature death (up to 50 years) among close relatives in the family. After collecting the data, the pediatric cardiologist will definitely prescribe the following types of diagnostic procedures:
- ECG with daily monitoring;
- ultrasound of the heart;
- Chest x-ray;
- Laboratory tests.

Instrumental methods of examination with the use of modern devices will clarify the parameters of the baby's heart and the features of its anatomical structure. Ultrasound diagnostics helps to identify defects in the heart chambers and great vessels. Having the data of all studies at hand, the pediatric cardiologist will draw up an individual treatment program, or prescribe additional procedures. In severe cardiac pathologies and rhythm disturbances, the question of a surgical way to eliminate the problem can be decided.
Examination and treatment in the center "Edkarik"
Among our guarantees:
- professionalism of doctors;
- high quality service;
- comfortable conditions in the clinic;
- individual approach;
- a wide range of services provided;
- accompanying patients during the rehabilitation period.
Our clinic is known not only in Kaliningrad, but also in other regions of the country.