Baby feeding chart australia
Infant formula feeding
Category: Child Health
Topics: Babies and Toddlers, Diet and Eating
If you are not able to breastfeed your baby, infant formula is the only safe way of feeding your baby to around 6 months of age. Formula-fed babies are kept on formula until 12 months of age in addition to complementary food. Talk to your doctor or child health nurse before you start feeding your baby infant formula.
When preparing and giving your baby infant formula:
- Follow the instructions on the can to make sure your baby is getting the right nourishment
- Sterilise bottles by boiling for 5 minutes
- Wash your hands before you prepare a bottle
- Keep feeding your baby on demand
- Hold your baby while he or she is drinking.
Combining breastfeeding and infant formula feeding
Feeding your baby any amount of breastmilk has benefits for you and your baby. You might be able to combine breastfeeding with formula feeding if you are unable to give your baby only breastmilk. Here are some tips to help you:
- Try to breastfeed first before giving formula.
- Any breastmilk has benefits to mother and baby, even if it is only a few drops.
- The more you can express or breastfeed, the more milk you will make.
Choosing an infant formula
There are many types of infant formula in grocery stores and chemists. Your doctor, child health nurse or dietitian will advise you on a suitable type of infant formula.
Remember…
- Cow’s milk-based formulas are right for most babies. They are recommended over infant formulas made from soy or goat’s milk.
- Special or soy-based formulas only need to be used for medical reasons. They should only be used with advice from a health professional.
- All infant formulas in Australia have enough nutrients to meet the growing needs of babies.
- Babies’ stomachs cannot break down regular milk. Avoid giving milk to babies younger than 12 months of age.
Getting started
Infant formulas can be a little bit different from one another. Always use the instructions on the can to make sure you are making it right for your baby. It is safest to feed your baby as soon as you make the formula. Only make 1 bottle at a time. Here is a list of steps for you to follow:
- Clean all preparation areas. Wash your hands using soap and water.
- Wash and sterilise bottles, teats and caps.
- Boil fresh water. If using an automatic kettle, let it switch off.
- Leave water to sit for at least 30 minutes to cool. Pour the right amount of water into the bottle.
- Add the amount of formula listed on the can. Too much and it can hurt your baby’s kidneys; too little and your baby won’t grow well. Measure the formula with the scoop from the can and level with a knife. Take care not to mix up scoops from other containers.
- Shake the bottle until the powder is dissolved.
- Check the temperature by putting a few drops on your wrist. It should feel just warm.
- You can now feed your baby. Hold your baby while he or she is drinking.
- Any formula left at the end of the feed must be discarded.
- Only keep made-up formula in the fridge for 24 hours.
Preparing feeds in advance
It is best to make 1 bottle of infant formula at a time, just before feeding. Sometimes you may need to make feeds in advance (e.g. for a babysitter). Here are some tips:
- Keep made-up feed in the fridge (temperature no higher than 5°C).
- Feeds can be stored in the fridge for up to 24 hours. Only remove when ready to be used.
Warming infant formula
- Stand the bottle of formula in a container of hot water for a few minutes (no more than 10 minutes). Using a microwave to rewarm feeds is not recommended, as it does not heat evenly and can burn your baby’s mouth.
 You can use a bottle warmer if you have one.
You can use a bottle warmer if you have one. - Check the temperature by putting a few drops onto the inside of your wrist. It should feel warm or even a little bit cool.
- Any formula left at the end of the feed must be discarded.
Transporting infant formula
The best way to transport formula is to carry individual portions of the powdered formula and cooled boiled water in sterilised containers. Formula can also be made before transporting. Here are some tips:
- Feeds that need to be transported should be put in the fridge until they are cold before transporting.
- Keep the feed in the fridge until it needs to be transported.
- Transport feeds in a cool bag with ice bricks and use within 2 hours. Place the formula in the fridge if you arrive before then. Use the formula within 24 hours from the time it was made.
Cleaning feeding equipment
Equipment needs to be cleaned and sterilised.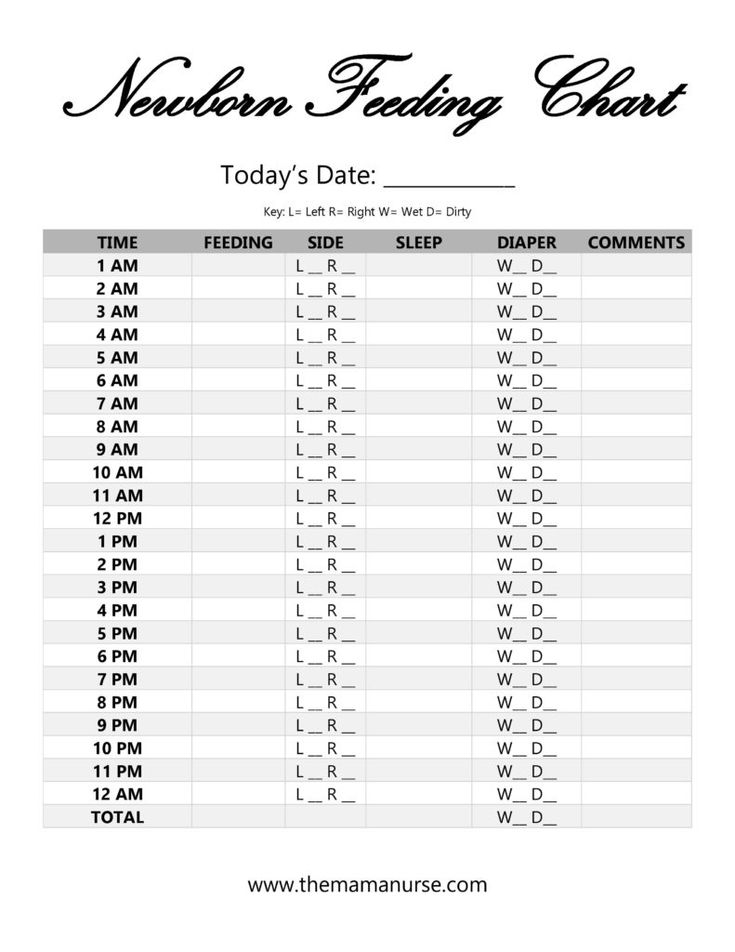 Clean bottles and teats by hand or in a dishwasher. Bottles and teats can be sterilised by boiling or with a steaming machine. (Use steamers according to the manufacturers’ instructions).
Clean bottles and teats by hand or in a dishwasher. Bottles and teats can be sterilised by boiling or with a steaming machine. (Use steamers according to the manufacturers’ instructions).
Boiling method
- Wash hands.
- Wash teats and bottles in hot, soapy water using a bottle brush and rinse well.
- Place equipment in a saucepan of cold water on a stove.
- Bring to the boil and boil for 5 minutes. Turn off and allow to cool.
- Store equipment in a clean container in the fridge if not being used immediately.
- Sterilised equipment can be stored in the fridge for up to 24 hours.
How much formula?
Feed your baby on demand. Each baby is different and needs vary from day to day. Refer to the Is my baby getting enough milk? sheet if you are concerned about how much your baby is drinking.
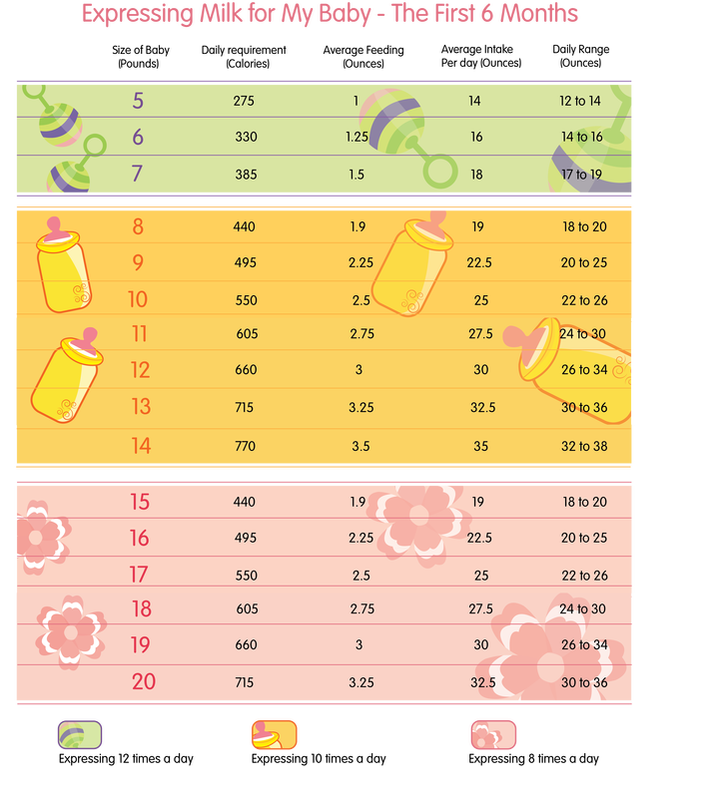
This is a general guide of how much infant formula your baby might need:
- 5 days to 3 months old: 150mL per kilogram of body weight each day.
- 3 to 6 months old: 120mL per kilogram of body weight each day.
- 6 to 12 months old: 100mL per kilogram of body weight each day. Babies at this age also eat complementary foods.
How to feed
- Sit comfortably with your baby in your arms while giving the bottle. Try holding your baby a different way each feed. This is because a baby’s skull is soft and changes in shape can occur if the baby always places their head in the same position.
- Hold the bottle tilted upside down. You can gently press under your baby’s chin to encourage your baby to firmly grip the teat. This will help the baby to not swallow air.
- Check the bottle flow. The milk should drop at a steady flow from the teat. Sometimes the teat gets clogged when a powdered infant formula is used.
- It is common for babies to swallow some air. You can help your baby to burp by holding them upright over your shoulder or on your lap. Pat or rub the middle of their back gently until they burp.

- If the baby is feeding happily, don’t stop until they are finished.
- Avoid leaving your baby to feed on their own or while going to sleep. The milk may flow too fast and cause your baby to choke.
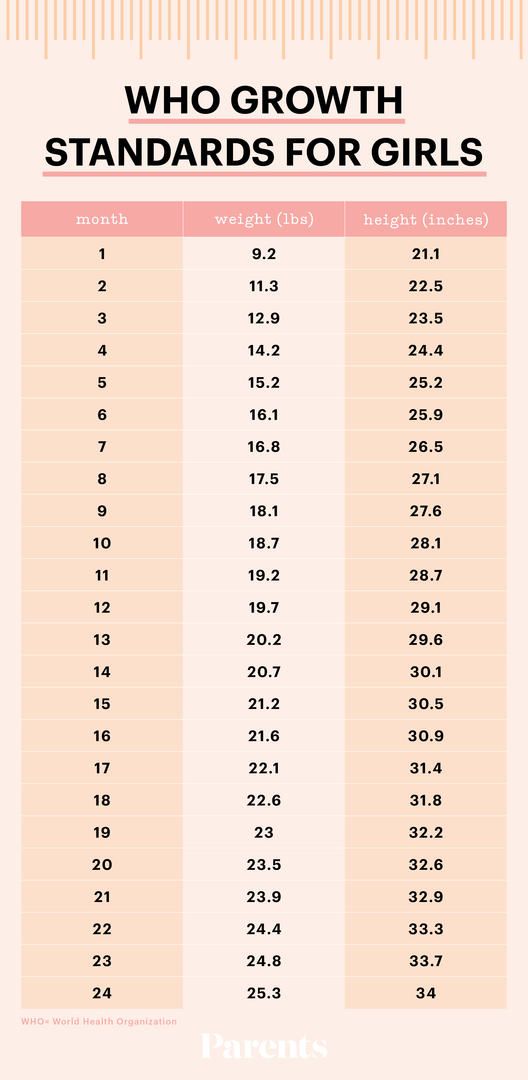
- Your baby is feeding well if they have 6 or more wet nappies per day, consistent weight gain (following a curve on their growth chart), and are alert and content after a feed.
Resources for parents, families and carers
Booklet: Child health information (PDF, 1.34MB), Queensland Government (given to parents of every baby born in Queensland with the Personal Health record)
Growing Strong—Formula feeding (PDF, 799kB), Queensland Government
Raising Children Network—Newborns nutrition, Australian Government
Raising Children Network—Breastfeeding videos, Australian Government
Booklet: Breastfeeding and postnatal care, New South Wales Government—available in English, Arabic, Chinese (Simplified), Chinese (Traditional), Farsi, Hindi, Korean, Punjabi and Tamil languages
Related content
The importance of breastfeeding
Managing common breast concerns
Is my baby getting enough milk?
Drinks for babies and toddlers
Acknowledgements
This fact sheet is consistent with the National breastfeeding strategy 2010–2015.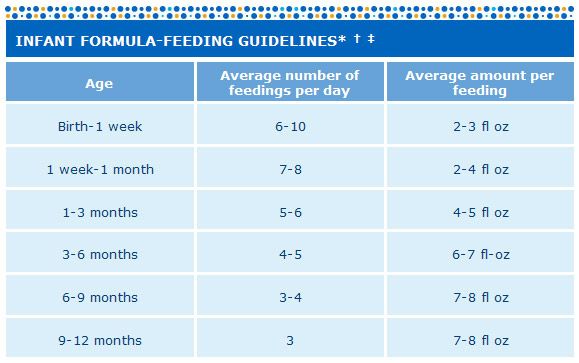
Information is drawn from:
- Children’s Health Queensland Hospital and Health Service 2015, Child health information: Your guide to the first 12 months.
- National Health and Medical Research Council 2012, Australian dietary guidelines.
- National Health and Medical Research Council 2012, Infant feeding guidelines.
- Preventative Health, Queensland Health 2008, Growing Strong: Feeding you and your baby.
- Preventative Health, Queensland Health 2010, Breastfeeding and your baby.
- Queensland Maternity and Neonatal Clinical Guidelines Program 2010, Breastfeeding initiation.
This fact sheet is also the result of input and effort from many health professionals in Queensland. Their assistance with the content is greatly appreciated.
This information is provided as general information only and should not be relied upon as professional or medical advice. Professional and medical advice should be sought for particular health concerns or events.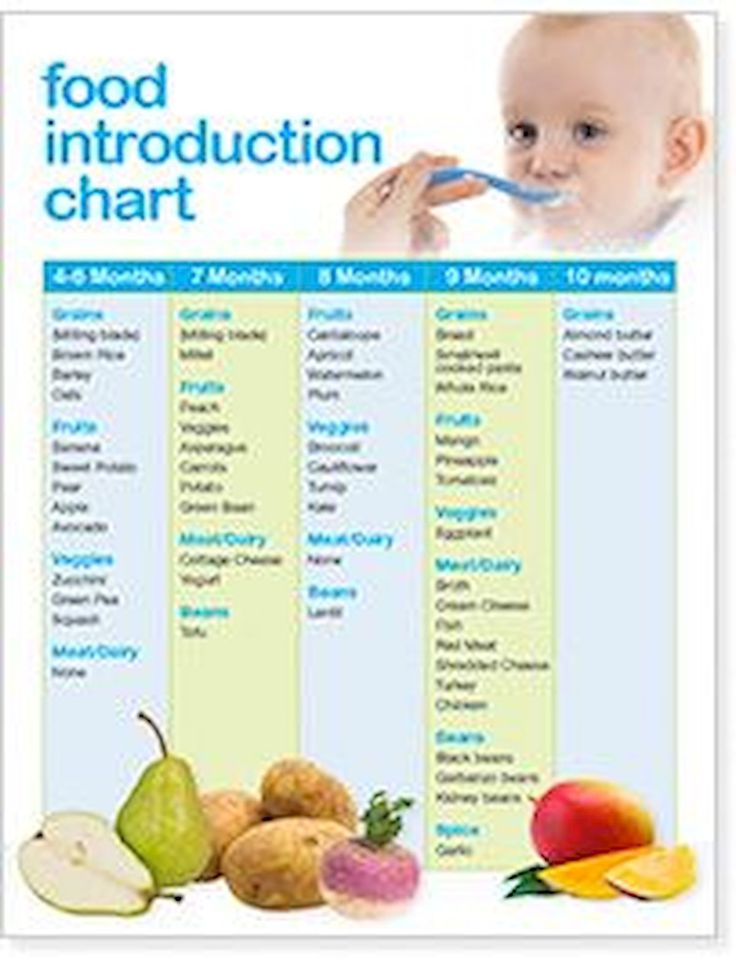 Best efforts have been used to develop this information, which is considered correct and current in accordance with accepted best practice in Queensland as at the date of production. The State of Queensland (Queensland Health) does not accept liability to any person for the information provided in this fact sheet nor does it warrant that the information will remain correct and current. The State of Queensland (Queensland Health) does not promote, endorse or create any association with any third party by publication or use of any references or terminology in this fact sheet.
Best efforts have been used to develop this information, which is considered correct and current in accordance with accepted best practice in Queensland as at the date of production. The State of Queensland (Queensland Health) does not accept liability to any person for the information provided in this fact sheet nor does it warrant that the information will remain correct and current. The State of Queensland (Queensland Health) does not promote, endorse or create any association with any third party by publication or use of any references or terminology in this fact sheet.
Back to top ( http://conditions.health.qld.gov.au/healthcondition/condition/8/31/325/infant-formula-feeding#top )
- Last updated:
- 20/09/2017 2:59:36 PM
Bottle-feeding babies: giving the bottle
About bottle-feeding
If your baby can’t always feed directly from your breast, you might choose to bottle-feed with expressed breastmilk. Or you might need to feed your baby infant formula, which is the only safe alternative to breastmilk.
Or you might need to feed your baby infant formula, which is the only safe alternative to breastmilk.
Before you bottle-feed your baby, it’s important to know how to clean and sterilise bottle-feeding equipment, as well as how to prepare, store and warm bottles of formula. This will help to keep your baby safe from infection and make sure baby is getting the right nutrition.
Getting the right flow when bottle-feeding
To test the flow of the formula or breastmilk, hold the bottle upside down when it’s filled with liquid at room temperature. The liquid should drip steadily from the teat but not pour out.
If you have to shake the bottle vigorously to see the drip, the flow is too slow. Your baby might go to sleep before drinking what they need.
When you feed your baby, you might see a little leakage at the corners of your baby’s mouth. This doesn’t mean the flow is too fast. It’s nothing to worry about. It will stop as your baby gets older.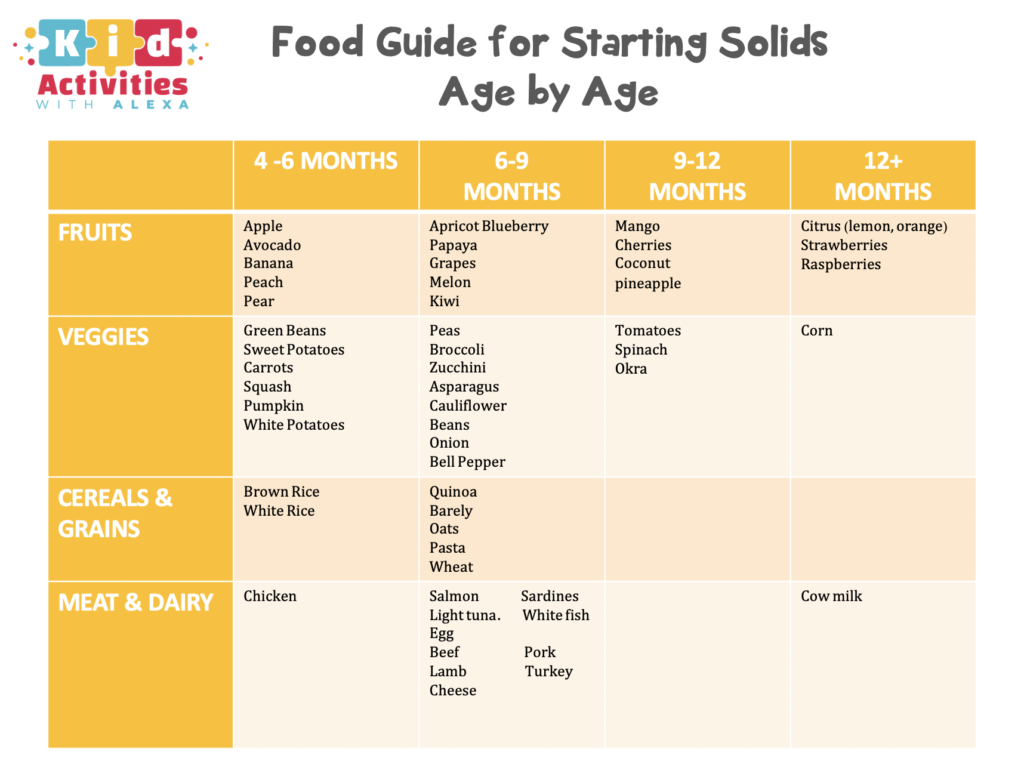
If you have trouble finding a teat with a flow to suit your baby, try a faster teat rather than a slower one. You might need to try a few different teats before you find one that suits.
Giving baby the bottle
Make yourself comfortable and cuddle your baby close to you, holding baby gently but firmly. It’s better for your baby to be on a slight incline so any air bubbles rise to the top, making burping easier.
Put the teat against your baby’s lips. Your baby will open their mouth and start to suck. Keep the neck of the bottle at an angle so it’s filled with formula or breastmilk.
When your baby stops sucking strongly or when about half of the formula or breastmilk has gone, gently remove the bottle and see whether baby wants to burp. Once you’ve tried burping your baby, you can offer the bottle again.
Paced bottle-feeding
Babies who are normally breastfed might find it hard to pace themselves when bottle-feeding, particularly if they’re premature.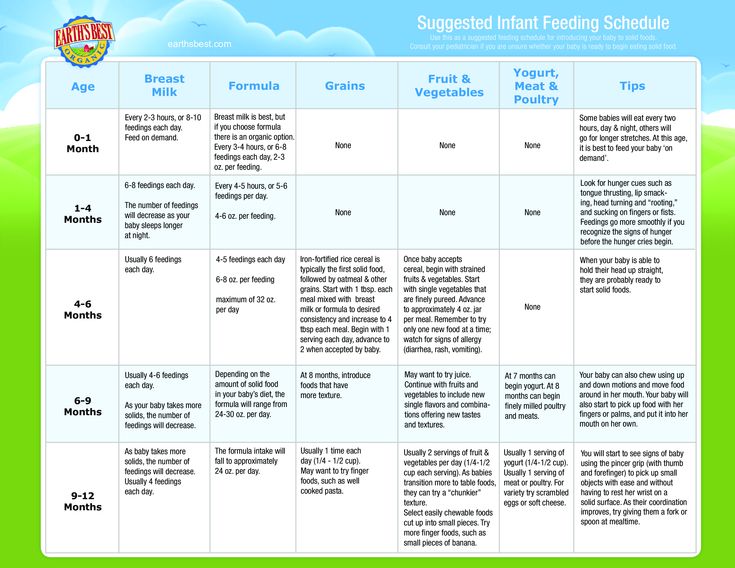 This is because they’re used to controlling the flow of breastmilk. Sometimes these babies can drink too much too quickly.
This is because they’re used to controlling the flow of breastmilk. Sometimes these babies can drink too much too quickly.
Paced feeding can sometimes help. This involves holding your baby in an upright position and letting them rest every few minutes. If you’re interested in paced bottle-feeding, it’s best to get help from your child and family health nurse or a lactation consultant.
Holding, cuddling and talking to your baby during feeding will help baby develop and grow. It’s also a great opportunity to bond with your baby.
When baby doesn’t finish the bottle or goes to sleep while feeding
Don’t worry if your baby doesn’t finish the bottle. Babies are very good at judging how much they need, so you can let your baby decide when they’ve had enough formula or breastmilk.
If your baby goes to sleep during a feed, put baby over your shoulder, rub their back, and stroke their head, legs and tummy. This can help your baby to wake up. A nappy change is a good way to wake up your baby if that doesn’t work.
Wait until your baby is properly awake before offering the rest of the formula or breastmilk.
If there’s any formula or breastmilk left in the bottle, throw it away after one hour. When your baby drinks from a bottle of formula or breastmilk, bacteria from their mouth get into the milk. The bacteria can grow and make your baby sick if you give your the baby the half-finished bottle later.
When baby refuses the bottle
Babies sometimes refuse a bottle altogether. Here are things to try if this happens:
- Try a new feeding position or change the feeding environment. For example, move around while you’re feeding, find a quieter place to feed, or play some relaxing background music.
- Try again later when your baby is more settled. For example, give your baby a bath and then try again.
- Ask your partner or another family member to give your baby the bottle.
- Try using a different teat. If the flow of formula or breastmilk is too slow, it might frustrate your baby.
- Let your baby open their mouth for the bottle when they’re ready, rather than putting the teat into their mouth.
- Offer the formula or breastmilk from a small cup or spoon. To do this, sit your baby up and offer them small sips.
If your baby is regularly refusing the bottle, you could try adjusting your routine.
If you think your baby is refusing the bottle because they’re unwell, treat your baby’s symptoms or take your baby to see your GP.
How much do bottle-feeding babies drink?
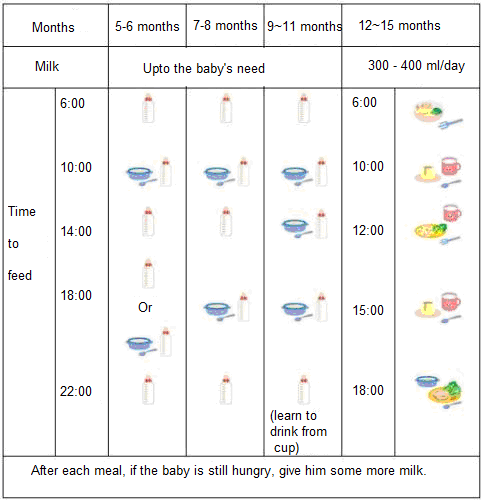
Newborn babies commonly have 6-8 feeds every 24 hours, but there’s no set amount of food or number of feeds your baby should have. Different babies drink different amounts of formula or breastmilk. Some might have feeds close together and others further apart. And it can change from day to day.
Just feed your baby whenever they’re hungry. You’ll see baby cues that say ‘I’m hungry’ – for example, your baby will make sucking noises or start turning towards the breast or bottle.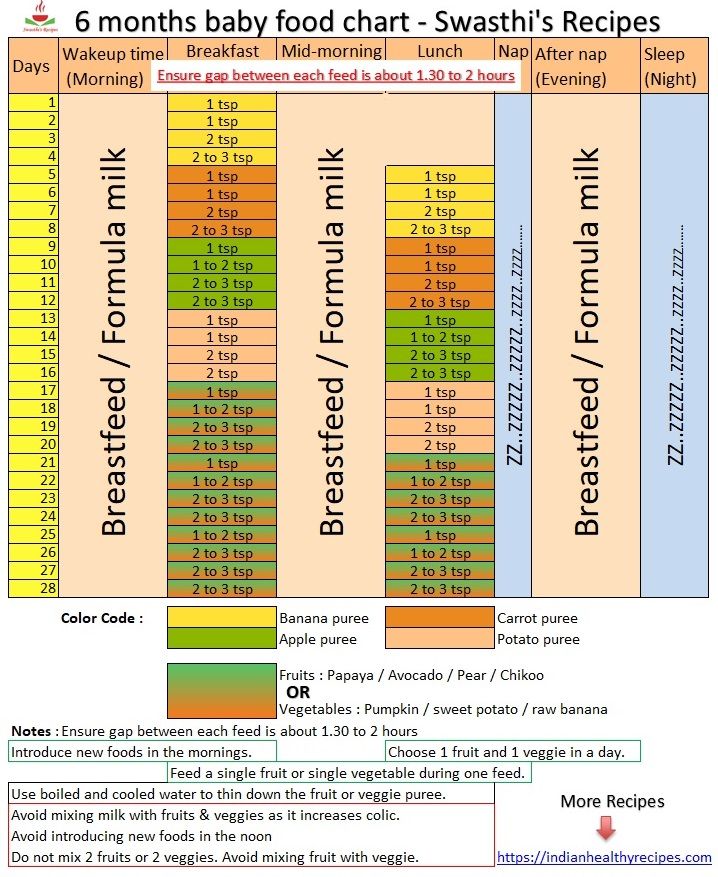 If your baby stops sucking or turns their head away from the bottle, you’ll know they’ve had enough.
If your baby stops sucking or turns their head away from the bottle, you’ll know they’ve had enough.
As your baby eats more and more solid food, the total amount of breastmilk or formula they take in a day will decrease. The amount of breastmilk or formula will also decrease as your baby starts to drink from a cup instead of a bottle.
Some babies never drink the ‘recommended amount’ for their age and size, and others need more. Plenty of wet nappies, consistent healthy weight gains, and a thriving, active baby mean all is well. If you’re concerned about how much breastmilk or formula your baby is taking, talk to your child and family health nurse or GP.
Bottle-feeding in bed: issues and risks
Sleep associations
If your baby gets used to falling asleep with a bottle in bed, they might depend on it to get to sleep. This can make it more difficult for your child to fall asleep or settle for sleep independently.
Bottle-feeding in bed also has several risks for your baby.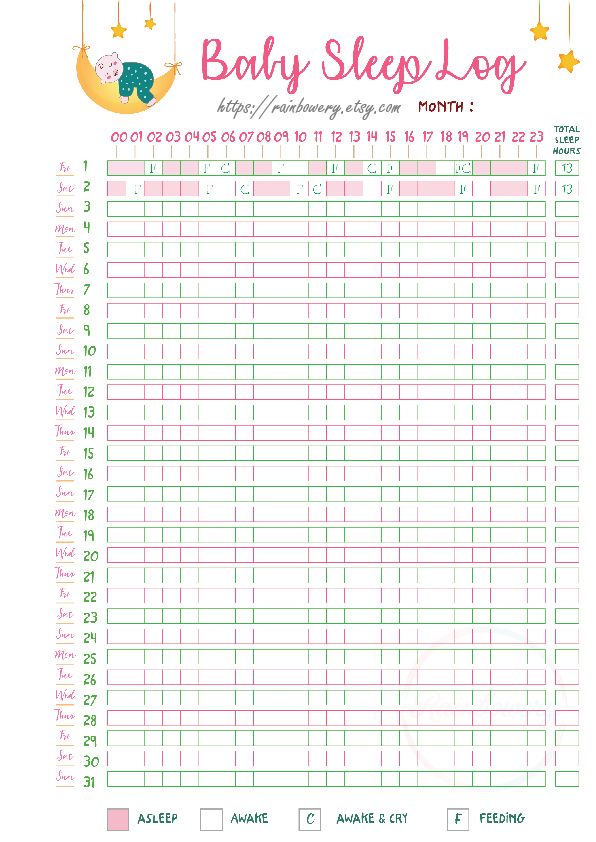
Choking
Babies who fall asleep while bottle-feeding can draw liquid into their lungs. They might then choke on it or inhale it.
Tooth decay
Babies have less saliva in their mouths to protect their teeth during sleep. If your baby falls asleep with a bottle, the lactose in the milk can build up on your baby’s teeth, putting your baby at risk of tooth decay.
Ear infections
If your baby drinks while lying flat, milk can flow into the ear cavity, which can cause ear infections.
It’s best to put your baby to bed without a bottle or to take the bottle away after your baby has finished feeding.
Using a feeding cup
When your baby is around 6 months old, you can help your baby start leaning to drink from a cup. It’s best to stop using bottles by the time your baby is 12 months old.
You should continue to thoroughly wash and sterilise feeding cups containing infant formula or breastmilk until your baby is 12 months old.
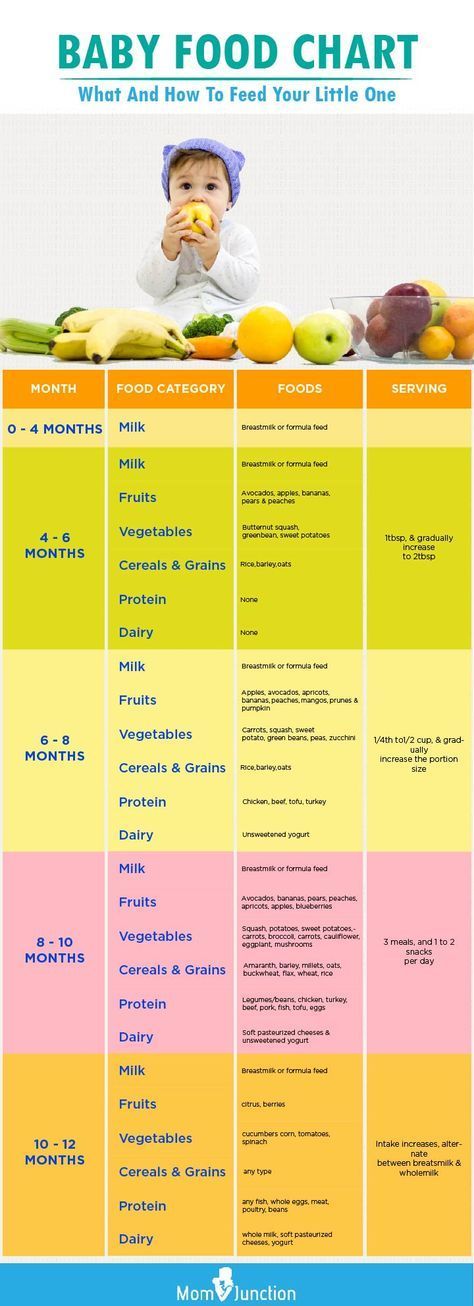
Complementary feeding scheme for artificial feeding. Complementary feeding table
For the full development of a child under 1 year of age who is artificially fed, timely and competent introduction of complementary foods is mandatory. It will prepare the baby's body for the assimilation of adult food and significantly enrich the baby's diet.
Lactose-free milk Valio Eila UHT, enriched with vitamin D, 1.5%, 1 l More
Drinking yogurt Viola without filler Clean Label®, fat-free, 280 g Read more
Formula-fed babies are more prepared to accept new foods than babies who are exclusively breastfed by their mothers. Nevertheless, there are important rules that you must know.
Complementary feeding on artificial feeding should be introduced gradually and only if the baby is healthy. Start with one product. The transition to the next one can be done only when the child is used to the previous type of complementary foods. Feed your baby only on a high chair and never when he is lying down. Start with mashed foods. When the child has a chewing reflex, the puree can be replaced with more solid foods. They will help to properly form the jaw apparatus. Be guided by the personal recommendations of your pediatrician and the table of complementary foods, and in between meals, do not forget to give your child water to drink.
Start with one product. The transition to the next one can be done only when the child is used to the previous type of complementary foods. Feed your baby only on a high chair and never when he is lying down. Start with mashed foods. When the child has a chewing reflex, the puree can be replaced with more solid foods. They will help to properly form the jaw apparatus. Be guided by the personal recommendations of your pediatrician and the table of complementary foods, and in between meals, do not forget to give your child water to drink.
Carefully monitor the reaction of the baby's body to each new product introduced. Symptoms such as loose stools, rashes or redness on the skin should not be ignored. Perhaps this indicates intolerance to a child's body of any product. In this case, you will have to exclude it from the baby's diet and replace it with another.
According to the recommendations of the World Health Organization, complementary foods should be introduced at the age of 6-8 months. The conducted scientific research and the accumulated experience of the Scientific Center for Children's Health of the Russian Academy of Medical Sciences allow us to propose some adjustments and additions to the specified scheme. It has been established that the minimum age at which the introduction of the first complementary foods is possible is 4 months. Before this period, the child is not yet ready to assimilate food other than human milk or infant formula. By 4 months With age, the child’s gastrointestinal tract becomes more mature: the initially increased permeability of the mucous membrane of the small intestine decreases, a number of digestive enzymes mature, a sufficient level of local immunity is formed, the child acquires the ability to swallow semi-liquid and thicker food, associated with the extinction of the “spoon ejection reflex”. At the same time, late feeding (after 6 months) can cause a pronounced deficiency of micronutrients (iron, zinc, etc.) and the need for the rapid introduction of a large number of products, which leads to an increased allergenic load, as well as a delay in the formation of chewing skills and swallowing thick food.
The conducted scientific research and the accumulated experience of the Scientific Center for Children's Health of the Russian Academy of Medical Sciences allow us to propose some adjustments and additions to the specified scheme. It has been established that the minimum age at which the introduction of the first complementary foods is possible is 4 months. Before this period, the child is not yet ready to assimilate food other than human milk or infant formula. By 4 months With age, the child’s gastrointestinal tract becomes more mature: the initially increased permeability of the mucous membrane of the small intestine decreases, a number of digestive enzymes mature, a sufficient level of local immunity is formed, the child acquires the ability to swallow semi-liquid and thicker food, associated with the extinction of the “spoon ejection reflex”. At the same time, late feeding (after 6 months) can cause a pronounced deficiency of micronutrients (iron, zinc, etc.) and the need for the rapid introduction of a large number of products, which leads to an increased allergenic load, as well as a delay in the formation of chewing skills and swallowing thick food.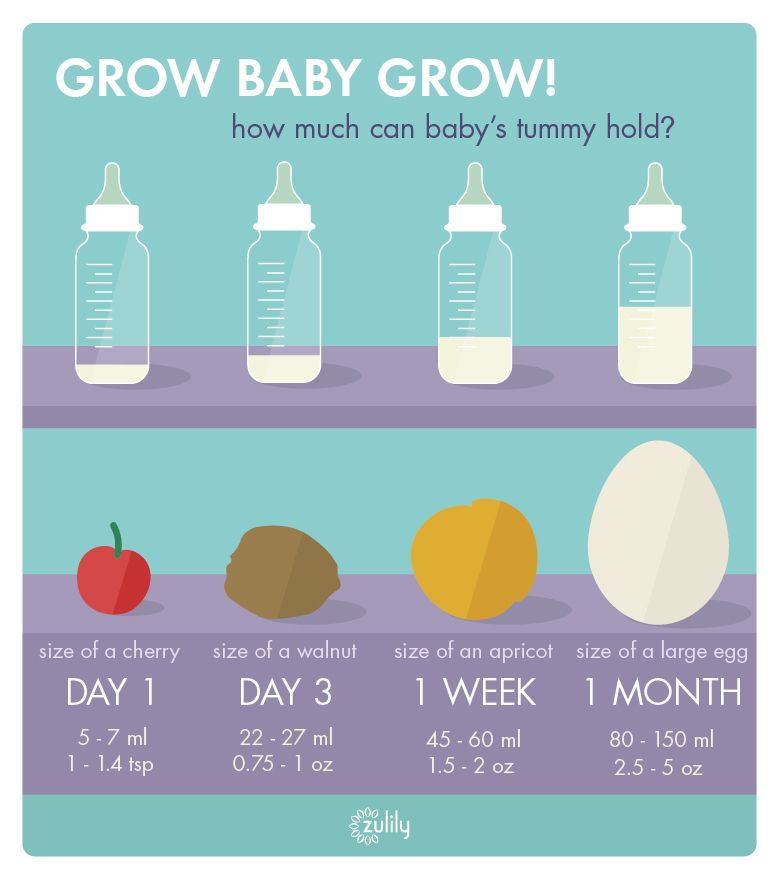 Therefore, it is advisable to introduce complementary foods to children at the age of 4–6 months. The timing of the introduction of complementary foods is set individually for each child, taking into account the peculiarities of the development of the digestive system, excretory organs, the level of metabolism, as well as the degree of development and functioning of the central nervous system, that is, its readiness to perceive new food.
Therefore, it is advisable to introduce complementary foods to children at the age of 4–6 months. The timing of the introduction of complementary foods is set individually for each child, taking into account the peculiarities of the development of the digestive system, excretory organs, the level of metabolism, as well as the degree of development and functioning of the central nervous system, that is, its readiness to perceive new food.
Given that modern adapted milk formulas contain the necessary set of vitamins and minerals, there is no need to correct for these substances with complementary foods earlier than when breastfeeding. Therefore, the scheme for the introduction of complementary foods can be the same. The proposed approximate scheme for the introduction of complementary foods to children of the first year of life is presented in the table. Up to six months, the child has an underdeveloped gastrointestinal tract and not all the enzymes necessary for the assimilation of complementary foods are produced.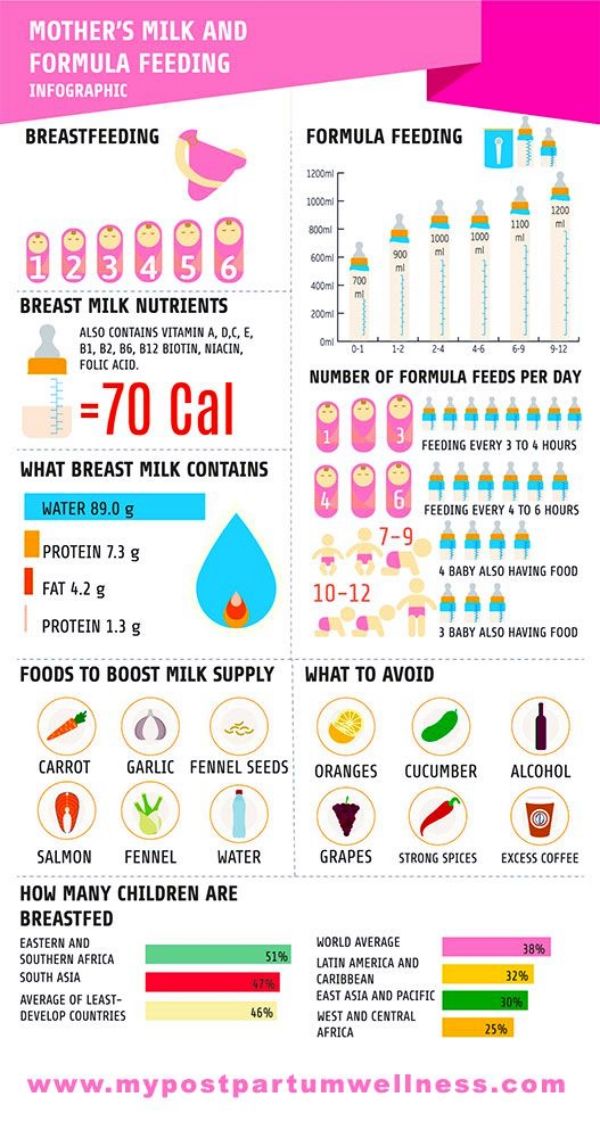 If complementary foods are introduced later than this period, it will be difficult for the baby to overcome the stereotype of eating only liquid food.
If complementary foods are introduced later than this period, it will be difficult for the baby to overcome the stereotype of eating only liquid food.
Complementary feeding table for children under 1 year of age with artificial feeding
Specialists in the field of baby food have developed the following table of complementary foods by month:
Before introducing complementary foods, make sure that the child's body is ready for it. Signs to look out for:
- maturity of the gastrointestinal tract;
- weakening of the ejection reflex of solid food;
- the readiness of the child for the chewing process - the appearance of the first teeth;
- the ability of the infant to be stable in a sitting position;
- emotional readiness of the baby to get acquainted with new taste sensations.
Learn more about the formula-fed baby menu in our blog. Consider all these recommendations, but do not forget that you need to introduce complementary foods to a child on artificial feeding under the supervision of the attending pediatrician.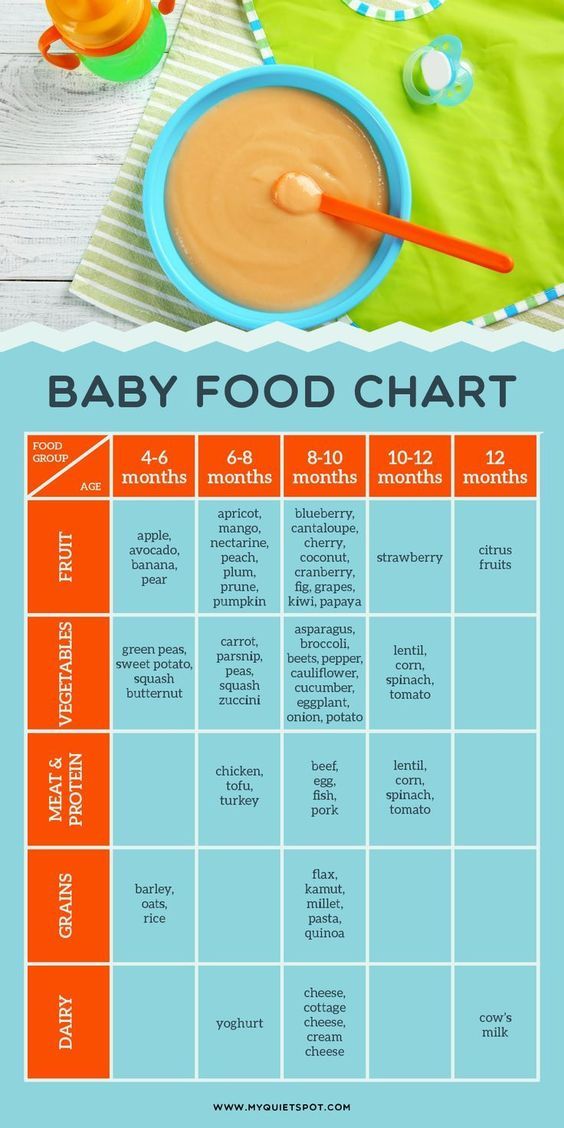 Be healthy!
Be healthy!
2.13 24
FoodShare:
Oksana Ivargizova
Medical Institute. Pavlova, specialization - pediatrics
You might be interested
Author: Reetta Tikanmäki
Palm oil in baby food
Infant milk formulas are made from cow's milk. However, in terms of fat composition, it differs significantly from that of the mother.
Read
Author: Ivargizova Oksana
How to choose milk formula for a baby
Breast milk is the best food for a newborn baby. It contains all the necessary nutritional components that fully meet the needs of the child and are necessary for his healthy and harmonious development.
It contains all the necessary nutritional components that fully meet the needs of the child and are necessary for his healthy and harmonious development.
Read
Show all
Complementary feeding schedule | Nutriclub
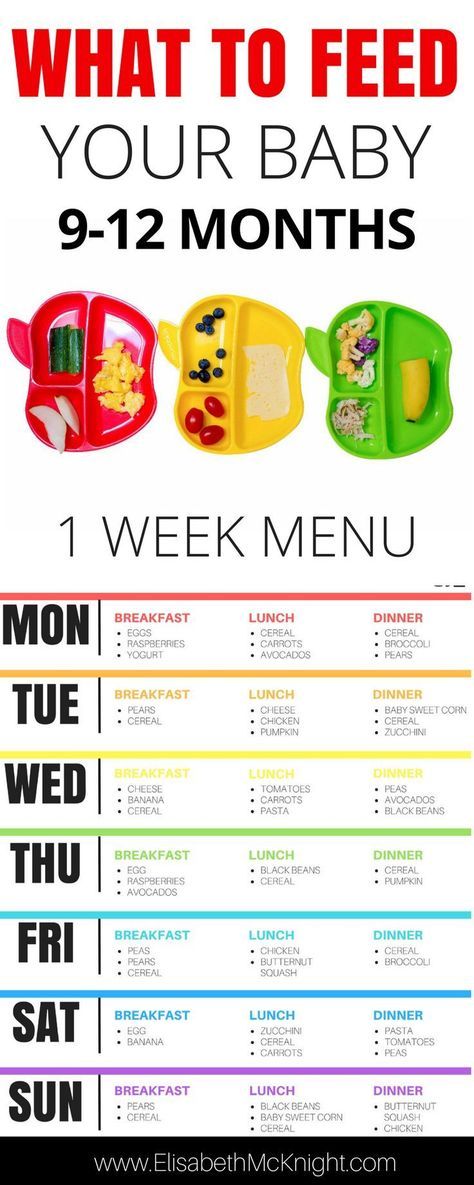
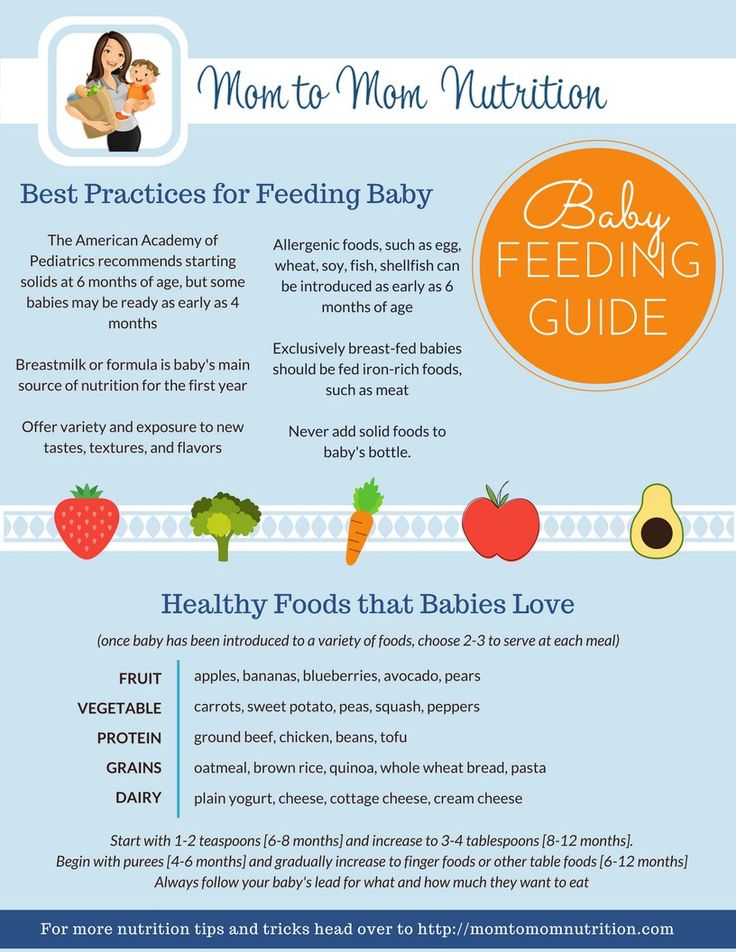
Regardless of whether your child is receiving breast milk or infant formula, at about six months of age, according to WHO* recommendations, the first complementary foods should be introduced. But where to start feeding? And how to do it right? Let's talk in order.
It is at the age of 6 months that the baby's body responds best to new foods. The first complementary foods in combination with breast milk should provide the child with all the useful substances necessary for his growth and development. Also, the timely introduction of complementary foods contributes to the development of the chewing skills of the baby. Russian pediatric practice also allows for earlier introduction of complementary foods - from 4-5 months **.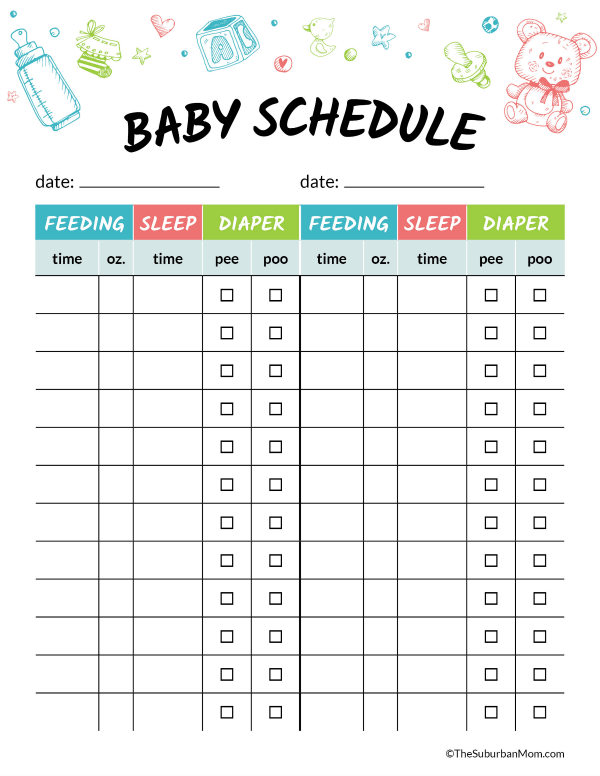
How many months to introduce complementary foods?
To know when it's time to consider introducing food other than milk or formula, watch for signs of complementary feeding. It's time to start complementary foods if:
- Baby sits with support, does not roll over
- The child shows food interest: follows the spoon with his eyes when you eat, tries to steal something from your plate
- Ejection reflex faded, child opens mouth when offered food
Consult your paediatrician before introducing complementary foods. And in order to introduce complementary foods correctly, read the complementary feeding scheme below.
Rules for the introduction of complementary foods
- All new products are started with ½ teaspoon and then gradually adjusted to the age norm.
- New products are best given in the morning or afternoon to be able to track the reaction throughout the day.
- Do not introduce a new product until the previous one has been brought to the age norm.
- Complementary foods are offered before feeding with breast milk or its substitute.
- Until the volume of the product per feeding is brought to the age norm, you should continue to supplement the baby with breast milk or infant formula. Thus, the volume of the complementary food product will gradually increase, and the volume of milk or formula, on the contrary, will decrease until it completely disappears.
Complementary feeding scheme
| Age | Foods and portion sizes |
| 4-5 months | Complementary foods at this early age should be introduced if the child is not gaining weight well or is at risk of developing iron deficiency anemia. Complementary foods are introduced to healthy children from 5 months. There are a number of contraindications for an early start of complementary foods, consult your pediatrician! What foods can we start with:
|
| 6 months | What foods should be in the baby's diet if you introduced complementary foods at 5 months:
What new products are introduced into the diet:
|
| 7 months | What foods should be in the baby's diet by the end of the 7th month:
What new products are introduced into the diet:
|
| 8 months | What foods should be in the baby's diet by the end of the 7th month:
What new products are introduced into the diet:
|
| 9-12 months | What foods should be in the diet of a child at this age:
What new products are introduced into the diet:
|
After 9-12 months volumes of previously introduced products will continue to increase, but remember that the older the child, the more pronounced the individual characteristics, therefore, the food needs of children at this age may differ.
Focus on your baby's weight gain, appetite, and your own common sense.
If you think your child is malnourished or is not gaining weight, please consult a pediatrician.
When using any materials from the site nutriclub.ru, a link to the site is required.
© Nutriclub, 2020
You will also be interested
- Learn more
- Lactose free food for babies
- How much food does a newborn baby need
- Baby food recommendation

- Hipp germany baby food

- Skip hop baby food organizer

- Baby tummy gurgling after feed

- Baby food catcher mat

- What to feed a one year old baby for dinner

- How to make solid food for baby

- Baby will not eat solid food
- What to feed baby carolina wrens