Baby food allergy rash around mouth
My child has a rash around the mouth. Is it a food allergy?
Rashes around children’s mouths are common. They can happen when an irritant touches the skin or through the overuse of topical products. Certain foods may also trigger eczema flare-ups. In rare cases, a food allergy causes the rash.
When a rash appears around the mouth, it can be itchy or cause a burning sensation. The rash may appear red on light skin but be skin-colored on dark skin.
Several substances may trigger a rash, but it is often difficult to identify the cause. Parents and caregivers can help a child avoid possible triggers, including food allergens.
This article reviews the possible causes of skin rashes around the mouth and the treatment options.
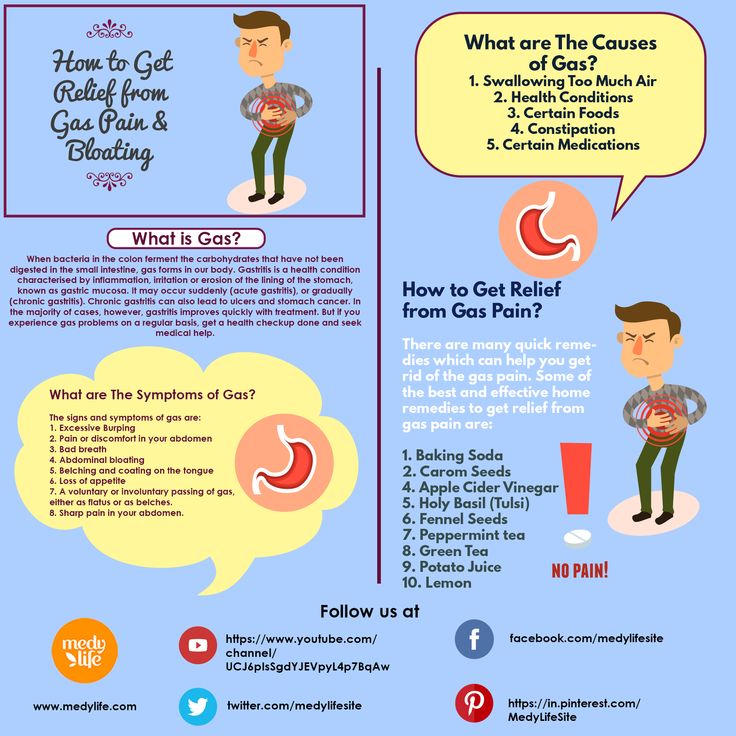
The American College of Allergy, Asthma, & Immunology notes that food allergies can cause skin reactions and rashes when a person comes into contact with an allergen.
However, a rash around the mouth is more likely to have other causes, such as perioral dermatitis.
Food allergy symptoms can range from mild to severe and appear either immediately or some time after contact with the allergen. A severe food allergy can cause anaphylaxis, which can be life threatening.
Quick reactions develop within 1–2 hours of eating a food. To test what causes a quick reaction, doctors use skin prick tests. When the test is positive, it means that the child has developed immunoglobulin E (IgE) antibodies in response to the food. It is easier for doctors to determine the trigger for quick reactions than for delayed reactions.
Delayed reactions develop over 24–48 hours and are probably due to immune cells in the skin reacting to the food. These cells are called T cells. Skin prick tests are often negative in these cases, as IgE antibodies do not cause the reaction.
To identify the cause of a delayed reaction, doctors often recommend eliminating foods from the diet one by one and monitoring any symptoms. This can take a lot of time and persistence.
To discover more evidence-based information and resources for asthma & allergies, visit our dedicated hub.
Various factors can cause children to develop a rash around the mouth. These include:
Perioral dermatitis
Perioral dermatitis is a rash that appears around the mouth. On light skin, it may appear red or pink, resembling an acne breakout. On dark skin, it may be skin-colored. It can cause itchiness, stinging, and burning.
There are several potential causes in children, which can vary among individuals. These include:
- the long-term use of topical steroid creams
- prolonged use of inhaled prescription steroid sprays
- the overuse of heavy face creams or moisturizers
- skin irritants, such as soaps and other substances
- fluoride toothpaste
- acidic foods, such as tomatoes, strawberries, and citrus fruits, touching the skin
Learn more about perioral dermatitis and see some pictures.
Eczema
Eczema is an inflammatory skin condition that typically causes the following skin issues:
- itching
- a raised rash
- dry skin
- oozing or crusting
- swelling
- discoloration
Eczema can develop at any age and sometimes affects the area around the mouth.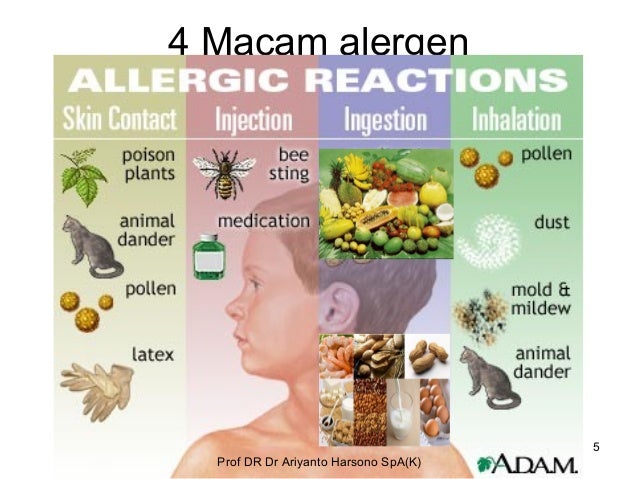 Certain foods, particularly acidic foods, may trigger an eczema flare-up, but they are not the underlying cause of eczema.
Certain foods, particularly acidic foods, may trigger an eczema flare-up, but they are not the underlying cause of eczema.
Learn more about eczema in children.
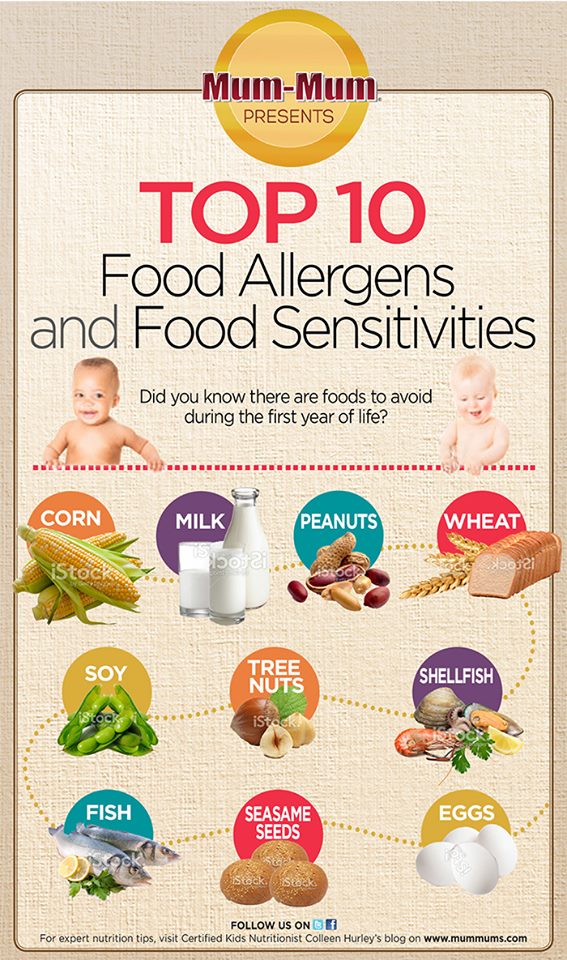
Certain foods can trigger a systemic reaction, including a rash around the mouth. The following food groups are the most common triggers of allergic reactions:
- shellfish
- soy
- peanuts
- cow’s milk
- tree nuts
- eggs
- wheat
- seafood
The following foods are acidic and may cause irritation if they come into contact with the skin:
- tomatoes and tomato sauces
- citrus fruits, such as oranges, lemons, and grapefruits
- strawberries
If a child regularly experiences a rash around the mouth, healthcare professionals may recommend that they undergo testing for food allergies.
Learn more about common foods that cause allergies.
It may not be possible to avoid a rash around the mouth, as the causes can vary. However, people can lower the likelihood of this symptom by:
- avoiding using topical steroid creams and heavy moisturizers around the mouth
- avoiding eating foods that can cause an allergic reaction
- limiting exposure to chemicals or other irritants
- wiping a child’s face gently with a damp face cloth after eating to avoid leaving traces of food on the skin
In some cases, the rash may resolve on its own. A child may only need to avoid exposing their skin to the irritant.
A child may only need to avoid exposing their skin to the irritant.
In other cases, a child may benefit from visiting a dermatologist, who may recommend:
- stopping using corticosteroids, including hydrocortisone cream, if applicable
- switching to fragrance-free, soap-free skin cleansers
- keeping the skin clean and applying fragrance-free moisturizer regularly
A dermatologist can help determine the best course of action and develop a personalized treatment plan for each child.
A parent or caregiver should consider contacting a doctor if a child regularly develops a rash around the mouth.
It is essential to seek emergency medical care if a child develops symptoms of anaphylaxis.
Anaphylaxis is a severe allergic reaction that can be life threatening. The symptoms develop suddenly and include:
- hives
- swelling of the face or mouth
- wheezing
- fast, shallow breathing
- a fast heart rate
- clammy skin
- anxiety or confusion
- dizziness
- vomiting
- blue or white lips
- fainting or loss of consciousness
If someone has these symptoms:
- Check whether they are carrying an epinephrine pen.
 If they are, follow the instructions on the side of the pen to use it.
If they are, follow the instructions on the side of the pen to use it. - Dial 911 or the number of the nearest emergency department.
- Lay the person down from a standing position. If they have vomited, turn them onto their side.
- Stay with them until the emergency services arrive.
Some people may need more than one epinephrine injection. If the symptoms do not improve in 5–15 minutes, or they come back, use a second pen if the person has one.
A rash around a child’s mouth may clear on its own, but it could require changes to the child’s diet or skin care routine. In some cases, a doctor may need to prescribe medication to help treat any underlying infections.
By avoiding triggers, a person should see improvements in their rash.
A rash around a child’s mouth can have various causes. Certain foods can sometimes trigger an immune response that leads to a rash and other symptoms. Severe allergic reactions can be life threatening.
Common causes of a rash around the mouth include reactions to a long-term topical steroid, the use of certain skin care products, or skin contact with highly acidic foods.
Once a person stops their exposure to the trigger, the rash should clear. Identifying triggers can take time and persistence.
My child has a rash around the mouth. Is it a food allergy?
Rashes around children’s mouths are common. They can happen when an irritant touches the skin or through the overuse of topical products. Certain foods may also trigger eczema flare-ups. In rare cases, a food allergy causes the rash.
When a rash appears around the mouth, it can be itchy or cause a burning sensation. The rash may appear red on light skin but be skin-colored on dark skin.
Several substances may trigger a rash, but it is often difficult to identify the cause. Parents and caregivers can help a child avoid possible triggers, including food allergens.
This article reviews the possible causes of skin rashes around the mouth and the treatment options.
The American College of Allergy, Asthma, & Immunology notes that food allergies can cause skin reactions and rashes when a person comes into contact with an allergen.
However, a rash around the mouth is more likely to have other causes, such as perioral dermatitis.
Food allergy symptoms can range from mild to severe and appear either immediately or some time after contact with the allergen. A severe food allergy can cause anaphylaxis, which can be life threatening.
Quick reactions develop within 1–2 hours of eating a food. To test what causes a quick reaction, doctors use skin prick tests. When the test is positive, it means that the child has developed immunoglobulin E (IgE) antibodies in response to the food. It is easier for doctors to determine the trigger for quick reactions than for delayed reactions.
Delayed reactions develop over 24–48 hours and are probably due to immune cells in the skin reacting to the food. These cells are called T cells. Skin prick tests are often negative in these cases, as IgE antibodies do not cause the reaction.
To identify the cause of a delayed reaction, doctors often recommend eliminating foods from the diet one by one and monitoring any symptoms. This can take a lot of time and persistence.
This can take a lot of time and persistence.
To discover more evidence-based information and resources for asthma & allergies, visit our dedicated hub.
Various factors can cause children to develop a rash around the mouth. These include:
Perioral dermatitis
Perioral dermatitis is a rash that appears around the mouth. On light skin, it may appear red or pink, resembling an acne breakout. On dark skin, it may be skin-colored. It can cause itchiness, stinging, and burning.
There are several potential causes in children, which can vary among individuals. These include:
- the long-term use of topical steroid creams
- prolonged use of inhaled prescription steroid sprays
- the overuse of heavy face creams or moisturizers
- skin irritants, such as soaps and other substances
- fluoride toothpaste
- acidic foods, such as tomatoes, strawberries, and citrus fruits, touching the skin
Learn more about perioral dermatitis and see some pictures.
Eczema
Eczema is an inflammatory skin condition that typically causes the following skin issues:
- itching
- a raised rash
- dry skin
- oozing or crusting
- swelling
- discoloration
Eczema can develop at any age and sometimes affects the area around the mouth. Certain foods, particularly acidic foods, may trigger an eczema flare-up, but they are not the underlying cause of eczema.
Learn more about eczema in children.
Certain foods can trigger a systemic reaction, including a rash around the mouth. The following food groups are the most common triggers of allergic reactions:
- shellfish
- soy
- peanuts
- cow’s milk
- tree nuts
- eggs
- wheat
- seafood
The following foods are acidic and may cause irritation if they come into contact with the skin:
- tomatoes and tomato sauces
- citrus fruits, such as oranges, lemons, and grapefruits
- strawberries
If a child regularly experiences a rash around the mouth, healthcare professionals may recommend that they undergo testing for food allergies.
Learn more about common foods that cause allergies.
It may not be possible to avoid a rash around the mouth, as the causes can vary. However, people can lower the likelihood of this symptom by:
- avoiding using topical steroid creams and heavy moisturizers around the mouth
- avoiding eating foods that can cause an allergic reaction
- limiting exposure to chemicals or other irritants
- wiping a child’s face gently with a damp face cloth after eating to avoid leaving traces of food on the skin
In some cases, the rash may resolve on its own. A child may only need to avoid exposing their skin to the irritant.
In other cases, a child may benefit from visiting a dermatologist, who may recommend:
- stopping using corticosteroids, including hydrocortisone cream, if applicable
- switching to fragrance-free, soap-free skin cleansers
- keeping the skin clean and applying fragrance-free moisturizer regularly
A dermatologist can help determine the best course of action and develop a personalized treatment plan for each child.
A parent or caregiver should consider contacting a doctor if a child regularly develops a rash around the mouth.
It is essential to seek emergency medical care if a child develops symptoms of anaphylaxis.
Anaphylaxis is a severe allergic reaction that can be life threatening. The symptoms develop suddenly and include:
- hives
- swelling of the face or mouth
- wheezing
- fast, shallow breathing
- a fast heart rate
- clammy skin
- anxiety or confusion
- dizziness
- vomiting
- blue or white lips
- fainting or loss of consciousness
If someone has these symptoms:
- Check whether they are carrying an epinephrine pen. If they are, follow the instructions on the side of the pen to use it.
- Dial 911 or the number of the nearest emergency department.
- Lay the person down from a standing position. If they have vomited, turn them onto their side.
- Stay with them until the emergency services arrive.
Some people may need more than one epinephrine injection. If the symptoms do not improve in 5–15 minutes, or they come back, use a second pen if the person has one.
A rash around a child’s mouth may clear on its own, but it could require changes to the child’s diet or skin care routine. In some cases, a doctor may need to prescribe medication to help treat any underlying infections.
By avoiding triggers, a person should see improvements in their rash.
A rash around a child’s mouth can have various causes. Certain foods can sometimes trigger an immune response that leads to a rash and other symptoms. Severe allergic reactions can be life threatening.
Common causes of a rash around the mouth include reactions to a long-term topical steroid, the use of certain skin care products, or skin contact with highly acidic foods.
Once a person stops their exposure to the trigger, the rash should clear. Identifying triggers can take time and persistence.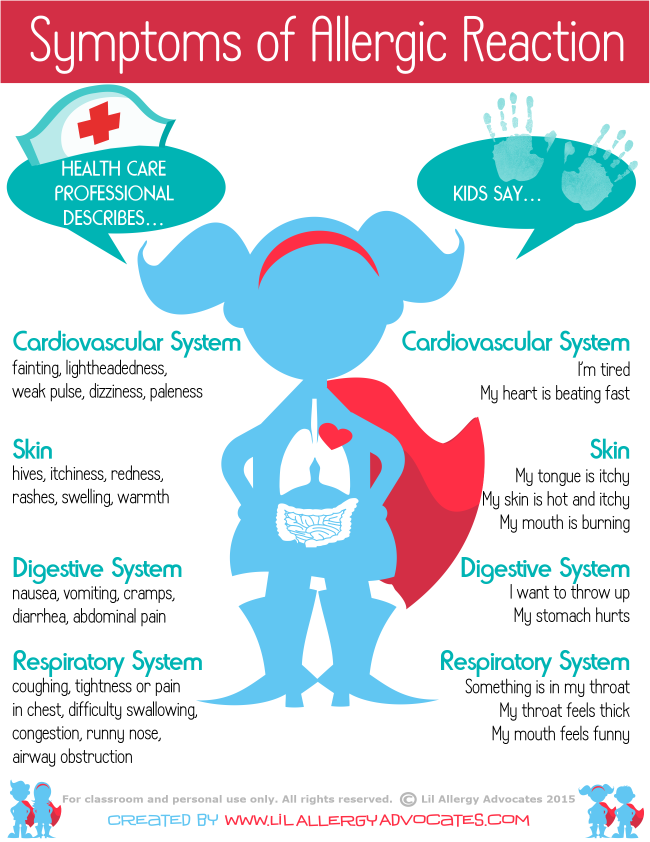
Allergy in infants treatment, allergy in newborns, allergy in infants, food allergy in infants, allergic rash in infants › Outpost Clinic
(044) 502-22-62
(multi-channel)
093 / 068 / 066 / 502-22-62
License of the Ministry of Health of Ukraine
(093) 502-22-62
(068) 502-22-62
- en
- en
- UK
What is the danger of developing allergies in an infant
One of the most common causes of allergy in infants is formula milk. Despite the fact that manufacturers try to adapt milk formulas as much as possible, they still cannot be fully adapted to the child.
If the parents or relatives of the baby have allergies, asthma, allergic rhinitis, urticaria or atopic dermatitis, then through the genes they can "reward" him with a predisposition to allergies. The risk of developing an allergy in a baby to milk formula depends on the degree of predisposition of the child, the more allergies in the family, the higher the likelihood of developing an allergy:
- 10-20% - family without allergies;
- 20-40% - 1 parent is allergic;
- 50-80% - both parents suffer from allergic diseases.
For children with a predisposition to allergies, it is very important not to get cow's milk, which is very high in casein (mother's milk is much less). Therefore, attention should be paid to the fact that children prone to allergies are not supplemented in maternity hospitals with conventional mixtures, as this leads to allergization of the child from the first days, while there is a breakdown in adaptation, and further such children are more likely to develop allergies.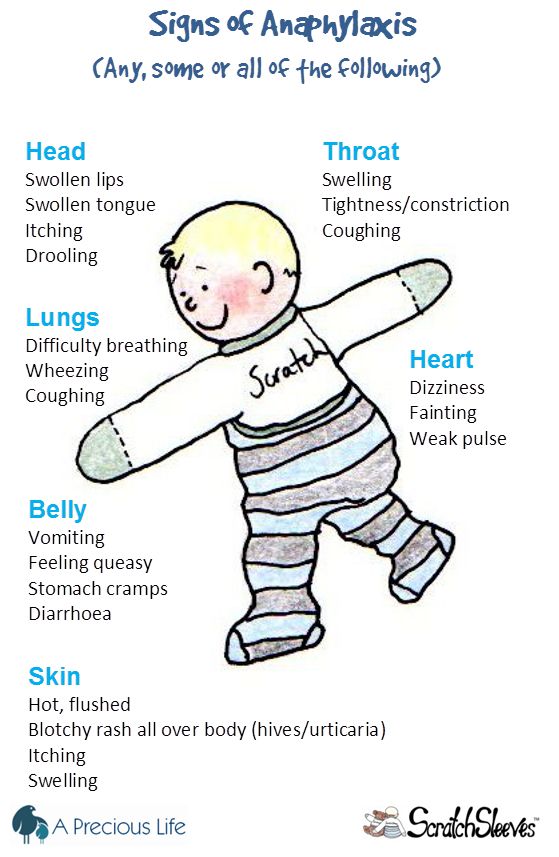
Manifestations of allergy in infants to milk formulas
Signs of allergy to milk protein can manifest themselves both in the immediate type (IgE-dependent, the reaction manifests itself after the use of the milk formula during the first 30 min-2 hours), and the delayed type (IgG4 dependent) - does not appear immediately, but within one or two days. Allergy in infants to formula milk is manifested by:
- rash on the skin in the form of various dermatitis, urticaria, rash around the mouth;
- inflammation on the cheeks, buttocks, legs, back, vulva in the form of redness, papules, accompanied by itching;
- gastrointestinal manifestations in the form of vomiting, hiccups, regurgitation, stool disorders (constipation, diarrhea, bloating, intestinal colic).
What components of milk formula cause allergies in a child? 80% of milk formulas are made on the basis of cow's milk, because cow's milk in its composition is the most identical to human milk and contains the necessary proteins and trace elements for the growth and development of the child.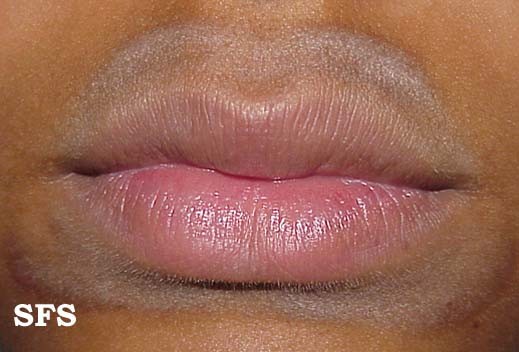 20% of mixtures are made on the basis of soy or goat milk.
20% of mixtures are made on the basis of soy or goat milk.
Food allergies in infants. Allergy of children under one year to milk
Cow's milk contains proteins such as casein, lactalbumin and lactoglobulin. All three proteins can cause allergies in a child, either individually or all at the same time. Lactalbumin and lactoglobulin are thermolabile, which means that they are destroyed by boiling and can no longer cause allergies in a child. Casein, on the other hand, is thermostable (that is, it does not break down when boiled and can cause an allergic reaction). Unfortunately, most children are allergic to casein.
Diagnosis of allergy in infants you can check for allergies in infants to all the main protein components of milk. This is possible only with the help of molecular allergy diagnostics, which determines the allergy not to the entire product, but to its individual components.
Allergic rash in infants. Allergy to cereals
Sometimes milk formulas may contain various cereals (buckwheat, oats, rice), then the child may be allergic to these cereals. Such mixtures are usually intended for older children - after 6 months. Accordingly, tests are made for the respective components of the cereals. You can just separately make IgE for wheat, rye and others. But it is best to do molecular component diagnostics → on the main (major) proteins of cereals (rPhl p1, rPhl p5b), which are included in buckwheat, wheat, rye, fescue and many other cereals, as well as minor (rPhl p7, rPhl p12) proteins, due to which cross-reactions with other foods and plants often occur.
Such mixtures are usually intended for older children - after 6 months. Accordingly, tests are made for the respective components of the cereals. You can just separately make IgE for wheat, rye and others. But it is best to do molecular component diagnostics → on the main (major) proteins of cereals (rPhl p1, rPhl p5b), which are included in buckwheat, wheat, rye, fescue and many other cereals, as well as minor (rPhl p7, rPhl p12) proteins, due to which cross-reactions with other foods and plants often occur.
What are hypoallergenic formulas and are they prescribed for allergies in infants? If initially we know that the parents are allergic and the likelihood of developing allergies in the child is high, then it is recommended to immediately start feeding with hypoallergenic mixtures, preventing the development of allergies in the child.
Hypoallergenic mixtures are hydrolysates of cow's milk proteins (i.e. the protein is broken down into amino acids). As a rule, there is no allergic reaction to these mixtures. But hydrolysates, due to the split protein, become bitter in taste. Therefore, at the beginning it happens that the child does not want to eat, and although his taste buds are not as developed as in an adult, he still feels a bitter taste, especially since mother's milk is sweet. Therefore, it is necessary to gradually accustom the child to the hydrolyzate, at first, in the first 3-5 days, he may refuse, and then he gets used to it. It is important that parents do not rush to cancel the mixture, as a mixture that cannot be fed to the child.
But hydrolysates, due to the split protein, become bitter in taste. Therefore, at the beginning it happens that the child does not want to eat, and although his taste buds are not as developed as in an adult, he still feels a bitter taste, especially since mother's milk is sweet. Therefore, it is necessary to gradually accustom the child to the hydrolyzate, at first, in the first 3-5 days, he may refuse, and then he gets used to it. It is important that parents do not rush to cancel the mixture, as a mixture that cannot be fed to the child.
Types of hypoallergenic mixtures for allergy in an infant
There are hydrolysates depending on the degree of milk protein hydrolysis: moderate and high hydrolysates. If the baby’s allergy is not severe, then moderate hydrolysates are recommended, since they have small amounts of allergens and thus “train” and “accustom” the baby’s immune system.
Does your child have skin rashes, gastro-intestinal problems?! This is a minimally traumatic tactic for examining infants and older children. Search for the cause of problems, taking into account possible allergies.
Search for the cause of problems, taking into account possible allergies.
Stages:
- Fecal analysis for a coprogram, which looks at the degree of digestion of food, signs of inflammation in the intestine, the presence of pathogenic (iodophilic) flora, etc.
- Ultrasound of the abdominal organs, which allows to detect possible developmental anomalies (atresia, underdevelopment of the bile ducts, deformation of the gallbladder, etc.)
- Blood test to determine the level of total immunoglobulin E and / or Phadiatop Infant. Fadiatop Infant is an allergy screening test that contains all the main foods - milk, eggs, wheat, etc., as well as inhaled allergens. If this test is positive, then component allergy diagnostics is necessary. If negative, then go to step
- Component diagnosis of allergy to casein, lactalbumin, lactoglobulin (if the child consumes only milk formula). If the child is more than 6 months old and he uses various cereals, then component diagnostics for cereals is necessary.

- If allergy tests are negative, tests for lactase deficiency and celiac disease are performed.
Prevention of allergies in newborns and older children
Breastfeeding helps to strengthen the child's immune system. Even though the parents are allergic, it is desirable that the mother breastfeed the child. Through breast milk, the child gets acquainted with all the proteins of the surrounding world and, along with an allergic reaction, an anti-allergic reaction, an adaptive one, is produced in it. Thus, the child quickly adapts and outgrows this increased sensitivity to various substances and proteins of the surrounding world.
care and treatment - how and how to cure atopic dermatitis in a child
Atopic dermatitis is a chronic skin disease. Due to a violation of biochemical processes, excessive dryness, peeling, redness occur, inflammatory processes develop, itching is felt. It develops under the influence of allergens, and is often combined with bronchial asthma, food allergies, and allergic rhinitis.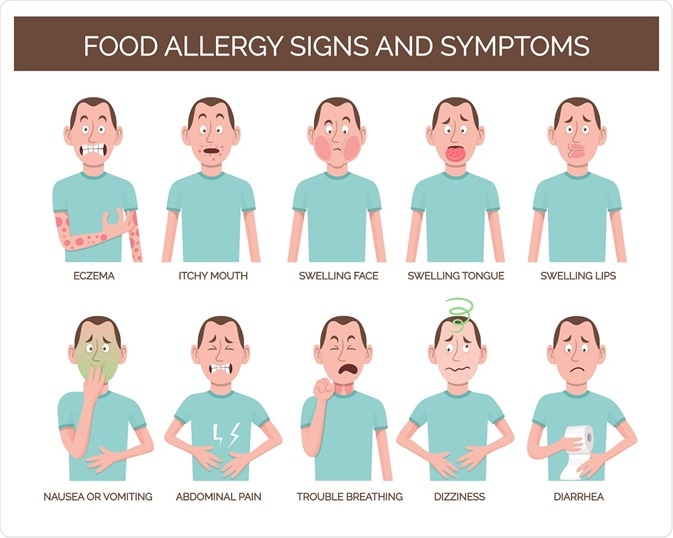 It manifests itself in the first years of life, more often up to 12 months or at the age of 2-3 years, when the children's diet expands and many allergen products enter it. With proper treatment and care, the disease enters the stage of a stable, long-term remission, but it can manifest itself in adolescents, young and old people when they come into contact with allergens, weaken the immune system, and after stress.
It manifests itself in the first years of life, more often up to 12 months or at the age of 2-3 years, when the children's diet expands and many allergen products enter it. With proper treatment and care, the disease enters the stage of a stable, long-term remission, but it can manifest itself in adolescents, young and old people when they come into contact with allergens, weaken the immune system, and after stress.
Symptoms
In children with atopic dermatitis, there is tightness of the skin, redness, the skin is flaky, feels rougher to the touch, thickening may appear. Microscopic bubbles form, around which moisture is released. The child is worried, combing the affected areas. When an infection enters, local inflammation develops, the wounds do not heal well. With a significant spread in young children, general intoxication of the body is manifested: the temperature rises, peripheral lymph nodes increase. Due to severe itching, sleep and appetite are disturbed, the child often cries. Dermatitis most often affects the face, neck, armpits, scalp, groin, areas under the earlobes, popliteal fossae, elbows.
Dermatitis most often affects the face, neck, armpits, scalp, groin, areas under the earlobes, popliteal fossae, elbows.
Prevention
Atopy is translated from Latin as oddity. The causes of the disease are not always possible to establish. But long-term observation of patients and members of their families made it possible to establish that it develops more often:
- with a genetic predisposition - if the parents are healthy, the probability of developing dermatitis in a child is 20%, if one of them is sick - 50%, if both - 80%;
- in case of unfavorable course of pregnancy, active or passive smoking of the expectant mother, eating food that provokes allergy attacks, taking certain medications;
- when a newborn is in a dusty room, insufficient care for his personal hygiene;
- with prolonged exposure to allergens that enter the child's body with food through the respiratory tract.
Breastfeeding up to 6 months and avoiding allergic foods reduces the chance of developing atopic dermatitis.
What to feed a child with atopic dermatitis
In order not to provoke an exacerbation of dermatitis, to relieve itching and redness of the skin, you need to follow a diet. Products that load the immune system are excluded from the children's diet: citrus fruits, chocolate, eggs, honey, seafood. Red (strawberries, cherries, currants, apples) and exotic (mangoes, coconuts, pineapples) fruits are dangerous.
Partial meals are recommended: small portions every 3-4 hours. Products are best boiled, stewed, baked, but not fried. Do not use spices, black pepper. The diet should be balanced and contain enough protein, vitamins, trace elements.
Avoid sugary sodas, chips, crackers, and other snacks for as long as possible. If the baby is breastfeeding, introduce new foods carefully. Add foods once a week to make sure it doesn't cause breakouts. After meals and between meals, offer your baby clean boiled water.
Skin care
To relieve itching and prevent infection of the affected skin, you need to properly care for the skin: cleanse, but do not dry the skin;

Cream or gel removes discomfort during an exacerbation and allows you to sleep, eat, play peacefully. Apply the drug to cleansed skin, treat atopic lesions and areas around them. Do not exceed the recommended dosage and frequency of use.
Rating of the best remedies for atopic dermatitis
For the treatment of atopic dermatitis, use special children's products recommended by a dermatologist. In the period of exacerbations, drugs are prescribed for oral administration, application to atopic areas and general body care:
- drugs for removing allergens from the body - Enterosgel, Laktrofiltrum, Enterodez;
- skin softeners - Atopic cream for daily care;
- anti-itch preparations - Panthenol spray;
- bath products - soft shower gels for atopic dermatitis should be bought at the pharmacy: dermatologists recommend using Atopic bathing gel from head to toe.
Bathing
After a light shower that cleanses the entire body, apply Atopic Bathing Gel to damp skin from head to toe, massage gently and rinse thoroughly. Dry your baby with a soft towel, blotting but not rubbing. After water treatment, apply Atopic skin softening cream for daily care. Apply it several times during the day: after washing your hands and washing your face.
Dry your baby with a soft towel, blotting but not rubbing. After water treatment, apply Atopic skin softening cream for daily care. Apply it several times during the day: after washing your hands and washing your face.
When taking a bath, the water temperature should not exceed 36 degrees. Put the child in the water, offer him toys or other entertainment. After 5-7 minutes, apply Atopic bathing gel from head to toe, rinse well. After bathing, use Atopic cream for daily care, and if itching bothers you, let the cream soak in, and then treat the affected skin with an itch reliever.
How to choose the right products for your child
A dermatologist can recommend more than one product to choose from. They have a similar mechanism of action, but their price can vary significantly. It depends on the active and excipients, the manufacturer, the form of release. When choosing a cream for atopic skin of a child, it is necessary to take into account the possible individual intolerance of individual components.