Baby food for reflux
Feeding A Baby With Reflux | Parenting Blog | Babocush Limited
It may seem like it was just yesterday when you brought home your little bundle of joy then just like that, it’s time to wean your baby off of milk and introduce solid foods. This process might feel overwhelming, especially if your child is still experiencing baby reflux.
What are the symptoms of baby reflux?
It is important to note the symptoms. Repeated crying, vomiting or spitting up, arching of the back or neck during or after feeds, recurrent ear infections, incapacity to sleep or frequent waking, irritability and lastly, frequent hiccups. Babies typically grow out of reflux within the first two years of their life. With that being said, there are still some foods that can aggravate reflux and others that can ease it.
If your baby suffers with reflux, you may feel more comfortable consulting your doctor before you wean your baby off milk and transition them onto solid foods. As a general rule of thumb, you should avoid giving your baby solid food before they’re four months old.
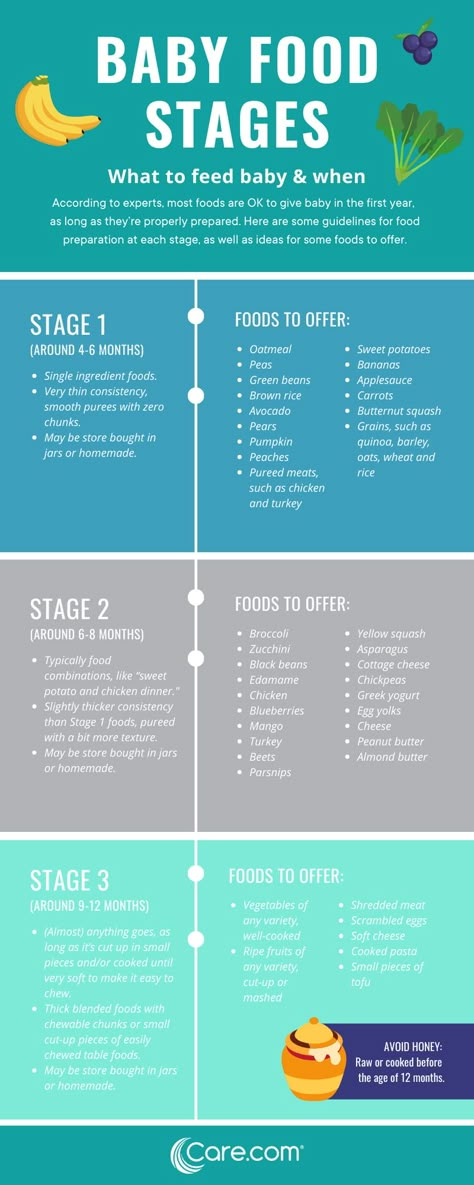
It’s important that you start the weaning process with purees and baby led weaning.The best foods to feed a baby with reflux are purees of vegetables, particularly root vegetables like potatoes, carrots, pumpkin, swede, parsnips and sweet potato. You can also feed your baby any non-acidic fruits. You should avoid citrus fruits like oranges, apples and grapes, tomatoes, peppers, courgettes, cucumbers and aubergines. In addition to that, you should also avoid any foods that have cow’s milk proteins as well as spicy foods.
How to introduce solid foods?
By the time your little one is 4 to 6 months old, you'll probably have your breastfeeding or formula drill down to an art. However, don’t get too comfortable - your baby will soon be ready for "real" food. When it comes to giving your baby solid food, there are a few tips you can follow that can make the process much easier…
Wean your baby slowly
As a general rule of thumb, you should wean your baby slowly and let them take the lead on how much food they need. Don’t hurry meal times, allowing plenty of time for food to settle in your baby’s tummy.
Don’t hurry meal times, allowing plenty of time for food to settle in your baby’s tummy.
Start with smooth foods
You should also start your baby on food that is completely smooth. The textures of different kinds of foods can be a trigger for your infant to spit it up. That is not to say you can never introduce different textures, just make sure that you do so slowly. You should also make sure that you sit your baby upright when feeding them.
Watch out for allergies
You can include any foods that are a part of your family’s diet during complementary feeding. As a precaution, you could introduce foods one at a time for three days at first and, if your baby has no issues, the next new food should be added.
This way, any problematic food would be easier to recognise in the unlikely event that an acute or delayed form of allergic reaction occurs. Once potential allergens, such as eggs and peanuts, have been introduced it is recommended that you continue to include them in your baby’s diet, ideally at least twice a week, to ensure that your baby remains tolerant to that particular food.
Spacing the time in between introducing new foods will give you the opportunity to discover the foods your baby likes and dislikes. Although your baby’s reflux can make introducing solid foods a challenge, it’s by no means impossible.
Related Blogs:
- Why Do Babies Hiccup?
- How To Burp A Baby
Infant Reflux and Introducing Solid Foods - Feeding a Baby with Infant Reflux Solid Foods
Learn about infant reflux and introducing solid foods to a reflux baby
Infant Reflux – Signs and Symptoms
Below are the most common signs and symptoms of Infant Reflux:
• “Colic”
• Irritability when feeding
• Arching back when feeding
• Refusing food or eating only small amounts
• Frequent vomiting
• Sudden or constant crying
• Colic
• Wet burps – when your baby burps and fluid escapes from the mouth
• Slow growth
• Weight loss
• Spells of not breathing
Infant reflux may also manifest with symptoms such as continual coughing or gagging, poor sleep habits, difficulty swallowing and frequent hiccups. Medical experts say that most young infants will spit-up between 1-3 times a day; this is normal and should not be taken as a sole indicator of infant reflux.
Medical experts say that most young infants will spit-up between 1-3 times a day; this is normal and should not be taken as a sole indicator of infant reflux.
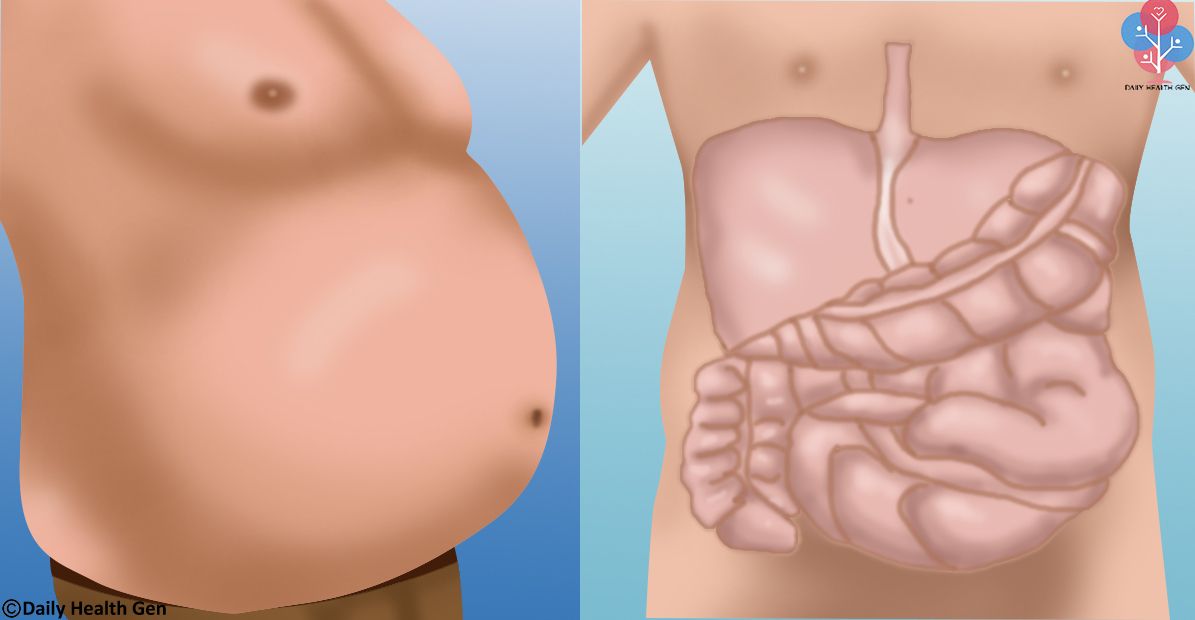
What is Infant Reflux? Is GERD the Same as Infant Reflux (GER)?
Did you know that more than 50% of all babies between the age of newborn to 3 months old will have reflux? For most of these babies, the reflux will disappear on its own and not need drastic medical intervention. Infant reflux affects both formula fed as well as breastfed babies however it is less common in breastfed babies. Infant reflux without the need for medical intervention is known as GER.
GER refers to Gastrosophageal Reflux and is a condition in which “food or liquid travels backwards from the stomach to the esophagus (the tube from the mouth to the stomach). This action can irritate the esophagus, causing heartburn and other symptoms such as spitting up. Gastroesophageal reflux is a common condition that often occurs without symptoms after meals. In some people, the reflux is related to a problem with the lower esophageal sphincter, a band of muscle fibers that usually closes off the esophagus from the stomach. If this sphincter doesn’t close properly, food and liquid can move backward into the esophagus and may cause the symptoms.” NIH
In some people, the reflux is related to a problem with the lower esophageal sphincter, a band of muscle fibers that usually closes off the esophagus from the stomach. If this sphincter doesn’t close properly, food and liquid can move backward into the esophagus and may cause the symptoms.” NIH
GERD is the same condition as GER however GERD will be a severe form of GER that will require medical treatment. Oftentimes GERD will interfere more with baby’s overall health, including weight loss, due to the vomiting and poor eating habits stemming from the pain and discomfort when feeding.
What Types of Solid Foods are Best for a “Reflux” baby?
Thus far, there are no solid food guidelines that have been developed solely for the reflux baby. Many pediatricians do suggest that reflux babies avoid foods that are acidic, such as citrus and tomato. These acidic foods should not be introduced until an infant is 12 months of age anyway due to the acidity. Here are a few of the recommendations for introducing solids for the reflux baby:
• Rice or other cereal – many pediatricians recommend that reflux babies be fed cereal mixed with their formula to help keep the formula down. The weight of the cereal helps keep the formula in baby’s tummy. You should consult your pediatrician prior to trying cereal in the bottle as it is a dangerous practice and recommended only in severe instances.
The weight of the cereal helps keep the formula in baby’s tummy. You should consult your pediatrician prior to trying cereal in the bottle as it is a dangerous practice and recommended only in severe instances.
• Avocado, pears and bananas tend to be good first foods for reflux babies. Avocado is dense and high in important nutrients and fats. Pears are very low in acidity and are easily digested. Studies have shown that Bananas have a mucosal property that actually aids in digestion.
Feeding the Reflux Baby Solid Foods
Making homemade baby food is particularly great for a baby who has reflux. You will be better able to control exactly what your baby is eating and stay away from hidden fillers and possible irritants.
When feeding a baby with reflux, you should try to follow these tips:
• Always feed your reflux baby in a upright position. This will help the food or liquid “stay down”.
• Do not lay your baby down directly after baby has been fed.
• Space out baby feedings of both solid foods and liquid foods into smaller more frequent feedings. This will help the reflux baby keep the foods in the tummy and also will aid in digestion. It is far easier for a reflux baby to digest small amounts as opposed to large amounts.
This will help the reflux baby keep the foods in the tummy and also will aid in digestion. It is far easier for a reflux baby to digest small amounts as opposed to large amounts.
• Avoid dairy products, even yogurts and cheeses.
When Should I Call the Pediatrician About Reflux?
Experts agree that you should call your pediatrician right away if any of the following occur:
• vomiting large amounts or persistent projectile (forceful) vomiting, particularly in infants younger than 2 months old
• vomiting fluid that is green or yellow or that looks like coffee grounds or blood
• difficulty breathing after vomiting or spitting up
• refusing food that seems to result in weight loss or poor weight gain
• excessive crying and irritability
It is very important to consult a pediatrician if your baby begins to refuse feedings. In extreme cases, babies with reflux may develop a feeding aversion and refuse both breast and bottle. It is just to painful for baby to eat and thus, baby chooses to not eat rather than endure the pain.
Infant Reflux – Common Medications and Treatments for Infant Reflux
• cimetidine (Tagamet)
• ranitidine (Zantac)
• famotidine (Pepcid)
• nizatidine (Axid)
Read More on Infant Reflux at
PAGER Pediatric/Adolescent Gastroesophageal Reflux Association
Acid Reflux Connection at Health Central
About.com – Spitting Up and Infant Reflux
Dr. Green – Infant Reflux and Treatment
This site complies with the HONcode standard for trustworthy health information:
verify here.
SHARE ON FACEBOOK SHARE ON PINTEREST
Proper nutrition for GERD - Clinic on Leninsky
The key to solving many problems with the gastrointestinal tract is proper nutrition. Gastroenterologist at the Clinic on Leninsky Katerina Chesskaya tells what you can and should eat for those who suffer from reflux disease.
What is GERD?
Gastroesophageal reflux disease (GERD) is a chronic relapsing disease in which there is a spontaneous, regularly repeated reflux of stomach contents into the esophagus. As a result, the lower esophagus is affected. The reflux of stomach contents into the esophagus is considered normal if it occurs occasionally and is not accompanied by negative factors. The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
As a result, the lower esophagus is affected. The reflux of stomach contents into the esophagus is considered normal if it occurs occasionally and is not accompanied by negative factors. The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
GERD is usually manifested by belching and heartburn after eating or bending forward, and also at night. Another indication of the presence of GERD is pain behind the sternum, extending to the interscapular region, lower jaw, and the left half of the chest. There are also signs of GERD that are not directly related to the esophagus - a cough, shortness of breath, often occurring when lying down, hoarseness, dry throat, rapid satiety, and bloating. The cause of chronic inflammatory diseases of the nasopharynx (pharyngitis, laryngitis, sinusitis, tonsillitis) in 30% of cases is GERD. It has been proven that against the background of GERD there is a risk of developing obstructive pulmonary diseases, including bronchial asthma.
Proper nutrition for GERD
As in the case of many other diseases of the gastrointestinal tract, the main principle of the treatment of GERD is proper nutrition. There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
Here is a list of foods to consider when planning your menu for the day.
Delete:
1. Bread: fresh rye bread, tarts and pancakes.
2. Meat: stewed and fried meat dishes from fatty meat, poultry.
3. Fish: fatty fish, fried, smoked, salty dishes.
4. Vegetables: white cabbage, turnip, rutabaga, radish, sorrel, spinach, onion, cucumbers, salted, pickled and pickled vegetables, mushrooms.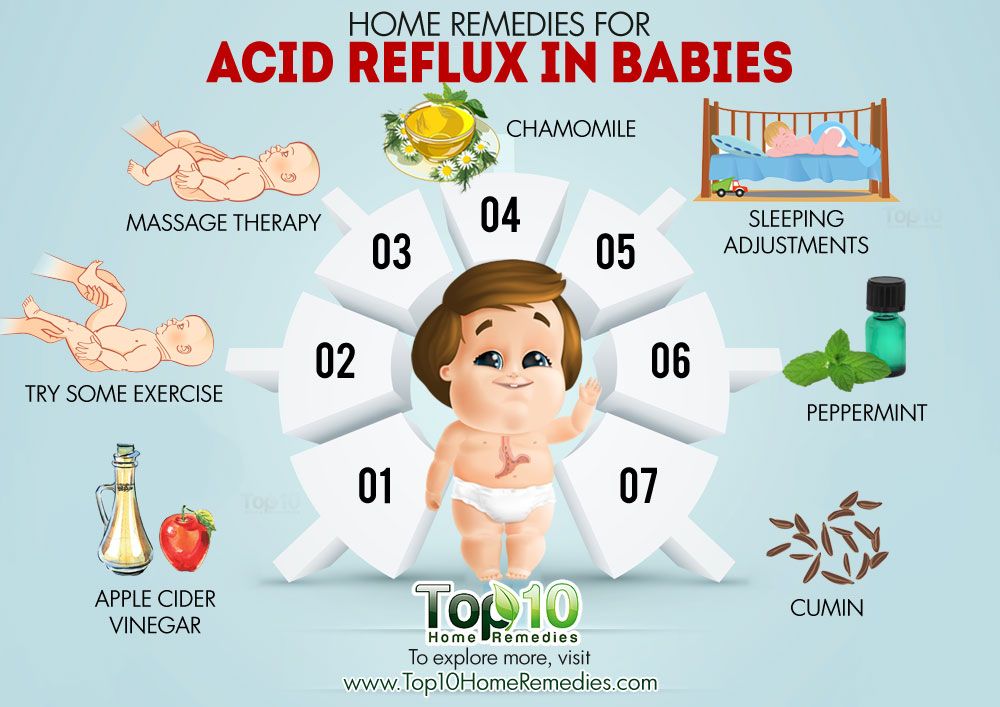
5. Fruit: Raw, sour, unripe fruit, dried fruit puree.
6. Cereals: millet, pearl barley, barley and corn grits, legumes.
7. High acidity dairy products, spicy and salty cheeses.
8. Sweet: halva, chocolate, ice cream, cakes.
9. Drinks: sour, carbonated, fruit drinks, strong tea, coffee and alcohol.
Recommended:
1. Bread: from wheat flour of the first or highest grade, yesterday, dry, uncomfortable baking.
2. Meat: Beef, veal, chicken, rabbit, turkey, all in the form of cutlets, meatballs, soufflés, mashed potatoes and quenelles.
3. Fish: boiled river fish - zander, pike, perch, any low-fat varieties.
4. Vegetables: carrots, cauliflower, potatoes, beets, squash and squash.
5. Fruits: Sweet berries, ripe fruits. Preferably mashed or baked.
6. Cereals: oatmeal, semolina, buckwheat (mashed), rice porridge, on the water with the addition of milk, boiled vermicelli.
7. Dairy products: milk, lean cheese and low-fat sour cream. Cottage cheese dishes made from pureed cottage cheese, for example, cheesecakes, casseroles.
Cottage cheese dishes made from pureed cottage cheese, for example, cheesecakes, casseroles.
8. Sweet: jam, marshmallows, honey, marshmallow, cream and milk puddings.
9. Drinks: weak tea or cocoa with milk, sweet juices and decoctions.
It is also important to adhere to the diet:
— Fractional meals in small amounts and often up to 5-6 times a day.
- Do not lie down immediately after eating, the last meal is 2-3 hours before bedtime.
- Do not work in a slope, exclude the "gardener" pose.
- Do not wear tight belts and limit abdominal exercise.
- Obese people need to normalize body weight.
Remember that only a gastroenterologist can make a diagnosis of GERD (however, like any disease), to accurately determine the patient's condition. At the appointment, the doctor, together with the patient, will find the cause of the disease, outline a treatment plan and further supportive therapy in order to avoid relapses.
At the Clinic on Leninsky, an appointment is being made:
- pediatric gastroenterologist Natalya Medvedeva;
- gastroenterologist Ekaterina Chesskaya.

You can make an appointment with a gastroenterologist at the Clinic on Leninsky
by calling +7 (495) 668-09-86 .
Moscow, Leninsky prospect, building 67, building 2
Tel. .-Fri. 7:30–20:00 Sat-Sun 9:00–18:00
reflux diet in children - 25 recommendations on Babyblog.ru
Good day everyone!
I came to this topic from a neighboring topic (ENT, otitis, runny nose ...), as I have extensive experience in the fight against cough and stenosing laryngotracheitis (stenosis of the larynx).
Six months ago, one of my children had another croup, but with loss of consciousness and respiratory arrest. The child was 5 years old.
All the doctors kept repeating that it was necessary to outgrow all this.
Fortunately, at that moment I came across a doctor who made me take a fresh look at our problem.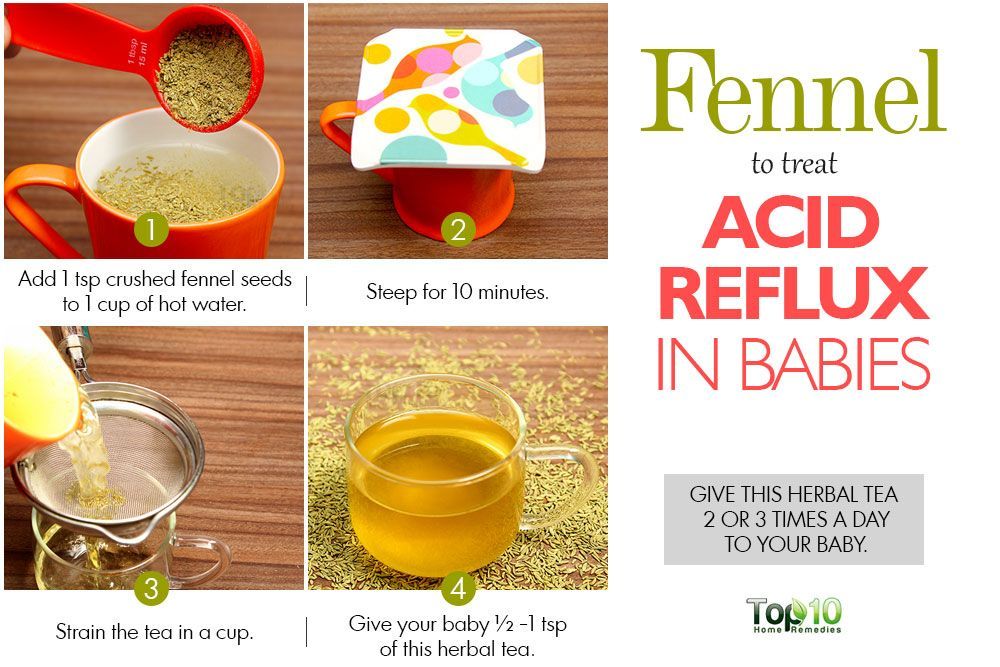 After listening to our story, she diagnosed us without any tests - it turned out to be Reflux (GER).
After listening to our story, she diagnosed us without any tests - it turned out to be Reflux (GER).
(Based on my bitter experience, I can already say for sure - few doctors in Russia will tell you this).
GER is the reflux of gastric juice (hydrochloric acid) into the esophagus and respiratory tract (larynx, bronchi, etc.) when the child is in a horizontal position, mainly during sleep, which causes inflammation of the mucous membrane of the nasopharynx and respiratory tract, with subsequent reactions - asthmatic manifestations , obstructive bronchitis, stenosis of the larynx, adenoids or otitis media.
In children, the ring (sphincter) between the stomach and esophagus is not yet completely closed, so the contents of the stomach freely enter the esophagus and further up, causing constant inflammation.
After this information, which was new to me, I immediately went to the Spiransky Children's Hospital with my two children for an examination. Among many studies (allergens, worms, chlamydia, endoscopy of the larynx, ECG, ultrasound), gastroscopy of the stomach was also done. The result of FGDS was: Duodenitis, Esophagitis, Eunit and GER (reflux).
The result of FGDS was: Duodenitis, Esophagitis, Eunit and GER (reflux).
That is, both children had inflammation of the entire gastrointestinal tract. And we lived and did not suspect it. The children, except for nighttime snoring and frequent morning coughs, had no acute problems (except for laryngitis, which I thought came from a problem in the upper respiratory tract, and not from the stomach).
After that, the gastroenterologist, already at the hospital, again told us about the connection between reflux and cough (in our case) and prescribed treatment for a month.
We treated the stomach. All our problems with coughing went away, we stopped getting sick often. And most importantly, we no longer have stenosing laryngotracheitis.
Now we have gone on a reflux diet (categorically not: chocolate, sour and fried), raised the head of the bed (remove physiologically throwing the contents up), stopped eating at night (last meal 3 hours before bedtime), removed physical activity before sleep and more importantly - after eating the child should be 30 minutes in an upright position.