Baby goes limp after feeding
My Three Day Old Baby Went Limp And Turned Blue; She Was Starving And I Almost Lost Her
First of all, I had always seen your Facebook page and thought to myself “this could never happen to me” or “I wouldn’t be that naive.” But now, can I share my story?
I was induced at 39 weeks due to preeclampsia. Since my cervix was stubborn, however, I ended up with a c-section. My baby was born 7 lbs 11 oz on January 10, 2018.
I was hooked up to magnesium to help with my blood pressure and was bedridden for 24 hours after the c-section. My hospital was a BFHI-certified hospital, and they bragged about their excellent lactation consultants (IBCLCs). That made me happy because I had always dreamed of breastfeeding. I never imagined how hard it would be.
I was recovering from major surgery and felt weak, overwhelmed and quickly became frustrated trying to take care of my baby and breastfeed her. I cried multiple times during my short stay. Why was this so hard? I constantly had to ask for breastfeeding help from the nurses and lactation consultants. By the end of the second day, though, I was proud I got my baby to breastfeed without help. She was constantly feeding, every hour on the dot. No one was concerned about her excessive breastfeeding at all. The nurses seemed pleased with her diapers counts.
We were discharged from the hospital not even 48 hours after my c-section. The first night with my baby was unbearably tough. If she wasn’t breastfeeding, she was crying. This was not fussing. She cried and screamed and the only way she stopped crying was if she was on my breast. My mom stayed by my side most of the night trying to help soothe her, but my baby only wanted to be on my breast.
I knew something was wrong, and I called the pediatrician first thing in the morning. We took the first appointment available, and watched as our little girl finally succumbed to the sheer exhaustion of frantic crying and fell asleep.
The doctor checked her out, and besides her losing 9.8 percent of her birth weight, he was not concerned. We changed a very dirty diaper at the appointment. I told him I had witnessed her peeing the night before as well. He said our little girl looked hydrated. He told us to come back the next day just to be safe, but my milk should be there any second. He never told me to supplement my baby.
The current guidelines by the American Academy of Pediatrics (AAP) now recommends a weight loss threshold of 7%, as the weight at which the feeding of the baby should be evaluated in order to ensure that they do not lose more weight. Weight loss is associated with dangerous conditions like pathological hyperbilirubinemia (jaundice), dehydration, hypoglycemia (low glucose) and hypernatremia (high sodium). All of those markers can be signs of underfeeding and hunger in the newborn.
I nursed her as soon as we got home and we both slept for three hours. When I woke up, I went to check on her and tried to wake her up to nurse. But she just screamed and would not latch. I broke down and sent my husband to the store to buy formula as I knew she needed to eat.
When I woke up, I went to check on her and tried to wake her up to nurse. But she just screamed and would not latch. I broke down and sent my husband to the store to buy formula as I knew she needed to eat.
Not even ten minutes later, my precious, three-day-old baby went limp and turned blue. My mom started trying to revive her as I panicked and called 911. Thankfully as my mom tilted her chin back, she let out a wail. The ambulance arrived a few minutes (but felt like hours) later.
She was rushed back to her birth hospital not even 24 hours after we left. Her blood sugar was only 22, which is dangerously low, and I almost lost my sweet girl. When I heard her blood sugar, guilt and grief overwhelmed me. I could not believe my baby girl was starving. I felt like the worst mom ever knowing I hadn’t been sufficient enough.
She was then transferred to a larger hospital where she spent three days in the NICU getting her blood sugar and electrolytes stabilized. My heart broke to see my baby hooked up to IVs and monitors in the intensive care when only two days earlier she was born perfect.
My heart broke to see my baby hooked up to IVs and monitors in the intensive care when only two days earlier she was born perfect.
Everyone kept telling me I was all she needed. I thought I failed her. Instead, the BFHI protocol failed us.
There, in the Children’s Hospital NICU while her health providers were fighting to stabilize her, I learned how common it was for the unit to get accidental starvation admissions of exclusively breastfed babies, just like mine. These babies do not get enough colostrum. The doctors and nurses in the NICU told me over and over that it wasn’t my fault. They showed me how to pump; they had us take an infant CPR class. My milk finally came in on the day we were being discharged—a full six days after my baby was born.
Now my daughter is two-weeks old and over her birth weight. We tried breastfeeding again, but she refuses to latch. I’m coming to terms with that. A fed baby is the best baby. She is a different baby now, and she hardly ever fusses. We adore her so much.
A fed baby is the best baby. She is a different baby now, and she hardly ever fusses. We adore her so much.
However, I’m still struggling with the guilt and the feeling of failure.
- I regret not self expressing or pumping in the hospital to see if I was making any colostrum (the BFHI hospital discouraged me from doing so).
- I regret not noticing sooner that she was starving.
- I regret being so anxious to leave the hospital after my c-section; if we had stayed one more night, maybe this wouldn’t have happened.
- The greatest feeling I have, though, is betrayal; accidential starvation while attempting to exclusively breastfeed is “common”, and I was not told this, nor was I given any warning signs to watch for.
- It is not talked about and families are not educated about the signs at the hospital. Breastfeeding advocates and BFHI-hospitals are so determined to portray breastfeeding as “perfect” and “natural” that they deny life saving information to families.
I am haunted still by the moment when she turned blue in my lap. Sharing my story helps me to cope. I don’t want any other parent to watch their newborn suffer and almost die from hypoglycemia. I wish every EBF baby would be required to get a glucose check before they leave the hospital and at their first appointment, especially when losing too much weight. Being a first-time mom, I wanted to do everything right. Now I know the public health policy of breastfeeding being “right” isn’t best for everyone, and my daughter was the victim of a flawed public health policy.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation.
 We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters. - Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going. Thank you for your advocacy!
Like this:
Like Loading...
Posted in: Baby-Friendly Protocol Complications: Starvation, Jaundice, Hypoglycemia, Dehydration, Newborn FallsView all posts by B. Jody Segrave-Daly, RN, IBCLC
Reflux in babies
Reflux is when the contents of the stomach come back up towards the mouth after feeding. Read about the complications of reflux and treatments for babies.
Reflux
Reflux in babies, also known as gastro-oesophageal reflux (GOR), is when the contents of the stomach come back up through the mouth after feeds. These regurgitations can sometimes be excessive, frequent and upsetting for your baby.
These regurgitations can sometimes be excessive, frequent and upsetting for your baby.
Reflux is caused by a weak cardia (the elastic-like muscle at the entry to the stomach that normally prevents liquids from being pushed back up). All babies are born with a weak cardia as it’s not yet fully developed. It doesn’t close properly, allowing gastric acid and food to go back up the food pipe.
Although common, especially in boys, reflux is mild most of the time and it disappears on its own when solids are introduced to baby’s diet and when baby starts walking, around the age of one.
It can be difficult to distinguish reflux from vomiting, but it’s important not to get the two confused. Vomiting involves a larger amount of sick which is projected forcefully, and when vomiting occurs frequently, it slows down weight gain.
As long as baby is putting on weight normally, reflux is harmless and you and baby simply have to bear with it.
Complications
Reflux can cause breathing or digestive problems such as oesophagitis (inflammation of the inner lining of the oesophagus caused by the reflux of acids). It can also lead to recurrent breathing infections or ear, nose and throat infections, particularly when the regurgitations take place during sleep, when baby is lying down.
It can also lead to recurrent breathing infections or ear, nose and throat infections, particularly when the regurgitations take place during sleep, when baby is lying down.
If baby becomes bluish or pale when regurgitating, suddenly limp after a feed, regurgitates traces of blood or regurgitates frequently after feeds or during sleep, you should consult a doctor.
Treatment
Baby needs to be calm and in a quiet setting during feeding. Place your baby in a half-sitting position, not lying down, even if you’re breastfeeding. Also, make sure you don’t overfeed.
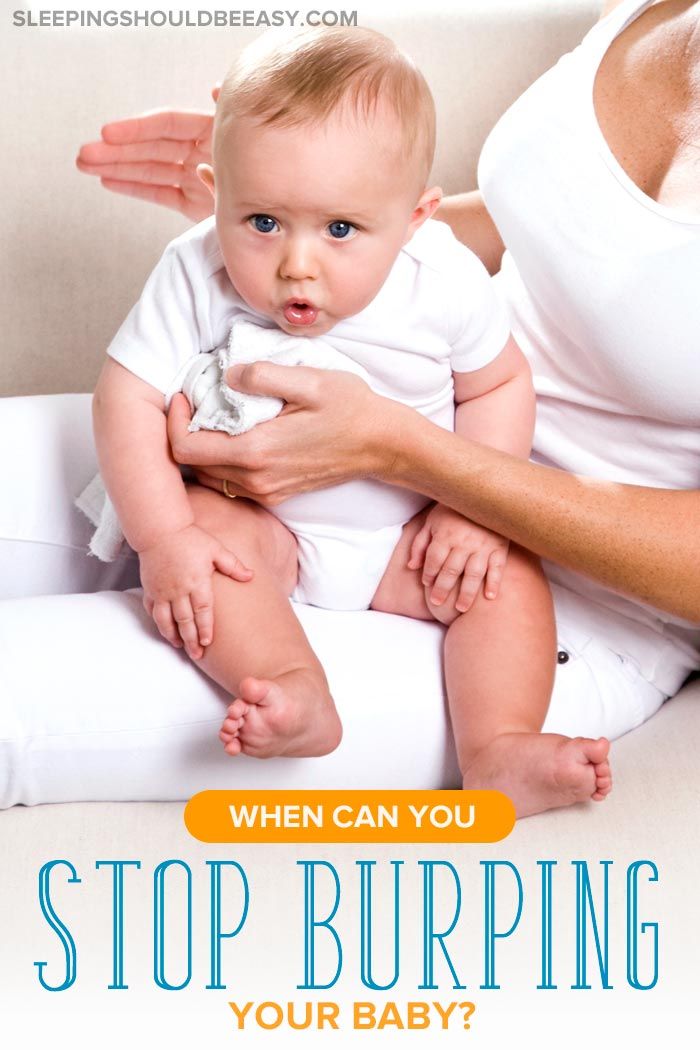
After the feed, put baby in a vertical position for winding: the best way to do this is to place baby against your chest, with the head on your shoulder. Hold the head of young babies, but don’t shake them.
It’s also recommended not to lay baby down straight after a feed. Later, put baby to sleep on the side, steadying the back with a pillow.
Depending on your baby’s age, it’s possible to thicken feeds with rice flour, cornflour or carob flour. Talk to your health visitor about this first.
Talk to your health visitor about this first.
In some cases, your doctor may prescribe medication that helps protect the inner lining of the oesophagus from the damage caused by reflux or reduces acid production in the stomach.
Additional tests
If baby becomes bluish during feeds or experiences other complications, further tests will be carried out to confirm the diagnosis, such as a pH probe that measures the level of acid in the stomach, or a fibroscopy.
If reflux is confirmed, antacids may be prescribed. In rare cases, surgery may be required to treat severe reflux.
why this happens and what needs to be done
When parents first encounter this phenomenon, they may be seriously alarmed. What is it - a symptom of a neurological disease or just whims? In most cases, when the baby arches, throwing his head back, there is nothing to worry about. But there are situations when the intervention of a specialist is necessary.
What you need to know if the baby throws his head back and arches
| The baby arches and throws his head back, but does not show discontent | Probably nothing to worry about. Perhaps he is trying to see something up or behind his back, or learning new skills. In some cases, this may be a manifestation of hypertonicity. In the first six months, this may be within the normal range, but if such phenomena are observed frequently or persist for a long time, you should see a doctor. Perhaps he is trying to see something up or behind his back, or learning new skills. In some cases, this may be a manifestation of hypertonicity. In the first six months, this may be within the normal range, but if such phenomena are observed frequently or persist for a long time, you should see a doctor. |
| The child shows anxiety | A lot here depends on the general condition of the baby. He may arch and whimper if his back is itchy or his nose is stuffy. More vivid signs of discontent will be if the child is tormented by colic, pain, or he is frightened. If you cannot find the cause and / or this condition recurs often, you need to see a doctor for a diagnosis. |
Variants of the physiological norm
In some cases, the child can pull the back of the head back for the simplest reasons: he is studying his body and the world around him. But there may be other reasons as well.
Below, we will consider in more detail all situations where “acrobatic stunts” are a physiological norm.
Hypertonicity in infants under 6 months
Physiological hypertonicity of the limb flexors in children under 6 months of age is considered normal. The fact is that at this age the maturation of the nervous system is still ongoing.
Mastering the skill
Baby mastering the skill of turning over on his stomach. In this case, the child lies on his side and throws his head back, trying to roll over from his back to his stomach. You can help the baby: throw one leg over the other crosswise in the direction where the child wants to roll over. After this, the baby must himself complete the coup with the upper body.
Hysteria
Often the baby, rolling in hysterics, arches, throws back his head, bursting into heart-rending crying. There is nothing wrong with this, take the baby in your arms and try to calm him down. You need to understand what alarmed him and eliminate the cause.
Affective-respiratory attacks
This is the name of the phenomenon when, for some reason, the child stops breathing for a short time. Often, such attacks are accompanied by tantrums, but they can also be provoked, for example, by fright or a sudden change in the environment (for example, when immersed in cold water). What it looks like: the child “rolls up” in a cry, his neck extensor muscles tighten, his torso arches, the nasolabial triangle turns blue, and at the height of the cry, the breath is suddenly held while inhaling, the skin turns blue (1). After a few seconds, the child comes to his senses, breathing becomes regular.
Often, such attacks are accompanied by tantrums, but they can also be provoked, for example, by fright or a sudden change in the environment (for example, when immersed in cold water). What it looks like: the child “rolls up” in a cry, his neck extensor muscles tighten, his torso arches, the nasolabial triangle turns blue, and at the height of the cry, the breath is suddenly held while inhaling, the skin turns blue (1). After a few seconds, the child comes to his senses, breathing becomes regular.
These seizures can occur in healthy children during the first year of life and are usually harmless. But if such situations are repeated often and, perhaps, for no apparent reason, you should consult a doctor to rule out various diseases.
Colic and bloating
A nightmare for parents of babies under the age of 3-4 months. Colic is also a variant of the norm, since intestinal motility in a child is not yet fully developed.
During colic, the baby screams heart-rendingly, arches and throws back his head, blushes strongly, clenching his fists and twisting his legs (2). The abdomen is hard and swollen, the child may refuse to eat. There are several ways to help a baby:
The abdomen is hard and swollen, the child may refuse to eat. There are several ways to help a baby:
- gently massage the tummy,
- put on a clean diaper, ironed with a hot iron,
- give medicine for colic (only after consulting a doctor!).
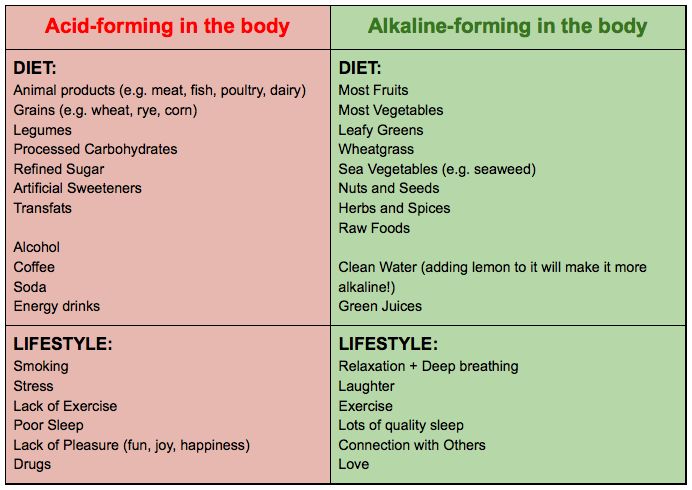
If the baby is breastfed, the mother should pay more attention to her diet and exclude foods that increase gas formation: cabbage, legumes, carbonated drinks, chocolate. In the most extreme cases, the use of a gas outlet tube is acceptable.
Runny nose
It happens that with a runny nose, when it is difficult for an infant to breathe, he begins to arch and worry. Try to help the baby by raising his mattress by 30 degrees to improve the outflow of mucus, and also monitor the humidity and air temperature in the room where the child sleeps.
Trying to find a sleeping position
Sometimes babies arch their backs and tilt their heads back, trying to get comfortable before going to bed. The fact is that in the womb, children are often in unnatural positions, and in the first months of life they can unconsciously repeat them.
The fact is that in the womb, children are often in unnatural positions, and in the first months of life they can unconsciously repeat them.
Other reasons
If the child is arching but not complaining, he may be trying to look at toys hanging over him.
Try to hang the mobile and rattles so that the child does not have to dodge to look at them. Keep in mind that if the toys are hung too close to the baby's face, it may adversely affect his vision.
In addition, the child may arch for very banal reasons: perhaps his back or neck itches.
When the child should be seen by a pediatrician or neurologist
What to do if you are convinced that the baby does not suffer from colic, have tried all the ways, but the baby does not calm down and continues to cry and arch, throwing his head back? To relieve yourself of anxiety, seek the advice of a pediatrician or neurologist.
Let's consider situations when such behavior of the baby may indicate health problems.
Increased intracranial pressure
Sometimes, if the pregnancy was complicated, the child developed intrauterine hypoxia, or there was a difficult delivery, then in the first months the baby may have increased intracranial pressure, due to which he will arch, throw back his head and cry. If intracranial pressure is suspected, it is urgent to show the baby to the doctor to avoid complications.
CSF hypertension symptoms
Irritability, tearfulness, constant crying for no apparent reason, negative reaction to bright lights or loud sounds. Also, often increased intracranial pressure is accompanied by convulsions, profuse regurgitation after feeding. The baby sleeps little and constantly wakes up, when he screams, his lips and chin tremble violently, and the nasolabial triangle also turns blue. In severe cases, the baby's fontanel swells and protrudes, strabismus develops.
Raised intracranial pressure can sometimes be a symptom of a serious illness, such as meningitis, which develops atypically in young children.
Muscular hypertonicity
Arching of the back and tilting of the head may be a sign of muscular hypertonicity in a child. Often, hypertonicity is a consequence of oxygen starvation, fetal hypoxia during pregnancy or during prolonged labor. The most severe consequences can be encephalopathy and cerebral palsy.
Muscle tension can be all over the body or affect only one side of the baby's body. Parents should be alerted not only by the frequent arching of the child and throwing back the head, but also by the violation of the grasping function. Muscle hypertonicity is a reason to show the child to a doctor who, if necessary, will prescribe a course of treatment and massage.
Torticollis
Tilt-back of the child's head can also be caused by torticollis (a pathology of the musculoskeletal apparatus in the neck, due to which the child's head deviates to the side or can be turned to the side). Parents should be alerted if the child's head is always in the same position, and when you try to turn it in the other direction, the child worries and cries. Torticollis requires mandatory treatment, which includes wearing a special collar, massage courses and physiotherapy.
Parents should be alerted if the child's head is always in the same position, and when you try to turn it in the other direction, the child worries and cries. Torticollis requires mandatory treatment, which includes wearing a special collar, massage courses and physiotherapy.
Meningeal syndrome
A complication may occur as a result of otitis media if treatment is started late. This is due to the underdevelopment of the structures of the middle ear in young children.
In this case, the child throws back his head unconsciously, trying to alleviate his condition (3). The following symptoms may also be observed:
- convulsions,
- vomiting,
- confusion,
- decreased motor activity.
You must go to the hospital immediately.
Epilepsy
During an epileptic seizure, the child may arch, throwing back his head strongly, and freeze in this state for a while. After the attack passes, the child relaxes, begins to cry, urination or defecation occurs. Treatment of epilepsy is prescribed only by a doctor and takes place under medical supervision.
Treatment of epilepsy is prescribed only by a doctor and takes place under medical supervision.
Cerebral palsy
If a child arches their back frequently for no apparent reason, this may be a sign of a pathology such as cerebral palsy (4). But other characteristic signs should also be observed:
- developmental delays (late crawling, sitting, walking, talking),
- low or increased muscle tone,
- problems with speech and swallowing, with only one hand, limps at an older age).
Some of these signs can also be observed in healthy children, but if something worries you, it is worth taking the child to specialists in order to rule out a problem or start treatment in time.
Diagnosis
Photo: Andrey Arkusha, globallookpress.com If you are worried that the baby often arches and throws his head back, it is better to seek advice from a doctor who will determine reliably whether this is a norm or a pathology. The doctor will listen to complaints, ask how the pregnancy, childbirth and the first days of the child's life proceeded, specify how often and under what circumstances the baby throws his head back, whether he cries or behaves calmly, whether the nasolabial triangle turns blue, whether the fontanel swells.
If necessary, the doctor can prescribe tests and examinations:
- general blood and urine tests,
- neurosonography (ultrasound of the brain through the fontanel),
- electroencephalography (to rule out epilepsy).
However, CT and MRI scans are extremely rare for young children, since these studies are performed under general anesthesia, so that the child is completely immobile.
Frequently asked questions and answers
Our expert answers readers' frequently asked questions, Veronika Oranskaya, neurologist, epileptologist, member of the League of Evidence-Based Medicine.
The baby throws back his head and arches after feeding - what can it be?
Sometimes tilting the head back after eating or only in a horizontal position during sleep can be a manifestation of the so-called Sandifer's syndrome, which occurs due to gastroesophageal reflux (reflux of stomach contents into the esophagus).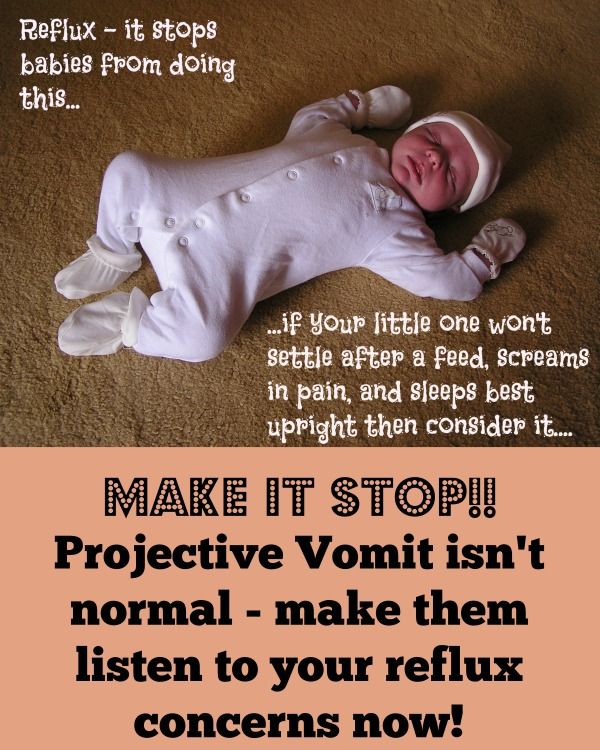 Requires medical advice and treatment.
Requires medical advice and treatment.
Can tilting the head be a symptom of a child's vision problems?
If for some reason (myasthenia gravis, oculomotor neuropathy, congenital feature) the child cannot raise the upper eyelid, he will tilt his head back.
What other possible pathologies can the tilting of the head and arching of the child indicate?
Sudden paroxysmal tilting of the head may be epileptic seizures. A forced constant tilt of the head back may indicate a brain tumor. When combined with an increase in temperature, tilting the head back may indicate meningitis. But most often the reasons for head tilt are all benign: the child doesn't like something, he is learning to roll over, or he just wants to look at something that is behind his head. If in doubt, consult a doctor.
Sources
- Age-dependent manifestations of neuroses in children. M.Yu. Bobylova // Pediatric practice. 2007. URL: https://medi.ru/info/11859/
- Infantile intestinal colic.
 Modern data. N.I. Ursova // Questions of modern pediatrics. 2011. URL: https://cyberleninka.ru/article/n/mladencheskie-kishechnye-koliki-sovremennye-dannye/viewer
Modern data. N.I. Ursova // Questions of modern pediatrics. 2011. URL: https://cyberleninka.ru/article/n/mladencheskie-kishechnye-koliki-sovremennye-dannye/viewer - Features of the treatment of acute otitis media during the Covid-19 pandemic. S.V. Ryazantsev, I.V. Tkachuk, A.E. Golovanov, P.V. Kireev, K.A. Balatskaya, O.S. Don // Medical Council. 2022. URL: https://cyberleninka.ru/article/n/osobennosti-lecheniya-ostrogo-srednego-otita-v-pandemiyu-covid-19/viewer
- What to Know About Back Arching in Babies. Dan Brennan // WebMD. URL: https://www.webmd.com/parenting/baby/what-to-know-about-back-arching-in-babies
the child is lame after DTP vaccination what to do - 22 recommendations on Babyblog.ru
And so I want not 32, but 39 and the finish)) The last ultrasound for sure promised us a daughter, in fact, they were waiting for her.
During this pregnancy, I was too lazy to fly shopping for bags with dowry to the maternity hospital, I decided to order everything on the Internet. Of all that was brought, I liked the envelope most of all, and the Velcro swaddling diapers, we will be discharged in them.
Of all that was brought, I liked the envelope most of all, and the Velcro swaddling diapers, we will be discharged in them.
I don't know who finds my pregnancy harder, me or my son. Of course, he understands that his mother cannot, as before, ride with him on the playground, climb ravines, walk 10 km on foot, etc. etc., and you can’t jump on her with a running start, crash into her stomach and tickle her, but she stubbornly forgets about it.
I'm trying to occupy myself with something creative, as a result there is an unfinished fox from The Little Prince, everything has stalled on the fact that I need to get a sewing machine, and it's a heavy infection. Then I thought about crocheting beaded cords, in general the principle is clear, now you need to fill your hand, plus I started crocheting 1.75, too big, I bought a unit, on Mon. I'll try again.
In general, no matter what the child enjoys)))
all my cleaning has stalled on purely male duties, hang a shelf for books, make room for a stroller, hang hooks, finish the hood . ... and my husband works and comes late. In general, I wipe the dust and vacuum, wash the floors too lazy - hard. I'm sorting out wardrobes from old things and things that I definitely won't wear anymore. I hinted to my husband that you can order a complete cleaning of the apartment in Diana while I'm in the hospital))
... and my husband works and comes late. In general, I wipe the dust and vacuum, wash the floors too lazy - hard. I'm sorting out wardrobes from old things and things that I definitely won't wear anymore. I hinted to my husband that you can order a complete cleaning of the apartment in Diana while I'm in the hospital))
I look at what medical conferences I miss and sigh sadly. I really want to go.
I also became interested in the battle between anti-vaccinators and those who support them with all their might and legs. Well, anti-vaxxers lie in a lot of places. I specifically checked, and some of their arguments are generally pseudoscientific, in general, I wonder why it doesn’t occur to anyone that maybe they are also paid extra? Who and why is another question.
But even with vaccinations, which is true, not everything is so clean and good. Even in the white paper Immunoprophylaxis, which is released every year, there are blunders. Our production and quality control are really very lame, and if we take DPT, then I would definitely wait for Infanrix, with which there are still interruptions.
Having interviewed numerous acquaintances of pediatricians, with little work experience and already a decent experience, I made several conclusions for myself:
1. Parents very often confuse a post-vaccination reaction and post-vaccination complications. It's not the same thing. If the first is a variant of the norm, the second is no longer.
2. Most of the complications that people (to be honest, very rarely literate in this matter) write about on forums and are furiously angry (well, they can be understood) rest on the human factor - an oversight at work (extremely rare)
- violation of the rules for vaccine administration, transportation, storage (the nurse forgot to shake the ampoule with the BCG vaccine, for example. More often, for example, vaccines for individual use should be diluted immediately before administration. But transportation and storage - then how lucky)
- The pediatrician did not examine the child well before vaccination, or did not look at all, took the word of the mother, did not measure the temperature before the introduction. (To be honest, this is negligence, and doctors are guilty of it, but this is not a problem for each individual doctor, but for the system as a whole, 60 people per appointment per 1 person is sadism)
(To be honest, this is negligence, and doctors are guilty of it, but this is not a problem for each individual doctor, but for the system as a whole, 60 people per appointment per 1 person is sadism)
- The mother deliberately lied or gave the doctor false or incomplete information about the child's condition. (For example, it’s very urgent to get vaccinated, oh-oh, we’re flying away tomorrow, and yesterday the snot flowed, we’ll smear anything in front of the office, we won’t notice anything, it’s nothing to worry about. Or the mother thinks that it’s not very important that the child has had ARVI 2 times in the last month. Or the pediatrician sees the child for the first time, there is no card, or not everything is written in it, and the mother does not remember anything, or remembers but not everything, or remembers everything, but does not know which of these is really important).
Such parents are the last to blame themselves for vaccine complications. In general, most parents are very afraid to admit to themselves that they are to blame for any serious condition of the child.
You can throw a pair of slippers at me. But this is my opinion based on experience, observation and no knowledge.
I vaccinated my first child. We just got a weakly diluted BCG, Mantoux is negative, so I will revaccinate at the age of seven. And there was a reaction to Infanrix in the form of edema and hyperemia at the injection site, nothing, it passed.
I will also vaccinate the second one, because I am a doctor and I can bring a bunch of different infections home, i.e. my family is a priori at risk.
From the rational proposals of Ms. Chervonskaya, for example, I definitely like the refusal of vaccinations in the maternity hospital, but I'm afraid that in our reality this is true only for children from normal births at term from healthy mothers who do not live with elderly relatives, alcoholics and others ... To be honest, we don't have many of them across the country. For a particular case, everything is always simple, but if you go beyond a specific family, you can get a disaster.