Baby not burping after night feed
How to Burp a Sleeping Baby: Step-by-Step Guide
Some babies are gassier than others, but most babies will need to be burped at some point. Babies need to burp a lot more often than older kids and adults. They drink all of their calories, which means they can gulp a lot of air.
Burping a baby can be important day and night. Sometimes babies fall asleep while eating and you may need to find a way to burp them while they’re still asleep. It’s remarkable how much a newborn can sleep through.
Even if your baby falls asleep, try burping them for a few minutes before placing them back down to sleep. Otherwise, they make wake up in pain with trapped gas.
Not all babies burp, though, no matter if it’s on their own or with your help. If your baby is one that needs to be burped, read on for ways to do so even when they’re asleep.
It’s common for babies to fall asleep while eating, whether nursing or bottle-feeding. As their tummy fills and they start soothing sucking motions, they often become happy and relaxed and tend to drift off.
This is especially likely to happen at night when their sleep drive is strong. But even if your little one looks content and totally asleep, for some babies it’s important you try to get a burp out of them before lying them back down.
Burping a sleeping baby is basically the same as burping a baby who’s awake. You might move slower to help them stay asleep. Some burping positions are a bit easier to maneuver with a sleeping baby.
For example, many people sit a baby upright on their knee while supporting the baby’s head by cradling their chin. This position uses gravity and the baby’s own weight to get air up and out. However, this position is more likely to wake a baby, so you might not want to try it if your aim is to keep the baby asleep.
To burp a baby, they should be in a slightly upright position so you can put pressure on their tummy. If your baby doesn’t poop right after eating, you may want to change their diaper before feeding them at night so you don’t have to wake them up if they fall back to sleep while eating.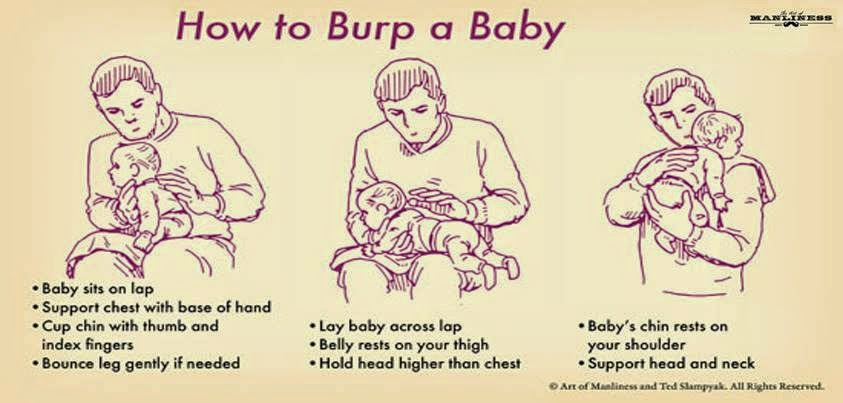
Here are some positions for burping a sleeping baby:
Burp between changing sides, or mid-bottle
A sleepy baby may enjoy their feeding so much that they overeat and don’t realize they need a pause to burp. Help your baby have a gentler burp and avoid any major gas pain by slowing down the feed.
Burp your baby between switching sides at the breast or before they finish their bottle. This will also help your baby make room for more milk instead of burping and spitting up any of their food.
Hold on your shoulder
If you feed your baby in a semi-upright position, you can gently move them all the way upright and onto your shoulder. Babies can keep sleeping in this cozy position while the pressure from your shoulder pushes on their tummy to release gas. Keep a burp rag over your shoulder if your baby tends to spit up.
Hold lower on your chest
Similar to the previous position, you can lift your baby from semi-upright to fully upright and keep them on your chest or sternum area. This may be most comfortable if you’re on a couch. Babies like to curl up with their legs in a frog position (a bonus move to release more gas from their bottoms) and you can support their head and wait for the burp to come.
This may be most comfortable if you’re on a couch. Babies like to curl up with their legs in a frog position (a bonus move to release more gas from their bottoms) and you can support their head and wait for the burp to come.
Rock on your arm (“sloth hold”)
After feeding, you can slowly turn them away from you at 45 degrees so their tummy rests on your forearm. Support their head in the crook of your elbow. Their legs may dangle on either side of your arm. This position puts pressure on their belly and you can gently pat their back until they burp. You can do this position while sitting or standing.
Lay on your knees
If you’re sitting in a chair, simply move your baby to a laying position on their tummy on your knees. You can move your legs side to side to rock them and gently pat or rub their back until a burp comes. A baby can remain asleep here as long as you want to stay sitting.
Burping is one of the many tasks parents have until their child grows into being more self-sufficient. Kids and adults can easily release their own gas, but many babies need help because they have so little control over how their bodies are positioned.
Kids and adults can easily release their own gas, but many babies need help because they have so little control over how their bodies are positioned.
You’ll figure out pretty quickly if your baby is the type who can eat without burping or if they need to be burped every time. If your baby has a lot of gas or spit-up, you should talk to your doctor about reflux.
If you do have a colicky baby but you can’t seem to get them to burp, focus on any comfort measures that work and don’t worry too much about getting burps out. One study suggests that burping won’t help decrease colic.
Whether your baby burps a lot during the day, it may be worth it to burp them after every nighttime feeding. Since you’re already up feeding the baby, make the most of your time by giving a solid attempt at burping. This may get everyone a long stretch of sleep after the feeding.
Gas drops and gripe water are readily available at pharmacies but ask your doctor first before using any of them. These supplements aren’t regulated for safety and may contain dangerous ingredients. If you have a very fussy and gassy baby — whether or not they spit up often — ask a doctor for coping skills. Most babies grow out of this after a few months.
These supplements aren’t regulated for safety and may contain dangerous ingredients. If you have a very fussy and gassy baby — whether or not they spit up often — ask a doctor for coping skills. Most babies grow out of this after a few months.
Risk of choking on spit-up is very rare. It’s still important not to overfeed your baby and to try to burp them after every feeding if they seem to benefit from it.
Burping usually only takes a minute or two. Sometimes a burp will come up as soon as you move your baby upright, and sometimes you have to wait a little while and help things with a gentle pat or tummy pressure.
Another helpful strategy is to get your baby in the habit of falling asleep in their crib rather than while feeding. When you notice them getting sleepy at the breast or bottle, stop the feeding, burp them for a minute or so, and then put them down to sleep. The younger you start this, the easier it is to do.
If your baby is often stiff and uncomfortable, talk with their doctor about more help for relieving gas. Some babies with bad reflux may need to stay upright for 30 minutes after eating, day or night.
Some babies with bad reflux may need to stay upright for 30 minutes after eating, day or night.
If your baby is asleep, try burping them for a minute before you lay them back down. Sometimes babies don’t need to burp as much at nighttime because they eat slower and don’t get as much air while feeding.
If they wake up crying, soothe them, check to see if they need a clean diaper, feed them again if it’s time, and try to burp them after that feeding.
Some people believe that bottle-fed babies are more likely to get gassy, but evidence of this is only anecdotal. Bottles may expose babies to more air as they gulp and may make it easier to overfeed your baby. But every baby is different and even breastfed babies can be very gassy — sometimes because they’re sensitive to food in their mother’s diet.
Though uncommon, a breastfeeding mother may have to experiment a lot before figuring out exactly what they ate to cause their baby’s upset stomach. There’s no solid research to tell a mother what exactly causes her baby’s excess gas. Also, many babies with gas aren’t bothered by it.
Also, many babies with gas aren’t bothered by it.
Burping is a basic but important way you can take care of your baby and keep them comfortable. Even if your baby is asleep, burping may be helpful to allow them to relieve gas so they don’t get uncomfortable or wake up too soon.
How to burp a sleeping baby: Effective methods
When a baby falls asleep without burping, parents and caregivers can try a few methods to help them relieve wind while staying asleep.
The act of breastfeeding or feeding from a bottle often has a calming effect. As a result, it can make many infants fall asleep during or after their meal.
This can pose a problem if the baby has swallowed air during their feed. They may need to release air through a burp, which is more difficult to do when asleep. Their body may be too relaxed to get into a burping position, or the parent or caregiver may not wish to risk waking the baby from their slumber.
However, many people find that they must burp their baby after every feed — sleeping or not. If the baby does not release air through a burp after feeding, they may have discomfort later as it moves through the intestines and causes gas.
If the baby does not release air through a burp after feeding, they may have discomfort later as it moves through the intestines and causes gas.
In addition, some babies are so sleepy at the breast or bottle that they fail to take in enough calories at their meals. It may sometimes be necessary to wake the baby during feeding to help them eat more. Burping the baby may help by eliminating some feelings of fullness and helping them stay awake longer.
A parent or caregiver will often need to decide on a case-by-case basis whether they should try to burp their sleeping baby or simply let them sleep.
Share on PinterestBurping a baby may help relieve discomfort after feedings.As air travels upward, burping positions usually require the baby to be at least partially upright. This position encourages any air bubbles to move upward, passing through the throat and out of the mouth.
It is possible to burp a sleeping baby, often without waking them completely. Each baby is different, so people may need to try various techniques to find one that works.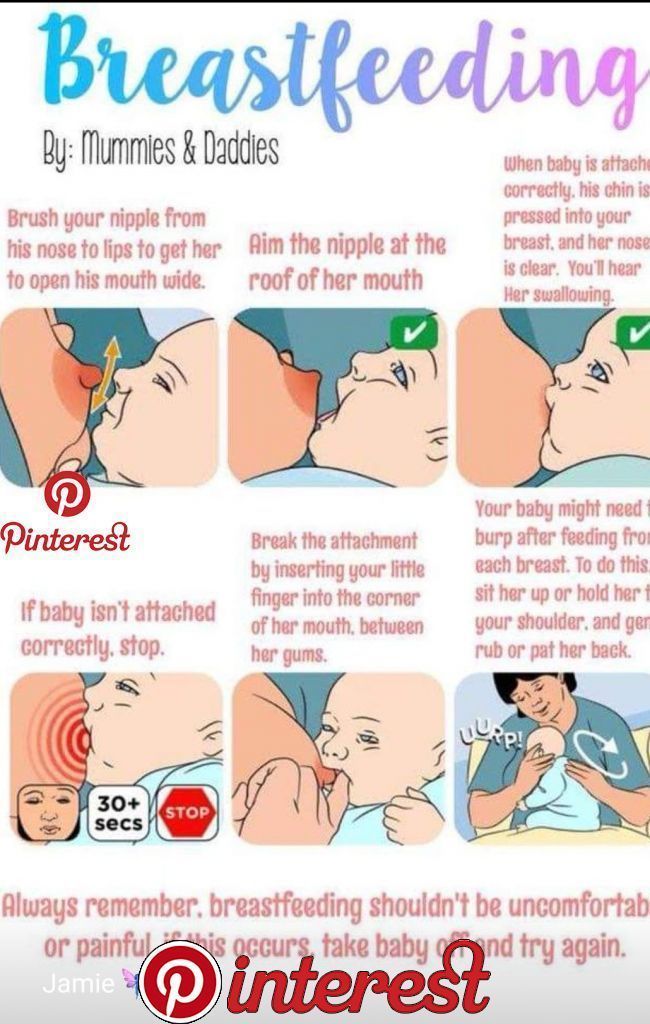
Method 1: Shoulder
This method is suitable for babies who are sound sleepers. It can also be useful if a person needs to wake a baby up to continue their feeding.
- Turn the baby upright and lean them against the upper chest. Put one hand under their buttocks for support. The baby’s head should be on top of the shoulder.
- Gently pat the baby’s back between their shoulder blades. Use an open palm to pat, being firm but gentle.
- If patting does not work, try rubbing their upper back in circular motions with the palm.
If the aim is to keep the baby awake, lightly bouncing them while they are on the shoulder may help wake them while also bringing up a burp.
Method 2: Chest
If a shoulder burp tends to wake the baby up, try a chest burp instead. Placing the baby on the chest can feel more comforting for them than the shoulder, so this position can often allow them to stay asleep after feeding.
- Gently lift the baby to the chest, putting one hand on their back and one under their buttocks.

- Avoid stretching their legs out. Allow their body to stay in a curled up position, which may make them less likely to wake up.
- Use the hand that is on their back to rub it, making circular motions first.
- If rubbing does not produce a burp, try gentle pats between their shoulders.
Method 3: Hip
The hip method works well for people who prefer to breastfeed their baby while lying down. It may help keep the baby asleep because the parent or caregiver does not have to sit up, and the baby is not fully upright.
- Gently place the baby’s tummy down over the hip or belly. Make sure that the baby’s head remains elevated above their body.
- Gently pat their back between the shoulder blades.
- Alternatively, rub their back in an upward circular motion.
Method 4: Arm hold
For smaller babies, the arm hold method can be useful. However, it is not always practical for older or larger babies.
- Place one arm under the baby’s back, allowing them to rest their body on the forearm.
 The baby may already be in this position for feeding.
The baby may already be in this position for feeding. - Carefully turn the baby’s body so that they are resting belly down on the parent’s or caregiver’s forearm with their head in the crook of the elbow. Place the hand between the baby’s legs, holding the baby for stability.
- Rub or pat the baby’s upper back with the other hand.
- When finished, gently roll the baby toward the body. They will then be face up to continue feeding or to go to sleep.
Method 5: Lap
If the parent or caregiver is already sitting in a chair or on a couch, the lap method may work well to keep the baby asleep. It does not require the baby to be upright, which may be more soothing for them.
- While in a sitting position, gently turn the baby over onto their tummy and allow them to rest on the parent’s or caregiver’s thighs.
- Place one arm under the baby’s chin and chest to raise their upper body slightly.
- Use the other hand to pat their back or rub it in circular motions.

- When finished, turn the baby back over onto their back.
The baby may not always burp during or after feeding. In some cases, this may be because the baby did not swallow much air.
Sometimes, however, it takes a little persistence to get a burp out. Here are some helpful tips for parents and caregivers in these instances:
- Burp the baby during the feed. When a baby has finished feeding, they may be especially drowsy and may have swallowed more air. Try burping them before switching breasts or when they are halfway through their bottle.
- If the baby does not burp after 5 minutes of trying, gently lie them down on their back, either in their crib or on another safe surface, such as a playpen. After a few minutes, carefully pick the baby up and try burping them again. Sometimes, lying down helps move the air bubbles around, making them easier to release.
- Keep the baby upright after their feed. Using a baby wrap or sling can be a good way to let the baby sleep in a semi-upright position, allowing the air bubble to escape without any work from the parent or caregiver.

- There is no need to stress if the baby does not burp. There are times when a baby will not burp or has no air to release. If the baby does not burp despite using the methods above, do not worry. One study found that burping does not significantly reduce colic episodes.
The best way to help prevent excess gas in a baby is to try to prevent them from swallowing too much air. Swallowing air is often the result of the baby eating too quickly.
When bottle feeding, follow these tips to help prevent gas:
- Use a slow flow nipple on bottles, especially for newborns. Fast flow nipples may cause the baby to swallow more air.
- Angle the bottle so that air is not getting into the milk or formula while feeding. Doing this usually means tipping the bottle upward at an angle and keeping it tipped as the baby finishes the bottle.
- Test the flow of a bottle’s nipple before giving it to the baby. Tip it upside down and allow a few drops to come out. If the liquid comes out quickly, the nipple may have become worn out.

- Replace bottle nipples if the hole gets bigger, or the nipple shows signs of wear.
When breastfeeding, follow these tips to help prevent gas in the baby:
- Watch for signs of a fast letdown of milk from the breast. If the milk comes out too quickly at the beginning, and the baby is gulping or gasping, take the baby off the breast for a few seconds. Catch the excess milk in a towel or cloth if necessary. Once the milk flow has slowed down, put the baby back on the breast.
- Experiment with different breastfeeding positions. Different babies and women find that certain positions allow them both to breastfeed comfortably. It may help to ask a lactation consultant for tips.
- Make sure that the baby has latched on correctly. The baby’s lips should be sealed and spread out around the nipple. Their lips should not turn inward.
There are ways to burp a sleeping baby without waking them, but no method is foolproof. Parents and caregivers may need to experiment with different burping methods to find which ones work best for them and the baby.
While many babies fall asleep while breastfeeding or bottle feeding, it is important to follow the American Academy of Pediatrics‘ safe sleep guidelines for babies. Following these guidelines may help prevent sudden infant death syndrome (SIDS) and sleep-related infant deaths.
Babies should have regular checkups with a pediatrician to be sure that they are feeding and gaining weight as necessary.
How to help the baby when regulating
Support icon ofKeywords for searching
Home ›!! How to help a child in sprinkling
Home Home ›!! How to help a child in regurgitation
↑ Verki
Breastal feeding - completely special time for mom and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get this straight: Why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagia. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
- Holding the child upright on your legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back.
 At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin. - Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up during feeding. If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
- When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.![]()
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.
Breastfeeding is a wonderful time to strengthen the bond between parent and baby. Every mom and every baby is different, so learning to help your newborn burp properly can take time and practice.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
why the baby spit up after feeding
If a child spits up after feeding, this is in most cases due to the anatomical immaturity of the upper digestive system. More often than others, premature babies, babies with congenital pathologies suffer from regurgitation. Sometimes the cause is the wrong breastfeeding technique.
Sometimes the cause is the wrong breastfeeding technique.
Regurgitation in infants is perhaps the most common occurrence in modern pediatrics. More than half of children spit up at least once a day, which is almost always a physiological reaction.
As the baby grows older, spitting up less and less and by 6 months it practically stops doing it. However, sometimes the problem remains, and burping continues for up to a year. In such a situation, you need to make sure that the gastrointestinal tract is functioning normally and consult a doctor.
Why does the baby spit up after every feed
There is a very simple explanation for this. The esophagus of newborns is a funnel with a wide part at the top, and the sphincter at the transition to the stomach actually gapes and hardly retains food.
Normally, after food enters the stomach, the sphincter contracts and prevents it from “returning” into the esophagus. But in this case, when the stomach is full, part of the contents immediately comes out if the baby takes an inclined or horizontal position.
Infants have two more features: increased pressure over the lower esophageal sphincter, as well as a straight and sometimes obtuse angle of His, formed by the side walls of the esophagus and stomach. In adults, this angle is sharp, which also prevents the reverse reflux of food eaten into the esophagus.
After feeding, do not put the baby on his stomach, it is better to hold him upright in your arms, trying not to put pressure on his chest. But if he still burps, you should not worry, this is a normal process. If in doubt, please contact our doctors. At a remote consultation, they will explain the causes of regurgitation, talk about pathologies. If necessary, they will tell you which specialists to go through.
A few more reasons why a child often spit up
Physiological belching after feeding is due to two factors: swallowing air (aerophagia) and increased intra-abdominal pressure. The first is usually associated with fast and greedy suckling, improper attachment of the baby to the breast, or the wrong position of the bottle when it comes to artificial feeding. An air bubble forms in the stomach, pushing out a small amount of milk or formula.
An air bubble forms in the stomach, pushing out a small amount of milk or formula.
The same results are obtained by a quick change in the position of the baby's body after feeding, which will easily burp if it is immediately started to swaddle, shake, bathe or massage. After all, his stomach resembles an open bottle: tilted / turned over - the contents spilled out.
As for the increase in intra-abdominal pressure, it increases with a too tight diaper or tight swaddling, as well as against the background of increased gas formation, intestinal colic or stool retention.
Regurgitation in newborns after feeding may be due to the lack of a feeding regimen and overeating.
Baby burps an hour after feeding: what does it mean
The most common cause is constipation, which increases intra-abdominal pressure. Food moves slowly through the gastrointestinal tract, so the child can burp an hour or two after feeding.
Attention! Delayed regurgitation combined with delayed defecation may be a sign of a lazy stomach. But such a diagnosis should be made by a doctor.
But such a diagnosis should be made by a doctor.
5 causes of regurgitation in newborns after formula feeding
The selection of artificial nutrition is a purely individual process with an unpredictable result. There is no 100% guarantee that the mixture will suit the child, even if the brand is very popular.
Poor digestion of the mixture may well cause not only frequent spitting up, but also other digestive problems, including colic, constipation and allergic reactions. In addition, store-bought baby food has a denser texture than breast milk and lasts longer in the stomach. Therefore, the likelihood of its reverse promotion to the esophagus after feeding is higher.
Your baby may spit up after every feed because:
- the proportions of dilution of the mixture are violated;
- the feeding regime is not observed;
- the transition from breastfeeding to artificial feeding was too abrupt;
- the wrong bottle is selected;
- allergy.
Improper mixing ratio
Each manufacturer indicates on the packaging of the mixture how much water is required to dilute it, and what volume is suitable for the baby by weight and age. Sometimes mothers mistakenly or intentionally dilute food in a way that is not recommended, and the child eats more than normal. As a result, the surplus, of course, comes out.
Case study:
A breast-fed child after 3 months suddenly began to behave restlessly, sleep poorly, spit up after eating, weight gain became slightly below normal. From a conversation with the mother, the doctor learned that the baby was fed too often, the feeding regimen was not observed. After increasing the intervals between breastfeeding, the regurgitation stopped.
Refusal of night feedings is also undesirable: the daily volume of food is distributed during the daytime, which leads to stomach overload and regurgitation.
Feeding schedule not followed
Unlike natural, artificial feeding involves eating by the hour.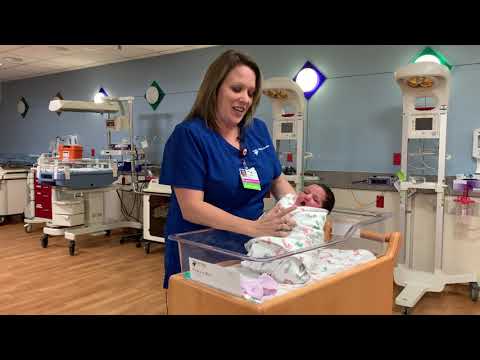
Baby food takes longer to digest, so the recommended interval between feedings is at least 3 hours. If you feed the child more often, he will “give out” the excess back, since the previous portion has not yet been absorbed.
Abrupt transition from breastfeeding to artificial feeding
When changing the diet, the child's body must first get used to, adapt to the new food. This applies not only to the transition from breastfeeding to artificial feeding, but also from one type of mixture to another.
Wrong bottle selected
This refers to the too wide neck of the container, because of which the child swallows a lot of air along with food. Its discharge will provoke regurgitation after feedings.
Allergy
An allergic reaction to cow's milk protein causes inflammation of the intestinal wall, which in turn leads to malabsorption. Carbohydrate metabolism worsens, since secondary lactase deficiency occurs against the background of an inflammatory reaction - a decrease in the synthesis of the lactase enzyme.
As a result, sugar is broken down incorrectly, increased gas formation occurs, and the baby spits up a fountain. In addition, the baby may feel discomfort at the beginning of feeding and react with an increase in nervous excitability during the period of increased intestinal motility. This also often leads to belching.
What does curd spitting up mean
Belching with curdled milk after feeding only indicates that the food was in the stomach for some time and managed to curdle - it was fermented. The reason may be in a change in body position or indicate pyloric stenosis with profuse vomiting with a fountain.
Attention! When spouting against the background of pyloric stenosis, the child spits up profusely, the jet scatters to a distance of half a meter.
What to do
First you need to make sure that you really need to do something. Pediatricians are advised to determine the intensity and frequency of regurgitation on a five-point scale.
| Points | Regurgitation frequency | Volume |
| one | No more than 5 per day | Not more than 3 ml |
| 2 | > 5 times a day | > 3 ml |
| 3 | > 5 times a day | > 0.5 volume of food eaten |
| four | After every feeding | Small amount over 30 minutes or more |
| 5 | At least half of the meals are accompanied by regurgitation | > 0.5 volume of food eaten |
Now you can determine if there really is a problem. The criteria are:
- the baby is not yet a year old;
- he spits up from 2 times a day for 3 weeks or longer;
- before burping there are no precursors, specific signs;
- during regurgitation, the tension of the anterior abdominal wall is not felt;
- there are no difficulties with swallowing, sucking, the child does not take any specific forced position;
- the baby does not begin to sweat a lot, turn pale after he burps, and feels normal;
- he is active, has a good appetite, and is gaining weight appropriately for his age.

The above points indicate that everything is in order.
If the intensity and frequency of spitting up is 3 points or more, this is a reason to consult a doctor. Our doctors are ready to advise on all issues at any time of the day. At a remote consultation, possible causes will be identified, and a plan of further actions will be drawn up.
How parents determine the amount of rejected food
Normal regurgitation after feeding occurs in small volumes, within 1-2 tablespoons. You can determine how much food came out when burping, as follows.
When the child burps into the diaper, you need to pour 1 tbsp. l. water and compare the size of the spots. If they are almost the same, there is no reason to worry.
Alarm symptoms
Medical assistance is necessary if the child spits up a lot after feeding, while crying and acting up. A bad symptom is the requirement of supplementary feeding, that is, the baby remains hungry after he has eaten his portion.
Serious illnesses can present with symptoms such as:
- sudden weight loss, weight gain does not meet the standards;
- lack of stool;
- profuse vomiting with an admixture of bile;
- urination less than 8-10 times a day;
- continued spitting up after the child is one year old.
How to deal with regurgitation: a step-by-step guide
If the baby is spitting up after feeding breast milk or formula, you can start with a nutritional adjustment. When breastfeeding, it is important to ensure that the baby completely captures the nipple along with the areola. His lower lip is usually slightly twisted.
Step 1
It is better to feed the baby while sitting, holding the baby at an angle of 45-60 ° to the chest. In this position, the air freely exits the stomach, thereby reducing the likelihood of reflux of food into the esophagus. After eating, it is preferable to put it on its side in the crib: so the masses, when returning from the stomach, will not enter the respiratory tract. If the child spit up, lying on his back, you should lift him up and turn him face down.
If the child spit up, lying on his back, you should lift him up and turn him face down.
Step 2
After the baby has eaten, it must be held upright (pose of a soldier) for at least 20 minutes.
Step 3
You can partially remove the air from the stomach before feeding, putting the baby on the stomach for 10-15 minutes. With a tendency to intestinal colic, a light massage of the abdomen, which is done in between meals, will help.
Step 4
Even if the child is constantly spitting up, this is not a reason to transfer him to artificial mixtures. But a clear feeding regimen is desirable after a more or less strict period of time. In addition, mom should follow a hypoallergenic diet and exclude foods that can provoke flatulence - cabbage, legumes, black bread.
Step 5
For artificial babies, it is preferable to use a special anti-colic bottle and a nipple with a special design. The bottle has a valve that prevents you from swallowing air while eating. It is also necessary to make sure that the milk does not flow like a river, but slowly drips, that is, the hole in the nipple must have the appropriate diameter.
It is also necessary to make sure that the milk does not flow like a river, but slowly drips, that is, the hole in the nipple must have the appropriate diameter.
Step 6
When buying a mixture for a spitting up baby, it is better to consult a pediatrician. He may recommend a hypoallergenic formula or a formula that does not contain bovine protein. For some children, the so-called anti-reflux mixture is suitable.
Step 7
Normally, complementary foods are introduced from the 4th month of a child's life, but in the presence of regurgitation, it is allowed to include food thickeners in the diet after the 1st month. It can be mixtures with rice flour, rice porridge without milk. But they are used in an amount of a maximum of 1 tsp. in one feeding.
Pitch 8
Do not swaddle too tightly, massage, and generally somehow disturb the child after eating. You can only lightly pat him on the back, putting him on his knees, to prevent spitting up.
Step 9
Is the child overeating? To check this, you just need to weigh it before feeding and after. And it does not matter what he eats - mother's or artificial milk.
FAQ
What symptoms should you call an ambulance for?
+
If, after spitting up, the child does not breathe or has lost consciousness; lips and face take on a bluish tint; reflux - gastric contents - has a green or brownish color, which may indicate intestinal obstruction, gastric bleeding.
Why does a baby spit up breast milk, but formula does not?
+
If everything is in order with the calculation of “doses”, and there is no overfeeding with breast milk, most likely it is lactose intolerance. To clarify the diagnosis, it is necessary to take tests.
Should I supplement my baby if he burps?
+
No, by no means.